Abstract
Introduction
Late presentation, usually to the emergency centre (EC), is frequently reported among patients with chronic kidney disease (CKD) in resource-limited settings, and is known to be associated with poor outcomes. This study aims to describe the pattern of EC presentation of adults with CKD in Southwest Nigeria.
Methods
This was a prospective observational study of 158 consecutively presenting CKD patients at the EC of two tertiary hospitals in Southwest Nigeria. Patients 18 years of age or older who were admitted into the EC at either study site with an admitting diagnosis of CKD and who consented to participate in the study were recruited. Socio-demographic characteristics, primary reason(s) for admission into the EC, requirement for dialysis, as well as the indication for dialysis were documented. The patients were followed-up for the duration of their stay in the EC and the outcome of EC admission documented.
Results
Overall, 54 (34.2%) were females, median age was 49 years and 74.1% were not known to have CKD prior to EC admission. The commonest indications for admission into the EC were uraemia, sepsis and hypertensive crisis, with 73.4% of the patients having at least one indication for dialysis at EC admission. The commonest indications for dialysis were uraemia, marked azotaemia and acute pulmonary oedema. The median time to first session of dialysis was 48 h and 24.1% of patients who required dialysis were not dialysed. Death during the period of EC admission occurred in 14 (8.9%) patients all of whom were not previously known to have CKD.
Discussion
There is a large pool of undiagnosed CKD among the general population. In many of these, the diagnosis will likely be made only when they present to the EC with complications. Late diagnosis is associated with worse outcomes.
Keywords: Chronic Kidney Disease, Late Presentation, Emergency Centre in the Article Info Section
African relevance
-
•
There is a lack of awareness of chronic kidney disease and its consequences amongst the general African population.
-
•
The first nephrology contact for many African chronic kidney disease patients appears to be the emergency centre.
-
•
Accessible renal care is inaccessible to many African chronic kidney disease patients.
Introduction
Late presentation is often reported among patients with chronic kidney disease (CKD) and has been variously defined as time between first contact with nephrologists and first dialysis of less than eight weeks [1], 90 days [2], [3], [4], [5], [6], and four months [7], [8], [9]. It has been suggested that the term “late referral” be applied to patients whose interval between first nephrologists’ contact and first dialysis is between one to three months, and the term “ultra late referral” be used for patients who start dialysis within one month of being seen by a nephrologist [10]. Nephrologists generally use the term “crashlander” when referring to patients presenting with advanced CKD requiring dialysis who weren’t previously under the care of a nephrologist [11]. Crashlanders frequently present at the emergency centre (EC) with peculiar requirements and management challenges which ultimately result in poorer outcomes [1], [3], [6], [7], [9], [12]. Wolfe et al. [13] recently coined the term chronic kidney disease presenting acutely (CKDPA), and suggested its use in describing patients with CKD who require dialysis within one week of their emergency presentation. Wolfe and co-workers consider this group of CKD patients a distinct subset under the “ultra late referrals” group.
Progressive CKD is often clinically silent or cause only vague symptoms until late in its course. It can however be readily detected by relatively inexpensive screening tools, such as urine dipstick testing and measurement of serum creatinine concentration. Despite this, late presentation, usually to the EC, is particularly common among CKD patients in resource-limited settings [14], where factors such as traditional beliefs about the cause(s) of disease and limited access to specialist care combine to result in poor health-seeking behaviour. In our practice experience, the first contact majority of patients with CKD have with a nephrologist is in the EC. Despite this however, there is genuine paucity of data on the acute presentation of patients with CKD. This is in contrast to the widely documented acute presentation of several other medical conditions. This study aims to describe the acute presentation of adult patients with CKD, by documenting the presentation patterns and outcomes of patients managed at the EC of two tertiary healthcare facilities located in the southwestern region of Nigeria.
