Abstract
Purpose
Genotoxic wastes are one type of hospital wastes that are extremely dangerous and may cause cell mutation or cancer and their disposal should be taken seriously. Cytotoxic drugs are main component of these wastes. The purpose of this study was to determine the types and quantities of genotoxic wastes in hospitals of Tehran University of Medical Sciences and evaluation of genotoxic waste management index.
Methods
For this purpose, a questionnaire was used to collect data. Each question was scored according to compliance or non-compliance with the law, and genotoxic hospital waste management index was calculated for each hospital.
Results
Various parameters including waste generation rate, segregation, collection, transportation, storage, disposal and the hygiene of personnel were evaluated. The results showed that 60% of hospitals ranked medium, 27% ranked poor and 13% ranked as very poor according to this index.
Conclusions
Since the condition of genotoxic waste management in this study was ranked as medium, therefore some steps of hospital waste management system require improvement.
Keywords: Genotoxic waste, Cytotoxic drugs, Genotoxic waste management index, GWMI, Hospital wastes management index, HWMI
Introduction
In recent decades an increase in the rate of medical waste generation occurs due to the population growth [1]. According to the law, healthcare waste can be classified into nine different categories including infectious, pathological, sharps, hazardous pharmaceuticals, genotoxic substances and dangerous chemical wastes with a high content of metals, pressurized containers, and radioactive materials. According to the documents of the World Health Organization (WHO), about 80% of hospital waste categorized as non-risk waste, while 20% of them is considered as hazardous waste. Genotoxic wastes are a subset of hazardous waste that may have mutagenic, teratogenic or carcinogenic properties. This kind of wastes include residues of certain cytostatic drugs or vomit, urine and feces from patients treated with cytostatic drugs, chemicals and radioactive material [2]. On the other hand, recent use of pharmaceuticals and anti-cancer drugs for treating a variety of diseases and cancers are increased, therefore some of these drugs also considered as genotoxic agents. Human exposure to these substances can occur during treatment or among people who work in the medicine factories, nurses and other hospital staff [3]. In a more comprehensive look, all of the healthcare workers, patients, waste handlers and the general public are exposed to health risks of healthcare wastes [4]. As mentioned, such waste can create serious safety problems. So poor management of these wastes leads to infertility, cancers, mutations and dermatitis [5, 6].
Healthcare waste management includes all activities involved: generation, segregation, transportation, storage, treatment, and the final disposal of wastes which is generated in the healthcare facilities [7]. Unfortunately healthcare waste management is performed poorly at a lot of healthcare facilities. Hence identifying the causes and then supporting the improvements of the system are two important key skills that healthcare facility management need for their development [8]. So in order to achieve these goals, training has an important role in healthcare waste management system. For example the results of a study in Spain showed that the training of health care waste management improves biomedical waste segregation at hospitals, so after the intervention, a significant weight reduction in the monthly average of infectious and genotoxic/pharmaceutical waste, observed [9]. Furthermore, a study in Ulaanbaatar, Mongolia indicated that the current system of healthcare waste management has fundamental problems, such as the lack of a comprehensive policy and strategy and inadequate knowledge and skills of healthcare sector personnel [10]. In addition, another study in Mauritius showed that, there is a poor management of medical waste in both institutions (private and public) because of the lack of a proper medical waste management policy for the separately disposal of medical wastes [11].
In this study, the status of genotoxic waste management in hospitals of Tehran University of Medical Sciences was determined. The present research aimed to identify the gaps in current practices of healthcare waste in the capital of Iran, Tehran, as a measured against the official rules.
Materials and methods
The study was carried out from April to July 2014. For this research fourteen public hospitals form Tehran University of Medical Sciences were selected. Different medical waste management process, namely segregation, collection, transportation, storage, treatment and also health conditions of healthcare workers were studied. For this purpose, a standardized questionnaire, approved by the Iran Ministry of Health, was used to collect data. This questionnaire consists of two general sections. The first section includes questions about the management of hospital waste (except genotoxic waste) and second section includes questions about the management of genotoxic waste. Each section consists of seven parts including general hospital information, health condition of the staff and personnel training, segregation, collection, transportation, storage, treatment and disposal of waste.
