Abstract
Objective:
To examine prospective relations of perceived racial discrimination at ages 16–18 with body mass index (BMI) at ages 19–21 and insulin resistance (IR) at ages 25 and 27 among Black youth in the rural South, and to determine whether BMI connected discrimination to IR as a mediator.
Method:
Participants were 315 African American adolescents in rural counties in Georgia who provided data on their perceptions of discrimination during adolescence. BMI was measured during a yearly home visit, and a certified phlebotomist drew a fasting blood sample from which IR was measured.
Results:
The data analysis, with all confounding variables controlled, revealed that, over time, (a) discrimination was associated positively with both BMI and IR; (b) BMI was associated positively with IR; and (c) BMI acted as a mediator connecting discrimination with IR.
Conclusions:
The findings are consistent with the hypothesis that exposure to discrimination presages IR through its effects on BMI.
Keywords: African Americans, body mass index, insulin resistance, racism, rural population
Compared with members of other racial groups, African Americans experience more aging-related diseases earlier in life, at greater severity, and with more serious consequences (Schuster et al., 2012). According to life-course and developmental perspectives, this disproportionate disease risk can be traced to systematic disadvantages and social inequities starting at conception and continuing throughout childhood, adolescence, and young adulthood (Krieger, 2014). The health-risk inequities that African Americans experience likely arise from more than class disadvantage alone. Psychological stressors that disproportionately affect African Americans have been suggested as a mechanism that weathers physiological systems and increases vulnerability to poor health (Geronimus, Hicken, Keene, & Bound, 2006). Racial discrimination presents daily challenges in the lives of African American youth and their families; recent reports indicate that racial discrimination remains a persistent, if not escalating, experience for African Americans (Williams & Mohammed, 2013). Discriminatory incidents are demeaning and induce stress, frustration, depression, and anxiety in adults (Pascoe & Smart Richman, 2009) and in adolescents (Priest et al., 2013).
An association between racial discrimination and outcomes relevant to physical health is also plausible. Research conducted primarily with adults has demonstrated that discrimination is associated with a range of health-relevant physiological processes, including dysregulated patterns of cortisol release and biomarkers of low-grade inflammation (Lewis, Cogburn, & Williams, 2015; Paradies et al., 2015). Mirroring these patterns, recent research with young African American populations indicated that experiences with racial discrimination were associated with flatter diurnal cortisol slopes, indicative of unhealthier outcomes, for young adults (Zeiders, Hoyt, & Adam, 2014), heightened levels of pro-inflammatory cytokines in young adults (Brody, Yu, Miller, & Chen, 2015), and of C-reactive protein in adolescents (Goosby, Malone, Richardson, Cheadle, & Williams, 2015). Together, these studies support the importance of understanding the health consequences of exposure to racial discrimination during adolescence, a developmental stage in which African American youth become keenly aware of targeted social rejection and their treatment by others (Stevenson, 2004).
Current estimates suggest that nearly 40% of Black adults living in the southeastern United States have diabetes (Centers for Disease Control and Prevention, 2014). This alarming prevalence rate is among the highest in the nation (Menke, Casagrande, Geiss, & Cowie, 2015). Many approaches can be taken in dealing with this situation, but health psychologists, pediatricians, and public health scientists agree that understanding the contributions of exposure to race-related stressors during childhood and adolescence is important (Shonkoff, Boyce, & McEwen, 2009). In response to this need, the first purpose of this study is to determine whether exposure to high levels of racial discrimination across adolescence will predict elevated rates of insulin resistance (IR) during young adulthood. In IR, muscle, fat, and liver cells do not respond properly to insulin, reducing the absorption of glucose into cells. As a result, excess glucose builds up in the bloodstream, which can lead to diabetes. The notion examined here is that recurring exposure to interpersonal discrimination leads to persistent activation of neuroendocrine and inflammatory response systems. The end products of these systems (cortisol, epinephrine, norepinephrine, cytokines, and chemokines) all contribute to the emergence of IR (Björntorp & Rosmond, 1999; Lackey & Olefsky, 2016; McEwen, 1998).
In addition to triggering sustained activation of stress responses, the experience of interpersonal discrimination may also place young people at risk for elevated body mass index (BMI), an indicator that controls for height when measuring weight and is a risk factor for IR. It has been hypothesized that frequent encounters with interpersonal discrimination are associated with overconsumption of high-calorie foods to alleviate the resulting symptoms of stress (J. S. Jackson, Knight, & Rafferty, 2010; Pascoe & Smart Richman, 2009). Such a stress-coping dynamic would be reflected in a positive association between elevated exposure to interpersonal discrimination and BMI. Surprisingly few studies have examined this association among African American adolescents and young adults. One study found a cross-sectional relationship between exposure to racial discrimination and BMI (Nelson et al., 2018). Results of studies examining this relationship among African American adults have been inconsistent. Some studies found a positive association (Stepanikova et al., 2017; Thorpe, Parker, Cobb, Dillard, & Bowie, 2017), some found no association (Hunte & Williams, 2009; Johnson, Risica, Gans, Kirtania, & Kumanyika, 2012; Shelton et al., 2009), and others found an association that is stronger among women than among men (Cunningham et al., 2013). Although the interpretation of these findings is complicated by differences in the ages of the samples and recruitment variations, in all of the studies participants are asked about their exposure to racial discrimination at only one point in time. This limits understanding about the ways in which differences in exposures to racial discrimination across time relate to BMI. To overcome this limitation, in this study we followed a cohort of African American adolescents who were within two years of each other in age and assessed their exposure to interpersonal discrimination from ages 16 to 18.
