Abstract
When comparing the relative effectiveness of different psychological treatment approaches using clinical trials, it is essential to establish fidelity to each manualized therapy, and differentiation between the treatment arms. Yet few psychological therapy trials include details about the assessment of treatment integrity and little is known about the specific techniques used by therapists, or to what degree these techniques are shared or distinct across different therapeutic approaches. The aims of this study were: to establish the fidelity of two established psychological therapies - cognitive-behaviour therapy (CBT) and short-term psychoanalytic psychotherapy (STPP) - in the treatment of adolescent depression; and to examine whether they were delivered with adherence to their respective treatment modalities, and if they could be differentiated from each other and from a reference treatment (a brief psychosocial intervention; BPI). The study also aimed to identify shared and distinct techniques used within and across the three treatments. Audio-tapes (N=230) of therapy sessions, collected as part of a trial, were blind double-rated using the Comparative Psychotherapy Process Scale (CPPS), which includes subscales for cognitive-behavioural and psychodynamic-interpersonal techniques. The treatments were delivered with reasonable fidelity and there was clear differentiation in the use of cognitive-behavioural and psychodynamic-interpersonal techniques between CBT and STPP, and between these two established psychological therapies and BPI. An item-level analysis identified techniques used across all three treatments, techniques that were shared between BPI and CBT, and techniques that were unique to CBT and STPP.
Keywords: adolescent, brief psychosocial intervention, cognitive behavioural therapy, depression, psychodynamic psychotherapy, therapist techniques
Introduction
According to the most widely-accepted hierarchy of evidence for the evaluation of health care outcomes (Oxford Centre for Evidence-Based Medicine, 2009), randomized controlled trials (RCT) are highly rated because of their capacity to minimize potential bias in the estimation of treatment effects. However, RCTs are not without their limitations; for instance, they do not tell us about the process of how treatments exert their effect, which can limit the degree to which their findings can help develop more effective therapies. Therefore while RCTs are important in establishing the evidence base for treatments, they cannot provide the answer to all clinically meaningful questions (Westen et al., 2004).
For RCT findings to be valid, it is essential to establish that the interventions were delivered as planned and that there are meaningful differences between the intervention(s) being tested. Whilst this is relatively straightforward to establish in a trial comparing, for example, two drug treatments, it is more complicated when comparing types of psychological therapy. These complex interventions depend on the skills and training of each clinician, so it must be established that these interventions are delivered as intended. To address these issues, high quality trials of psychological therapies require that interventions are manualized, so that the key principles of each intervention are described in sufficient detail that they can be replicated (Ogrodniczuk & Piper, 1999). But in itself, providing a treatment manual is not sufficient without a process to assess that treatments are delivered as intended (Leichsenring et al., 2011). This process is known as establishing ‘treatment integrity’.
Treatment integrity comprises two key components: treatment fidelity and treatment differentiation. Treatment fidelity considers whether the therapist delivered the treatment as intended by the manual, while treatment differentiation means that the treatments were sufficiently distinct from each other in the techniques used (Perepletchikova, Treat, & Kazdin, 2007). Establishing treatment fidelity and differentiation between treatment arms are essential validity steps in determining the relative effectiveness of different treatment approaches (Perepletchikova & Kazdin, 2005; Sharpless & Barber, 2009), the key objective of most RCTs. Failure to demonstrate treatment integrity makes it difficult to establish if findings are the result of poorly operationalized treatments (Bhar & Beck, 2009). Treatment integrity has also been linked with better clinical outcomes (Katz & Hilsenroth, 2017). If a study fails to establish treatment differentiation, internal validity is compromised, as similarity in outcomes of trialled treatments may be due to unintentional overlap in therapeutic techniques, so cannot be interpreted as evidence for equivalence of outcomes (Bhar & Beck, 2009).
Although the importance of treatment integrity in psychotherapy trials has been recognized (Perepletchikova et al., 2007), the majority of RCTs have failed to adequately describe or evaluate it (Amole et al., 2017; Bhar & Beck, 2009; Perepletchikova et al., 2007). Reasons for this include lack of standardized procedures to assess treatment integrity and demand on resources, as integrity ratings are labour intensive and costly and many studies may not be sufficiently funded. However, there are substantial benefits to using process measures to assess treatment integrity. Rating therapy sessions using validated measures of treatment interventions provides opportunities to explore therapeutic processes used by therapists. Researchers have proposed a number of possible mechanisms of therapeutic change (Webb, DeRubeis, & Barber, 2010), including “common factors”, i.e. elements of treatment that are shared across most or all therapeutic modalities, and “specific factors”, i.e. those which are core, theory-specific techniques that are prescribed for a particular treatment modality (Castonguay, 1993; Castonguay & Holtforth, 2005).
Research comparing therapeutic processes has tended to focus on the techniques that differentiate treatments. For instance, two review papers found seven distinctive features of short-term psychodynamic psychotherapy (STPP; Blagys & Hilsenroth, 2000) and six distinctive features of cognitive-behavioural therapy (CBT; Blagys & Hilsenroth, 2002). These distinctions were replicated in a recent study which used the Comparative Psychotherapy Process Scale (CPPS) to compare the techniques used by master therapists from cognitive-behavioural and psychodynamic orientations (Pitman et al., 2017). In that study, psychodynamic therapists focused on the patients’ emotional and relational patterns, whereas CBT therapists took a more active stance, such as offering advice, providing psycho-education and teaching techniques for coping with symptoms.
Far less is known about the therapy techniques that are shared across modalities. It is possible that different therapeutic approaches share core features, whilst also having their own distinct characteristics. Much of the literature on common factors has focused on therapists’ interpersonal skills and the relationship between therapist and patient (Wampold, 2015), rather than the specific techniques used by therapists across modalities. However, as therapies develop, techniques may migrate from one modality of therapy to another or may be shared by different modalities but referred to and described in different ways. Shared therapeutic techniques may help to explain recent meta-analyses demonstrating equivalent outcomes from different types of therapy for depression in adults (Marcus, O’Connell, Norris, & Sawaqdeh, 2014).
Context for the current study
The data reported in this paper were collected as part of the “Improving Mood with Psychoanalytic and Cognitive Therapies” (IMPACT) RCT. The trial assessed the clinical and cost effectiveness of CBT and STPP, compared to a control treatment, brief psychosocial intervention (BPI) - in the treatment of adolescents with moderate to severe unipolar depression. The planned duration of the treatments were 12, 20 and 28 sessions in the BPI, CBT and STPP arms respectively. Whilst CBT and STPP are established models of therapy, the BPI intervention evolved from non-manualized clinical care used in a previous trial that formalized clinical care as practiced by child psychiatrists and non-medical specialists in a specialist CAMHS setting (Goodyer et al., 2007; Kelvin, Wilkinson, & Goodyer, 2009). In the IMPACT trial, no significant differences in clinical or cost-effectiveness between the three interventions approximately one year after the end of treatment were found (for full details, please refer to Goodyer et al., 2011, 2017). Treatment manuals provided clinical guides and described core principles, treatment procedures, and interventions, based on the underlying theoretical model, rather than giving prescriptive instructions (Cregeen, Hughes, Midgley, Rhode, & Rustin, 2016; IMPACT Study CBT Sub-Group, 2010; Kelvin, Dubicka, Wilkinson, & Goodyer, 2010). The IMPACT study provides an opportunity to investigate the techniques used by therapists in the three treatment arms. Treatment integrity and differentiation of the interventions were reported briefly in the main study report (Goodyer et al., 2017). The aim of this paper is to describe in more detail the distinct and shared therapy techniques used in each of the three treatment arms. Specifically, it aims to address the following research questions:
-
1)
To what degree did CBT and STPP therapists use procedures identified as characteristic of their own therapy modality ('treatment fidelity')?
