Abstract
Background
The exosomal miRNAs have been emerged as biomarkers and therapeutic targets for various diseases, however, the function of exosomal miRNAs in stroke remains largely unknown.
Methods
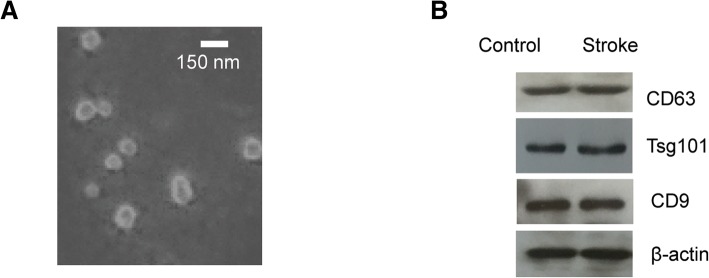
The blood samples from acute ischemic stroke (AIS) patients and normal controls were collected. The exosomes were isolated from the blood samples, which were confirmed by electron microscopy and western blot with the specific exosomes biomarker CD9, CD63 and Tsg101.
Results
RT-qPCR analysis showed that exosomal miR-134 was significantly increased in AIS patients within 24 h after stroke onset compared with that of control group. Highly expressed exosomal miR-134 was correlated with the National Institutes of Health Stroke Scale (NIHSS) scores, infarct volume and positively associated with the worse prognosis of the stroke patients. Additionally, the exosomal miR-134 was strong positively correlated with the expression of serum interleukin 6 (IL-6) and plasma high-sensitivity C relative protein (hs-CRP). The receiver operating characteristic (ROC) curve suggested that miR-134 might be a potential factor to discriminate AIS patients from non-stroke controls.
Conclusions
The exosomal miR-134 as a possible novel biomarker for the diagnosis and prognosis of stroke.
Keywords: Acute ischemic stroke, Exosome, miR-134, National Institutes of Health stroke scale scores, Infarct volume
Background
Stroke is the main cause of neurological dysfunction, which has been considered as the second most common cause of death worldwide and brings heavy burden to the society and family [1–6]. Although remarkable progress has been made in the treatment of stroke, the diagnosis of stroke is still difficult as determining the cause of stroke remains complicated in up to 25% of the patients. Currently, there are no blood-based biomarkers with clinical utility for acute ischemic stroke. Therefore, exploring novel biomarkers involved in the pathogenesis of stroke still remains a challenge.
Tissue responding to the injury caused by stroke and the neuron remodeling after ischemia have been considered as a promising strategy for stroke treatment [7–10]. This process requires the alternation of gene expression in neurons. MicroRNAs (miRNAs) are characterized as non-coding RNAs that inhibit the gene expression via post- transcriptionally regulating the targets via binding the 3′-untranslational region [11–14]. MiRNAs are key regulators of the cell proliferation, differentiation and migration [15]. Aberrant expression of miRNAs has been found in a variety of human diseases. Recent studies showed that circulating miRNAs are highly stable and detectable in the serum of patients with ischemic stroke [16–19]. Up-regulated or down-regulated circulating miRNAs has been identified in stroke patients, which suggested that circulating miRNAs might be a potential biomarkers and therapy targets in stroke.
It has been reported that miRNA can be secreted from cells into the body fluids via exosomes [20–23]. Exosomes are identified as 30–100 nm vesicles that are released into the extracellular space, which deliver protein, mRNA, miRNA or lipid from parent cells to recipient cells [24]. Exosomal miRNAs establish the communication between cell-to-cell and are involved in regulating different biological processes via modulating the expression of target genes. Notably, the critical role of exosomal miRNAs in the development of stroke is emerging [17, 19, 25]. Recent study showed that the plasma exosomal miR-422a and miR-125b-2-3p were potential blood-base biomarkers for monitoring and diagnosing of IS patients [26]. Additionally, the exosome mediated delivery of miR-124 promoted the cortical neurogenesis after stroke [27]. On the other hand, aberrant release of exosomal miRNAs leads to the alternation of gene expression that may induce the initiation and development of cerebral ischemia reperfusion injury. Among these miRNAs, miR-134 was a brain-specific miRNA that was associated with the development of dendritic and synaptic spine [28]. It has been reported that miR-134 was differentially expressed in brain tissues with ischemic injury [29, 30]. In rat model, miR-134 was down-regulated by electroacupuncture and promoted the expression of LIM domain kinase to enhance the synaptic-dendritic plasticity after ischemic stroke [31]. It was also found that overexpression of miR-134 significantly promoted neuron death induced by oxygen-glucose deprivation/reoxygenation by in vitro study [29]. These reports suggested the potential critical roles of miR-134 in regulating cerebral ischemic injury, however, the expression and correlation between miR-134 with the clinical parameters of acute ischemic stroke patients remains largely unknown.