This study also addressed a methodological issue. Prior research has shown that African American youth have qualitatively different experiences of racial discrimination across adolescence. Most youth encounter low but increasing exposures to racial discrimination, whereas others experience high exposures that remain stable over time (Brody et al., 2006; Greene, Way, & Pahl, 2006; Simons, Chen, Stewart, & Brody, 2003). Among adolescents who experience exclusively high exposures to racial discrimination, prospective associations with psychosocial and health-related indicators emerge (Brody, Yu, & Beach, 2016). Thus, perceived discrimination was hypothesized to follow qualitatively different trajectories across ages 16 to 18 years. This study was designed to test the hypotheses that exposure to high levels of discrimination across ages 16 to 18 years would be associated with BMI across ages 19 to 21 years, and that BMI would serve as a mediator connecting racial discrimination during adolescence to IR during young adulthood at ages 25 and 27 years.
Methods
Sample
Data for this study were drawn from the Strong African American Healthy Adult Project (SHAPE; Brody et al., 2013). Starting in 2001, 667 African American children in fifth grade (mean age = 11.2 years; range 11 to 13 years) and their primary caregivers were enrolled in SHAPE. The families resided in nine rural counties in Georgia, where poverty rates are among the highest in the nation. In 2009–2010, when the youth had reached ages 19 and 20, a subgroup was randomly selected for a substudy of stress hormones and blood pressure. In 2015–2016 and 2017, when the youth’s mean ages were 25 and 27 years, blood draws were obtained from 391 participants at the age 25 assessment and 388 participants at age 27. Overnight fasting blood glucose and insulin samples were assayed from the blood samples. For the current study, the analytic sample consists of the 337 participants for whom complete data were available for all study variables across ages 16 to 27. Compared with the original cohort, the analytic sample included a higher percentage of female participants (61.1% vs. 52.8%); otherwise, the samples were demographically similar. The University of Georgia’s Institutional Review Board approved the protocol and, at all waves of data collection, written informed consent was obtained from caregivers of youth under age 18 and from youth 18 and older. Minor youth assented in writing.
Data Collection Procedures
All data were collected in participants’ homes using a standardized protocol. A field researcher who was also a certified phlebotomist went to each participant’s home to collect self-report data and to draw a blood sample for the assessment of glucose and insulin.
Measures
Racial discrimination was assessed at ages 16, 17, and 18. BMI was measured at ages 19, 20, and 21. Fasting blood glucose and insulin were assessed at ages 25 and 27. The covariates gender, cumulative SES risk, life stress, and depressive symptoms were assessed at ages 16 to 18, overlapping the assessment of racial discrimination. The lifestyle covariates of drug use and exercise were assessed at ages 19 to 21, concurrently with the measurement of BMI. These variables were controlled in every analysis.
Racial discrimination.
At ages 16 to 18 years, youth responded to nine items from the Schedule of Racist Events (Landrine & Klonoff, 1996), which was designed to be developmentally appropriate for Black adolescents (Brody et al., 2006). This scale has been used extensively in public health and biomedical research and has demonstrated predictive validity for both psychosocial and physical health indicators (Lewis et al., 2015). The scale was used to assess the frequency during the past year with which the respondent experienced specific discriminatory events. These events included racially based slurs and insults, disrespectful treatment from community members, physical threats, and false accusations from business employees or law enforcement officials. Responses to items were summed at each wave across ages 16 to 18 years. Cronbach’s alphas ranged from .87 to .89 across assessments.
Body mass index.
Each participant’s weight and height at ages 19 to 21 years were used to calculate BMI (weight in kilograms divided by the square of height in meters). Researchers measured weight using a standard home scale and height using a tape measure. BMI was averaged across ages 19 to 21 years.
Young adult blood glucose, insulin, and insulin resistance.
At the age 25 and 27 assessments, a phlebotomist visited each participant’s home in the morning to draw an overnight fasting blood sample. Blood was drawn into serum separator tubes (Becton, Dickinson and Company, Franklin Lakes, NJ, USA). Specimens were centrifuged on site at 1500 × g for 20 minutes. The serum was harvested, divided into aliquots, and immediately frozen on dry ice. Upon arrival at the lab, it was placed in storage at −80 C until the end of the project. At that point, serum glucose was measured photometrically using a UV test on a Roche/Hitachi Cobas c502 instrument. This assay has a dynamic range of 2–750 mg/dL and intra-assay coefficient of variation of 0.7%. Serum insulin was assayed in duplicate using a multiplex, electrochemiluminescent immunoassay (Human Leptin/Insulin Kit K15164C; MesoScale Discovery) on a SECTOR Imager 2400A (MesoScale Discovery). This assay has an 8-point standard curve, with a lower limit of detection of 25 pg/ml for insulin. The intra-assay coefficient of variation for duplicate pairs averaged 3.8%. The indicator of IR was estimated according to the original homeostasis assessment model (HOMA; Matthews et al., 1985), where IR was calculated as [fasting glucose (mmol/L) × fasting insulin (mIU/L)] / 22.5. IR levels were log-transformed because of the skewed distribution and were averaged across ages 25 and 27 (r = .57, p < .001).