-
2)
Did CBT and STPP treatments differ from each other and from the control condition (BPI), along critical dimensions of therapist technique ('treatment differentiation')?
-
3)
Among techniques considered to be part of their own conceptual model, which techniques were most or least commonly used in CBT and STPP, and were some specific techniques shared or distinct between therapists offering BPI, CBT and STPP?
Method
Design
Therapists and young people in the IMPACT study agreed to their therapy sessions being audio recorded for research purposes. A sample of therapy session audio recordings were rated using the CPPS to assess treatment fidelity, and the present study draws on these data to address the research questions outlined above. In addition, young people completed a battery of measures before, during, and after treatment, which are not reported here. The IMPACT study protocol was approved by the Cambridgeshire 2 Research Ethics Committee (Reference: 09/H0308/137).
Sample
A sample of 230 tapes (76 CBT tapes, 81 STPP tapes and 73 BPI tapes) were randomly selected from the available session recordings across the entire study and stratified by modality and timing (‘early’ or ‘mid/late’). ‘Early’ sessions were those in the first third of the planned treatment (N = 114); mid-late sessions were those in the middle or last third of the planned treatment (N = 116). The slight difference in the number of sessions rated in each arm was not deliberate, but arose due to the number of tapes available by treatment arm and site, with slightly more tapes being available for the STPP arm of the study.
The 230 sessions used in this study were selected from the treatment of 139 patients. For 91 patients, an early and mid-late session was rated and for the remaining 48 cases, one session was rated (24 early sessions; 24 mid-late sessions). The sample consists of sessions from 27 BPI, 26 CBT and 27 STPP therapists who had a mean of 2.9 therapy session rated. Therapists had training in one of the three modalities and therefore therapists did not crossover between treatment arms.
The average age of adolescents in this sample was 15.66 (SD = 1.57) and 70% were female, similar to the overall IMPACT sample, so our subset is representative of the full IMPACT sample in terms of age and gender. The average number of therapy sessions attended for the cases in the sample were 10.67 (SD = 6.06), 11.46 (SD = 5.49) and 17.77 (SD = 8.74) in the BPI, CBT and STPP arms respectively. This is somewhat higher than the mean number of sessions attended by young people in the study overall, likely to be the result of randomly selecting sessions, so that patients with more sessions had a higher chance of having their session selected.
Instrument
Comparative Psychotherapy Process Scale – External Rater form (CPPS)
The CPPS assesses the degree to which a therapist uses general techniques of psychodynamic-interpersonal (PI) and/or cognitive behavioural psychotherapy (CB) (Hilsenroth, Defife, Blake, & Cromer, 2007). CPPS items (shown in Table 1) are rated on a 7-point response scale, ranging from 0 (“not at all characteristic”) to 6 (“extremely characteristic”). The 20-items form two distinct subscales: PI and CB. The psychometric properties of the CPPS have been well established in studies with adults (Goldman, Hilsenroth, Owen, & Gold, 2013; Hilsenroth et al., 2007).
Table 1.
Items on the CPPS, and mean scores for each of the treatment arms.
| Scale | Item | Description | BPI | CBT | STPP |
|---|---|---|---|---|---|
| CBT | 2 | Therapist gives explicit advice or direct suggestions to the patient. | 1.98 (1.66) | 2.55 (1.78) | 0.32 (0.59) |
| 3 | Therapist actively initiates the topics of discussion and therapeutic activities. | 3.65 (1.12) | 3.91 (0.97) | 1.92 (1.21) | |
| 6 | Therapist focuses discussion on the patient’s irrational or illogical belief systems. | 0.75 (1.05) | 2.30 (1.95) | 0.37 (0.52) | |
| 9 | Therapist suggests specific activities or tasks (e.g. homework) for the patient to attempt outside of session. | 0.47 (0.82) | 2.35 (1.67) | 0.04 (0.29) | |
| 11 | Therapist explains the rationale behind his or her technique or approach to treatment. | 1.36 (1.13) | 2.69 (1.52) | 0.44 (0.81) | |
| 12 | Therapist focuses discussion on the patient’s future life situations. | 1.24 (0.98) | 1.41 (1.19) | 0.94 (1.08) | |
| 15 | Therapist provides the patient with information and facts about his or her current symptoms, disorder, or treatment. | 3.18 (1.65) | 4.11 (1.52) | 0.93 (0.97) | |
| 17 | Therapist explicitly suggests that the patient practice behavior(s) learned in therapy between sessions. | 0.21 (0.66) | 0.83 (1.19) | 0.01 (0.08) | |
| 18 | Therapist teaches the patient specific techniques for coping with symptoms. | 0.38 (1.05) | 1.11 (1.30) | 0.02 (0.10) | |
| 20 | Therapist interacts with the patient in a teacher-like (didactic) manner. | 2.48 (1.66) | 3.59 (1.43) | 0.49 (0.73) | |
| PI | 1 | Therapist encourages the exploration of feelings regarded by the patient as uncomfortable (e.g. anger, envy, excitement, sadness, or happiness) | 1.23 (1.10) | 1.56 (1.26) | 3.00 (1.53) |
| 4 | Therapist links the patient’s current feelings or perceptions to experiences of the past. | 0.84 (1.09) | 0.71 (1.07) | 1.12 (1.05) | |
| 5 | Therapist focuses attention on similarities among the patient’s relationships repeated over time, settings, or people. | 0.66 (0.79) | 0.82 (1.03) | 1.69 (1.29) | |
| 7 | Therapist focuses discussion on the relationship between the therapist and patient. | 0.28 (0.55) | 0.39 (0.67) | 2.23 (1.88) | |
| 8 | Therapist encourages the patient to experience and express feelings in the session. | 2.96 (1.28) | 3.19 (1.41) | 4.35 (1.43) | |
| 10 | Therapist addresses the patient’s avoidance of important topics and shifts in mood. | 0.62 (0.89) | 0.60 (0.86) | 1.53 (1.45) | |
| 13 | Therapist suggests alternative ways to understand experiences or events not previously recognized by the patient. | 2.42 (1.53) | 2.63 (1.62) | 4.41 (1.53) | |
| 14 | Therapist identifies recurrent patterns in patient’s actions, feelings, and experiences. | 1.08 (1.07) | 1.53 (1.30) | 2.23 (1.47) | |
| 16 | Therapist allows the patient to initiate the discussion of significant issues, events, and experiences. | 2.29 (1.08) | 2.09 (0.97) | 4.10 (1.16) | |
| 19 | Therapist encourages discussion of patient’s wishes, fantasies, dreams, or early childhood memories (positive or negative). | 1.27 (1.35) | 1.29 (1.25) | 1.77 (1.28) |
Note: CPPS (Comparative Psychotherapy Process Scale); CB (Cognitive-Behavioural); PI (Psychodynamic-Interpersonal).