Methods
This was a prospective observational study involving 158 consecutively presenting patients with CKD conducted at the EC of two tertiary care hospitals, one each in Lagos and Ondo states, both in Southwest Nigeria. Lagos is a cosmopolitan state, which according to the last official national census figures, has a population of about 9,200,000 people [15]. The state has two main mutlidisciplinary, tertiary care hospitals, one of which is the study site in the state. The Lagos study site is staffed by four consultant nephrologists who are primarily responsible for the care of patients with kidney disease. Ondo state on the other hand, is a semi-urban state with a population of 3,440,000 people [15]. The state has one main mutlidisciplinary tertiary care hospital, and it is the study site in the state. The hospital is staffed by two consultant nephrologists who are primarily responsible for the care of patients with kidney disease.
Both study sites run similar protocols for admitting adult patients into the hospital via the EC. This protocol can be summarised as follows:
-
1.
All patient’s presenting to the EC are initially attended to by EC staff.
-
2.
Individuals with minor acute presentations are treated by EC staff and discharged.
-
3.
Those who are deemed to require further evaluation (including laboratory tests and additional specialist review) are admitted into a designated observation unit within the EC.
-
4.
Once the results of laboratory tests become available (usually within two to six hours), the patients are reviewed by the appropriate specialty unit while still in the EC.
-
5.The specialty unit:
-
a)Determines whether or not the patient requires in-hospital care.
-
b)Establishes the patient’s diagnosis.
-
c)Determines whether the patient requires out-patient care, “short-term” in-hospital care (usually not exceeding a 48–72 h) which may be provided in the EC, or “longer-term” in-hospital care for which the patient is admitted into a dedicated ward in the hospital.
-
d)Documents a definitive plan for the management of the patient.
-
a)
-
6.
All patients requiring dialysis are offered the procedure. However, because of the out-of-pocket nature of healthcare financing, the timing of dialysis is determined by ability to pay for the procedure.
-
7.While awaiting dialysis, interventions to address life-threatening complications of CKD are instituted, such as:
-
a)Intravenous glucose/insulin infusion and intravenous calcium gluconate for patients with serum potassium concentration above 6 mmol/L.
-
b)Oral or intravenous sodium bicarbonate therapy for patients with serum bicarbonate concentrations below 15 mmol/L.
-
c)Intranasal oxygen therapy and high-dose intravenous loop diuretics for patients with pulmonary oedema.
-
a)
-
8.
Patients are generally not expected to remain in the EC beyond 72 h.
All patients admitted into the EC at either study site who, following review by the nephrologist, had an admitting diagnosis that included any of the following phrases: “chronic kidney disease”, “chronic renal failure” or “end-stage renal disease”, were identified and reviewed for eligibility for inclusion in the study. Those who were 18 years of age or older, and consented to participate in the study were recruited. Patients with a diagnosis of acute kidney injury were excluded. The study protocol was approved by the Health Research Ethics Committee (HREC) of the Lagos University Teaching Hospital (Ref No: ADM/DCST/HREC/APP/1552). Recruitment into the study took place over a twelve month period between 1st January 2014 and 31st December 2014.
Information, including the socio-demographic characteristics, diagnosis at presentation to the EC, primary reason(s) for admission into the EC and presence of symptoms suggestive of uraemia, were retrieved from the study participants using a structured interviewer administered questionnaire. Results of laboratory investigations conducted at the time of admission into the EC, whether or not the patient required dialysis, as well as the indication(s) for dialysis, were extracted from the patients’ hospital records. Each patient was followed-up for the duration of their stay in the EC and the outcome of the EC admission was documented. The patient’s diagnosis at the time of admission, indication for hospital admission, need for dialysis and indication for dialysis were as documented in patients’ records by the nephrologists at the study site.
For the purposes of this study, the term “admitted to the EC” is used to describe the patient’s admission into the observation unit of the EC, while “admitted into the hospital” refers to when a patient is admitted into a dedicated ward of the hospital. Severe azotaemia refers to patients with serum urea concentrations above 20 mmol/L, but who have no symptoms of uraemia, while uraemia refers to severe azotaemia associated with symptoms such as nausea, vomiting, hiccups, altered consciousness or seizures. Time to first session of dialysis was the duration between documentation of the need for dialysis and when the patients were first dialysed. Patients were known to have CKD if they had been reviewed at least once by a nephrologist or had been informed by any other healthcare provider that they had kidney disease prior to onset of the symptoms that necessitated the current EC presentation.