It should be noted that the rearrangement method was used for checking of the reliability and validity of questionnaire. Such that after filling out the questionnaires in the first step and after passing a short time, under the previous conditions, again the questionnaires were filled and finally the coefficient of reliability (Cronbach’s alpha) was calculated. Cronbach’s α is a function of the number of items in a test, the average covariance between item-pairs, and the variance of the total score. The results showed that in this case, 113 questions in the re-test had the same response among the all questions (total questions = 124) and the Cronbach’s alpha coefficient in the rest of the questions (11 questions) was calculated between 0.7 to 1 which is the indication of the validity of our questionnaires.
After filling the questionnaires for each of the hospitals, each part was scored according to the compliance with the standards from zero to ten. The sum of scores in each phase of the management process (segregation, etc.) was divided by the number of questions in that section and multiplied by 100 to convert the initial scores of answers to the score of the related management process. Finally to convert the final score of each hospital to HWMI (Hospital Waste Management Index), the weighting factor associated to each healthcare waste management process were used according to Table 1. The weighting factors and ranking criteria were set up by a panel of experts [12]. The ranking criteria for the interpretation of HWMI values are included in Table 2.
Table 1.
Hospital waste management weighting factors
| Healthcare waste management process | Weight |
|---|---|
| Segregation | 10 |
| Collection | 10 |
| Transportation | 10 |
| Storage | 10 |
| Disposal | 50 |
| Personnel hygiene condition | 10 |
Table 2.
Hospital waste management ranking criteria
| Range | Rank |
|---|---|
| 91–100 | Excellent |
| 71–90 | Good |
| 51–70 | Medium |
| 26–50 | Poor |
| 0–25 | Very poor |
Results and discussion
As previously mentioned one of the main purposes of this study was investigation and evaluation of the current status of genotoxic waste management that has to be managed in order to comply with the law. The regulation and law focus more on segregation and collection of healthcare waste, right at the point of production. To meet this goal, practically they are required to separate healthcare wastes according to the color coding system of the WHO. In addition, the law discusses the properties of the “storage location” of genotoxic waste as well as their transportation regulations by emphasizing on the use of trolleys which should to be changed at the end of the ward, on the way to the temporary storage location. There are also guidelines for disposal of genotoxic waste. Here the results of each part of healthcare waste management will be investigated separately.
Generation rate: In fact, the quantity of healthcare waste generated varies in different countries and even within in a single country. Healthcare waste production depends on different factors such as the number of hospital’s beds, the socio-economic and cultural status of patients, knowledge of workers, the number of customers, and the waste management process [13]. For present study the numbers of occupied beds in each 14 hospitals and the total amounts of generated waste per beds (1000 Kg/Year) are present in Table 3. In addition, the total statistical analysis of general waste, infectious wastes and genotoxic wastes (in kg per year) are given in Table 4.
Table 3.
The numbers of occupied beds and the total amounts of generated waste
| Hospital | No. Bed | Waste(1000 Kg/Year) |
|---|---|---|
| 1 | 557 | 324 |
| 2 | 338 | 145.8 |
| 3 | 171 | 134.64 |
| 4 | 352 | 226.8 |
| 5 | 227 | 129.6 |
| 6 | 69 | 72 |
| 7 | 185 | 72 |
| 8 | 518 | 432 |
| 9 | 113 | 46.8 |
| 10 | 122 | 126 |
| 11 | 450 | 576 |
| 12 | 120 | 126 |
| 13 | 232 | 334.8 |
| 14 | 290 | 389.52 |
Table 4.
