Abstract
As improved treatments for congenital heart disease (CHD) have increased life expectancy, neurodevelopmental impairments have been observed in many survivors. These impairments include developmental delays, difficulty in school, and challenges living independently. Understanding the causes of these impairments and minimizing their impact are important goals to allow survivors to have the best possible quality of life.
Keywords: brain, congenital heart defects, follow-up studies
How does congenital heart disease affect the brain?
CHD may affect the brain in several ways. First, the heart pumps blood that carries nutrients and oxygen to the brain to allow it to grow and develop. Some types of CHD may reduce the amount of blood reaching the brain and/or the oxygen content of the blood. Starting in the fetal period, reduced blood flow and oxygen content may impede brain maturation. Indeed, full-term babies with some types of heart defects have brain maturity that is about one month delayed, i.e., similar to those of premature babies born at 36 weeks.1
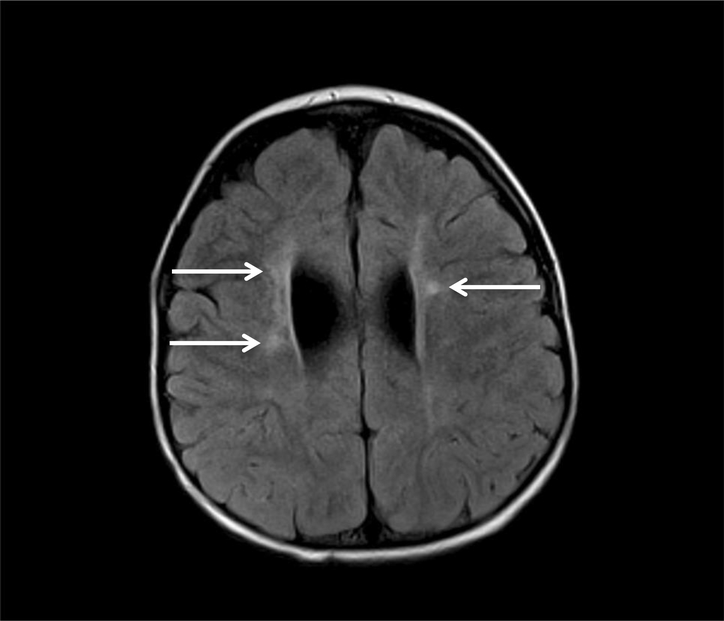
Brain injury may also occur in CHD. Brain immaturity increases the risk of brain injury with stresses such as labor and delivery, blood pressure instability, or infection. White matter, a tissue connecting different regions of the brain, is particularly vulnerable to injury. White matter injury can impair motor and cognitive systems critical for development and learning (see Figure). Children with CHD may also experience acute events, such as cardiac arrest. Depending on the severity, cardiac arrest may cause widespread injury or more limited injury to brain structures that are most sensitive to oxygen and nutrient deprivation. Some types of CHD allow blood clots to form and travel to the brain, blocking blood vessels and causing stroke. Cardiac operations and cardiac catheterizations can also be complicated by stroke. Although children’s brains have a remarkable capacity for recovery, these injuries may impact communication between different brain systems, such as the visual and motor systems, or directly damage regions of brain important for specific tasks.
Figure.
Brain MRI showing white matter injury, the white patchy areas next to the ventricles (two dark oblong areas that are fluid-filled compartments of the brain).
Finally, genetic factors contribute. In some children, CHD is part of a genetic syndrome. The genes causing abnormal heart formation may also cause abnormal brain formation. In other cases, a named genetic syndrome may not be identified, but subtle changes to the child’s genes may impact both heart and brain. Together, reduced blood flow and/or oxygenation, specific injuries, and genetic factors all increase the risk of brain abnormalities in children with CHD.2
What neurodevelopmental issues are children with CHD at risk for?
CHD affects neurodevelopment across the lifespan. In infants, developmental delays may occur. These range from hypotonia (low muscle tone) in infancy to persistent delays affecting many aspects of development, such as language, social skills, and feeding. Some children reach early milestones on time, but school demands unmask impairments that were not apparent at younger ages. For example, difficulty with calculation may be undetected in infancy but become obvious in second grade. Higher-level organizational issues may emerge in high school when students balance multiple courses.
Aspects of neurodevelopment most commonly impacted in school-age children with CHD include organization, visuospatial skills, memory, mathematics, and language.3 Some children struggle with social skills, anxiety, or depression. Attention deficit hyperactivity disorder (ADHD) also occurs, often accompanied by other learning difficulties.