Data obtained was analysed using Epi Info™ statistical software (United States Centers for Disease Control and Prevention), version 7.2.0.1. Continuous variables are presented as medians and interquartile range, while categorical variables are presented as percentages.
Results
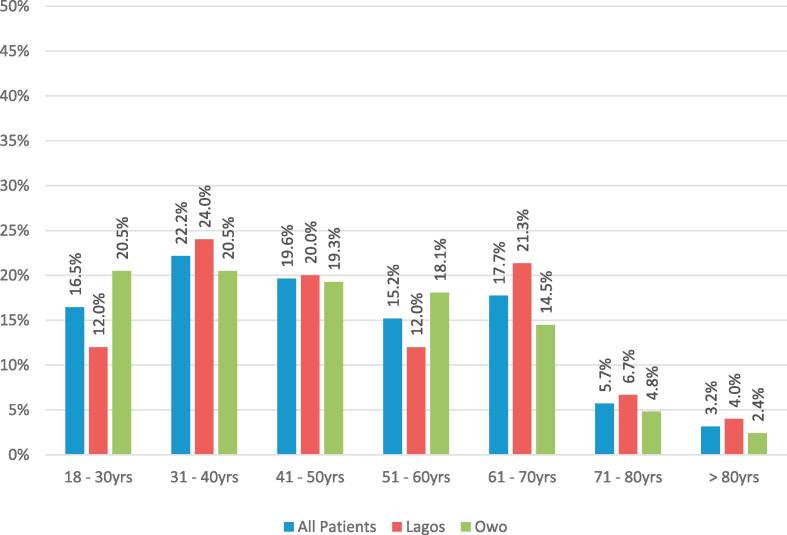
Of the 158 patients recruited into the study, 83 (52.5%) were recruited at the study site in Owo, while 75 (47.5%) were recruited at the study site in Lagos. Overall, 54 (34.2%) of the study participants were female. The median age of the study population was 49 years (range 20–95), with 58.3% of the study population being 50 years of age or younger. The peak age range of the study population was between 31 and 40 years (Fig. 1). Compared to female study participants, male participants had a slightly higher median age, estimated monthly income, haemoglobin concentration, and serum creatinine. Also, a higher proportion of males were known to have CKD prior to presentation at the EC.
Fig. 1.
Age range distribution of the study population.
Table 1 shows the baseline sociodemographic, clinical and laboratory parameters of the study population stratified according to study site. A lower proportion of patients at Owo were female and were previously known to have CKD. Patients at Owo also had a lower average monthly income. They, however, had much higher serum urea and creatinine concentrations.
Table 1.
Baseline characteristics of the study population stratified according to location of the emergency centre.
| Characteristics | All Patients n = 158 |
Lagos n = 75 (47.5%) |
Owo n = 83 (52.5%) |
|---|---|---|---|
| Median Age | 49 [32–62] | 49 [32–64] | 48 [32–60] |
| Female Gender | 34.2% | 37.3% | 31.3% |
| Median Monthly Income | aN17,500 ($57.2) [10,000–30,000] | aN20,000 ($65.4) [15,000–30,000] | aN15,000 ($49.0) [10,000–20,000] |
| Previously Known CKD | 25.9% | 32.0% | 20.5% |
| Median SBP (mmHg) | 160 [138–183] | 158 [130–181] | 160 [140–190] |
| Median DBP (mmHg) | 100 [80–110] | 91 [80–110] | 100 [80–110] |
| Median Hb Conc (g/dL) | 8.0 [6.3–9.5] | 8.5 [7.3–10.3] | 7.7 [6.1–9.0] |
| Median Serum Na+ (mmol/L) | 131 [128–136] | 134 [126–140] | 130 [128–134] |
| Median Serum K+ (mmol/L) | 4.9 [4.2–5.8] | 4.6 [3.5–5.8] | 5.0 [4.3–5.8] |
| Median Serum Cl- (mmol/L) | 100 [95–107] | 102 [94–108] | 100 [95–105] |
| Median Serum HCO3− (mmol/L) | 19 [16–23] | 20 [13–24] | 19 [18–21] |
| Median Serum Urea (mmol/L) | 27.1 [14.0–40.0] | 16.3 [5.4–38.9] | 31.9 [23.0–41.3] |
| Median Serum Creatinine (µmol/L) | 815 [440–1539] | 712 [327–1328] | 920 [500–1770] |
| Required Dialysis | 73.4% | 64.0% | 81.9% |
CKD = chronic kidney disease; SBP = systolic blood pressure; DBP = diastolic blood pressure; Hb Conc = hemoglobin concentration; Na+ = Sodium; K+ = Potassium; Cl = chloride; HCO3− = serum bicarbonate concentration; N = Naira; $ = Unites States Dollar.