Confounder variables.
Family SES-related disadvantage was measured as the sum of six indicators (0 if absent, 1 if present; see Brody et al., 2013): current family poverty, primary caregiver’s noncompletion of high school or an equivalent, primary caregiver current unemployment, single-parent family structure, current receipt of Temporary Assistance for Needy Families, and income rated by the caregiver as inadequate to meet all needs. The average number of indicators across ages 16 to 18 constituted the measure of SES-related disadvantage. Personal life stress was assessed with a 12-item checklist (Brody, Chen, & Kogan, 2010) on which youth indicated whether stressors, such as experiencing a serious injury or illness, acute economic stress, or parental divorce, had occurred during the previous 6 months. The number of endorsed items was tallied at each wave, and these sums were averaged across ages 17 and 18. Depressive symptoms were assessed with the Children’s Depression Inventory (Kovacs, 1979); alphas ranged from .84 to .86. Depression scores at ages 16 and 17 were averaged. Drug use was assessed at ages 19, 20, and 21 using items from the Monitoring the Future study (Johnston, O’Malley, Bachman, & Schulenberg, 2007). The items assessed past-month cigarette, alcohol, and marijuana use, as well as binge drinking. Responses to these items were summed to form a drug use composite. Exercise was measured with a single item indicating the number of days during the past week the participant was physically active for 60 minutes. The drug use and exercise items were averaged separately across ages 19 to 21.
Statistical Approach
Black youth living in both rural and urban areas experience heterogeneity in their exposure to racial discrimination across adolescence. Thus, the first data analytic step was to identify youth who experienced distinct trajectories of exposure to racial discrimination across ages 16 to 18 years. Latent growth curve analysis and latent growth mixture modeling were used to do this. First, latent growth curve models (LGCM) were executed to characterize the overall experience of racial discrimination across ages 16, 17, and 18. Linear growth models were fit with two individual growth parameters: an intercept parameter representing the level of racial discrimination at the starting point (age 16) and a linear slope parameter representing the rate at which racial discrimination changed across the three waves of data collection. Second, latent growth mixture models (LGMM) were executed to identify distinct groups characterized by different levels of exposure to racial discrimination. LGMM determines whether the population under study is composed of distinct classes of individuals based on variation in intercepts or slopes. Model fits were compared for one-, two-, and three-class LGMM, assessing relative fit with conventional indices, including the Bayesian information criterion (BIC) and entropy values. Lower BIC scores indicate better fit, whereas higher entropy scores reflect greater accuracy in classification. Optimal models were chosen on the basis of goodness of fit and parsimony.
After distinct classes of exposure to racial discrimination were identified, univariate analyses of covariance (ANCOVA) were conducted to determine whether members of the racial discrimination trajectory groups differed significantly on their BMI at ages 19 to 21 and IR levels at ages 25 and 27. Hierarchical linear regression analyses were then conducted to determine whether BMI would mediate the association of racial discrimination with IR. For all models, covariates were entered first, followed by racial discrimination trajectory group and BMI. Indirect (or mediation) effects were tested by calculating bias-corrected 95% CIs using bootstrapping with 1000 resamples via the Process procedure for SPSS (Hayes, 2013).
Results
The LGCM analysis revealed that racial discrimination increased over time (mean slope = 0.784, p < .001). The analysis also revealed significant variation in the intercept (variance = 10.390, p < .001) and the slope (variance = 2.171, p < .001). The results of the LGMM analyses revealed that the three-class model had the lower BIC statistics (6904.85 for three-class vs. 6921.34 for two-class); however, the entropy values indicated that the two-class model fit the data better (0.77 for three-class vs. 0.81 for two-class). The two-class model, therefore, was chosen for follow-up hypothesis testing. The majority of participants (77.7%) were assigned to the low-and-increasing class, which had a low intercept at age 16 (mean intercept = 2.169, 95% CI [1.804, 2.534], p < .001) with increasing exposure to discrimination from ages 16 to 18 (mean slope = 0.961, 95% CI [0.773, 1.149], p < .001). The second group, which comprised 22.3% of the sample, was the high-and-stable class. Youth in this group reported a high level of racial discrimination that remained high across time (mean intercept = 8.610, 95% CI [7.691, 9.529], p < .001; mean slope = 0.160, 95% CI [−0.287, 0.607], p = .484). Figure 1 illustrates the discrimination trajectories for the classes identified. Table 1 presents demographic characteristics for both racial discrimination exposure groups and for the entire sample. As Table 1 indicates, both the entire sample and the high-and-stable class included more female than male youth.
Figure 1.