Statistical analysis of different waste types in hospitals (N = 14)
| Statistical analysis parameters | Kg/Bed.Year | ||
|---|---|---|---|
| General wastes | Infectious wastes | Genotoxic wastes | |
| Mean | 846.1 | 631.1 | 14.3 |
| Median | 810.7 | 575.5 | 4.5 |
| Standard Deviation | 357.8 | 291.1 | 28.8 |
| Minimum | 389.2 | 298.2 | 0.5 |
| Maximum | 1443.1 | 1319 | 103.2 |
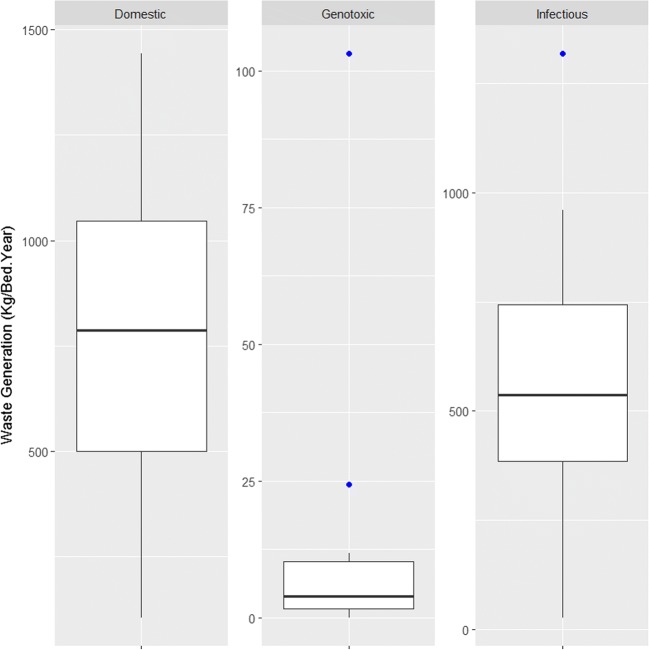
Records showed that the amount of domestic, infectious and genotoxic wastes respectively are 2.18, 1.64 and 0.036 kg bed−1 day−1. Also the box plot for showing the distributions of these three kinds of waste is given in Fig. 1.
Fig. 1.
Distribution of domestic, infectious and genotoxic waste
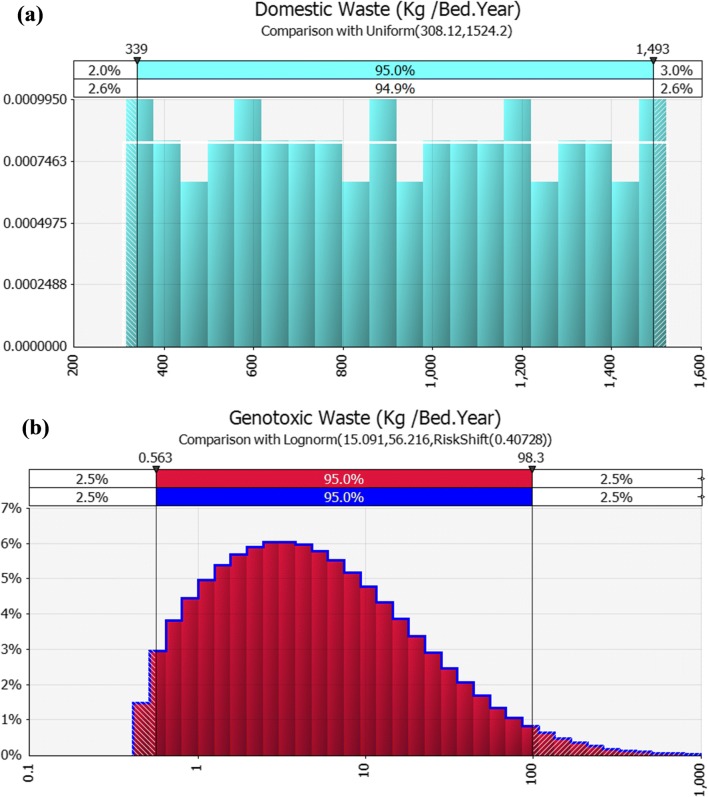
Furthermore Fig. 2 shows the distribution of two main waste type (domestic and genotoxic waste) distributions. As shown in Fig. 2a, domestic waste’s production follows a uniform distribution, which shows that %95 of the production of domestic waste is between 339 and 1493 kg per year per bed. While the distribution of genotoxic waste Fig. 2b follows a lognormal distribution which shows that %95 of the genotoxic waste’s production is between 0.563 and 98.3 kg per year per bed.
Fig. 2.
