Abstract
Introduction
The implementation of a triage system is a vital step in improving the functioning and patient flow of the emergency centre in a rural district hospital. The South African Triage Scale (SATS) is a well validated and reliable tool used widely in South Africa and other low- and middle-income countries. This study aims to assess the validity of the SATS in a rural district hospital context.
Methods
This is a cross-sectional study. All patients presenting to the Zithulele Hospital emergency centre from 1 October 2015 to 31 December 2015 were triaged using the SATS system, routinely collected data was used to determine the correlation between assigned acuity and outcome to determine rates of under- and over-triage. Patient demographics were collected and waiting times were compared to existing standards of the SATS tool.
Results
Of the 4002 patients presenting to the emergency centre during the study period, 2% were triaged as emergency patients, 15% as very urgent, 38% as urgent and 45% as routine. The assigned acuities correlate well with outcome (f = 0.37; p < 0.0001) and an acceptable rate of over-triage (49%) and under-triage (9%) was found. Waiting time targets were poorly achieved with only 49% of emergency, 23% very urgent, 46% urgent and 69% routine patients seen within ideal target times.
Discussion
The SATS is a valid tool to implement in a rural district emergency centre. Strict waiting time goals may not be achievable in this setting without structural and resource allocation changes to allow for improvements in the surge capacity of staff to manage urgent and emergency patients.
Keywords: South African Triage Scale, SATS, Triage, Emergency department, Waiting times, Rural in the article info section
African relevance
-
•
Triage systems may be successfully implemented in emergency centres run by general practitioners without specialist input.
-
•
Implementing objective triage is an important part of the development of emergency medicine in low-resource settings.
Introduction
The World Health Organization estimates that a significant proportion of death and disability in low- and middle-income countries (LMIC) could be prevented by the establishment of comprehensive and effective emergency care systems [1]. Initial triage and emergency care provision are poorly done in most LMICs where demand for emergency care frequently outstrips the available material and human resources [2].
In South Africa, district hospitals fulfill a crucial role in being the first point of doctor-led emergency care and serve as a ‘bridge’ between the primary health care system and the more specialised secondary and tertiary level hospital-based care. District hospital emergency centres (EC) are characteristically a 24-hour service, run by generalist medical officers, and are expected to manage any presenting emergency competently. After-hours laboratory and radiological service are not always available.
The South African Triage Scale (SATS), formerly the Cape Triage Score, comprises a five-tiered acuity (level of severity of illness) score derived from a combination of a list of discriminators (presentation, mechanism of injury and pain) and a physiology based score known as the Triage Early Warning Score (TEWS) [3]. The SATS also allows for the opinion of the senior health care provider to override any acuity score. In this way, clinical judgement acts as a safety net for patients who the system triages incorrectly. Acuity scores are colour coded as red (emergency), orange (very urgent), yellow (urgent), green (routine) and blue (deceased).
The Cape Triage Group [3] has, since it was developed in 2004, been widely implemented in South Africa as well as other LMICs. The SATS has not yet been evaluated to the same extent as other internationally recognised triage systems like the Canadian triage score, Manchester Triage score or the Australasian triage score [11]. In South Africa, the SATS has been evaluated at two urban regional hospitals [10], [16], one rural regional hospital [9] and one district hospital [8]. The performance of the SATS in paediatric patients was evaluated in a multi-centre study involving community health centres and regional and tertiary hospitals [14]. The SATS has also been implemented and assessed at a teaching hospital in Ghana [4], and referral hospitals in Somaliland [5] and Malawi [6]. Further afield it has been evaluated in Pakistan [7], and more recently in Haiti and Afghanistan [17]. Clinical evaluation of the SATS was used in four of the above studies [5], [9], [14], [17], while the rest were evaluated in non-clinical settings, using either triage paper reviews or vignettes [4], [6], [7], [8], [10]. The SATS has not been validated in the South African rural district hospital setting.