Currency conversion rate $1 = N306 (Central Bank of Nigeria official dollar exchange rate as of 12th May 2017: available at http://www.cbn.gov.ng/rates/exchratebycurrency).
Table 2 shows the indications for admission into the EC among the study participants. The commonest indication for admission into the EC was uraemia. This was followed by sepsis, hypertensive crisis and marked azotaemia. Severe anaemia, symptomatic heart failure and stroke were the other more common indications for admission. Overall, 73.4% of the patients (64% in Lagos and 81.9% in Owo) had at least one indication for dialysis at the time of admission into the EC.
Table 2.
Indications for admission into the emergency centre (in %).
| All Patients | All Patients | Lagos | Owo |
|---|---|---|---|
| Acute Pulmonary Oedema | 4.5 | 4.1 | 4.9 |
| Dialysis Disequilibrium | 0.7 | 1.4 | 0.0 |
| Symptomatic Heart Failure | 7.1 | 4.1 | 9.9 |
| Hyperglycaemia | 2.6 | 5.4 | 0.0 |
| Hypertensive Crisis | 12.9 | 4.1 | 21.0 |
| Hypoglycaemia | 1.9 | 1.4 | 2.5 |
| Hypotension | 0.7 | 0.0 | 1.2 |
| Marked Azotemia | 10.3 | 17.6 | 3.7 |
| Relief of Urinary Obstruction | 3.2 | 2.7 | 3.7 |
| Sepsis | 16.8 | 20.3 | 13.6 |
| Severe Anaemia | 9.7 | 5.4 | 13.6 |
| Severe Hyperkalemia | 0.7 | 1.4 | 0.0 |
| Stroke | 5.8 | 9.5 | 2.5 |
| Upper Gastrointestinal Bleeding | 1.9 | 4.1 | 0.0 |
| Uraemia | 21.3 | 18.9 | 23.5 |
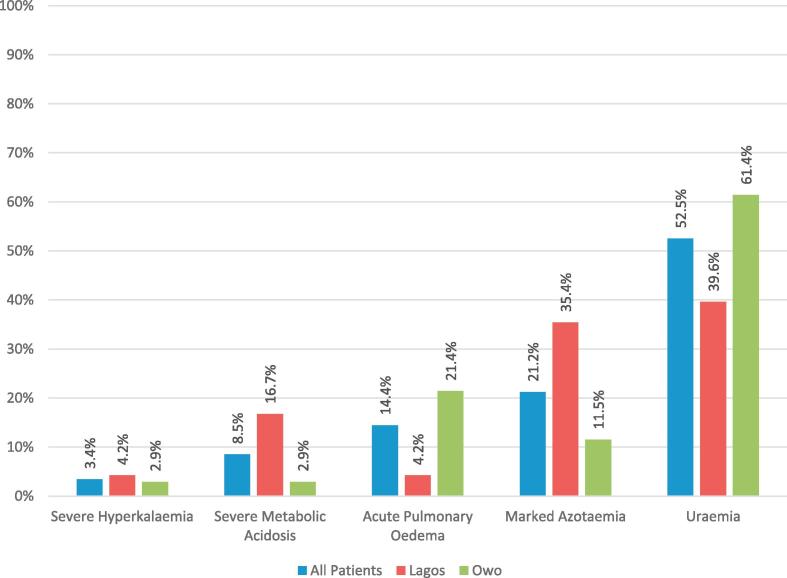
Fig. 2 shows the indications for dialysis in the study population. The most frequent indication for dialysis was uraemia. This was followed by marked azotaemia, and then acute pulmonary oedema.
