Abstract
Hyponatremia often associates with heart failure. Although severe salt restriction is generally recommended in heart failure treatment, it may promote hyponatremia which is a risk factor for increased morbidity and mortality in heart failure patients. Therefore, it is not yet clear whether correction of hyponatremia is an effective treatment in congestive heart failure with hyponatremia. We experienced a successful case of refractory congestive heart failure with hyponatremia treated with hypertonic saline and furosemide. A 45-year-old man, suffering from dilated cardiomyopathy, was admitted to our hospital for heart failure worsening with hyponatremia. We started diuretics therapy without correction of hyponatremia, but his clinical status of heart failure was not improved. Therefore, we additionally started to correct hyponatremia by continuous injection of hypertonic saline. The correction of hyponatremia increased urinary volume dramatically, and improved cardiac output and clinical status of heart failure. This case strongly suggests that combination of hypertonic saline and furosemide could enhance diuretic effect, and improve the clinical status of heart failure in congestive heart failure patients with hyponatremia.
<Learning objective: Hyponatremia is a major problem associated with heart failure, but it is not yet clear whether correction of hyponatremia is an effective treatment in patients with congestive heart failure. We experienced a successful case of refractory congestive heart failure with hyponatremia treated with hypertonic saline and low dose furosemide. This case strongly suggests that aggressive correction of hyponatremia can be an effective treatment for refractory congestive heart failure with hyponatremia.>
Keywords: Diuretics, Heart failure, Hypertonic saline, Hyponatremia
Introduction
Hyponatremia is a major problem associated with heart failure. Previous studies reported that hospital and post-discharge mortality were higher and hospital stay was longer in heart failure patients with hyponatremia than in those without hyponatremia [1]. However, there are no guidelines for the appropriate approach to treat hyponatremia associated with heart failure. We describe a successful case of refractory congestive heart failure with hyponatremia, in which 40 mg of furosemide and correction of hyponatremia with hypertonic saline increased urinary volume and cardiac output, and improved the clinical status of heart failure.
Case report
A 45-year-old man with general fatigue and dyspnea at rest was admitted to our hospital in January 2013. He had been diagnosed with dilated cardiomyopathy after various examinations in 1993. His clinical status gradually got worse regardless of optimal medical therapy including carvedilol, lisinopril, spironolactone, furosemide, and amiodarone. He received cardiac resynchronization therapy device implantation in September 2011, but his clinical status was not improved and it continued to deteriorate. Eventually, he was hospitalized in our hospital in January 2013. His laboratory data showed 136 mEq/L of serum sodium, 1.8 mg/dL of serum total bilirubin, 0.97 mg/dL of serum creatinine, and 2860 pg/mL of plasma B-type natriuretic peptide on admission. His body weight was 78 kg on admission, which was a 5 kg gain compared with that of the previous hospital discharge. Transthoracic echocardiography showed an ejection fraction of 19%, left ventricular (LV) diastolic diameter of 78 mm, and velocity time integral at LV outflow tract (LVOT-VTI) of 8.0 cm. These data suggested hypervolemic hyponatremia, liver congestion, and low cardiac output due to right- and left-sided heart failure.
We started continuous intravenous infusion of furosemide 40 mg/day, but that could not induce effective diuresis. Therefore, we additionally started intravenous infusion of inotropes, low-dose dobutamine 3 μg/kg/min, and that could induce effective diuresis. His body weight decreased to 71 kg about a week after the start of the therapy. However, serum sodium level and urinary volume started to decrease gradually (Fig. 1). Despite 7 kg of body weight loss, he was still presenting pulmonary and peripheral congestion about a month after the start of the therapy. A hemodynamic study was performed on the 31st hospital day, and it showed 18 mmHg of mean right atrial pressure, 38 mmHg of mean pulmonary artery wedge pressure, and 1.5 L/min/m2 of cardiac index. His laboratory data on the same day showed 129 mEq/L of serum sodium. Transthoracic echocardiography showed LVOT-VTI of 8.8 cm. These data suggested that his clinical status was not improved and hyponatremia was the cause. We decided to introduce tolvaptan, vasopressin type 2 receptor antagonist, at 3.75 mg/day. One week after the start of tolvaptan, urinary volume increased slightly and body weight reduced by 1.5 kg, but his symptoms of general fatigue and dyspnea were not improved (Fig. 1). His laboratory data on that day showed 128 mEq/L of serum sodium and 12.7 pg/mL of plasma arginine vasopressin (AVP) level, and his echocardiography showed LVOT-VTI of 5.6 cm. Despite the administration of tolvaptan, his clinical status was not improved (Table 1).
Fig. 1.
Time course of serum sodium level, urinary volume, body weight, and chest X-ray. Serum sodium level was gradually decreasing, and became less responsive to diuretics about one or two weeks after the start of the treatment. After the start of the combination of hypertonic saline and furosemide, urinary volume increased and body weight decreased. Serum sodium level was gradually improved. One week after the tolvaptan, cardiothoracic ratio (CTR) of chest X-ray was increased, compared with that on 31st hospital day. One week after the start of the combination of hypertonic saline with low-dose furosemide, the CTR was improved.