The validity of a triage score is a measure of how well the scored acuity correlates with the true acuity of the patient. The impossibility of determining a true acuity makes validation of a triage system inherently problematic and there is no gold standard for identifying the true acuity of a patient [12]. The majority of validation studies have used either the utilisation of resources (time or monetary expense per patient) or the disposition of patients from the emergency centre (i.e. admission, discharge, transfer or death) as a proxy measure for actual acuity [11]. For this study, disposition of patient from the EC was used to ensure our data is comparable to that of the majority of other SATS validation studies [5], [9], [14], [17]. There are inconsistencies in how the SATS has been validated in previous studies in clinical settings with regard to which categories constitute high acuity (Red only [17], Red and Orange [5], [9] or Red, Orange and Yellow [14]), as well as the outcomes used to confirm high acuity (admission [14], [17], admission and death [5], [9]); Low acuity is uniformly regarded as Green and outcome confirmed as discharge.
The decision to regard both red (patients needing immediate doctor evaluation) and orange (patients needing evaluation within ten minutes) acuity patients as high acuity in this study was made following the precedent set by two clinical studies in the literature review set in Ngwelezane [9] and Somaliland [5].
The aim of this study was to assess if the SATS is a valid and practical tool in a rural district emergency centre. The objectives were:
-
•
To validate the SATS in a rural district hospital emergency centre.
-
•
To assess the ability of a rural district hospital emergency centre to meet the waiting time targets stipulated by the SATS.
Methods
Zithulele Hospital is a 147-bed district hospital set in the deeply rural Eastern Cape Province of South Africa serving a population of 130,000 people. It receives referrals from 14 primary level health care clinics and refers to a centre 85 km away. The emergency centre is staffed with five to six nurses and two doctors on weekdays (8 am–5 pm), and two to three nurses and one doctor after-hours and on weekends.
The outpatient building at Zithulele Hospital previously served both emergencies and scheduled follow-up patients, without discriminating between them. No formal triage system was in place to prioritise emergencies. The continuation of this informal system was deemed to be ineffective in objectively identifying urgent cases. The establishment of a triage system was necessary not only to identify high-risk patients but also to ensure prompt provision of emergency care to decrease preventable deaths, as recommended by the World Health Organization [1]. As part of a quality improvement process in June 2015, the outpatient building was divided into an outpatient follow-up section and an emergency intake section to streamline services. The SATS was identified as the preferred triage system for the South African context and was implemented as part of the change. Before implementation of the SATS, age-specific triage forms were designed for under three years; age three to twelve years; and over twelve years to correlate with age stratification used in the SATS. The EC nurses were given two one-hour training sessions on the SATS based on the standardised SATS training material which is freely available on the Emergency Medicine Society of South Africa website [18]. The training consisted of introduction to the concept of nurse-led triage and explanation of the use of the forms and the process which should be followed to assess patients’ acuities using the TEWS and SATS discriminators.
This was a cross-sectional study where all patients presenting to the emergency centre of Zithulele district hospital from 1 October 2015 to 31 December 2015 were included. All patients were triaged by nursing staff according to the SATS on pre-existing age specific triage forms, which were archived as hospital records. The time of triage, age, sex, referral source, TEWS score, discriminator, and final acuity were recorded by the triage nurse at the time of triage. If the final colour was changed in the EC by a senior healthcare professional, this was taken to be the final triage acuity, as opinion of the senior health care provider is the final step in the SATS process. The time seen, final diagnosis and outcome were recorded by the doctor during the consultation.
All triage forms for the study period were collected and evaluated by the investigators. The forms were correlated with the patient registry for that day to confirm the outcomes of patients where outcome was not recorded by the consulting doctor. Any forms without a recorded acuity were excluded. The information was recorded anonymously on an electronic data sheet using Microsoft Excel. Information collected included the patient’s age, sex, time of arrival/triage, TEWS score, discriminator used, final acuity, time seen by doctor and outcome.