Fig. 2.
Indications for dialysis in the study population.
Table 3 shows a comparison of the clinical and laboratory parameters of patients who were known to have CKD prior to presentation at the EC with those who were not.
Table 3.
Comparison of clinical and laboratory parameters of patients who were previously known to have CKD with those who were not.
| Characteristics | All patients | Previously known to have CKD | Not Previously known to have CKD |
|---|---|---|---|
| 158 | 41 (25.9%) | 117 (74.1%) | |
| Median Age (years) | 49 | 46 [34–42] | 50 [32–60] |
| Female Gender | 34.2% | 29.3% | 35.9% |
| Median Monthly Income | aN17,500 ($57.20) [10,000–30,000] | aN25,000 ($81.70) [10,000–50,000] | aN15,000 ($49.02) [11,500–22,500] |
| Median Systolic BP (mmHg) | 160 [138–183] | 169.5 [149.5–192] | 160 [130–180] |
| Median Diastolic BP (mmHg) | 100 [80–110] | 100 [81.5–112] | 98 [80–110] |
| Median Hb Conc (g/dL) | 8.0 [6.3–9.5] | 7.7 [6.2–9.0] | 8.3 [6.3–9.7] |
| Median Serum Na+ (mmol/L) | 131 [128–136] | 132.5 [125–137] | 131 [128–136] |
| Median Serum K+ | 4.9 [4.2–5.8] | 5.1 [4.2–6.3] | 4.8 [4.1–5.7] |
| Median Cl (mmol/L) | 100 [95–107] | 100 [94–107] | 101 [95–107] |
| HCO3− (mmol/L) | 19 [16–23] | 19.5 [16–21.5] | 19 [16–23] |
| Median Serum Urea (mmol/L) | 27.1 [14.0–40.0] | 21.7 [11.9–38] | 28.2 [15.8–41.3] |
| Median Serum Creatinine (µmol/L) | 815 [426–1539] | 850 [500–1589] | 810 [416–1522] |
| Required Dialysis | 73.4% | 80.5% | 70.9% |
| Patient Dialyzed | 75.9% | 87.9% | 71.1% |
| Median time to first session of dialysis (Hours) | 48 [25–72] | 48 [24–72] | 48 [27–72] |
CKD = chronic kidney disease; SBP = systolic blood pressure; DBP = diastolic blood pressure; Hb Conc = hemoglobin concentration; Na+ = Sodium; K+ = Potassium; Cl = chloride; HCO3− = serum bicarbonate concentration; N = Naira; $ = Unites States Dollar.
Currency conversion rate $1 = N306 (Central Bank of Nigeria official dollar exchange rate as of 12th May 2017: available at http://www.cbn.gov.ng/rates/exchratebycurrency).
Patients who were previously known to have CKD had higher monthly incomes. Also a higher proportion of patients previously known to have CKD required dialysis at the time of presentation. However, among patients who required dialysis, a lower proportion of patients who were not previously known to have CKD received dialysis. The median time from presentation to the first session of dialysis was however similar in both groups (48 h).
Of the 158 study participants, three (1.9%) were discharged home from the EC following treatment, 126 (79.7%) required further in-hospital care and were admitted into the medical wards, eight (5.1%) were transferred to a healthcare facility other than the one they presented at, seven (4.4%) discharged themselves against medical advised and 14 (8.9%) died in the EC. All deaths occurred among patients who were not known to have CKD prior to presentation at the EC. Mortality was also higher in males compared with females (11.5% vs 3.7%) and in patients who were admitted at the Owo compared with those who were admitted at the Lagos study site (10.8% vs 6.6%). Of the 14 patients who died in the EC, 13 (92.9%) were patients who had indications for dialysis and all 13 received at least one session of dialysis.