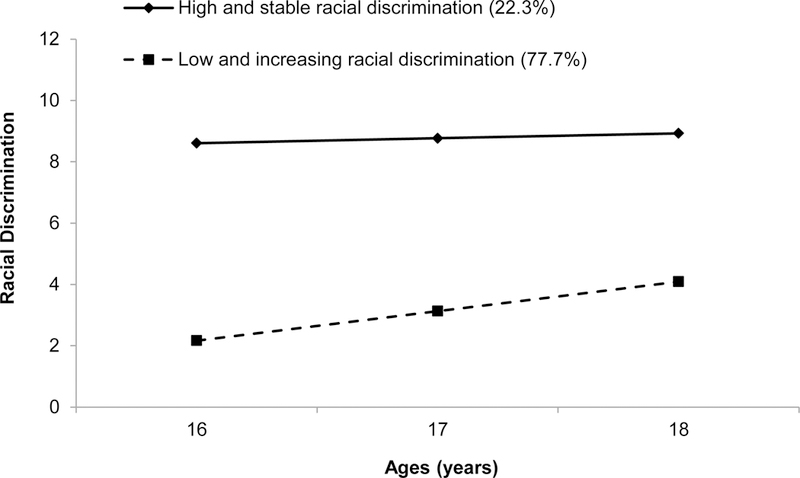
The estimated trajectories of racial discrimination for each class.
Table 1.
Demographic Characteristics by Racial Discrimination Trajectory Groups
| Whole Sample (N = 337) |
Low-and-Increasing Class (n = 262) |
High-and-Stable Class (n = 75) |
|
|---|---|---|---|
| Characteristics | % or Mean (SD) | % or Mean (SD) | % or Mean (SD) |
| Age 16 | |||
| Target age (in years) | 15.58 (0.49) | 15.57 (0.50) | 15.60 (0.49) |
| Parent age (in years) | 42.20 (7.51) | 42.26 (7.77) | 41.99 (6.58) |
| Target gender, male | 38.9% | 40.5% | 33.3% |
| Family poverty | 48.2% | 49.2% | 44.9% |
| Parent unemployment | 23.1% | 22.8% | 24.0% |
| Parent education | |||
| < high school | 21.9% | 23.6% | 16.0% |
| HS degree or GED | 32.4% | 31.4% | 36.0% |
| Some college or technical school |
38.1% | 38.46% | 37.3% |
| ≥ college graduate | 7.5% | 6.6% | 10.7% |
| Single-parent status | 58.7% | 61.8% | 48.0% |
Racial Discrimination Trajectory Group Differences on Body Mass Index and Insulin Resistance
The first ANCOVA revealed that youth in the high-and-stable racial discrimination trajectory group displayed significantly higher IR scores at ages 25 and 27 (M = 1.355, 95% CI [1.288, 1.422]) than did those in the low-and-increasing group (M = 1.264, 95% CI [1.229, 1.299]), Cohen’s d = 0.313. Figure 2a depicts this finding. The second ANCOVA showed that youth in the high-and-stable group had significantly higher BMI at ages 19 to 21 (M = 31.211, 95% CI [29.259, 33.163]) than did those in the low-and-increasing group (M = 28.044, 95% CI [27.024, 29.064]), Cohen’s d = 0.377. Figure 2b illustrates this result.
Figure 2.
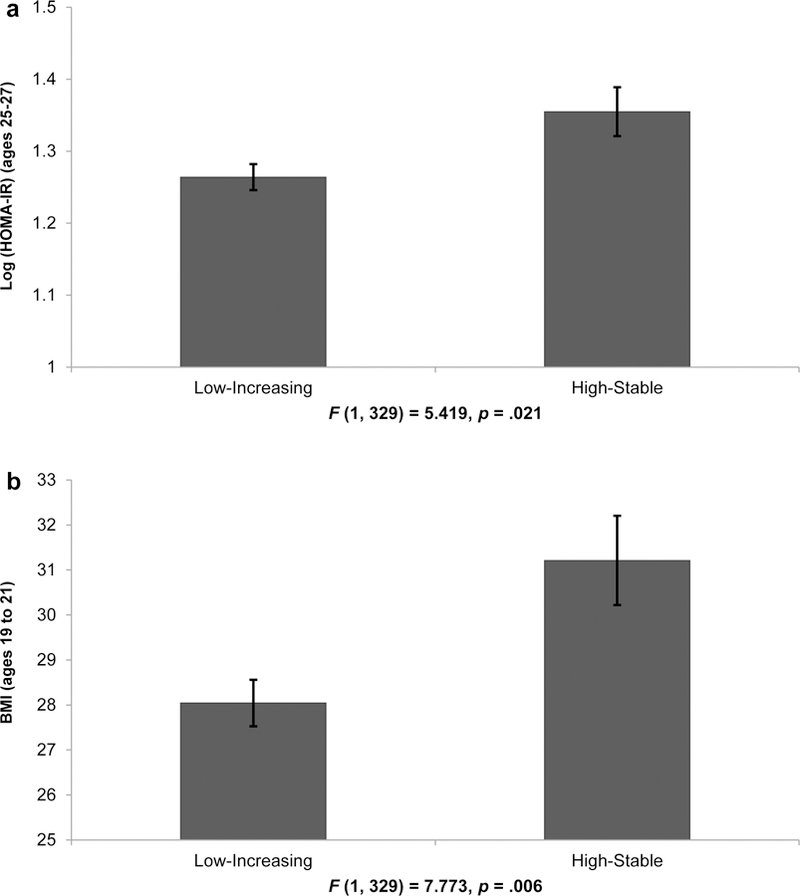
Means of (a) IR levels at ages 25 to 27 and (b) BMI at ages 19 to 21 for the racial discrimination trajectory groups. Error bars = ±1 standard error. Analyses controlled for gender, family SES disadvantage, depressive symptoms, life stress, drug use, and exercise.