Outcomes were recorded as admitted, discharged, transferred, or died. ‘Admitted’ were patients who left the EC to be admitted to one of the hospital wards. ‘Discharged’ were patients who left the EC to go home after being seen by a doctor. ‘Transferred’ were patients referred from the EC to a tertiary/specialist level hospital for further investigations and/or management. ‘Died’ were patients who died in the EC. These were then divided into two categories: namely, outcomes suggestive of a high acuity (admitted, transferred and died) and outcome suggestive of a low acuity (discharged). Patients who absconded were defined as patients who left the EC without being seen by a doctor or left against medical advice. Patients who absconded or whose outcomes were unknown were excluded from the final analysis.
A valid triage system correctly identifies the urgency with which a patient needs to be assessed (acuity). Over-triage is defined as non-urgent cases which are incorrectly classified as urgent. We have regarded over-triage in this study as the proportion of patients identified as red or orange by the SATS who were subsequently discharged. Under-triage is defined as urgent cases which are incorrectly classified as non-urgent, which has been regarded in this study as the proportion of patients identified as green by the SATS who were subsequently admitted, transferred or who died. The acceptable limits set by the American College of Surgeons Committee on Trauma of an under-triage rate of less than 10% and over-triage rate of 30–50% was used as a standard for this study [13]. This standard has been used for validation in other studies [5], [9], [14], [17].
For analysis, high acuity was considered as all patients triaged as red or orange. Patients triaged green were considered low acuity.
Correlation between acuity and outcome was assessed using the χ2 test and correlation coefficient was derived by Cramer’s V. Relative risk of an outcome suggestive of a high acuity in a patient triaged orange or red as compared to green was assessed by univariate analysis.
Ethics approval was obtained from the University of Cape Town Human Research Ethics Committee. Individual participant consent is usually not required for review of routine hospital records. Due to the prospective nature of the data collection, however, verbal consent was obtained from each participant by the nurse performing triage and was recorded on the triage form. This was done in consultation with the ethics committee.
Results
From 1 October to 31 December 2015, 4011 patients presented to the Zithulele Hospital EC. Eight patients were seen by a doctor without being assigned a triage acuity and one patient was dead on arrival (triaged blue). These cases were excluded from the data analysis.
Of the 4002 patients analysed, 359 (9%) patients were under three years of age, 422 (10.5%) patients were between three and twelve years of age, 3142 (78.5%) patients were over the age of twelve, and 79 (2%) of the patients’ ages were not recorded.
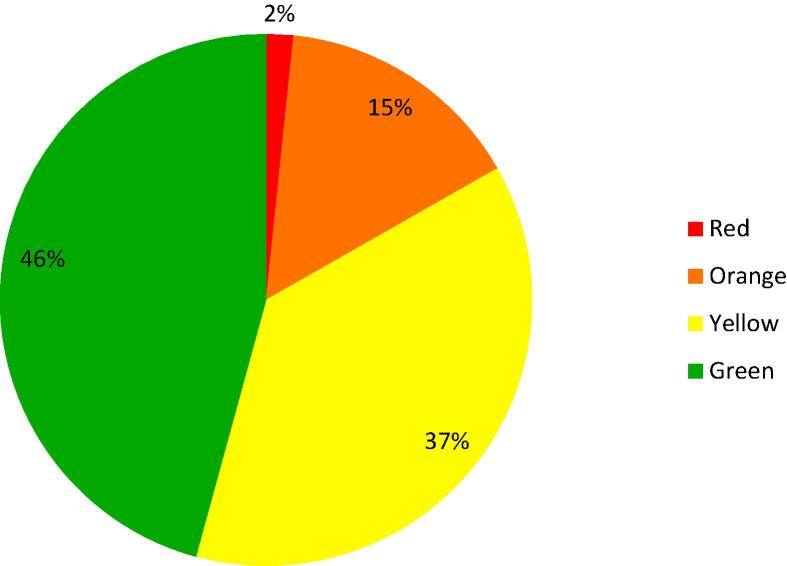
In total, 66 Red patients, 605 Orange patients, 1500 Yellow Patients, and 1831 Green patients were triaged and seen in the EC (Fig. 1). Twenty-seven patients were re-triaged by a senior healthcare provider in the EC after being assigned a triage colour by the triage nurse; six were assigned a higher acuity, and 21 were assigned a lower acuity.