Distribution pattern of (a) domestic and (b) genotoxic waste
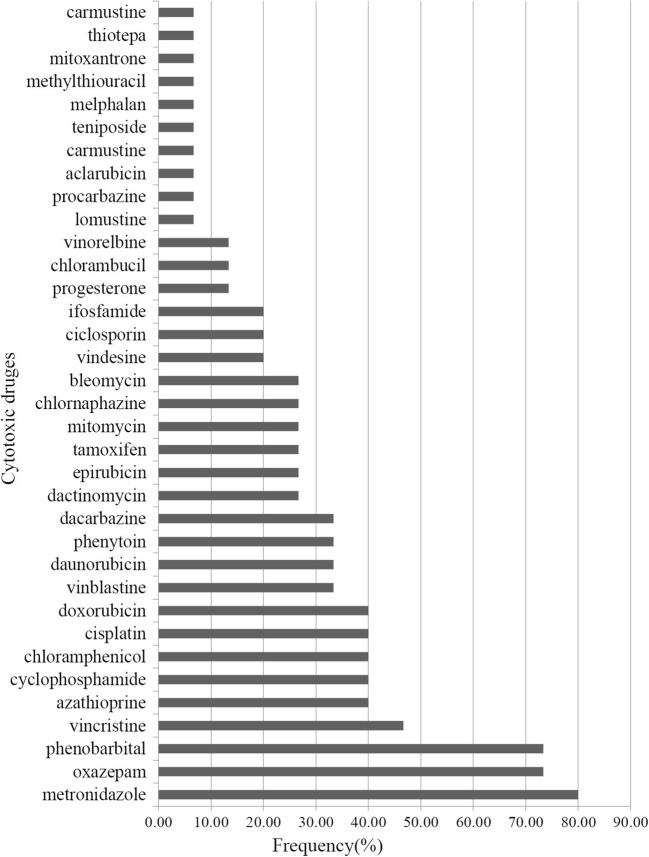
On the other hand, Fig. 3 showed the most common cytotoxic drugs which used in our under studied hospitals. This results show that the most common cytotoxic drugs that are used in hospitals are: Metronidazole, Oxazepam and Phenobarbital.
Fig. 3.
The most common cytotoxic drugs used in hospitals
To find the answer of this question which what is the correlation between the number of beds with the types and amount of genotoxic waste, Pearson’s correlation coefficient was calculated. In this test the R correlation coefficient was equal to 0.0882453 which is insignificant and means that the correlation between the number of beds with the types and amount of genotoxic waste is only about %8 which is very weak. This means that our variables are approximately independent and there is no relationship between them. This is because of this reason that most of the patients who require genotoxic drugs need to receive an outpatient treatment and do not occupy any bed.
Similar studies which conducted in other Iranian cities, for example a survey conducted in Fars province, revealed that the average of waste generation in a university hospital was 4.5 kgbed−1 day−1, from which 1.9 kgbed−1 day−1was domestic wastes and 2.4 kgbed−1 day−1was infectious wastes [14]. In other study which conducted in Kerman province of Iran, the total amounts of healthcare waste generation were estimated between 69.5 to 1315 kgday−1which included 71.37% general waste, 23.14% infectious waste and 0.93% pharmaceutical and chemical waste [15].
