Abstract
We report a case of acute myocardial infarction caused by left anterior descending artery occlusion presenting as ST elevation in the inferior leads and ST depression in the precordial leads, suggesting an involvement of the right coronary artery (RCA). However, coronary angiography (CAG) showed a complete occlusion of the proximal left anterior descending (LAD) coronary artery and collaterals from the left circumflex coronary artery and the RCA. Although he underwent primary percutaneous coronary intervention (PCI), he had chest pain at four days after primary PCI. His electrocardiogram (ECG) showed precordial ST elevation, suggesting an involvement of the LAD. Emergent CAG showed a complete occlusion of the proximal LAD without collaterals, but his ECG showed precordial ST elevation that was different from ST changes seen on admission. These unusual ST-segment changes might be associated with a weaker anterior ischemia due to collaterals and a strong inferior ischemia due to wrapped LAD artery.
<Learning objective: Inferior ST elevation and anterior ST depression generally indicate inferior myocardial infarction. However, the unusual ST-segment changes seen in this patient with anterior myocardial infarction might be associated with a weaker anterior ischemia due to collaterals and a strong inferior ischemia due to wrapped left anterior descending artery.>
Keyword: Acute myocardial infarction, Electrocardiogram, Collaterals
Introduction
Acute ST-segment elevations in the inferior leads generally suggest acute occlusion of the right coronary artery (RCA). Occlusion of the left anterior descending coronary artery (LAD) may cause infarction of the anterior wall of the left ventricle, manifested as precordial ST-segment elevations. Inferior ST-segment elevations due to occlusion of a LAD may reflect an ischemia of wrapped LAD artery [1], [2]. We describe a patient with ST elevation in inferior leads and ST depression in precordial leads caused by acute occlusion at the proximal segment LAD with collateral flow from the left circumflex (LCx) coronary artery and RCA.
Case report
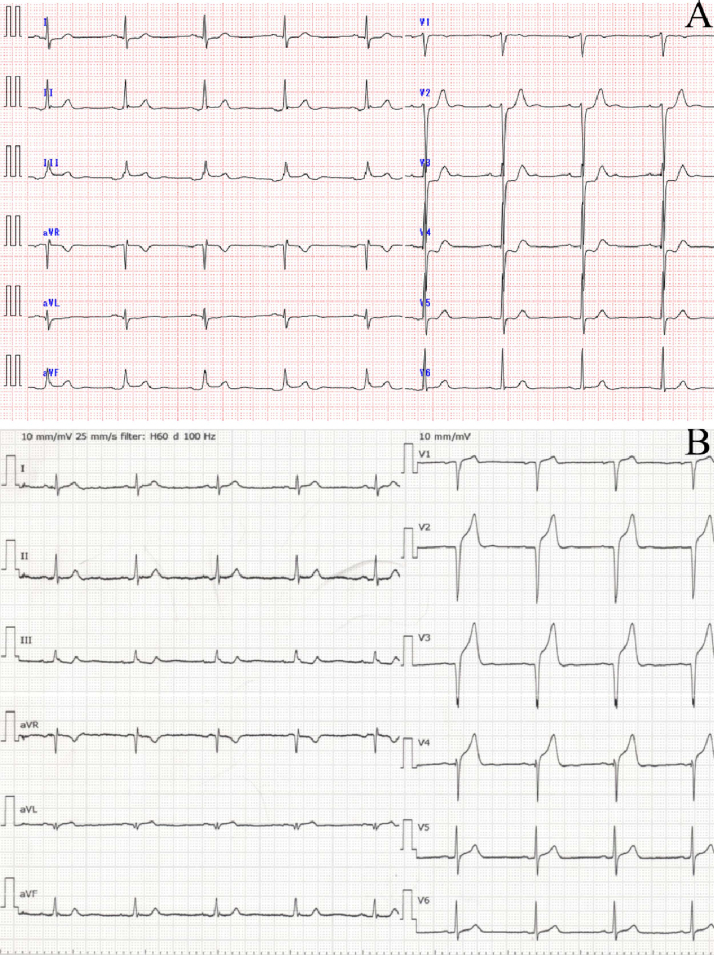
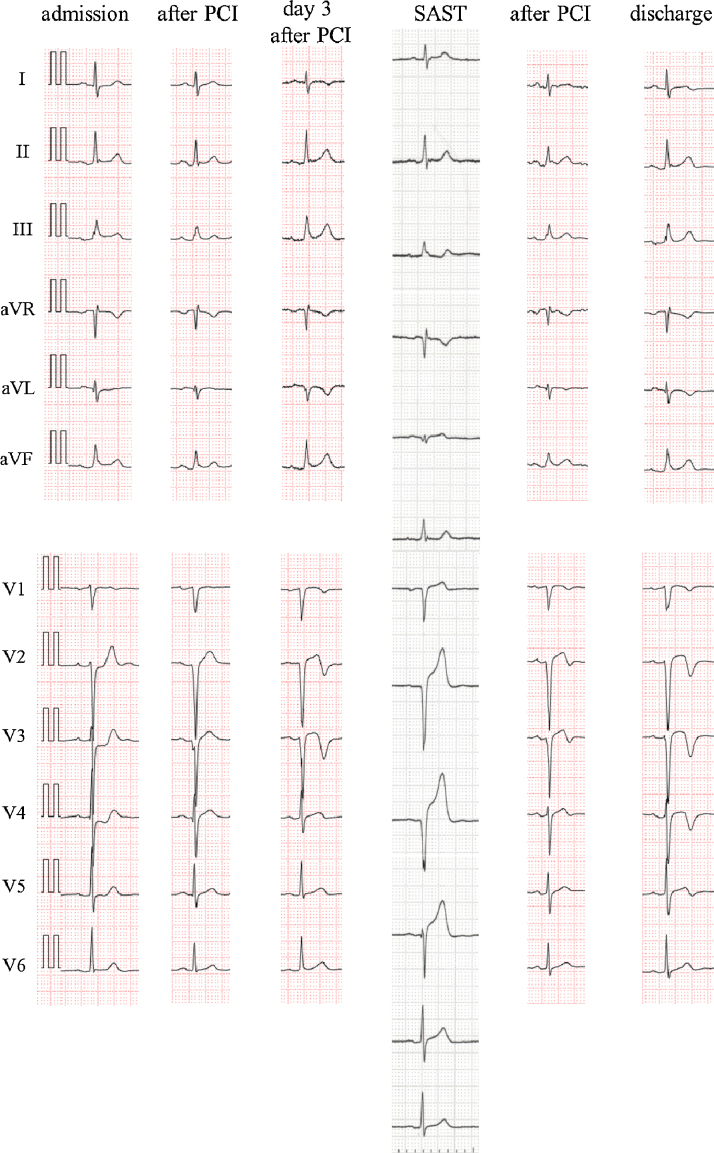