Fig. 1.
SATS Acuities of patients presenting to Zithulele Hospital ED 1 October-31 December 2015 (n = 4002).
There were 798 (19.94%) admissions, 2901 (72.4%) discharges, 8 (0.19%) deceased, 94 (2.34%) transfers, 156 (3.89%) absconders, and 45 untraceable outcomes. Of the eight patients who died in the EC, one patient was under three years, six patients were adults, and one patient did not have a recorded age; two were triaged as red, three as orange, two as yellow and one triaged green.
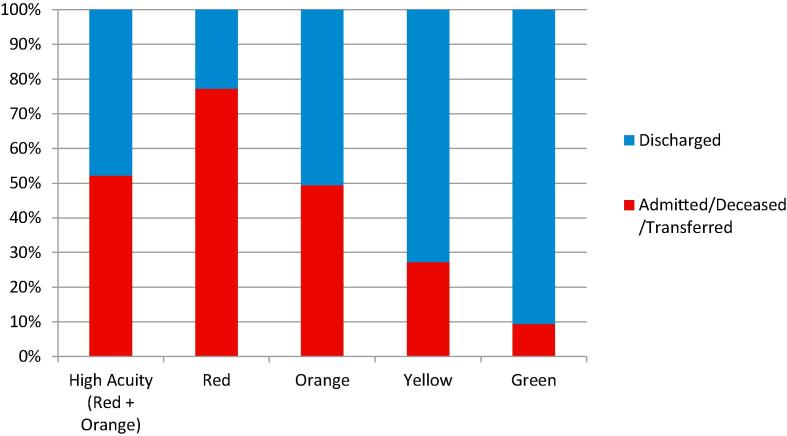
These outcomes, i.e. admitted, transferred, deceased, and discharged, were assessed in relation to patients’ assigned acuity. 77.3% of red patients had an outcome suggestive of high acuity as compared to 49.4% for orange, 27.3% for yellow and 9.4% for green (Fig. 2). Inversely green patients had an outcome suggestive of low acuity in 90.6%. Unknown outcomes and absconded patients were not included in the assessment of true acuity.
Fig. 2.
Outcomes by SATS acuities (n = 3801).
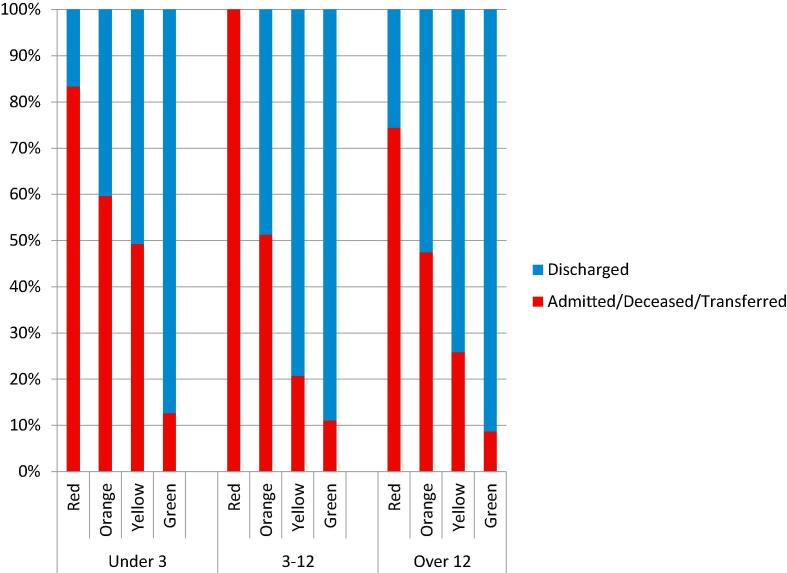
A moderately positive correlation (f = 0.37; p < 0.0001) exists between the triage category and outcome. The unadjusted relative risk of admission, transfer or death was 5.54 (95%CI 4.7–6.54; p < 0.0001) for patients triaged as red or orange when compared to patients triaged as green. An over-triage rate (patients classified as red or orange by SATS who were subsequently discharged) of 47.8% and an under-triage rate (patients classified as green by SATS who were subsequently admitted, deceased or transferred) of 9.4% overall are both within the target range. Acuity, outcomes, over- and under-triage rates were stratified by age group and are demonstrated in Fig. 3 and Table 1.