Body Mass Index at Ages 19 to 21 as a Mediator of the Association between Racial Discrimination and Insulin Resistance at Ages 25 and 27
Table 2 presents descriptive statistics for, and correlations among, the study variables. The previously described analyses established associations of racial discrimination with subsequent BMI across ages 19 to 21 and IR at ages 25 and 27. Indirect (i.e., mediated) effects of racial discrimination on IR through BMI levels were also hypothesized. Figure 3 provides a conceptual diagram of the mediational analyses conducted. MacKinnon, Lockwood, Hoffman, West, and Sheets (2002) suggested that mediation analyses should be conducted when a relation exists between both a predictor and a mediator (Path A in Figure 3) and a mediator and an outcome (Path B in Figure 3). To be considered a mediator, the strength of the direct relation between the predictor and outcome (Path C in Figure 3) must decrease when the mediator is entered into the analysis (Path C′ in Figure 3). Covariates included in the mediational analysis were the same as those in prior analyses and only applied to the outcome variables. First, the relationship was established between the predictor (racial discrimination) and the potential mediator (BMI) and then the relationship of the mediator to the outcome (IR) was examined. Upon determining whether the mediator-to-outcome relationship was significant, BMI’s possible reduction of the direct effect of racial discrimination on IR was explored.
Table 2.
Correlations and Descriptive Statistics among Study Variables
| Study Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Log (HOMA-IR) (ages 25–27) | -- | ||||||||
| 2. BMI (ages 19–21) | .593*** | -- | |||||||
| 3. Discrimination class a (ages 16–18) | .091 | .138* | -- | ||||||
| 4. Gender (male = 1) | −.303*** | −.181** | −.061 | -- | |||||
| 5. Family SES disadvantage (ages 16–18) | .125* | .107* | −.095 | −.010 | -- | ||||
| 6. Depressive symptoms (ages 16–17) | −.069 | −.034 | .209*** | −.044 | .069 | -- | |||
| 7. Personal life stress (ages 17–18) | .024 | .058 | .106 | .144** | .152** | .303*** | -- | ||
| 8. Substance use (ages 19–21) | −.215*** | −.073 | .151** | .269*** | −.051 | .130* | .247*** | -- | |
| 9. Exercise (ages 19–21) | −.103 | −.096 | −.090 | .239*** | .027 | −.095 | .046 | .017 | -- |
| Mean | 1.28 | 28.75 | 0.22 | 0.39 | 2.35 | 7.17 | 15.70 | 0.73 | 2.82 |
| SD | 0.31 | 8.58 | 0.42 | 0.49 | 1.25 | 5.22 | 1.56 | 0.65 | 1.55 |
Note. N = 337.
Membership in the high-and-stable class was coded as 1, and membership in the low-and-increasing class was coded as 0. BMI, body mass index; SES, socioeconomic status.
p < .05
p < .01
p < .001.
Figure 3.
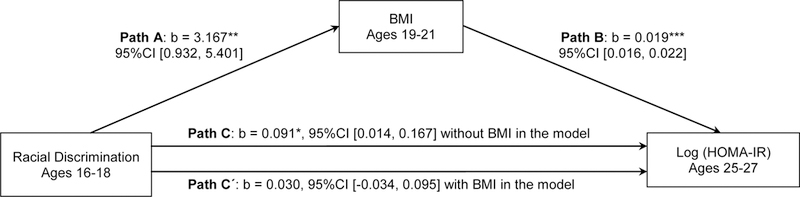
BMI at ages 19 to 21 as a mediator of the relation between racial discrimination at ages 16 to 18 and IR at ages 25 to 27. Family socioeconomic-related risk at ages 16 to 18, gender, youth depressive symptoms at ages 16 to 17, youth personal life stress at ages 17 to 18, and youth substance use and exercise at ages 19 to 21 were controlled (not shown). Unstandardized coefficients with 95% confident intervals (CI) are presented. N = 337. *p < .05; **p < .01; ***p < .001.
Figure 3 also shows the results of the mediational analyses. In the regression analyses, membership in the low-and-increasing trajectory group was assigned a value of 0; membership in the high-and-stable group was assigned a value of 1. As hypothesized, the presence of the mediator, BMI at ages 19 to 21, reduced the direct effect of membership in the high-and-stable group at ages 16 to 18 on risk for elevated IR at ages 25 and 27, from b = 0.091, 95% CI [0.014, 0.167], p = .021 to b = 0.030, 95% CI [−0.034, 0.095], p = .356. The indirect effect of high racial discrimination levels on risk for elevated IR via BMI was significant (estimates = .060, 95% BCA [0.014, 0.115] with 1000 bootstrapping).
To clarify the results further, life stress, depression, exercise, and drug use were considered as possible mediators. These variables were included in separate models as mediators linking racial discrimination with IR. None of these indirect/mediating pathways, however, reached statistical significance. Gender was also considered as a potential moderator of the pathways in the mediation model. None of the interactions with gender reached statistical significance.