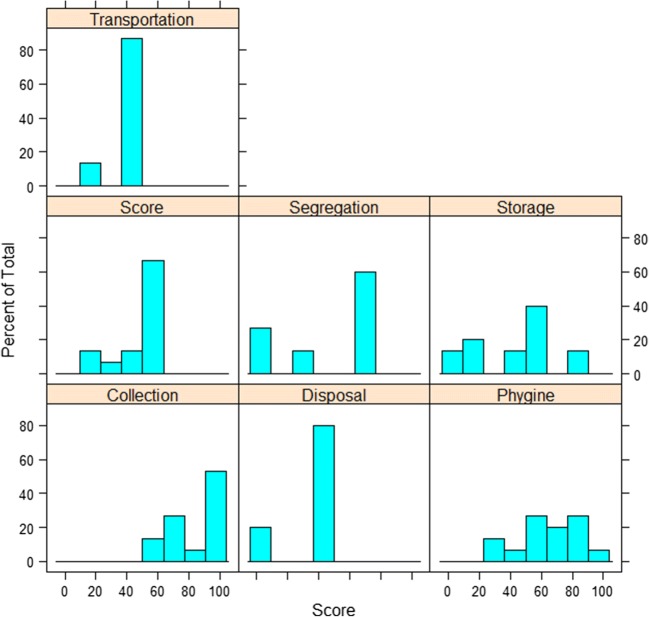
The research of Taghipour and Mosaferi (2009) showed that in Tabriz, the largest city in north western of Iran, the average of total production of healthcare waste was 3.8 kgbed−1 day−1, out of which 1.0 kgbed−1 day−1was infectious waste and 2.4 kgbed−1 day−1of them was domestic waste [16]. It is necessary to noting that the amount of infectious waste in some other countries is lower than that observed in this study. For example, the results of a study conducted in Istanbul, Turkey (2007), showed that the average waste production was 0.9 kgbed−1 day−1, out of which 0.3 kg of them was infectious and 0.1 kg was sharps wastes [17]. Another study in Brazil showed that the total and infectious waste generation rates in Brazilian hospitals were 3.245 and 0.57 kgbed−1 day−1, respectively [18]. The contribution and descriptive statistics of each rank in different stages of genotoxic wastes management is presented in Table 5. Also the score of each stage of genotoxic waste management in the selected hospitals are shown in Fig. 4. As the Fig. 4 and Table 5 present, the greatest weakness at the management of genotoxic waste is in the segregation, storage and disposal phase. As well as in transportation phase most hospitals are in the same situation.
Segregation: An important key factor to minimize of waste generation and effective management of healthcare waste is segregation; this needs to take place as close as possible to where the waste is generated. In addition, the categories of healthcare waste should be identified by using color-coded containers [2]. In present research, at the segregation phase, 60% of hospitals were in medium status, 13% was poor and 27% ranked as very poor. Segregation of genotoxic waste was not performed in 27% of hospitals; and in other hospitals that segregation of the genotoxic waste happened, 23% used brown color bags and 77% used white bags. About 73% of hospitals in which the source genotoxic waste segregation is done, used warning sign at the collecting bags. The results of a similar study that conducted in Brazil demonstrated that 86% of the healthcare facilities separated hazardous wastes from domestic waste at source and stores their solid wastes in separate plastic bags and containers [19].
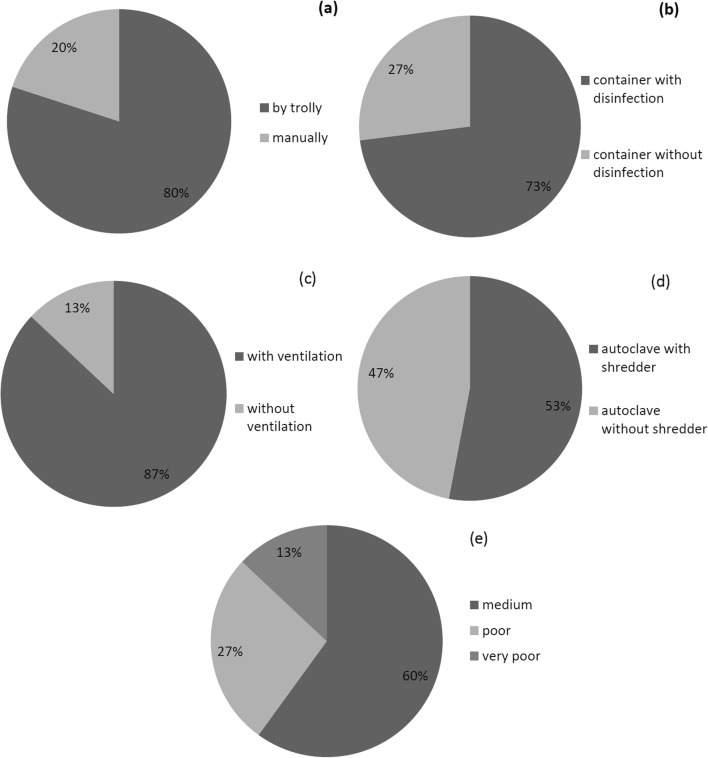
Collection: Status of the healthcare waste collection in hospitals in our study were acceptable, so that 53% of hospitals ranked as excellent, 27% ranked as good and 20% ranked as medium. Wastes in 80% of hospitals collected by trolley and in the other remaining 20% collected manually (Fig. 5a). In 47% of hospitals, medical wastes were collected from hospital wards twice a day and in 53% of them three times a day. Also the results of the research found that 73% of the containers in our under studied hospitals were properly disinfected and washed (Fig. 5b. It was also revealed that the bags are tightly sealed, and collected when three-quarters of their volume is filled. So with this interpretation, collection phase has a good status in our hospitals.