The spectrum of neurodevelopmental impairment is wide. Some children have minimal to no impairment, while others are severely affected. In general, children with milder forms of heart disease, such as isolated ventricular septal defects, have fewer neurodevelopmental sequelae than those with complex lesions, such as hypoplastic left heart syndrome, but medical, environmental, and genetic factors all play a role.
How are neurodevelopmental disabilities diagnosed?
Primary care physicians assess neurodevelopment at scheduled visits but do not usually perform diagnostic testing. When a parent has concerns about a child’s development or the initial assessment reveals delays, a developmental specialist should perform a formal evaluation. In younger children, the evaluation will include gross motor, fine motor, language, social, and daily living skills. In older children, it will emphasize skills important for school and independent living, such as attention, organization, social interaction, coordination, and self-care. The American Heart Association has described categories of children at high risk for neurodevelopmental impairment (see Table) and recommends these children be formally evaluated with periodic re-evaluation at 12–24 months, 3–5 years, and 11–12 years, even if no concerns arise on routine screening.2
Table.
Children at Highest Risk for Neurodevelopmental Impairment*
| 1. | Neonates or infants requiring open heart surgery |
| 2. | Children with other cyanotic (“blue”) heart lesions not requiring infant heart surgery |
| 3. | Congenital heart disease combined with any of the following: |
| a. Prematurity less than 37 weeks | |
| b. Developmental delay | |
| c. Suspected genetic abnormality or syndrome associated with developmental delay | |
| d. History of mechanical support (extracorporeal membranous oxygenation or ventricular assist device) | |
| e. Heart transplantation | |
| f. Cardiopulmonary resuscitation | |
| g. Hospital stay longer than two weeks after surgery | |
| h. Perioperative seizures | |
| i. Abnormal findings on brain imaging or small head circumference | |
| 4. | Other conditions determined by medical home provider |
Adapted from Marino et al., 20122
What treatment is available?
The treatments for neurodevelopmental disability are tailored to the specific situation. Early Intervention provides services to children younger than three years of age with developmental delays or a high risk of delays, such as those who have had heart surgery. It is a federally mandated program, available in all states, and typically includes developmental educators as well as physical, occupational, and speech therapists. For older children, Individualized Education Programs and academic modifications can address learning difficulties. A psychologist or other mental health professional can help children suffering from anxiety or depression. Finally, medications may be part of a multifaceted treatment plan for conditions such as ADHD or mood disorders.
As a parent, you will often be the first to notice neurodevelopmental issues. If you have concerns, notify your child’s physicians right away so they can make an appropriate referral. Even if your child seems to be doing well, if he/she meets the high-risk criteria, enroll your child in Early Intervention and obtain the recommended periodic evaluations. By doing so, you will help ensure skilled surveillance and prompt treatment so that your child can achieve the best possible outcome.
Acknowledgments
Funding
This work was supported by the K12 NS079414 from the National Institute of Neurological Disorders and Stroke and the Kenrose Kitchen Foundation.
Footnotes
Resources
Conflict of Interest Disclosures
None.
Contributor Information
Caitlin K. Rollins, Departments of Neurology, Boston Children’s Hospital; Departments of Neurology, Harvard Medical School
Jane W. Newburger, Departments of Cardiology, Boston Children’s Hospital; Departments of Pediatrics, Harvard Medical School
References
- 1.Miller SP, McQuillen PS, Hamrick S, Xu D, Glidden DV, Charlton N, Karl T, Azakie A, Ferriero DM, Barkovich AJ, Vigneron DB. Abnormal brain development in newborns with congenital heart disease. N Engl J Med. 2007;357:1928–1938. [DOI] [PubMed] [Google Scholar]
- 2.Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, Mussatto KA, Uzark K, Goldberg CS, Johnson WH Jr., Li J, Smith SE, Bellinger DC, Mahle WT; on behalf of the American Heart Association Congenital Heart Defects Committee of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, and Stroke Council. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126:1143–1172. [DOI] [PubMed] [Google Scholar]
- 3.Bellinger DC, Wypij D, Rivkin MJ, DeMaso DR, Robertson RL Jr., Dunbar-Masterson C, Rappaport LA, Wernovsky G, Jonas RA, Newburger JW. Adolescents with d-transposition of the great arteries corrected with the arterial switch procedure: neuropsychological assessment and structural brain imaging. Circulation. 2011;124:1361–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]