Discussion
During their high school years, African American adolescents simultaneously experience emotional and social challenges while developing independence, a sense of self, and racial identity. Adolescence is also a time when African American youth become keenly aware of their treatment relative to others and are particularly cognizant of targeted rejection. Against this developmental backdrop, and building on previous studies of exposure to racial discrimination and preclinical indicators such as elevated glucocorticoids and pro-inflammatory cytokines (Lewis et al., 2015), exposure to high doses of racial discrimination across adolescence were found to presage IR diagnosed 7 years later. These findings are among the first to establish a link between racial discrimination and a clinical indicator of cardiometabolic health during the transition to adulthood. If their risk for IR persists, these young adults will likely experience disproportionately high rates of morbidity and mortality from type 2 diabetes and cardiovascular disease in future decades (Mottillo et al., 2010).
Evidence, shown in Figure 2, emerged to indicate that BMI mediates the linkage between exposure to relatively high levels of racial discrimination across adolescence and IR. Adolescents exposed to more race-related stress are at heightened risk for IR, and this association is largely attributable to elevated BMI. These findings extend earlier research by focusing on a group of adolescents close in age, obtaining repeated assessments of racial discrimination and BMI, and testing the hypothesis that BMI serves as a mediator linking trajectories of racial discrimination to IR. Although these are important additions to the literature on the development of IR in cardiometabolic risk, caution must be exercised in their interpretation.
BMI may have contributed to exposure to racial discrimination; even though discrimination was assessed before BMI, it was not necessarily experienced first. In future longitudinal studies, it will be important to determine whether having an elevated BMI increases exposure to racial discrimination. In addition, future research should examine potential mediators between exposure to discrimination and BMI. Stress reduction is a plausible mediator. When young people are exposed frequently to racial discrimination in their daily lives, some may increase their consumption of high-calorie foods to help alleviate negative affect and other effects of stress (J. S. Jackson et al., 2010).
Recent research has begun to establish that perceived weight stigma, principally weight discrimination, is associated with physical health consequences. Perceived weight discrimination is associated with increases in weight, waist circumference, and, for those in the overweight range, the development of obesity over time (S. E. Jackson, Beeken, & Wardle, 2014). The effects of weight discrimination are particularly pernicious among those who internalize discriminatory weight-based attitudes. This self-directed stigma, also known as weight-based internalization (WBI), is associated with increases in binge eating (Hübner et al., 2016), reductions in physical activity (Pearl, Puhl, & Dovidio, 2015), and the presence of metabolic syndrome (Pearl et al., 2017). Thus, as intersectionality paradigms have suggested (Himmelstein, Puhl, & Quinn, 2017), research on the contributions of racial discrimination to cardiometabolic outcomes should include measures of weight discrimination and WBI. This approach not only will disentangle the unique contributions of racial discrimination and weight discrimination, but also will allow the testing of a “double jeopardy hypothesis” that persons of color with higher weight are at particularly high cardiometabolic risk.
Several potential explanations for this study’s findings were eliminated. First, family SES risk, depressive symptoms, and personal life stress were assessed at the same time as racial discrimination. The results in Table 2 show that neither depressive symptoms nor personal life stress was associated with subsequent assessments of BMI or IR. Conversely, racial discrimination was associated over time with both health indicators. Because family SES risk is associated with both BMI and IR, SES risk was controlled in all data analyses. Physical activity was not associated with IR. Drug use was negatively associated with IR, suggesting that it does not act as a mediator connecting racial discrimination with IR. These findings are consistent with results from other studies showing that, although obesity and drug use take a toll on health outcomes, they may do so in different ways. Drug use increases risks for mental health problems, including depression, anxiety, and delinquency (Elliott, Huizinga, & Menard, 2012; Grant et al., 2004). In contrast, to the extent that it leads to obesity, overeating heightens risk for IR and, later in life, cardiovascular disease (Grundy, 2004; Guh et al., 2009). Although other stress-related mediators of racial discrimination effects exist, such as sleep loss, elevated adrenocortical and sympathetic outflow, or inflammatory activity (Kelly & Ismail, 2015), the results of this study support the plausibility of the underlying model of racial discrimination → BMI → IR. This study reinforces the notion that exposure to racial discrimination during adolescence has consequences for cardiometabolic health. The results suggest that race-related stressors contribute to cardiometabolic risk in young Black adults and may exacerbate existing community health disparities.
Strengths of this study include the longitudinal, prospective design that included assessments of racial discrimination and BMI across time, as well as their associations with IR. The lack of a BMI or IR assessment at the first wave of data collection is a major limitation. Because this study was not initially designed to focus on health, it included no individual health, family health history, biological, or anthropometric measures. In addition racial discrimination before age 16 years was not assessed, even though the literature suggests that exposure to discrimination before age 12 could have an important impact on children (Lee & Ahn, 2013; Sanders-Phillips et al., 2014; Schmitt, Branscombe, Postmes, & Garcia, 2014). Thus, future research should be designed to determine whether the relations found in this study, including trajectories of discrimination, are evident at younger ages. Finally, because this study was conducted with rural African American adolescents, future research should be designed to determine whether patterns would be different among urban African American adolescents, other minority groups, or Caucasian adolescents. These cautions notwithstanding, this study is among the first to show a positive, prospective association between perceived discrimination and IR.
Acknowledgments
This work was supported by award number R01 HD030588 from the National Institute of Child Health and Human Development and award number P30 DA027827 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Gene H. Brody, Center for Family Research, University of Georgia
Tianyi Yu, Center for Family Research, University of Georgia.
Edith Chen, Department of Psychology and Institute for Policy Research, Northwestern University of Georgia.