Table 5.
Descriptive statistics and the share of each rank in different stages of genotoxic wastes management (N = 14)
| Statistics | Segregation | Collection | Transportation | Storage | Disposal | Personnel hygiene condition |
|---|---|---|---|---|---|---|
| Mean | 44.73 | 84.93 | 45.6 | 44 | 35.8 | 66 |
| Median | 67 | 92 | 50 | 60 | 43 | 70 |
| St. dev | 30.11 | 19.56 | 11.61 | 19.56 | 19.56 | 19.53 |
| Minimum | 0 | 63 | 17 | 0 | 7 | 30 |
| Maximum | 67 | 100 | 50 | 80 | 43 | 100 |
| Percentage of hospitals in each ranges | ||||||
| Excellent | 53 | 7 | ||||
| Good | 27 | 13 | 27 | |||
| Medium | 60 | 20 | 40 | 46 | ||
| Poor | 13 | 87 | 34 | 80 | 20 | |
| Very poor | 27 | 13 | 13 | 20 | ||
| Total | 100 | 100 | 100 | 100 | 100 | 100 |
Fig. 4.
Score of each stage of genotoxic waste management in selected hospitals
Fig. 5.
a Percentage of the type of genotoxic collection device, (b) percentage of washing and disinfection of waste containers, (c) percentage of existence of ventilation in temporary storage area, (d) percentage of type of autoclave and (e) the status of Genotoxic Waste Management Index (GWMI) in selected hospitals
The results of another study in Tehran in 2008 showed that in 17% of hospitals, medical wastes were collected daily and in 25%the collection program was unsteady. The medical wastes could be collect either by trolley or manually. In46% of hospitals these wastes were collected by trolley and in 46% manually and in 8% both systems were applied (Dehghani et al. 2008).
Transportation: It was found that among the studied hospitals, 87% of them were ranked as poor in transportation phase and 13% ranked as very poor. Despite the emphasis of the law on changing the trolleys at the terminal point of each ward, unfortunately it was observed that most of the hospitals did not adhere to this law. This issue can transform domestic waste into infectious waste. So the rank of the transportation phase could be improved if trolleys were replaced with new ones at the terminal point of the ward, before transfer to the storage area. It should be noted that when the rules of transportation are not observed, the health risks increase in both staff and general public, so this step is very important. Our observations showed that the off-site genotoxic waste transportation from hospitals was done by private contractors and in 100% of them, there were no control on transportation processes.
Storage: The storage phase in 13% of hospitals ranked good, 40% of hospitals ranked medium, 34% of hospitals ranked poor and in 13% of hospitals ranked very poor. Storage locations in all selected hospitals were designated inside the hospital area in the yard. The distance between these sites to the nearest department in 33% of hospitals was lower than 100 m, in 27% of hospitals was between 100 and 200 m and in 40% of hospitals was between 200 and 1000 m. 87% of hospitals had a well sanitized and secured temporary storage area and the others (13%) had poorly sanitized temporary storage areas (Fig. 5c. The storage time for genotoxic wastes in 54% of hospitals were 30 days, 16% of hospitals 7 days, 15% of hospitals 60 days and 15% of them 90 days. The law stipulates that a separate place (specific storage location) should be designed for genotoxic waste but none of the hospitals had no separate storage location for genotoxic wastes.