Table 1.
Time course of echocardiographic parameters, blood examination, and atrial blood gas LVDd, left ventricular diastolic diameter; LVOT, velocity time integral at left ventricular outflow tract; TR-PG, tricuspid regurgitation peak pressure gradient; AVP, arginine vasopressin; BUN, serum blood urea nitrogen level; Cre, serum creatinine level; PaO2, partial pressure of oxygen in arterial blood; PaCO2, partial pressure of carbon dioxide in arterial blood. The combination therapy of hypertonic saline with furosemide increased serum sodium level, not exponentially but gradually. Additionally, it did not lead to renal dysfunction and improved plasma AVP level.
| Hospital day | 1 | 31 | 38 | 45 |
|---|---|---|---|---|
| Echocardiographic parameters | ||||
| Ejection fraction (%) | 19 | 20 | 16 | 20 |
| LVDd (mm) | 78 | 76 | 75 | 77 |
| LVOT-VTI (cm) | 8.0 | 8.8 | 5.6 | 10.7 |
| Stroke volume (mL) | 27 | 30 | 19 | 36 |
| TR-PG (mmHg) | 52 | 41 | 34 | 43 |
| Blood examination | ||||
| AVP (pg/mL) | – | – | 12.7 | 3.6 |
| BUN (mg/dL) | 24 | 24 | 17 | 13 |
| Cre (g/dL) | 0.97 | 0.75 | 0.86 | 0.78 |
| Serum sodium (mEq/L) | 136 | 129 | 128 | 132 |
| Arterial blood gas | ||||
| PaO2 | 70 | 122 | – | 95 |
| PaCO2 | 37 | 20 | – | 36 |
| pH | 7.382 | 7.554 | – | 7.422 |
| Base excess | −3.4 | −5.5 | – | −1.5 |
Therefore, we decided to correct hyponatremia aggressively. We started continuous infusion of hypertonic saline (10% solution of sodium chloride, 46 mL/day) in addition to 40 mg of furosemide. After that, urinary volume markedly increased and body weight decreased by 4.5 kg in a week. Serum sodium level was improved (132 mEq/L) and plasma AVP level decreased dramatically (3.6 pg/mL) (Fig. 1 and Table 1). LVOT-VTI increased from 5.6 cm to 10.7 cm in echocardiographic assessment. These data suggest that the combination therapy of furosemide and correction of hyponatremia with hypertonic saline enhanced diuretic effect, and increased cardiac output.
Although cardiac output was improved, it was difficult to wean inotrope. Therefore, we evaluated the status of his heart failure as “end-stage”, INTERMACS profile 3: stable but inotrope dependent, and decided an indication of heart transplantation [2]. Eventually he underwent the implantation of an artificial heart, EVAHEART® (Sun Medical, Nagano, Japan) with stable state in March 2013, for the purpose of “bridge to transplantation”.
Discussion
Hyponatremia is a major problem associated with heart failure, and no previous studies describe how to treat hyponatremia in patients with heart failure. Salt restriction is believed to be an essential management of heart failure in clinical practice. The 2010 Heart Failure Society of America guideline on acute decompensated heart failure recommends a sodium intake of <2 g/day in patients with recurrent or refractory volume overload [3]. Most medical providers believe this management is applied in every status of heart failure. However, some previous studies reported that severe salt restriction increases neurohormonal activity, and reduces renal blood flow and glomerular filtration rate 4, 5. Therefore, it is not yet clear whether aggressive correction of hyponatremia is an effective treatment in patients with congestive heart failure complicated by hyponatremia.
Generally, cardiac output and effective blood circulation volume are decreased in patients with severe congestive heart failure [6]. In such patients, non-osmotic stimulation of AVP is promoted via baroreceptor signal, and an elevation of plasma AVP level leads to water retention, resulting in hypervolemic hyponatremia [7].
Hyponatremia is also caused as a complication of heart failure therapy. Intravenous diuretics are administered to most patients hospitalized for decompensated severe heart failure with volume overload. Although intravenous diuretics are effective drugs for water excretion, they also facilitate excretion of sodium, resulting in hyponatremia [8]. Additionally, salt restriction which is recommended in the guideline also promotes hyponatremia. Therefore, hyponatremia can be caused by both diuretics and salt restriction which are major therapies of heart failure [9].
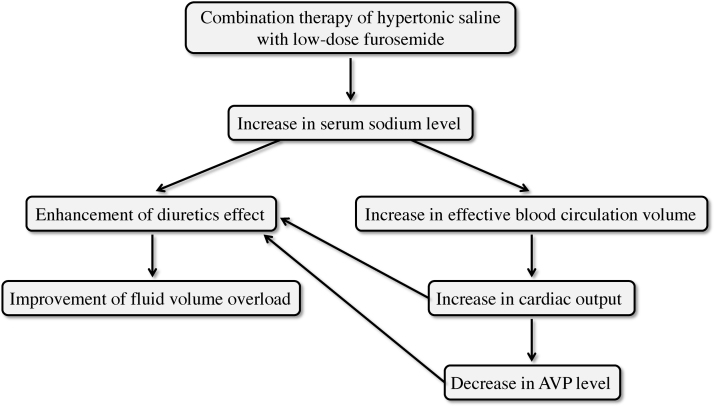
Hyponatremia was reported as a risk factor for increased morbidity and mortality in patients with chronic heart failure [1]. Therefore, aggressive correction of hyponatremia may have favorable effects on heart failure complicated by hyponatremia. It may increase cardiac output through an increase in effective blood circulation volume, improve inappropriate elevation of AVP, and enhance effects of diuretics (Fig. 2).