Fig. 3.
Age-stratified outcomes by SATS acuity (n = 3729).
Table 1.
Age-stratified acuities and outcomes, over- and under-triage rates, and relative risks.
| Total number | Admitted/died/transferred | Discharged | Over-triage rate | Under-triage rate | Relative risk | |
|---|---|---|---|---|---|---|
| (95% CI) | ||||||
| <3 years | 348 | 133 | 215 | 36.5% | 12.7% | |
| Red + Orange | 74 | 47 | 27 | 5.01 (3.11–8.1) | ||
| p < 0.0001 | ||||||
| Green | 134 | 17 | 117 | 1 | ||
| 3–12 years | 405 | 84 | 321 | 42.2% | 11% | |
| Red + Orange | 45 | 26 | 19 | 5.23 (3.2–8.56) | ||
| p < 0.0001 | ||||||
| Green | 172 | 19 | 153 | 1 | ||
| >12 years | 2976 | 661 | 2315 | 50.3% | 8.7% | |
| Red + Orange | 521 | 259 | 262 | 5.7 (4.7–6.92) | ||
| p < 0.0001 | ||||||
| Green | 1355 | 118 | 1237 | 1 | ||
| Overall | 3801 | 900 | 2901 | 47.8% | 9.4% | |
| Red + Orange | 661 | 345 | 316 | 5.54 (4.7–6.54) | ||
| p < 0.0001 | ||||||
| Green | 1689 | 159 | 1530 | 1 | ||
CI, confidence interval
The overall average waiting time was 125 min. 67% of green patients, 46% of yellow, 23% of orange and 49% of red patients were seen by doctors within the target times (Table 2).
Table 2.
Achievement of waiting time targets.
| Green | Yellow | Orange | Red | |
|---|---|---|---|---|
| Target Time | <4 h | <1 h | 10 min | Immediate |
| % seen within target time | 69% | 46% | 23% | 49% |
| % seen within one hour of target time | 81% | 69% | 73% | 94% |
| Average waiting time | 2 h 56 min | 1 h 37 min | 55 min | 11 min |
Discussion
This study demonstrated the validity of the use of the SATS to triage patients in a rural district hospital EC. The assigned acuity correlated well (f = 0.37; p < 0.0001) with the outcome and acceptable rates of over-triage (49%) and under-triage (9%) were found. This confirms the validity displayed in previous studies conducted on the SATS in other settings. It also confirms that with very limited training the EC nursing staff were able to utilise the SATS successfully.
This study was conducted in an operational clinical setting following the model set by previous validation studies of the SATS [5], [9]. This allowed for validation of the tool’s performance when utilised by real nurses with real presentations in a busy rural district hospital. Inter-observer accuracy of the SATS was intentionally not assessed to allow for assessment of validity in a setting where mistakes are inevitably made. Despite this presumption of inaccuracy, this study has added to the literature confirming that the SATS is a robust tool in a real clinical setting.