In the IMPACT trial, the CPPS was used to assess treatment fidelity in the CBT and STPP arms. BPI sessions were also rated on the CPPS to assess if BPI could be differentiated from CBT and STPP sessions. The CPPS was not expected to capture specific techniques used by BPI therapists and therefore an additional measure was used to rate fidelity to the BPI model. The development and results of application of a new BPI specific measure (BPI-S) has been reported elsewhere (Goodyer et al., 2017). The present article focuses on the data collected using the CPPS, allowing comparison of techniques across the three treatment modalities.
As this was the first study to use the CPPS with an adolescent population, there were no predetermined cut-offs established for 'adherence'. Based on discussion with the manual leads, using their clinical judgement and knowledge of the treatment models, it was pre-determined that sessions would be judged to be ‘adherent’ to the CBT model if the total mean score for items on the CB subscale of the CPPS was ≥ 2, indicating that the use of CB techniques was at least ‘somewhat characteristic’ of a session. The same criteria was applied to sessions, with average ratings ≥ 2 on the PI subscale being considered adherent to the STPP model.
Seven postgraduate psychologists, blind to treatment allocation, rated the selected sessions using the CPPS. Raters received approximately 30 hours of training, until they demonstrated high inter-rater reliability. Raters, who were not clinicians and had no specific allegiance to any treatment arm in the study, listened to the entire session before coding. All tapes were double rated for the purpose of reliability and to improve the precision of the estimate for each tape. An intraclass correlation coefficient (ICC) was calculated to evaluate reliability between the double ratings. An average measure ICC of 0.83 on the PI subscale and 0.88 on the CB subscale indicated good reliability on both subscales (Fleiss, Levin, & Paik, 2004). As the double ratings were deemed reliable, the two ratings for each session were averaged and the average scores are used for the analyses in this study.
Statistical Analysis
Statistical analyses were conducted in R version 3.3.2 (R Core Team, 2016) and figures were created using the ggplot2 package (Wickham, 2009). We tested the effect of timing (early vs mid/late) using mixed effects models with random intercepts for participants and therapists. We found no evidence for an effect of time (early or mid/late) on scores on the subscales, or on scores on the individual CPPS items. Therefore subsequent analyses were conducted without including terms for time.
To assess treatment fidelity, summary statistics of the two subscales (CB and PI) of the CPPS were determined for each treatment modality. To assess treatment differentiation, scores on the CB and PI subscales were compared using linear mixed effects models with random intercepts for therapists and participants, and fixed effects for treatment arms. The following hypotheses were tested:
-
(i)
STPP sessions should be lower than CBT on the CB subscale.
-
(ii)
CBT sessions should be lower than STPP on the PI subscale.
-
(iii)
BPI sessions should be lower than CBT on the CB subscale, and lower than STPP on the PI subscale.
Descriptive statistics were calculated to assess which techniques, considered part of their own conceptual model, were most or least commonly used in CBT and STPP. To assess whether some specific techniques were shared or distinct between therapists offering the three therapies, for each of the 20 items on the CPPS, mixed effects models were used to test treatment arm differences. As before, treatment arms were included as fixed effects and therapists and participants were included as random effects. These analyses were exploratory, so no hypotheses were tested.
Results
Research Question 1: To what degree did CBT and STPP therapists use procedures identified as characteristic of their own therapy modality?
Based on the CPPS ratings, 74% of the CBT sessions had a score of ≥ 2 (‘somewhat characteristic’) on the CB subscale and could therefore be considered adherent to the CBT model. A total of 80% of the STPP sessions had a score of ≥ 2 (‘somewhat characteristic’) on the PI subscale and could therefore be considered adherent to the STPP model (Table 1). For the purposes of comparison, the BPI fidelity assessment found that, based on the BPI-S ratings, 81% of the BPI sessions were rated as 2 or above on 2 out of 3 'core' items and 4 out of 8 items in total, so could be considered adherent to the BPI model (Goodyer et al., 2017).
Research Question 2: Did CBT and STPP treatments differ from each other and from BPI, along critical dimensions of therapist technique?
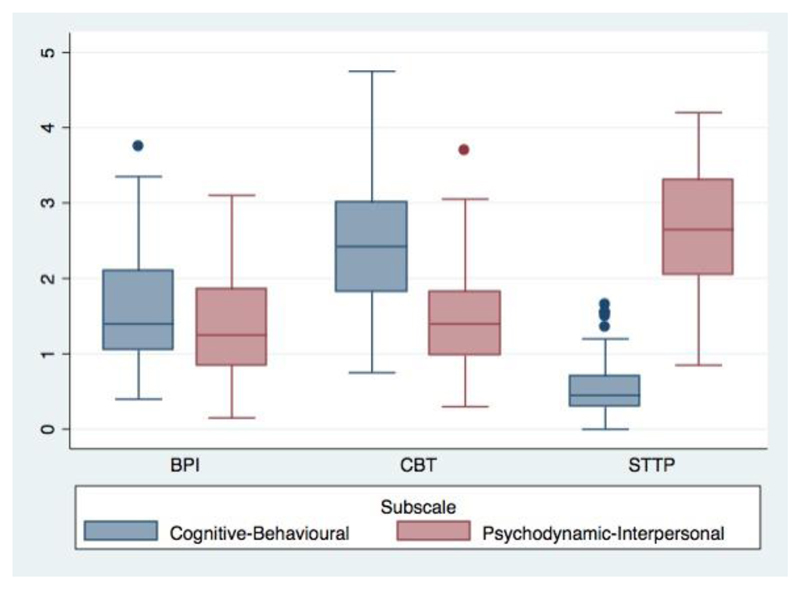
Box plots of the mean scores for each domain of the CPPS for the three treatments are shown in Figure 1. Corresponding summary statistics are presented in Table 2 and model estimates are shown in Table 3. As predicted, CBT sessions were rated significantly higher on the CB subscale than STPP sessions (mean difference = +1.96, 95% confidence interval (CI) 1.71 to 2.21; p < 0.001) and STPP sessions were rated significantly higher on the PI subscale than CBT sessions (mean difference = +1.21, 95% CI 0.90 to 1.52; p < 0.001). BPI sessions were significantly lower on the CB subscale than CBT sessions (mean difference = -0.90, 95% CI -1.16 to -.65; p < 0.001) and significantly lower on the PI subscale than STPP sessions (mean difference = -1.22, 95% CI -1.53 to -0.92; p < 0.001). Thus, CBT and STPP treatment arms were significantly differentiated, based on the CPPS ratings; and both were significantly differentiated from the reference treatment, BPI.