Fig. 2.
Mechanism of hypertonic saline effects in congestive heart failure complicated with hyponatremia. Hypertonic saline firstly increases serum sodium level. An increase in serum sodium level leads to an increase in cardiac output and a decrease in AVP level, through an increase in effective blood circulation volume. Those changes enhance diuretics effect, and lead to an improvement in fluid volume overload. AVP, arginine vasopressin.
We actually administered 46 mL of hypertonic saline (10% solution of sodium chloride) with 40 mg of intravenous furosemide in this case. This combination therapy of hypertonic saline with low-dose furosemide dramatically increased the urinary volume and decreased his body weight. Additionally, the LVOT-VTI, indicator of cardiac output, was dramatically improved. Hyponatremia was gradually improved, and the plasma AVP level dramatically decreased from 12.7 to 3.6 pg/mL.
Licata et al. previously reported that combination of hypertonic saline and furosemide was useful therapy in heart failure [10]. However, an extremely high dose of furosemide (500–1000 mg) was administered in the study, whereas the dose of furosemide was only 40 mg in our case. There is no report regarding the combination of hypertonic saline and low-dose furosemide.
In conclusion, this case strongly suggests that the combination therapy of hypertonic saline with low-dose furosemide is an effective treatment in patients with refractory congestive heart failure complicated with hyponatremia.
Conflict of interest
Authors declare no conflict of interest.
References
- 1.Abdel-Qadir H.M., Tu J.V., Yun L., Austin P.C., Newton G.E., Lee D.S. Diuretics dose and long-term outcomes in elderly patients with heart failure after hospitalization. Am Heart J. 2010;160:264–271. doi: 10.1016/j.ahj.2010.05.032. [DOI] [PubMed] [Google Scholar]
- 2.Stevenson L.W., Pagani F.D., Young J.B., Jessup M., Miller L., Kormos R.L., Naftel D.C., Ulisney K., Desvigne-Nickens P., Kirklin J.K. INTERMACS profiles of advanced heart failure: the current picture. J Heart Lung Transplant. 2009;28:535–541. doi: 10.1016/j.healun.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Heart Failure Society of America, Lindenfeld J., Albert N.M., Boehmer J.P., Collins S.P., Ezekowitz J.A., Givertz M.M., Katz S.D., Klapholz M., Moser D.K., Rogers J.G., Starling R.C., Stevenson W.G., Tang W.H., Teerlink J.R. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1–e94. [Google Scholar]
- 4.Tikellis C., Pickering R.J., Tsorotes D., Huet O., Chin-Dusting J., Cooper M.E., Thomas M.C. Activation of the renin angiotensin system mediates the effects of dietary salt intake on atherogenesis in the apolipoprotein E knockout mouse. Hypertension. 2012;60:98–105. doi: 10.1161/HYPERTENSIONAHA.112.191767. [DOI] [PubMed] [Google Scholar]
- 5.Mori T., Kurumazaka D., Matsumoto C., Shirakawa H., Kimura S., Kitada K., Kobayashi K., Matsuda H., Kitaura Y., Matsumura Y. Dietary salt restriction activates mineralocorticoid receptor signaling in volume-overloaded heart failure. Eur J Pharmacol. 2009;623:84–88. doi: 10.1016/j.ejphar.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Thibonnier M. Vasopressin receptor antagonists in heart failure. Curr Opin Pharmacol. 2003;3:683–687. doi: 10.1016/j.coph.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Szatolowicz V.L., Arnold P.E., Chaimovitz C., Bichet D., Berl T., Schrier R.W. Radioimmunoassay of plasma arginine vasopressin in hyponatremic patients with congestive heart failure. N Engl J Med. 1981;305:263–266. doi: 10.1056/NEJM198107303050506. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg A. Diuretic complications. Am J Med Sci. 2000;319:10–24. [PubMed] [Google Scholar]
- 9.Hirano T., Yamamura Y., Nakamura S., Onogawa T., Mori T. Effects of the V2-receptor antagonist OPC-41061 and the loop diuretic furosemide alone and in combination in rats. J Pharmacol Exp Ther. 2000;292:288–294. [PubMed] [Google Scholar]
- 10.Licata G., Di Pasquale P., Parrinello G., Cardinale A., Scandurra A., Follone G., Argano C., Tuttolomondo A., Paterna S. Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as bolus in refractory congestive heart failure: long-term effects. Am Heart J. 2003;145:459–466. doi: 10.1067/mhj.2003.166. [DOI] [PubMed] [Google Scholar]