A 53-year-old man was referred to our hospital for chest pain he had experienced for a few hours. His electrocardiogram (ECG) showed ST-segment elevation in the inferior leads and ST-segment depression in the V2–V4 leads (Fig. 1, Fig. 2), suggesting an involvement of the RCA. However, emergent coronary angiography (CAG) showed a complete proximal occlusion of the LAD coronary artery (Fig. 3A, arrow 1) and collaterals from the LCx coronary artery (Fig. 3A and B, arrows 2–3) and the RCA (Fig. 3C, arrows 4–5). He underwent primary percutaneous coronary intervention (PCI) with coronary artery stenting to the infarct-related LAD. Four days after primary PCI, he had chest pain again. His ECG showed precordial ST elevation (Fig. 1, Fig. 2), suggesting an involvement of LAD. Emergent CAG showed a complete proximal occlusion of the LAD without collaterals (Fig. 3D, arrow 6). He underwent PCI for subacute stent thrombosis (SAST) (Fig. 3E and F).
Fig. 1.
Electrocardiogram (ECG) on admission and at the time of subacute stent thrombosis (SAST). (A) ECG on admission and (B) ECG at the time of SAST.
Fig. 2.
Electrocardiogram (ECG) evolution. ECG after admission in emergency room demonstrated ST-elevation in II, III, aVF leads with combined ST-depression in V2–V4 leads. After primary PCI, ST was normal with abnormal Q wave in V1–V3 leads. At 4 days after primary PCI, ST-elevation in V1–V4 leads was detectable. After PCI, ST was normal. Negative T waves were present before discharge in V1–V4, aVL leads.
Fig. 3.
Coronary angiography (CAG) on admission and at the time of subacute stent thrombosis (SAST). (A) CAG on admission, 1: occlusion of the proximal LAD, 2: collaterals from LCx to diagonal branch, (B) CAG on admission, 3: collaterals from LCx to diagonal branch, (C) CAG on admission, 4: collaterals from RCA to septal branch, 5: collaterals from RCA to the distal LAD, (D) CAG at the time of SAST, 4: occlusion of the proximal LAD, (E) CAG at the time of SAST, and (F) CAG at the time of SAST, 7: wrapped LAD.
Discussion
We report for the first time that coronary artery occlusion at the same segment in a patient showed different ECG changes. Although his ECG on admission showed ST-segment elevation in the inferior leads and ST-segment depression in the V2–V4 leads (Fig. 1, Fig. 2), his ECG at four days after primary PCI showed precordial ST elevation (Fig. 1, Fig. 2). Interestingly, the culprit lesion in these coronary events was the same segment, proximal LAD.