Figure 1. Distribution of scores on the Cognitive-Behavioural and Psychodynamic-Interpersonal subscales on the CPPS, for each of the treatment arms.
Note: BPI = Brief Psychosocial Intervention; CBT = Cognitive-Behavioural Therapy; STPP = Short-Term Psychoanalytic Psychotherapy.
Table 2.
Treatment fidelity on the CPPS by Treatment Arm
| Cognitive-Behavioural Subscale | Psychodynamic-Interpersonal Subscale | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentile | Percentile | ||||||||||||||
| N | ≥2 | % adherent |
Mean | S.D. | Median | 25 | 75 | ≥2 | % adherent |
Mean | S.D. | Median | 25 | 75 | |
| BPI | 73 | 21 | 28.77 | 1.57 | 0.71 | 1.40 | 1.05 | 2.10 | 13 | 17.81 | 1.37 | 0.66 | 1.25 | 0.85 | 1.85 |
| CBT | 76 | 56 | 73.68 | 2.49 | 0.91 | 2.43 | 1.83 | 3.00 | 15 | 19.74 | 1.48 | 0.69 | 1.40 | 0.98 | 1.83 |
| STPP | 81 | 0 | 0.00 | 0.55 | 0.37 | 0.45 | 0.30 | 0.70 | 65 | 80.25 | 2.64 | 0.8 | 2.65 | 2.05 | 3.30 |
Note: Subscale score ≥ 2 is considered adherent to the CB / PI subscale
Table 3.
Model estimates from mixed effect models comparing mean scores on the CPPS subscale
| Comparison | CPPS subscale | Mean difference | 95% CI |
|---|---|---|---|
| CBT vs STPP | CB | +1.96* | 1.71 to 2.21 |
| STPP vs CBT | PI | +1.21* | 0.90 to 1.52 |
| BPI vs CBT | CB | -0.90* | -1.16 to -0.65 |
| BPI vs STPP | PI | -1.22* | -1.53 to -0.92 |
Note: * p <0.001; CB = Cognitive Behavioural; PI = Psychodynamic Interpersonal; CI = Confidence Interval.
In some sessions, therapists appeared to employ techniques typically associated with a treatment other than the therapist’s specialty. Table 2 illustrates the mean score on the CB and PI subscales for each of the three treatments. 20% of CBT sessions had a mean rating of 2 or above on the PI subscale of the CPPS, indicating that PI techniques were ‘somewhat characteristic’ of a minority of CBT sessions. By contrast, none of the 81 STPP sessions were considered as using CBT techniques at a 'somewhat characteristic' level. 29% of BPI sessions were rated as 2 or above on the CB subscale of the CPPS, indicating that in a minority of BPI sessions, CB techniques were used at a 'somewhat characteristic' level. Some BPI sessions (18%) were rated as 2 or above on the PI subscale of the CPPS, indicating that PI techniques were ‘somewhat characteristic’ of a minority of BPI sessions.
Research Question 3: Which techniques, considered to be part of their own conceptual model, were most or least commonly used in CBT and STPP, and were some specific techniques shared or distinct between therapists offering BPI, CBT and STPP?
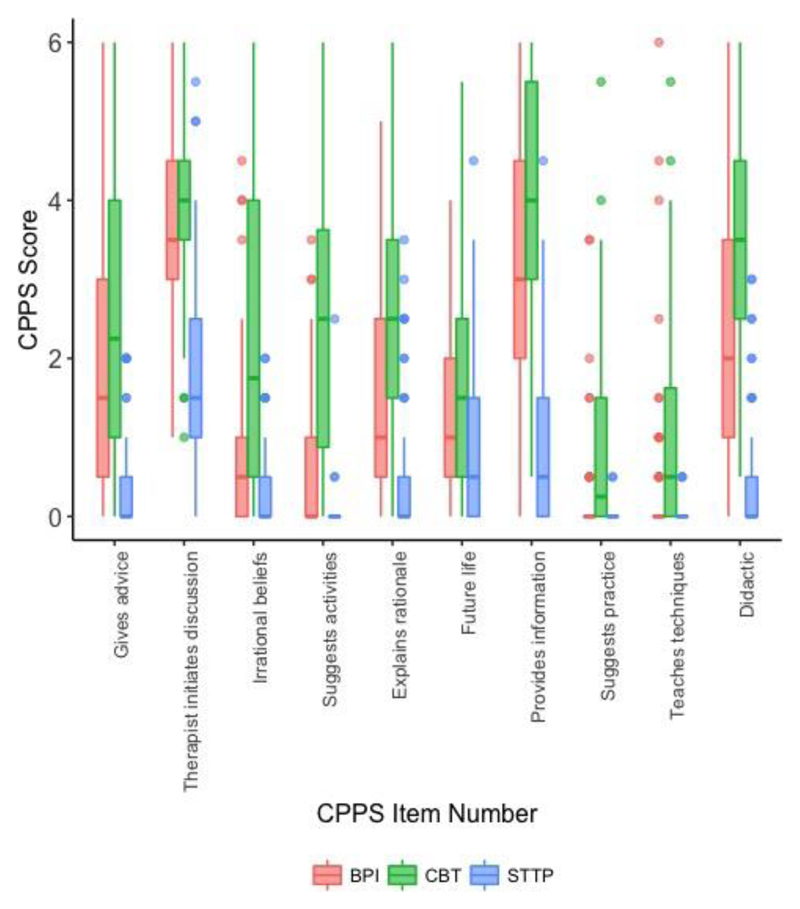
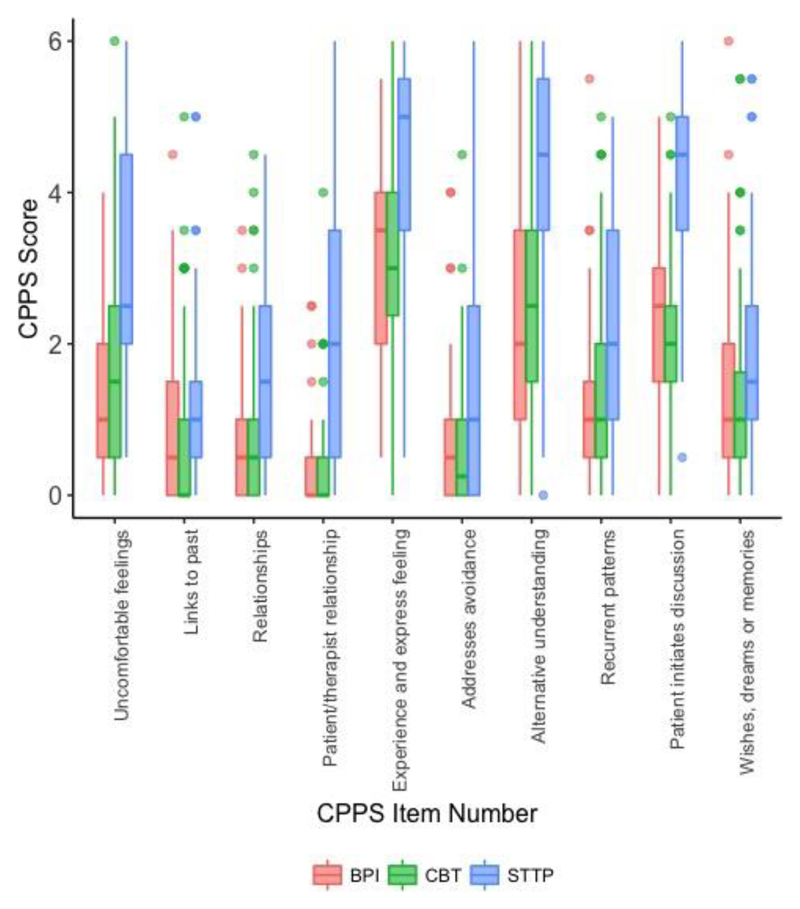
Figures 2 and 3 show the frequency distributions of individual CB and PI items for the three treatment arms, and Table 1 shows the average ratings for each item for each treatment arm. This indicates that for STPP the most commonly used techniques from the PI subscale were item 8 (“the therapist encourages the patient to experience and express feelings in the session”), item 13 (“the therapist suggests alternative ways to understand experiences or events not previously recognized by the patient”), item 16 (“the therapist allows the patient to initiate the discussion of significant issues, events, and experiences”), and item 1 (“the therapist encourages the exploration of feelings regarded by the patient as uncomfortable”). The items on the PI subscale that were used the least in the STPP sessions (i.e. had an average rating below 2) were item 4 (“the therapist links the patient’s current feelings or perceptions to experiences of the past”), item 5 (“the therapist focuses attention on similarities among the patient’s relationships repeated over time, settings, or people”), item 10 (“the therapist addresses the patient’s avoidance of important topics and shifts in mood") and item 19 (“the therapist encourages discussion of patient’s wishes, fantasies, dreams, or early childhood memories”).
Figure 2. Boxplots to show distribution of Cognitive-Behavioural items in each of the treatment arms.