The high acuity rate (red and orange acuity) of 17% in this study is lower than the rate of 32.1% reported in Ngwelezane [9], a rural regional hospital, but comparable to the 22% noted in Somaliland [5]. Patients triaged as routine (green) were the largest proportion of patients at 46%. This probably reflects our district health system more than the triage system. In our setting where access to a doctor is limited, patients often utilise the EC as a first point of contact with a doctor. Poor emergency medical services, poor road infrastructure, and limited access to alternative transport especially after-hours are specific barriers to access to hospital care in our setting which may influence the acuities of patients presenting to our EC.
Under-triage in this clinical setting results in potentially dangerous delays in access to appropriate care. The under-triage rate of 9.4% in our study meets the ASCOT target of less than 10% which is comparable to rates of under-triage in validity studies published from elsewhere [5], [14].
The under-triage rate for patients under three years old was 12.7% and for patients three to twelve years old 11%, which is above the target range and is not consistent with a much larger multicentre study in a paediatric population which reported an under-triage rate of 9% [14]. The higher under-triage rate in paediatric patients may indicate that the paediatric SATS process is more clinically challenging and may therefore be more prone to errors. When implementing the SATS in other rural district hospitals, we suggest paediatric assessment should be emphasised more in training. A marginally higher under-triage rate may also be appropriate in this context amongst a team of clinicians who have actively decided on a lower admission threshold, not solely informed by the acuity of the patient, but influenced by reasons such as socio-economics, geography and access to transport, and limited opportunity for proper medical work-up outside of hospital. This highlights a key limitation in this study, and indeed most triage validity studies, in that the outcome variables of admission, transfer and discharge are all heavily influenced by the context.
Our reported rate of over triage is 49% which is within the ASCOT target of 30–50%. The potential danger of over-triage is the risk of congestion and delays in attending to the true urgent cases. The rate is on the upper limits of acceptable and may have contributed to waiting time targets not being met.
The explicit target waiting times specific to each designated acuity suggested by the SATS were not well achieved. In Zithulele Hospital as well as other district hospitals the EC is serviced by hospital generalists with competing responsibilities within the hospital rather than a dedicated EC doctor. The triage form only recorded time of assessment by a doctor. In reality, nurse led triage with an objective triage tool identified high acuity patients and frequently prompted nursing interventions to stabilise patients even before doctor assessment. Staffing, patient load, peak time assessment, over-triage rate, structural and system factors all affect the achievability of the targets and a pragmatic view needs to be taken in the rural district EC. The overall average waiting time of 125 min compares favourably with other published data [15].
A limitation of this study is that longitudinal follow up was not possible and the outcomes selected as surrogate markers of acuity take into account only the patients’ time spent in the emergency centre. A patient assessed as having low acuity, for example, may have been discharged only to be admitted the next day. Two of the investigators were intermittently involved in patient care in the EC during the data collection process. The investigators, however, were part of a team of 14 doctors focused on clinical care. Their presence as part of the team is likely to have had little or no influence on the data. The clinical staff was aware of the study which may have introduced a Hawthorne effect, but this too was limited as the staff were not aware of the methods of evaluation. No data was collected on patient presentations, outcomes, and patient waiting times pre-implementation of the triage system, therefore, we are unable to compare the functioning of the EC pre- and post-implementation of the triage system.
In conclusion, the South African Triage Scale is a valid triage tool in a rural district EC with acceptable levels of under- and over-triage after implementation with minimal training of EC nurses, and should be considered the standard of care in rural district emergency centres.
Acknowledgments
Acknowledgements
We would like to acknowledge Nonceba Sigonya-Ndesi who was responsible for data collection and Molly and Steffan Glaze whose assistance was invaluable in outcome tracing.
Conflicts of interest
The authors declare no conflict of interest.
Dissemination of results
Results were presented to the clinical team as part of the academic programme as well as at the Rural Health Conference 2017.
Authors’ contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: GM, TNM and CBG contributed 33% each. All authors approved the version to be published, and agreed to be accountable for all aspects of the work.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.World health organization. Emergency care systems, http://www.WHO.int/emergency are/systems/en/. [accessed 15/5/2017].