Here, in this study, we detected the expression level of miR-134 in the serum exosomes from the patients with stroke and non-stroke subjects. To determine the clinical significance of miR-134 in stroke, the correlation between the expression of exosomal miR-134 with the National Institutes of Health Stroke Scale (NIHSS) scores, infarct volume, and prognosis of stroke patients were analyzed. The potential application of exosomal miR-134 as a novel biomarker for the diagnosis and therapy of stroke was also discussed.
Methods
Clinical sample collection
The 50 stroke patients were recruited between April 2015 and December 2016 in The Second Affiliated Hospital of Hainan Medical University. The ischemic stroke of these patients was confirmed by magnetic resonance imaging (MRI). The severity of stroke was evaluated with the NIHSS score by experienced neurologists. These AIS patients were divided into different Trial of Org 10,172 in Acute Stroke Treatment (TOAST) subtypes including cardioembolism, large artery atherosclerotic stroke and small artery stroke (Table 1). Control group were enrolled from those who underwent an annual medical examination and denied history of stroke attack at The Second Affiliated Hospital of Hainan Medical University. The cell-free serum samples were collected from the peripheral blood via centrifugation and stored at − 80 °C. This study was approved by The Second Affiliated Hospital of Hainan Medical University. Written consent was obtained from each participant. The clinical characteristics of the stroke patients and controls were described in Table 2.
Table 1.
Stroke patients with different TOAST subtypes
| Subtypes | Number |
|---|---|
| Cardioembolism | 23 |
| Large artery atherosclerotic stoke | 10 |
| Small artery stroke | 17 |
| Total | 50 |
Table 2.
Baseline clinical characteristics of the AIS patients and normal controls
| Parameter | AIS patients (n = 50) | Control (n = 50) | P value |
|---|---|---|---|
| Mean age | 65.42 ± 10.25 | 63.33 ± 14.32 | > 0.05 |
| Gender (Male/Female) | 26/24 | 22/28 | > 0.05 |
| Race (Asian, %) | 100% | 100% | > 0.05 |
| Ethnicity (Han, %) | 100% | 100% | > 0.05 |
| Stroke risk factors | |||
| Hypertension | 30 (60.0%) | 27 (54.0%) | > 0.05 |
| Diabetes mellitus | 24 (48.0%) | 8 (16.0%) | < 0.01 |
| Atrial Fibrillation | 15 (30.0%) | 12 (24.0%) | > 0.05 |
| Hyperlipidemia | 30 (60.0%) | 13 (26.0%) | < 0.01 |
| NIHSS score | 7.82 ± 1.36 | NA | NA |
| mRS ≤2 | 32 (64.0%) | NA | NA |
| > 2 | 18 (36.0%) | NA | NA |
Serum collection and exosomes isolation
Five milliliters of fresh whole blood from stroke patients within 24 h of stroke onset or control groups was collected into the promoting coagulating tubes and incubated at 37 °C for 20 min. And then the blood was centrifuged at 1600 g for 10 min. The serum was transferred into a new tube and centrifuged at 20,000 g at 4 °C for 15 min. The supernatant was collected and kept at − 80 °C until use. The serum exosomes were extracted with the ExoQuick exosome precipitation solution (System Biosciences, CA, USA). Briefly, the serum sample was centrifuged at 3000 g for 15 min at 4 °C. The supernatant was transferred into a fresh tube and one-fourth volume of ExoQuick Solution was added. The samples were mixed well and incubated at 4 °C for 2 h. And then the mixture was centrifuged at 1500 g for 30 min. The supernatant was discarded and the pellet was re-centrifuged for another 5 min at 4 °C. The exosome-containing pellet was resuspended with nuclease-free water. The size and morphology of exosomes were detected by transmission electron microscopy (TEM, Phillip CM120, 60 kV).