Discussion
The results of this study suggest that majority of CKD patients presenting to the EC in our practice setting have advanced disease when one considers the incident serum urea, creatinine and haemoglobin concentrations. In fact, over 70% could be considered as belonging to Wolfe et al.’s subset of ultra-late referrals labelled CKDPA, having not been previously known to have CKD and requiring dialysis at the time of admission into the EC. The proportion of CKDPA patients in this study is much higher than those reported from developed countries [8], [16]. This marked disparity is likely a reflection of differences in both patient and health system characteristics. Navaneethan et al. [17] highlighted in a systematic review that lower socioeconomic status and educational levels, lack of referring physician knowledge about the appropriate timing of referral, absence of communication between referring physicians and nephrologists, and dialysis care delivered at tertiary medical centers were all characteristics associated with late referral of patients with CKD. These factors are prevalent in resource-limited settings such as ours.
The spectrum of clinical indications for EC admission in the study population was wide, with uraemia, sepsis and marked azotaemia being the most common individual indications. However, three categories of conditions account for approximately 80% of all indications for EC admission; direct complications of severe renal failure, cardiovascular disease and sepsis. Direct complications of severe renal failure (uraemia, marked azotaemia, pulmonary oedema, severe hyperkalemia and severe anaemia) were responsible for 36.6% admissions, cardiovascular diseases (heart failure, hypertensive crisis, stroke and hypotension) contributed to 26.5%, while sepsis was responsible for 16.8% of admissions. The preponderance of complications of CKD as an indication for EC admission in this study population is likely a direct effect of late presentation to care. As a result of late presentation, the patients had missed out on interventions that prevent and/or address many of the complications that develop much earlier in the course of CKD. Similarly, the high rates of cardiovascular morbidity in the study is in keeping with the established fact that CKD is an independent risk factor for cardiovascular disease [18], [19], [20].
As alluded to earlier, over 70% of the patients required dialysis at the time of EC admission. Despite this, about 25% of patients who required dialysis could not be dialysed while in the EC mainly because of inability to pay for the procedure. Even among those who received at least one session of dialysis in the EC, there was generally a delay of about 48 h in instituting dialytic therapy. This is a sad but entirely understandable commentary on the state of access to renal care in the country. Currently, the cost of a single session of haemodialysis (the more commonly available dialysis modality in the country) is more than twice the national monthly minimum wage, and peritoneal dialysis may actually cost more. This, combined with out-of-pocket payment for healthcare in an economy that is largely subsistence in nature, makes it unsurprising that a significant proportion of patients who required dialysis were unable to access it, and that those who were dialysed experienced significant delay before undergoing the procedure. This delay was probably as a result of the need to raise funds required to pay for the procedure.
There was a disparity in EC mortality between patients who were known to have CKD prior to admission into the EC and those that were not. All EC mortality occurred among patients who were not known to have CKD prior to EC admission. EC mortality appeared to be directly related to this “crashlander” status of the patients rather than degree of renal impairment or an inability to access dialysis. Two findings support this view of ours; firstly, surrogate markers of severity of CKD were either similar between the two groups or slightly better among patients who were not previously known to have CKD, and secondly, none of the patients who required dialysis but could not be dialysed died in the EC. This further reaffirms the widely documented finding that CKD patients who present as “crashlanders” are more likely to have poor outcomes [1], [3], [6], [7], [9], [12]. One must however also consider the possibility that the observed differences in income between the two groups may have influenced mortality.
It is also noteworthy that mortality was higher among males. The reason for this gender difference in EC mortality is unclear since there were no major differences in baseline clinical or laboratory parameters between male and female patients in the study. In fact, the expectation was that EC mortality would be lower among males, as a higher proportion of male patients in the study were known to have CKD prior to admission into the EC. However, male gender has previously been reported to be associated with worse patient and renal outcomes in CKD [21], [22], [23].