Gregory E. Miller, Department of Psychology and Institute for Policy Research, Northwestern University of Georgia
Katherine B. Ehrlich, Department of Psychology and Center for Family Research, University of Georgia.
References
- Björntorp P, & Rosmond R (1999). Hypothalamic origin of the metabolic syndrome X. Annals of the New York Academy of Sciences, 892, 297–307. 10.1111/j.1749-6632.1999.tb07803.x [DOI] [PubMed] [Google Scholar]
- Brody GH, Chen Y.-f., & Kogan SM (2010). A cascade model connecting life stress to risk behavior among rural African American emerging adults. Development and Psychopathology, 22, 667–678. 10.1017/S0954579410000350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Chen Y.-f., Murry VM, Ge X, Simons RL, Gibbons FX, … Cutrona CE (2006). Perceived discrimination and the adjustment of African American youths: A five-year longitudinal analysis with contextual moderation effects. Child Development, 77, 1170–1189. 10.1111/j.1467-8624.2006.00927.x [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, & Beach SRH (2016). Resilience to adversity and the early origins of disease. Development and Psychopathology, 28(4, pt. 2), 1347–1365. 10.1017/S0954579416000894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen Y. f., Kogan SM, Evans GW, Beach SRH, … Philibert RA (2013). Cumulative socioeconomic status risk, allostatic load, and adjustment: A prospective latent profile analysis with contextual and genetic protective factors. Developmental Psychology, 49, 913–927. 10.1037/a0028847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Miller GE, & Chen E (2015). Discrimination, racial identity, and cytokine levels among African American adolescents. Journal of Adolescent Health, 56, 496–501. 10.1016/j.jadohealth.2015.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). National Diabetes Statistics Report: Estimates of Diabetes and its Burden in the United States, 2014 Atlanta, GA: U.S. Department of Health and Human Services; Retrieved from https://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. [Google Scholar]
- Cunningham TJ, Berkman LF, Kawachi I, Jacobs DR Jr., Seeman TE, Kiefe CI, & Gortmaker SL (2013). Changes in waist circumference and body mass index in the US CARDIA cohort: Fixed-effects associations with self-reported experiences of racial/ethnic discrimination. Journal of Biosocial Science, 45, 267–278. 10.1017/S0021932012000429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, & Menard S (2012). Multiple problem youth: Delinquency, substance use, and mental health problems New York, NY: Springer Science+Business Media. [Google Scholar]
- Geronimus AT, Hicken M, Keene D, & Bound J (2006). “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health, 96, 826–833. 10.2105/AJPH.2004.060749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Malone S, Richardson EA, Cheadle JE, & Williams DT (2015). Perceived discrimination and markers of cardiovascular risk among low-income African American youth. American Journal of Human Biology, 27, 546–552. 10.1002/ajhb.22683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, … Kaplan K (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 61, 807–816. Retrieved from http://jamanetwork.com/journals/jamapsychiatry/fullarticle/482045 [DOI] [PubMed] [Google Scholar]
- Greene ML, Way N, & Pahl K (2006). Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: Patterns and psychological correlates. Developmental Psychology, 42, 218–236. 10.1037/0012-1649.42.2.218 [DOI] [PubMed] [Google Scholar]
- Grundy SM (2004). Obesity, metabolic syndrome, and cardiovascular disease. Journal of Clinical Endocrinology and Metabolism, 89, 2595–2600. 10.1210/jc.2004-0372 [DOI] [PubMed] [Google Scholar]
- Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, & Anis AH (2009). The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health, 9:88 10.1186/1471-2458-9-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach New York, NY: Guilford Press. [Google Scholar]
- Himmelstein MS, Puhl RM, & Quinn DM (2017). Intersectionality: An understudied framework for addressing weight stigma. American Journal of Preventive Medicine, 53, 421–431. 10.1016/j.amepre.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Hübner C, Baldofski S, Crosby RD, Müller A, de Zwaan M, & Hilbert A (2016). Weight-related teasing and non-normative eating behaviors as predictors of weight loss maintenance. A longitudinal mediation analysis. Appetite, 102, 25–31. 10.1016/j.appet.2016.02.017 [DOI] [PubMed] [Google Scholar]
- Hunte HER, & Williams DR (2009). The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. American Journal of Public Health, 99, 1285–1292. 10.2105/AJPH.2007.128090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, & Rafferty JA (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100, 933–939. 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SE, Beeken RJ, & Wardle J (2014). Perceived weight discrimination and changes in weight, waist circumference, and weight status. Obesity, 22, 2485–2488. 10.1002/oby.20891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson P, Risica PM, Gans KM, Kirtania U, & Kumanyika SK (2012). Association of perceived racial discrimination with eating behaviors and obesity among participants of the SisterTalk study. Journal of the National Black Nurses Association, 23, 34–40. [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2007). Monitoring the Future national survey results on drug use, 1975-2006. Volume I: Secondary school students (NIH Publication No. 07–6205). Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Kelly SJ, & Ismail M (2015). Stress and type 2 diabetes: A review of how stress contributes to the development of type 2 diabetes. Annual Review of Public Health, 36, 441–462. 10.1146/annurev-publhealth-031914-122921 [DOI] [PubMed] [Google Scholar]