Figure 3. Boxplots to show distributions of Psychodynamic-Interpersonal item in each of the treatment arms.
For CBT sessions, among the techniques on the CB subscale, the three most used techniques were item 15 (“the therapist provides the patient with information and facts about his or her current symptoms, disorder, or treatment”), item 3 (“the therapist actively initiates the topics of discussion and therapeutic activities”), and item 20 (“the therapist interacts with the patient in a teacher-like manner”). The items on the CB subscale that were used the least in the CBT sessions were item 12 (“the therapist focuses discussion on the patient’s future life situations”), item 17 (“the therapist explicitly suggests that the patient practice behavior(s) learned in therapy between sessions”) and 18 (“the therapist teaches the patient specific techniques for coping with symptoms”).
Model estimates are presented in Table 4, which compare the therapist techniques by treatment arm. Three techniques were commonly used in all three treatments (i.e. median rating ≥ 2; Figure 3). All three were items on the PI subscale: item 8 (“the therapist encourages the patient to experience and express feelings in the session”), item 13 (“the therapist suggests alternative ways to understand experiences or events not previously recognized by the patient”) and item 16 (“the therapist allows the patient to initiate the discussion of significant issues, events, and experiences”). It is not surprising that although they were used in all three therapies, they were substantially more characteristic of STPP sessions than CBT or BPI sessions.
Table 4.
Mixed effects models testing treatment arm differences for therapist techniques used, accounting for participant and therapist effects.
| PI Items | CB Items | ||||
|---|---|---|---|---|---|
| Item | Estimate (99% CI) | Item | Estimate (99% CI) | ||
| Uncomfortable feelings | Intercept | 1.25 | Gives advice | Intercept | 2.07 |
| CBT | 0.32 (-0.36, 1.04) | CBT | 0.50 (-0.20, 1.21) | ||
| STPP | 1.77 (1.11, 2.44) | STPP | -1.75 (-2.43, -1.07) | ||
| Links to past | Intercept | 0.89 | Therapist initiates discussion | Intercept | 3.60 |
| CBT | -0.19 (-0.75, 0.38) | CBT | 0.36 (-0.19, 0.92) | ||
| STPP | 0.22 (-0.31, 0.78) | STPP | -1.69 (-2.23, -1.15) | ||
| Relationships | Intercept | 0.72 | Irrational beliefs | Intercept | 0.74 |
| CBT | 0.08 (-0.47, 0.63) | CBT | 1.58 (1.00, 2.21) | ||
| STPP | 0.98 (0.36, 1.51) | STPP | -0.37 (-1.00, 0.19) | ||
| Patient/therapist relationship | Intercept | 0.30 | Suggests activities | Intercept | 0.50 |
| CBT | 0.09 (-0.61, 0.77) | CBT | 1.91 (1.37, 2.40) | ||
| STPP | 1.95 (1.30, 2.59) | STPP | -0.46 (-0.94, 0.04) | ||
| Experience and express feelings | Intercept | 3.01 | Explains rationale | Intercept | 1.52 |
| CBT | 0.15 (-0.60, 0.89) | CBT | 1.25 (0.63, 1.91) | ||
| STPP | 1.37 (0.71, 2.04) | STPP | -1.08 (-1.76, -0.41) | ||
| Addresses avoidance | Intercept | 0.66 | Future life | Intercept | 1.20 |
| CBT | -0.07 (-0.65, 0.58) | CBT | 0.22 (-0.32, 0.75) | ||
| STPP | 0.88 (0.32, 1.43) | STPP | -0.24 (-0.82, 0.29) | ||
| Alternative understanding | Intercept | 2.55 | Provides information | Intercept | 3.33 |
| CBT | 0.05 (-0.87, 0.93) | CBT | 0.85 (0.11, 1.55) | ||
| STPP | 1.84 (0.94, 2.68) | STPP | -2.41 (-3.15, -1.74) | ||
| Recurrent patterns | Intercept | 1.13 | Suggests practice | Intercept | 0.23 |
| CBT | 0.38 (-0.31, 1.07) | CBT | 0.59 (0.21, 0.98) | ||
| STPP | 1.14 (0.46, 1.74) | STPP | -0.22 (-0.61, 0.17) | ||
| Patient initiates discussion | Intercept | 2.33 | Teaches techniques | Intercept | 0.40 |
| CBT | -0.28 (-0.79, 0.26) | CBT | 0.70 (0.24, 1.12) | ||
| STPP | 1.78 (1.28, 2.35) | STPP | -0.38 (-0.81, 0.04) | ||
| Wishes, dreams or memories | Intercept | 1.26 | Didactic | Intercept | 2.62 |
| CBT | 0.01 (-0.71, 0.67) | CBT | 1.06 (0.36, 1.77) | ||
| STPP | 0.51 (-0.15, 1.16) | STPP | -2.14 (-2.84, -1.45) | ||
Random intercept variance estimates not shown; reference group: BPI.