RT-qPCR analysis
Total RNA extraction from the serum exosomes was performed with the Exosome RNA Purification Kit (System Biosciences Inc., Mountain View, CA, USA) according to the manufacturer’s instructions. The concentration and quality of the RNA was determined using the NanoDrop ND-2000 spectrophotometer (Thermo Scientific Rockford, IL, USA). Single strand cDNA was synthesized with the First Strand cDNA Synthesis Kit (Ferments, Vilnius, Lithuania). The expression of miR-134 was detected by real time PCR using the SYBR Green Master Mix (Applied Biosystems) on the Applied Biosystems 7900 real-time PCR machine. All the reactions were performed in triplicate. The PCR condition was set as the follows: 95 °C for 10 min, and then 42 cycles of 95 °C for 10s and 60 °C for 1 min. The relative expression abundance of miR-134 was calculated with the 2-∆∆Ct method.
Western blot
Exosomal protein was extracted with the RIPA lysis buffer (Thermo Fisher Scientific, IL, USA). The protein concentration was determined by the Pierce BCA protein assay kit (Thermo Fisher Scientific, IL, USA). 20 μg of protein was loaded and separated by the 12% SDS-PAGE followed by transferred to polyvinylidene fluoride membranes. Afterwards, the membrane was blocked with 5% non-fat milk for 1 h at room temperature (RT) and then incubated with the indicated primary antibodies for 2 h at RT. The bands were detected by incubating the membrane with horse radish peroxidase (HRP)-conjugated secondary antibody for 1 h at RT and visualized using the ECL detection kit (Thermo Fisher Scientific, IL, USA).
Antibody characterization
The antibodies against CD9 (1:1000, sc-13,118, Santa Cruz Biotechnology), CD63 (1:1000, sc-365,604, Santa Cruz Biotechnology), β-actin (1:2000, sc-47,778, Santa Cruz Biotechnology) and Tsg101 (1:2000, ab30875, Abcam) were purchased from the company.
Statistical analysis
The statistical analysis was performed with the SPSS software (version 13.0, Chicago, IL, USA). Difference between two groups was compared by the Student’s t test and multiple comparisons between more than two groups were determined by the one-way analysis of variance (ANOVA) followed by the Bonferroni test. The Chi-squared test was used to assess the correlation between the expression of miR-134 and clinicopathological factors. The exosomal miR-134 expression with the conventional risk factors of stroke was analyzed by the multivariable logistic regression. The correlation between the expression level of miR-134 and the NIHSS score of the stroke patients was determined with the Pearson’s correlation test. P < 0.05 was considered as statistically significant.
Results
Identification of the serum exosomes isolated from the AIS patients
To isolate exosomes from the blood, ExoQuick kit was used to precipitate the microvesicles. Electron microscopy and western blot analysis have been the gold standard for exosome confirmation. The vesicles isolated in the study displayed a spherical structure with 30–100 nm nano-size (Fig. 1a), which is consistent with the diameter of exosomes. To further confirm this, the expression of CD9, CD63 and Tsg101, the commonly used exosomal markers, was detected by western blot. As shown in Fig. 1b, the protein bands of CD9, CD63, Tsg101 and β-actin were all observed with the indicated antibodies respectively. These data suggested that the isolation method we used was suitable for exosome purification.
Fig. 1.
The isolation of exosomes from the serum of AIS patients and controls. a The transmission electron microscope of the exosomes purified from the serum. Scale bar, 150 nm. b Western blot analysis of the exosomal markers with the indicated antibodies
The level of exosomal miR-134 was significantly elevated in stroke patients
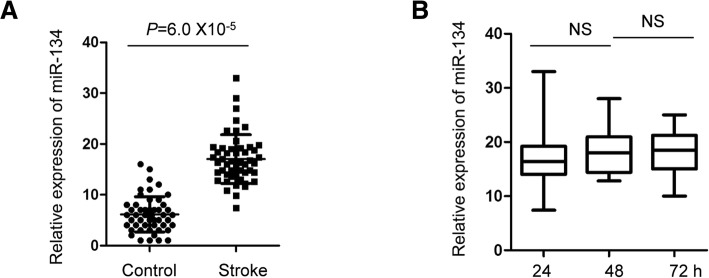
To compare the expression abundance of exosomal miR-134 in stroke patients and normal controls, RT-qPCR analysis was performed with exosomes isolated from patients and the control group. As shown in Fig. 2a, compared with the control group, the expression of exosomal miR-134 was significantly increased in stroke patients within 24 h of the stroke onset. To detect whether the increased expression of miR-134 was a dynamic process after stroke, the expression level of miR-134 in the circulating exosome was examined at 24-, 48- and 72 h after stroke occurred. The data showed that there was no significant difference for the expression of exosomal miR-134 between different time points of the stroke (Fig. 2b).