We also noted differences in the clinical and laboratory parameters, requirement and indications for dialysis, as well as outcomes between patients at the two study sites. Patients at Owo appeared to have more severe disease at EC admission as evidenced by indicators such as lower haemoglobin concentration, and higher serum urea and creatinine concentrations, as well as a higher proportion of patients requiring dialysis. EC mortality was also higher among patients at Owo. Some of these differences likely reflect inherent differences in socio-demographic characteristics in the populations of both states. Lagos is the economic capital of the country with a more cosmopolitan population whose per capita income is significantly higher than is the case in Ondo state. Others may reflect differences in practice patterns amongst the nephrologists at the two study sites. The higher EC mortality however is likely due to the combination of a higher proportion of male participants and “crashlanders” at the Owo study site.
One limitation of our study is that because we recruited only patients whose admitting diagnosis included the phrases “chronic kidney disease”, “chronic renal failure” or “end-stage renal disease”, it is possible that certain patients with CKD but whose admitting diagnosis didn’t include any of these phrases would have been inadvertently excluded.
In conclusion, our findings suggest that there is a large pool of undiagnosed CKD in the general population in Southwest Nigeria. In many of these patients, the diagnosis of CKD will likely be made only when they present to the EC with complications of CKD. Late presentation to care is associated with adverse outcomes.
Action in the form of increased public health campaigns, especially at schools and worship centers, is needed to increase awareness about CKD. Also, as was done recently for diabetes in the country, a deliberate and mandatory policy of screening for all patients above the age the age of 25 years for CKD in public hospitals would increase detection rates for CKD in Nigeria.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
The results of this study were shared with members of staff of the nephrology units and emergency centre at both the Lagos University Teaching Hospital and Federal Medical Center Owo through an informal presentation.
Authors’ contributions
BTB conceived the original idea of the study. BTB and OEO developed the study design and methods, including the data collection instruments. OFO and AAA collected the study data. BTB carried out analysis of the data. BTB and OFO produced the initial draft of the manuscript. OEO and AAA revised the draft manuscript critically for important intellectual content. BTB, OEO, OFO and AAA approved the final version of the manuscript that was submitted.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Schwenger V., Morath C., Hofmann A. Late referral: a major cause of poor outcome in the very elderly dialysis patient. Nephrol Dial Transplant. 2006;21:962–967. doi: 10.1093/ndt/gfk030. [DOI] [PubMed] [Google Scholar]
- 2.Ellis P., Reddy V., Bari N. Late referral of end-stage renal failure. Q J Med. 1998;91:727–732. doi: 10.1093/qjmed/91.11.727. [DOI] [PubMed] [Google Scholar]
- 3.Goransson L., Bergrem H. Consequences of late referral of patients with end-stage renal disease. J Intern Med. 2001;250:154–159. doi: 10.1046/j.1365-2796.2001.00869.x. [DOI] [PubMed] [Google Scholar]
- 4.Avorn J., Winkelmayer W.C., Bohn R.L. Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J Clin Epidemiol. 2002;55:711–716. doi: 10.1016/s0895-4356(02)00415-8. [DOI] [PubMed] [Google Scholar]
- 5.Goncalves E.A., Andreoli M.C.C., Watanabe R. Effect of a temporary catheter and late referral on hospitalization and mortality during the first year of haemodialysis treatment. Artif Organs. 2004;28:1043–1049. doi: 10.1111/j.1525-1594.2004.00016.x. [DOI] [PubMed] [Google Scholar]