Three further techniques from the PI subscale were also substantially more characteristics of STPP sessions than BPI or CBT sessions. These were item 1 (“the therapist encourages the exploration of feelings regarded by the patient as uncomfortable”), item 7 (“the therapist focuses discussion on the relationship between the therapist and patient”) and item 14 (“the therapist identifies recurrent patterns in patient’s actions, feelings, and experiences”).
Four techniques were more evident in CBT than in STPP or BPI sessions: item 6 (“the therapist focuses discussion on the patient’s irrational or illogical belief systems”), item 9 (“the therapist suggests specific activities or tasks”), item 11 (“the therapist explains the rationale behind his or her technique or approach to treatment”) and item 20 (“the therapist interacts with the patient in a teacher-like (didactic) manner”).
No techniques on the CPPS were specific to BPI. However, three CB techniques were commonly used in both BPI and CBT sessions. Item 3 (“the therapist actively initiates the topics of discussion and therapeutic activities”) was about equally characteristic of CBT and BPI sessions, while items 15 (“the therapist provides the patient with information and facts about his or her current symptoms, disorder, or treatment”) and 20 (“the therapist interacts with the patient in a teacher-like manner”) were significantly more characteristic of CBT sessions than BPI sessions, yet were also characteristic of BPI sessions. Overall, while there were some shared techniques between the three treatments, BPI and CBT appeared to be more similar to each other than to STPP.
Discussion
Despite decades of psychotherapy research we do not know what components of therapy are associated with the improvements they seek to bring about. This study aimed to evaluate treatment fidelity for two established psychological therapies (CBT and STPP) and treatment differentiation between these approaches and a reference treatment, BPI. In addition, the study aimed to explore which therapeutic techniques captured by the CPPS were used most and least in each of the therapies, and to identify shared and distinct techniques used by therapists working with depressed adolescents in each treatment. There was a relatively high level of fidelity to the models by therapists in each arm of the study, with 80% of STPP and 74% of CBT sessions rated as adherent to their respective models. In addition, treatment differentiation was established between all three treatment arms, as STPP and CBT sessions were significantly differentiated from each other, and from BPI.
Average scores on the CPPS were relatively low, on both the CB subscale for CBT sessions (M = 2.49) and the PI subscale for STPP sessions (M = 2.64). Thus, for items on the respective subscale for both treatments, on average, techniques were used at a ‘somewhat characteristic’ level. These ratings are lower than some previous studies using the CPPS to assess psychodynamic and cognitive-behavioural therapies for adults (e.g. Hilsenroth, Ackerman, Blagys, Baity, & Mooney, 2003; Slavin-Mulford, Hilsenroth, Weinberger, & Gold, 2011), but fits with findings from a recent study of therapeutic techniques by master therapists from the American Psychological Association PsychTHERAPY database (Pitman et al., 2017). Pitman et al. found comparable mean ratings to the current study for CBT therapists on the CB subscale (M = 2.64) and Psychodynamic-Relational therapists on the PI subscale (M = 2.83) and argued that these findings reflect that master therapists do not utilize a “more is better” approach with regards to therapeutic techniques (p. 162). This may reflect that therapists adapt their approach according to the patients’ presenting problems, characteristics and engagement; in line with the flexibility encouraged in the IMPACT treatment manuals. Therapists working with depressed adolescents may also use a lower intensity of the techniques on the CPPS, a measure that was originally developed to assess psychotherapy with adults. Much of the literature on therapy with adolescents (e.g. Briggs, 2002; Verduyn, Rogers, & Wood, 2009) emphasizes the importance of responsiveness to the developmental and therapeutic needs of the young person, over rigid adherence to any particular model of therapy.
The findings regarding the most and least used items in CBT and STPP were broadly as expected, but produced some unexpected findings. For STPP, the most characteristic features were all from the PI subscale, suggesting that the model as practiced in the UK by child and adolescent psychotherapists working with depressed adolescents is still quite faithful to a psychodynamic approach. The low use of CB items by STPP therapists indicates psychodynamic therapy in this context has incorporated few techniques typically associated with CBT. Nevertheless, it is noticeable that STPP therapists focused less on certain classical psychoanalytic features, such as exploration of dreams and fantasies, the past and repetitive patterns in relationships, than on working with the adolescent's current preoccupations and helping them to express and understand their feelings and experiences. In a time-limited psychoanalytic model of working with adolescents this suggests there may be less emphasis on exploring the past and more focus on working in the here and now, especially around expression of emotions.
The most commonly used techniques by CBT therapists were the therapist providing information about the patients’ difficulties and treatment, initiating the discussion and interacting in a teacher-like manner. Comparatively less commonly used techniques by CBT therapists were focusing on the adolescents’ future life situations, teaching coping techniques, and suggesting the adolescent practice behaviours between sessions (although this was more evident in CBT than in BPI or STPP sessions). It is interesting that these techniques were not used more, as they have been considered fundamental to the CBT approach (Beck, 1995). This may again reflect the pragmatic adaptation of therapies to the needs of adolescents, some of whom may for example experience ‘homework’ as frankly aversive. Other techniques that were specific to CBT were that the therapist focused on distorted cognitions and explained the rationale behind the treatment approach. These techniques fit with the expected collaborative stance of a CBT therapist, evidenced by instruction and information-giving by therapists whilst also explaining the rationale and allowing the patient to initiate discussion of topics. However, this contradicts, to some extent, the predominance of a didactic approach in the CBT sessions, which may reflect the more educative components of CBT, or could result from depressed adolescents needing more active therapist instruction in response to the lack of motivation and self-efficacy that can be characteristic of depression.
It is interesting that a substantial minority of CBT sessions utilized techniques from the PI sub-scale, such as encouraging expression and experience of affect, suggesting alternative ways of understanding experiences, and allowing the patient to initiate discussion. Despite being considered PI techniques on the CPPS, these would be considered legitimate CBT techniques within the IMPACT CBT manual and in CBT practice generally with young people in the UK.
There were no techniques on the CPPS specific to BPI, but this was unsurprising as the CPPS was not designed to capture unique features of BPI. Given the promising outcomes for BPI in the main trial, future studies should examine what techniques are uniquely characteristic of BPI, using measures developed specifically for this approach. BPI included slightly less of an emphasis on giving explicit psycho-education and advice than CBT, with a greater divergence noted for item number 18, teaches the patient specific techniques for coping with symptoms. This is of interest because psychoeducation is considered one of the key features of the BPI approach. However, the BPI therapists were tasked with avoiding techniques core to CBT or STPP so to keep ‘clear blue water’ between the three interventions. This may explain the relatively lower scores for CPPS items examining psycho-education.