- 2.Razzaq J.A., Kellermann A.L. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. [PMC free article] [PubMed] [Google Scholar]
- 3.Gottschalk S.B., Wood D., De Vries S. The cape triage score, a new triage system South Africa. Proposal from the cape triage group. Emerg Med J. 2006;23:149–153. doi: 10.1136/emj.2005.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rominski S., Bell S.A., Oduro G. The implementation of the South African Triage Score (SATS) in an urban teaching hospital, Ghana. Afr J Emerg Med. 2014;4:71–75. doi: 10.1016/j.afjem.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanyoto T., Van Den Berg R., Valles P. Providing emergency care and assessing a patient triage system in a referral hospital in Somaliland: a cross-sectional study. BMC Health Serv Res. 2014;14:531. doi: 10.1186/s12913-014-0531-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison H.L., Raghunath N., Twomey M. Emergency triage, assessment and treatment at a district hospital in Malawi. Emerg Med J. 2012;29:924–925. doi: 10.1136/emermed-2011-200472. [DOI] [PubMed] [Google Scholar]
- 7.Dalwai M.K., Twomey M., Maikere J. Reliability and accuracy of the South African Triage Scale when used by nurses in the emergency department of Timergara Hospital, Pakistan. S Afr Med J. 2014;104(5):372–375. doi: 10.7196/samj.7604. [DOI] [PubMed] [Google Scholar]
- 8.Gordon S.A.N., Brits H., Raubenheimer J.E. The effectiveness of the implementation of the Cape Triage Score at the emergency department of the National District Hospital, Bloemfontein. S Afr Fam Pract. 2015;57(1):18–23. [Google Scholar]
- 9.Rosedale K., Smith Z.A., Davies H. The effectiveness of the South African Triage Score (SATS) in a rural emergency department. S Afr Med J. 2011;101:537–540. [PubMed] [Google Scholar]
- 10.Hanewinckel R., Jongman H., Wallis L. Emergency Medicine in Paarl, South Africa: a cross-sectional descriptive study. Int J Emerg Med. 2010;3:143–150. doi: 10.1007/s12245-010-0185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farrohknia N., Castren M. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resuscit Emerg Med. 2011;19:42. doi: 10.1186/1757-7241-19-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Twomey M., Wallis L.A., Myers J.E. Limitations in validating emergency department triage scales. Emerg Med J. 2007;24:477–479. doi: 10.1136/emj.2007.046383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American College of Surgeons Committee on Trauma (ASCOT) American College of Surgeons; Chicago: 1999. Resources for Optimal Care of the Injured Patient. [Google Scholar]
- 14.Twomey M., Cheema B., Base H. Vital signs for children at triage in multicentre validation of the revised South African Triage Scale for children. S Afr Med J. 2013;103(5):304–308. doi: 10.7196/samj.6877. [DOI] [PubMed] [Google Scholar]
- 15.Bruijns S.R., Wallis L.A., Burch V.C. Effect of introduction of nurse triage on waiting times in a South African emergency department. Emerg Med J. 2008;25:395–397. doi: 10.1136/emj.2007.049411. [DOI] [PubMed] [Google Scholar]
- 16.Bruijns S.R., Wallis L.A., Burch V.C. A prospective evaluation of the Cape triage score in the emergency department of an urban public hospital in South Africa. Emerg Med J. 2008 Jul;25(7):398–402. doi: 10.1136/emj.2007.051177. [DOI] [PubMed] [Google Scholar]
- 17.Dalwai M., Valles P., Twomey P. Is the South African Triage Scale valid for use in Afghanistan, Haiti and Sierra Leone? BMJ Global Health. 2017;2(2):e000160. doi: 10.1136/bmjgh-2016-000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emergency Medicine Society of South Africa. The South African Triage Scale. 2012 [Internet]. Available from: https://emssa.org.za/sats/. [Accessed 12 March 2018].