- 6.Dogan E., Erkoc R., Sayarlioglu H. Effects of late referral to a nephrologist in patients with chronic renal failure. Nephrology. 2005;10:516–519. doi: 10.1111/j.1440-1797.2005.00433.x. [DOI] [PubMed] [Google Scholar]
- 7.Arora P., Obrador G.T., Ruthazer R. Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol. 1999;10:1281–1286. doi: 10.1681/ASN.V1061281. [DOI] [PubMed] [Google Scholar]
- 8.Roderick P., Jones C., Tomson C. Late referral for dialysis: improving the management of chronic renal disease. Q J Med. 2002;95:363–370. doi: 10.1093/qjmed/95.6.363. [DOI] [PubMed] [Google Scholar]
- 9.Kazmi W.H., Obrador G.T., Kahn S.S. Late nephrology referral and mortality among patients with end-stage renal disease: a propensity score analysis. Nephrol Dial Transplant. 2004;19:1808–1814. doi: 10.1093/ndt/gfg573. [DOI] [PubMed] [Google Scholar]
- 10.Obiolo C.I., Ofili E.O., Quarshie A. Ultralate referral and presentation for renal replacement therapy: socio-economic implications. Am J Kidney Dis. 2005;46:881–886. doi: 10.1053/j.ajkd.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Ali I. Caring for the “crash-landers”. BMJ. 2017;17(356):j229. doi: 10.1136/bmj.j229. [DOI] [PubMed] [Google Scholar]
- 12.Kemp K.V., Mikhail A. Starting dialysis in south west wales: does inpatient status affect outcome? Nephrol Dial Transplant. 2015;30(Suppl 3):iii604–iii630. [Google Scholar]
- 13.Wolfe M., Almond A., Robertson S., Donaldson K., Isles C. Chronic kidney disease presenting acutely: presentation, clinical features and outcome of patients with irreversible chronic kidney disease who require dialysis immediately. Postgrad Med J. 2010;86(1017):405–408. doi: 10.1136/pgmj.2009.078956. [DOI] [PubMed] [Google Scholar]
- 14.Awobusuyi J.O., Amira C.O., Umeizudike T., Babafemi J.O., Shoyinka F., Ojuroye J.O. Lagos renal registry: an audit of renal replacement therapy in five public dialysis units in Lagos Metropolis. Trop J Nephrol. 2011;6(2):97–105. [Google Scholar]
- 15.National Population Commission: Official Results of the 2006 Population Cencus. http:// www.population.gov.ng/index.php/state-population. [Last accessed on 10th April 2017].
- 16.Danish Nephrology Registry, Annual Report 2013. Available from: http://www.Nephrology.dk. [Last accessed on 24th April 2017].
- 17.Navaneethan S.D., Aloudat S., Singh S. A systematic review of patient and health system characteristics associated with late referral in chronic kidney disease. BMC Nephrol. 2008;25(9):3. doi: 10.1186/1471-2369-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ene-Iordache B., Perico N., Bikbov B., Carminati S., Remuzzi A. Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health. 2016;4(5):e307–e319. doi: 10.1016/S2214-109X(16)00071-1. [DOI] [PubMed] [Google Scholar]
- 19.Lim C.C., Teo B.W., Ong P.G., Cheung C.Y., Lim S.C. Chronic kidney disease, cardiovascular disease and mortality: a prospective cohort study in a multi-ethnic Asian population. Eur J Prev Cardiol. 2015;22(8):1018–1026. doi: 10.1177/2047487314536873. [DOI] [PubMed] [Google Scholar]
- 20.Weiner D.E., Tighiouart H., Amin M.G., Stark P.C., MacLeod B. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol. 2004;15(5):1307–1315. doi: 10.1097/01.asn.0000123691.46138.e2. [DOI] [PubMed] [Google Scholar]
- 21.Eriksen B.O., Ingebretsen O.C. The progression of chronic kidney disease: a 10-year population-based study of the effects of gender and age. Kidney Int. 2006;69(2):375–382. doi: 10.1038/sj.ki.5000058. [DOI] [PubMed] [Google Scholar]
- 22.Neugarten J., Acharya A., Silbiger S.R. Effect of gender on the progression of nondiabetic renal disease: a meta-analysis. J Am Soc Nephrol. 2000;11:319–329. doi: 10.1681/ASN.V112319. [DOI] [PubMed] [Google Scholar]
- 23.Seliger S.L., Davis C., Stehman-Breen C. Gender and the progression of renal disease. Curr Opin Nephrol Hypertens. 2001;10:219–225. doi: 10.1097/00041552-200103000-00010. [DOI] [PubMed] [Google Scholar]