This study provides a glimpse into shared components across different theoretical orientations in the treatment of adolescent depression. There were three techniques characteristic of BPI, CBT and STPP. These were that (i) the therapist encourages the patient to experience and express feelings, (ii) suggests alternative ways to understand experiences or events not previously recognized by the patient, and (iii) allows the patient to initiate the discussion of significant issues, events and experiences. Interestingly, in Pitman et al's (2017) study, they found that third-wave CBT therapists used significantly more PI techniques than 'classical' CBT therapists and incorporated areas outside of the classical CBT model, focusing more on the patients’ emotional expression and exploration compared with traditional CBT therapists. Similarly, allowing patients to explore and understand their difficulties appeared to be a core technique shared across the three arms in the present study. While all three shared items belonged to the PI subscale of the CPPS, these items would not be considered as a violation of the BPI or CBT approaches in the IMPACT study. Meta-analytic studies of adolescent psychotherapies highlight the importance of care that is founded on interpersonal effectiveness, warmth and trust leading to a therapy that is a collaborative experience between the therapist and patient (Weisz, Jensen-Doss, & Hawley, 2006). It is perhaps unsurprising that basic clinical engagement items such as encouragement of emotional exploration, and a general helping stance were shared between the interventions. These are likely to be primary ingredients of building a therapeutic alliance with depressed adolescents, and should no longer be considered exclusive to a psychodynamic model. This may indicate that a focus on encouraging emotional expression, which may classically have been considered characteristic of psychodynamic therapies, is now a generic feature of a range of therapies. The IMPACT trial found equivalence of outcomes between the three treatments (Goodyer et al., 2017), and it is possible that these shared techniques may reflect some of the important helping aspects of therapy. We cannot say this from the current study, but will be an intriguing line for future enquiry.
BPI and CBT were found to be more similar to each other than to STPP, as there were shared items between BPI and CBT that were not shared with STPP. These were all items on the CB subscale, which related to the therapist actively initiating the topics of discussion and activities, provides the patient with information and facts about their symptoms, disorder or treatment, and interacts with the patient in a didactic manner. These items essentially represent a more active, directive stance, demonstrating overlap between BPI and CBT, emphasising activation and problem solving, using a more directive, active approach to treatment.
Strengths and limitations
The strengths of this study are it provides an insight into the techniques typically used by therapists working with depressed adolescents, an area which little is known about. However, we note several limitations. As the sessions were randomly sampled, the selected sessions were from therapies that had longer duration than the average treatment, so the techniques identified in this study may be more typical of therapies where the young person had a longer engagement in treatment. This study used the CPPS, which was not developed from the treatment manuals used in the IMPACT trial, and had not previously been validated with an adolescent population; rather, the CPPS represents a prototype of CBT and psychodynamic treatment based on an empirical review of studies of therapy with adults, mostly in North America. There may be differences in how these therapies have developed in the UK, and how they may have been adapted to this developmental context. Although we were concerned that the use of audio, rather than video-tapes, might limit our capacity to rate elements of the therapy (such as affect focus), we did not find this to be the case. However, by focusing only on techniques captured by this measure, it remains unknown whether there is a further set of components of care not articulated by the CPPS, specific to this context and that may contribute to the efficacy of the treatments. The CPPS also captures only the adherence aspect of treatment fidelity, which does not allow for a consideration of how well or how effectively (that is, how competently) the techniques were used.
Conclusion
This study demonstrates that therapists offering CBT or STPP to depressed adolescents, as part of an RCT in the UK, were able to deliver the respective therapies with relatively good levels of fidelity to the general features of cognitive-behavioural and psychodynamic therapy respectively. The techniques used by the CBT and STPP therapists could be differentiated from each other, and from a reference treatment, BPI. Closer inspection at an item level identified some variation in which techniques from their own therapeutic approach were more or less commonly used by CBT and STPP therapists, and identified shared techniques across the three treatment arms. Some techniques, such as helping adolescents to express their feelings, may have traditionally been associated with a psychodynamic approach, are now a common element of a range of therapies with depressed adolescents. Further work is needed regarding the validation of the CPPS measure in the context of psychotherapy for young people, and outside of North America. It will also be important to complement studies of this sort with ones that focus on the client's own experiences of therapy. As the CPPS measures only the use of techniques, it will be important for future studies to focus on the quality of therapist actions (i.e. competence), as well as to explore possible associations between shared or unique treatment techniques and outcomes. This could help to throw light on the primary outcomes of the IMPACT study itself (i.e. no significant differences in outcome between the different treatment arms), in particular whether more effective psychological therapies are dependent on the use of shared features, or whether there are unique pathways to change in different modalities of psychological therapy.
Acknowledgements
The study was funded by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme (project number 06/05/01). Dr Loades is funded by the National Institute for Health Research (Doctoral Research Fellowship, DRF-2016-09-021). This report is independent research. The views expressed in this publication are those of the authors(s) and not necessarily those of the NHS, The National Institute for Health Research or the Department of Health.
Footnotes
This paper is not the copy of record and may not exactly replicate the final, authoritative version of the article. Please do not copy or cite without authors permission.