- Kovacs M (1979). Treating depressive disorders: The efficacy of behavior and cognitive therapies. Behavior Modification, 3, 496–517. 10.1177/014544557934004 [Google Scholar]
- Krieger N (2014). Discrimination and health inequities. International Journal of Health Services, 44, 643–710. 10.2190/HS.44.4b [DOI] [PubMed] [Google Scholar]
- Lackey DE, & Olefsky JM (2016). Regulation of metabolism by the innate immune system. Nature Reviews Endocrinology, 12, 15–28. 10.1038/nrendo.2015.189 [DOI] [PubMed] [Google Scholar]
- Landrine H, & Klonoff EA (1996). The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology, 22, 144–168. 10.1177/00957984960222002 [Google Scholar]
- Lee DL, & Ahn S (2013). The relation of racial identity, ethnic identity, and racial socialization to discrimination distress: A meta-analysis of Black Americans. Journal of Counseling Psychology, 60, 1–14. 10.1037/a0031275 [DOI] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11, 407–440. 10.1146/annurev-clinpsy-032814-112728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. 10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, & Turner RC (1985). Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 28, 412–419. 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. 10.1111/j.1749-6632.1998.tb09546.x [DOI] [PubMed] [Google Scholar]
- Menke A, Casagrande S, Geiss LS, & Cowie CC (2015, September 8). Prevalence of and trends in diabetes among adults in the United States, 1988–2012. Journal of the American Medical Association, 314, 1021–1029. 10.1001/jama.2015.10029 [DOI] [PubMed] [Google Scholar]
- Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, … Eisenberg MJ (2010). The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. Journal of the American College of Cardiology, 56, 1113–1132. 10.1016/j.jacc.2010.05.034 [DOI] [PubMed] [Google Scholar]
- Nelson DS, Gerras JM, McGlumphy KC, Shaver ER, Gill AK, Kanneganti K, … Hasson RE (2018). Racial discrimination and low household education predict higher body mass index in African American youth. Childhood Obesity, 14, 114–121. 10.1089/chi.2017.0218 [DOI] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, … Gee GC (2015, September 23). Racism as a determinant of health: A systematic review and meta-analysis. PLoS ONE, 10:e0138511 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135, 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, Puhl RM, & Dovidio JF (2015). Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. Journal of Health Psychology, 20, 1626–1632. 10.1177/1359105313520338 [DOI] [PubMed] [Google Scholar]
- Pearl RL, Wadden TA, Hopkins CM, Shaw JA, Hayes MR, Bakizada ZM, … Alamuddin N (2017). Association between weight bias internalization and metabolic syndrome among treatment‐seeking individuals with obesity. Obesity, 25, 317–322. 10.1002/oby.21716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, & Kelly Y (2013). A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science and Medicine, 95, 115–127. 10.1016/j.socscimed.2012.11.031 [DOI] [PubMed] [Google Scholar]
- Sanders-Phillips K, Kliewer W, Tirmazi T, Nebbitt V, Carter T, & Key H (2014). Perceived racial discrimination, drug use, and psychological distress in African American youth: A pathway to child health disparities. Journal of Social Issues, 70, 279–297. 10.1111/josi.12060 [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, & Garcia A (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140, 921–948. 10.1037/a0035754 [DOI] [PubMed] [Google Scholar]
- Schuster MA, Elliott MN, Kanouse DE, Wallander JL, Tortolero SR, Ratner JA, … Banspach SW (2012, August 23). Racial and ethnic health disparities among fifth-graders in three cities. New England Journal of Medicine, 367, 735–745. 10.1056/NEJMsa1114353 [DOI] [PubMed] [Google Scholar]
- Shelton RC, Puleo E, Bennett GG, McNeill LH, Sorensen G, & Emmons KM (2009). The association between racial and gender discrimination and body mass index among residents living in lower-income housing. Ethnicity and Disease, 19, 251–257. [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, & McEwen BS (2009, June 3). Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. Journal of the American Medical Association, 301, 2252–2259. 10.1001/jama.2009.754 [DOI] [PubMed] [Google Scholar]
- Simons RL, Chen Y. f., Stewart EA, & Brody GH (2003). Incidents of discrimination and risk for delinquency: A longitudinal test of strain theory with an African American sample. Justice Quarterly, 20, 827–854. 10.1080/07418820300095711 [Google Scholar]
- Stepanikova I, Baker EH, Simoni ZR, Zhu A, Rutland SB, Sims M, & Wilkinson LL (2017). The role of perceived discrimination in obesity among African Americans. American Journal of Preventive Medicine, 52(Suppl 1), S77–S85. 10.1016/j.amepre.2016.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson HC (2004). Racial socialization. In Jones RL (Ed.), Black psychology (4th ed., pp. 176–189). Hampton, VA: Cobb and Henry. [Google Scholar]
- Thorpe RJ, Parker LJ, Cobb RJ, Dillard F, & Bowie J (2017). Association between discrimination and obesity in African-American men. Biodemography and Social Biology, 63, 253–261. 10.1080/19485565.2017.1353406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57, 1152–1173. 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders KH, Hoyt LT, & Adam EK (2014). Associations between self-reported discrimination and diurnal cortisol rhythms among young adults: The moderating role of racial–ethnic minority status. Psychoneuroendocrinology, 50, 280–288. 10.1016/j.psyneuen.2014.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]