Disposal: In the disposal stage, 80% of hospitals ranked poor and 20% of hospitals ranked as very poor. In order dispose the genotoxic waste, 80% of the hospitals used incineration and all of them used non incineration methods (such as autoclave and hydroclave) for sterilization of infectious waste (Fig. 5d. Incineration is done by private contractors but there is no documentation in this regard. A study in Tehran by Dehghani in year 2008 showed that in all hospitals, liquid pharmaceutical and chemical wastes were poured into the sewage system [20]. Another study which conducted in Limpopo province, South Africa, revealed that the incinerators which used to treat the healthcare waste are rudimentary and have poor design and suffer operational problems [21]. In Spain despite the environmental problems created, still the most common treatment proposed for healthcare wastes is incineration [22].
Hygiene of personnel: In the present study, the rank of hygiene of the personnel was not satisfactory; 7% of hospitals ranked as excellent, 27% of hospitals ranked good, 46% of hospitals ranked medium and 20% of hospitals ranked as poor. In this study, the personals of 67% of hospitals are educated about collection and transportation of genotoxic wastes. In 13% of hospitals, there is no personal protective equipment and7% of hospitals even don’t have a waste management expert.
The status of genotoxic waste management index of hospitals is illustrated in Fig. 5e. As shown, 60% of hospitals ranked medium, 27% ranked poor and 13% ranked very poor. This study showed that improvement of hospital waste management in Tehran in order to fully abide by the law and to have a comprehensive operational plan to reduce the amount of waste is necessary. A study conducted in 12 Asian countries, namely Cambodia, China, Japan, Laos, Thailand, Vietnam, Singapore, Malaysia, Mongolia, Myanmar, Indonesia, and the Philippines, showed that healthcare waste management is an issue of concern in all these countries. Although some countries were ambitious to undertake healthcare waste management progressively, they either lacked the required knowledge, strategies, legislation, or budget, or a combination of these [23].
Conclusion
As mentioned, segregation is the first step of genotoxic waste management and in this study the status of segregation was ranked as medium and poor. This is due to the lack of knowledge and awareness in the field of genotoxic waste and its hazards as well as the lack of proper guidelines, legislation, regulations and instructions on health care waste management and lack of a specific plan for the management of genotoxic wastes. Since the condition of genotoxic waste management in this study was ranked as medium, therefore some steps of hospital waste management system require improvement. So, it is concluded that by following the state regulations and providing more training to the involved staff in future, an acceptable practice of healthcare waste management can be achieved.
Acknowledgments
This research was supported by grants from Tehran University of Medical Sciences and Health Services. The authors would like to acknowledge staff of all those hospitals in Tehran that participated in this study and helped the present research to develop.
Compliance with ethical standards
Conflict of interest
No potential conflict of interest was reported by the author.
References
- 1.Oweis R, Al-Widyan M, Al-Limoon O. Medical waste management in Jordan: a study at the king Hussein medical center. Waste Manag. 2005;25(6):622–625. doi: 10.1016/j.wasman.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Townend WK. Safe management of wastes from health care activities. Bull World Health Organ. 2001;79:171. [Google Scholar]
- 3.Keshava N, T-m O. Occupational exposure to genotoxic agents. Mutat Res Rev Mutat Res. 1999;437(2):175–194. doi: 10.1016/S1383-5742(99)00083-6. [DOI] [PubMed] [Google Scholar]
- 4.Kumar R, Khan EA, Ahmed J, Khan Z, Magan M, Nousheen, et al. Healthcare waste management (HCWM) in Pakistan: current situation and training options. J Ayub Med Coll Abbottabad. 2010;22(4):101–105. [PubMed] [Google Scholar]
- 5.Johannssen LM, Dijkman M, Bartone C, Hanrahan D, Boyer MG, Chandra C. Health care waste management guidance note. HNP discussion paper series. Washington, DC: World Bank; 2000. [Google Scholar]
- 6.Smith CA. Managing pharmaceutical waste: what pharmacist should know. J Pharm Soc Wis. 2002:17–22.