Inferior ST-segment elevation during anterior wall acute myocardial infarction (AMI) due to LAD coronary artery occlusion is uncommon [3], [4]. Usually, 2 conditions are thought to be necessary for these findings: relatively small mass of ischemic anterior wall myocardium, resulting in a weaker anterior injury current and less reciprocal inferior ST-segment depression, and a concomitant inferior wall transmural ischemia that further shifts the inferior ST segments upward. According to other studies, inferior ST-segment elevation was related to a distal LAD stenosis or a wrapped LAD artery [1], [2].
In our case report, first ECG might be associated with a weaker anterior ischemia due to collaterals and a strong ischemia due to a wrapped LAD artery. It might be associated with rich collaterals from RCA and LCx to middle segment of LAD and diagonal branch and fewer collaterals to apical segment of LAD. This unusual pattern was previously presented by Brunetti et al. However, a pathophysiological explanation for this peculiar ECG pattern was explained with distal embolization into the distal, inferior part either of the LAD or LCx, or a concomitant spasm of the RCA because they did not undertake emergent coronary angiography [5]. In our patient, rich collaterals from the LCx and RCA supplied the anterior wall and the total occlusion of the wrapped LAD caused an ischemia of the inferior wall.
The second ECG shows the complete occlusion of the proximal LAD. This was explained with an ischemia of anterior wall, because there were not collaterals from other coronary arteries. First, past study showed that coronary collaterals accompanied with coronary occlusion in dogs disappeared within 24 h after reperfusion [6]. Second, a previous study demonstrated that collateral flow might increase considerably over time even in the first 6 h following acute coronary occlusion [7]. In this case, the time from chest pain to angiography was only 25 min at the time of SAST although it was 3.3 h on admission. The collaterals to LAD might not work at SAST, because they had already disappeared after primary PCI and there was not enough time for the collaterals to LAD to develop again.
In summary, this is an exceptional ECG showing inferior ST elevation and anterior ST depression, secondary to occlusion of LAD.
Conflict of interest
We do not have a direct financial relation with the commercial identities mentioned in our paper that might lead to conflict of interest for any of the authors.
References
- 1.Sapin P.M., Musselman D.R., Dehmer G.J., Cascio W.E. Implication of inferior ST-segment elevation accompanying anterior wall acute myocardial infarction for the angiographic morphology of the left anterior descending coronary artery morphology and site of occlusion. Am J Cardiol. 1992;69:860–865. doi: 10.1016/0002-9149(92)90783-u. [DOI] [PubMed] [Google Scholar]
- 2.Sasaki K., Yotsukura M., Sakata K., Yoshino H., Ishikawa K. Relation of ST-segment changes in inferior leads during anterior wall acute myocardial infarction to length and occlusion site of the left anterior descending coronary artery. Am J Cardiol. 2001;87:1340–1345. doi: 10.1016/s0002-9149(01)01549-1. [DOI] [PubMed] [Google Scholar]
- 3.Kosuge M., Kimura K. Clinical implication of electrocardiograms for patients with anterior wall ST-segment elevation acute myocardial infarction in the interventional era. Circ J. 2012;76:32–40. doi: 10.1253/circj.cj-11-1119. [DOI] [PubMed] [Google Scholar]
- 4.Kosuge M., Ebina T., Hibi K., Iwahashi N., Tsukahara K., Endo M., Maejima N., Nagashima Z., Suzuki H., Morita S., Umemura S., Kimura K. Differences in negative T waves between Takotsubo cardiomyopathy and reperfused anterior acute myocardial infarction. Circ J. 2012;76:462–468. doi: 10.1253/circj.cj-11-1036. [DOI] [PubMed] [Google Scholar]
- 5.Brunetti N.D., Correale M., Ieva R., De Gennaro L., Pellegrino P.L., Cucclo A., Di Biase M. An usual case of left anterior descending coronary artery occlusion-anterior ST depression and inferior ST elevation. J Electrocardiol. 2009;42:449–452. doi: 10.1016/j.jelectrocard.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Khouri E.M., Greqq D.E., McGranahan G.M., Jr. Regression and reappearance of coronary collaterals. Am J Physiol. 1971;220:655–661. doi: 10.1152/ajplegacy.1971.220.3.655. [DOI] [PubMed] [Google Scholar]
- 7.Elsman P., van‘t Hof A.W., de Boer M.J., Hoorntje J.C., Suryapranata H., Dambrink J.H., Zijlstra F., Zwolle Myocardial Infarction Study Group Role of collateral circulation in the acute phase pf ST-segment-elevation myocardial infarction treated with primary coronary intervention. Eur Heart J. 2004;25:854–858. doi: 10.1016/j.ehj.2004.03.005. [DOI] [PubMed] [Google Scholar]