References
- Amole MC, Cyranowski JM, Conklin LR, Markowitz JC, Martin SE, Swartz HA. Therapist Use of Specific and Nonspecific Strategies Across Two Affect-Focused Psychotherapies for Depression: Role of Adherence Monitoring. Journal of Psychotherapy Integration. 2017;27(3):381–394. doi: 10.1037/int0000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JS. Cognitive therapy: Basics and beyond. New York: Guilford Press; 1995. [Google Scholar]
- Bhar SS, Beck AT. Treatment Integrity of Studies That Compare Short-Term Psychodynamic Psychotherapy With Cognitive-Behavior Therapy. Clinical Psychology: Science and Practice. 2009;16(3):370–378. doi: 10.1111/j.1468-2850.2009.01176.x. [DOI] [Google Scholar]
- Blagys MD, Hilsenroth MJ. Distinctive Features of Short-Term Psychodynamic-Interpersonal Psychotherapy: A Review of the Comparative Psychotherapy Process Literature. Clinical Psychology: Science and Practice. 2000;7(2):167–188. doi: 10.1093/clipsy/7.2.167. [DOI] [Google Scholar]
- Blagys MD, Hilsenroth MJ. Distinctive activities of cognitive–behavioral therapy: A review of the comparative psychotherapy process literature. Clinical Psychology Review. 2002;22(5):671–706. doi: 10.1016/S0272-7358(01)00117-9. [DOI] [PubMed] [Google Scholar]
- Briggs S. Working with adolescents: A contemporary psychodynamic approach. Basingstoke, UK: Palgrave; 2002. [Google Scholar]
- Castonguay LG. “Common factors” and “nonspecific variables”: Clarification of the two concepts and recommendations for research. Journal of Psychotherapy Integration. 1993;3(3):267–286. doi: 10.1037/h0101171. [DOI] [Google Scholar]
- Castonguay LG, Holtforth MG. Change in psychotherapy: A plea for no more “nonspecific” and false dichotomies. Clinical Psychology: Science and Practice. 2005;12(2):198–201. doi: 10.1093/clipsy/bpi026. [DOI] [Google Scholar]
- Cregeen S, Hughes C, Midgley N, Rhode M, Rustin M. Short-term psychoanalytic psychotherapy for adolescents with depression: A treatment manual. Karnac Books; 2016. [Google Scholar]
- Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. John Wiley & Sons, Inc.; 2004. The Measurement of Interrater Agreement; pp. 598–626. [DOI] [Google Scholar]
- Goldman RE, Hilsenroth MJ, Owen JJ, Gold JR. Psychotherapy integration and alliance: Use of cognitive-behavioral techniques within a shortterm psychodynamic treatment model. Journal of Psychotherapy Integration. 2013;23(4):373–385. doi: 10.1037/a0034363. [DOI] [Google Scholar]
- Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al. Harrington R. Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: randomised controlled trial. BMJ. 2007;335(7611):142. doi: 10.1136/bmj.39224.494340.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer IM, Reynolds S, Barrett B, Byford S, Dubicka B, Hill J, et al. Fonagy P. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiatry. 2017;4(2):109–119. doi: 10.1016/S2215-0366(16)30378-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer IM, Reynolds S, Barrett B, Byford S, Dubicka B, Hill J, et al. Fonagy P. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled trial. Health Technology Assessment. 2017;21(12) doi: 10.3310/hta21120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer IM, Tsancheva S, Byford S, Dubicka B, Hill J, Kelvin R, et al. Fonagy P. Improving mood with psychoanalytic and cognitive therapies (IMPACT): a pragmatic effectiveness superiority trial to investigate whether specialised psychological treatment reduces the risk for relapse in adolescents with moderate to severe unipolar depression. Trials. 2011;12(1):175. doi: 10.1186/1745-6215-12-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilsenroth MJ, Ackerman SJ, Blagys MD, Baity MR, Mooney MA. Short-term psychodynamic psychotherapy for depression: An examination of statistical, clinically significant, and technique-specific change. The Journal of Nervous and Mental Disease. 2003;191(6):349–357. doi: 10.1097/01.NMD.0000071582.11781.67. [DOI] [PubMed] [Google Scholar]
- Hilsenroth MJ, Defife JA, Blake MM, Cromer TD. The effects of borderline pathology on short-term psychodynamic psychotherapy for depression. Psychotherapy Research. 2007;17(2):172–184. doi: 10.1080/10503300600786748. [DOI] [Google Scholar]
- IMPACT Study CBT Sub-Group. Cognitive behaviour therapy for depression in young people: Manual for therapists. 2010 Retrieved from http://dev.psychiatry.cam.ac.uk/projects.
- Katz M, Hilsenroth MJ. Psychodynamic technique early in treatment related to outcome for depressed patients. 2017:1–11. doi: 10.1002/cpp.2167. [DOI] [PubMed] [Google Scholar]
- Kelvin R, Dubicka B, Wilkinson P, Goodyer IM. Brief Psychosocial Intervention (BPI): A specialist clinical care treatment manual for CAMHS use. 2010 Retrieved from http://dev.psychiatry.cam.ac.uk/projects.
- Kelvin R, Wilkinson P, Goodyer IM. Treating Child and Adolescent Depression Philadelphia. Philadelphia, PA: Lippincott, Williams and Wilkins; 2009. Managing Acute Depressive Episodes: Putting it Together in Practice; pp. 162–73. [Google Scholar]
- Leichsenring F, Salzer S, Hilsenroth MJ, Leibing E, Leweke F, Rabung S. Treatment integrity: An unresolved issue in psychotherapy research. Current Psychiatry Reviews. 2011 doi: 10.2174/157340011797928259. [DOI] [Google Scholar]
- Marcus DK, O’Connell D, Norris AL, Sawaqdeh A. Is the Dodo bird endangered in the 21st century? A meta-analysis of treatment comparison studies. Clinical Psychology Review. 2014;34(7):519–530. doi: 10.1016/j.cpr.2014.08.001. [DOI] [PubMed] [Google Scholar]
- Ogrodniczuk JS, Piper WE. Measuring therapist technique in psychodynamic psychotherapies: development and use of a new scale. Journal of Psychotherapy Practice and Research. 1999;8(2):142–154. [PMC free article] [PubMed] [Google Scholar]
- Oxford Centre for Evidence-Based Medicine. Levels of evidence. 2009 Retrieved August 21, 2017, from http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- Perepletchikova F, Kazdin AE. Treatment integrity and therapeutic change: Issues and research recommendations. Clinical Psychology: Science and Practice. 2005;12(4):365–383. doi: 10.1093/clipsy/bpi045. [DOI] [Google Scholar]
- Perepletchikova F, Treat TA, Kazdin AE. Treatment integrity in psychotherapy research: analysis of the studies and examination of the associated factors. Journal of Consulting and Clinical Psychology. 2007;75(6):829–841. doi: 10.1037/0022-006X.75.6.829. [DOI] [PubMed] [Google Scholar]
- Pitman SR, Hilsenroth MJ, Goldman RE, Levy SR, Siegel DF, Miller R. Therapeutic technique of APA master therapists: Areas of difference and integration across theoretical orientations. Professional Psychology: Research and Practice. 2017;48(3):156–166. doi: 10.1037/pro0000127. [DOI] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2016. [Google Scholar]
- Sharpless BA, Barber JP. A conceptual and empirical review of the meaning, measurement, development, and teaching of intervention competence in clinical psychology. Clinical Psychology Review. 2009;29(1):47–56. doi: 10.1016/j.cpr.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavin-Mulford J, Hilsenroth M, Weinberger J, Gold J. Therapeutic interventions related to outcome in psychodynamic psychotherapy for anxiety disorder patients. The Journal of Nervous and Mental Disease. 2011;199(4):214–221. doi: 10.1097/NMD.0b013e3182125d60. [DOI] [PubMed] [Google Scholar]
- Verduyn C, Rogers J, Wood A. Depression: Cognitive behaviour therapy with children and young people. London: Routledge; 2009. [Google Scholar]
- Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14(3):270–277. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Barber JP. Therapist adherence/competence and treatment outcome: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):200–211. doi: 10.1037/a0018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Jensen-Doss A, Hawley KM. Evidence-based youth psychotherapies versus usual clinical care: a meta-analysis of direct comparisons. The American Psychologist. 2006;61(7):671–689. doi: 10.1037/0003-066X.61.7.671. [DOI] [PubMed] [Google Scholar]
- Westen D, Novotny CM, Thompson-brenner H. The Empirical Status of Empirically Supported Psychotherapies: Assumptions, Findings, and Reporting in Controlled Clinical Trials. Psychiatric Bulletin. 2004;130(4):631–663. doi: 10.1037/0033-2909.130.4.631. [DOI] [PubMed] [Google Scholar]
- Wickham H. ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag; New York: 2009. [Google Scholar]