- 7.Manyele SV, Lyasenga TJ. Factors affecting medical waste Management in low-Level Health Facilities in Tanzania. Afr J Environ Sci Technol. 2010;4(5):304–318. [Google Scholar]
- 8.WHO RCfEHA, Bank W. Better health care waste management: an integral component of health investment. World Health Organization; 2005.
- 9.Mosquera M, Andres-Prado MJ, Rodriguez-Caravaca G, Latasa P, Mosquera ME. Evaluation of an education and training intervention to reduce health care waste in a tertiary hospital in Spain. Am J Infect Control. 2014;42(8):894–897. doi: 10.1016/j.ajic.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 10.Shinee E, Gombojav E, Nishimura A, Hamajima N, Ito K. Healthcare waste management in the capital city of Mongolia. Waste Manag. 2008;28(2):435–441. doi: 10.1016/j.wasman.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 11.Bokhoree C, Beeharry Y, Makoondlall-Chadee T, Doobah T, Soomary N. Assessment of environmental and health risks associated with the Management of Medical Waste in Mauritius. APCBEE Procedia. 2014;9(Supplement C):36–41. doi: 10.1016/j.apcbee.2014.01.007. [DOI] [Google Scholar]
- 12.Aghapour P, Nabizadeh R, Nouri J, Monavari M, Yaghmaeian K. Analysis of the health and environmental status of sterilizers in hospital waste management: a case study of hospitals in Tehran. Waste Manag Res. 2013;31(3):333–337. doi: 10.1177/0734242X12472706. [DOI] [PubMed] [Google Scholar]
- 13.Patil AD, Shekdar AV. Health-care waste management in India. J Environ Manag. 2001;63(2):211–220. doi: 10.1006/jema.2001.0453. [DOI] [PubMed] [Google Scholar]
- 14.Askarian M, Vakili M, Kabir G. Hospital waste management status in university hospitals of the Fars province, Iran. Int J Environ Health Res. 2004;14(4):295–305. doi: 10.1080/09603120410001725630. [DOI] [PubMed] [Google Scholar]
- 15.Bahrami H, Malakootian M, Mousavi Nasab SD, Jaafarzadeh N, Askarian M, Samadi S, et al. WITHDRAWN: an overview of the present status of hospital waste management in Kerman, Iran. J Infect Public Health. 2014. 10.1016/j.jiph.2014.07.007. [DOI] [PubMed]
- 16.Taghipour H, Mosaferi M. Characterization of medical waste from hospitals in Tabriz, Iran. Sci Total Environ. 2009;407(5):1527–1535. doi: 10.1016/j.scitotenv.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 17.Alagoz AZ, Kocasoy G. Determination of the best appropriate management methods for the health-care wastes in Istanbul. Waste Manag. 2008;28(7):1227–1235. doi: 10.1016/j.wasman.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 18.Da Silva CE, Hoppe AE, Ravanello MM, Mello N. Medical wastes management in the south of Brazil. Waste Manag. 2005;25(6):600–605. doi: 10.1016/j.wasman.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Mohamed LF, Ebrahim SA, Al-Thukair AA. Hazardous healthcare waste management in the Kingdom of Bahrain. Waste Manag. 2009;29(8):2404–2409. doi: 10.1016/j.wasman.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 20.Dehghani MH, Azam K, Changani F, Dehghani Fard E. Assessment of medical waste management in educational hospitals of Tehran university medical sciences. Iran J Environ Health Sci Eng. 2008;5(2):131–136. [Google Scholar]
- 21.Nemathaga F, Maringa S, Chimuka L. Hospital solid waste management practices in Limpopo Province, South Africa: a case study of two hospitals. Waste Manag. 2008;28(7):1236–1245. doi: 10.1016/j.wasman.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Insa E, Zamorano M, López R. Critical review of medical waste legislation in Spain. Resour Conserv Recycl. 2010;54(12):1048–1059. doi: 10.1016/j.resconrec.2010.06.005. [DOI] [Google Scholar]
- 23.Ananth AP, Prashanthini V, Visvanathan C. Healthcare waste management in Asia. Waste Manag. 2010;30(1):154–161. doi: 10.1016/j.wasman.2009.07.018. [DOI] [PubMed] [Google Scholar]