Fig. 2.
The level of exosomal miR-134 was significantly elevated in stroke patients. a RT-qPCR analysis was performed to detect the expression of serum exosomal miR-134 in both the AIS patients and healthy controls. Student’s t test, n = 50 in stroke group and n = 50 in control group. b The expression level of serum exosomal miR-134 of the AIS patients at different time points after the stroke occurred. N = 50. Ns, no significance. One-way ANOVA
Exosomal miR-134 was a possible biomarker for the diagnosis of AIS
The high expression of exosomal miR-134 in stroke patients led us to determine whether exosomal miR-134 was an independent risk factor in AIS. To this end, logistic regression analysis was performed to evaluate the impact of diabetes mellitus and hyperlipidemia on the expression of exosomal miR-134 between the stroke patients and normal controls. The data suggested that exosomal miR-134 has the possibility to be an independent risk factor of AIS (Table 3). To determine whether the serum exosomal miR-134 can be considered as a biomarker for the diagnosis of AIS, the receiver operating characteristic (ROC) curve was generated with the expression level of miR-134 in the serum exosomes. As shown in Fig. 3, the area under the curve (AUC) of miR-134 was 0.834 (95% confidence interval, 0.88–0.97), with a sensitivity of 75.3%, a specificity of 72.8%, a positive of 94.0%, and a negative predictive value of 88.0%. This data suggested that miR-134 is a possible potential biomarker to discriminate AIS patients from non-stroke controls.
Table 3.
Expression of serum exosomal miR-134 and the risk of stroke
| Characteristics | P value | OR | 95% CI |
|---|---|---|---|
| miR-134 | 0.003 | 2.668 | 1.183–6.441 |
| Diabetes mellitus | 0.001 | 2.842 | 1.514–5.333 |
| Hyperlipidemia | 0.047 | 1.617 | 1.128–3.038 |
Fig. 3.
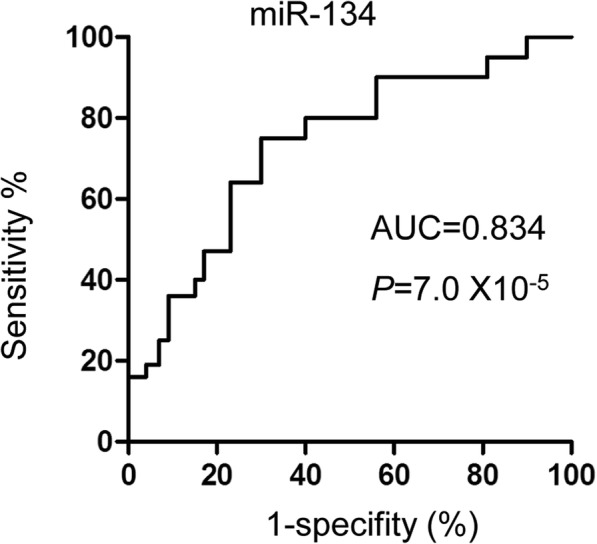
Diagnostic value of serum exosomal miR-134 in AIS. ROC curve was generated based on the level of serum exosomal miR-134 to distinguish AIS patients (n = 50) from normal controls (n = 50). The area under the cure was 0.834 (95% confidence interval, 0.88–0.97)
The relationship between the expression of exosomal miR-134 and the NIHSS score, infarct volume of the stroke patients
To determine the clinical significance of exosomal miR-134 in the diagnosis of acute ischemic stroke, the correlation between the expression of miR-134 and NIHSS scores, infarct volume was examined by the Pearson correlation test. As presented in Fig. 4a, significant correlation between the level of miR-134 and the NIHSS score was observed. Consistent with this data, the expression abundance of exosomal miR-134 was also significantly correlated with the infarct volume of the acute ischemic stroke patients (Fig. 4b). Additionally, to detect the relationship between the expression of circulating exosomal miR-134 with the 3-month prognosis of the stroke patients, the expression level of miR-134 in patients with good or poor outcome was compared. As shown in Fig. 4c, higher abundance of the exosomal miR-134 was found in stroke patients with poor prognosis. These findings suggested the potential clinical application of exosomal miR-134 in stroke.
Fig. 4.
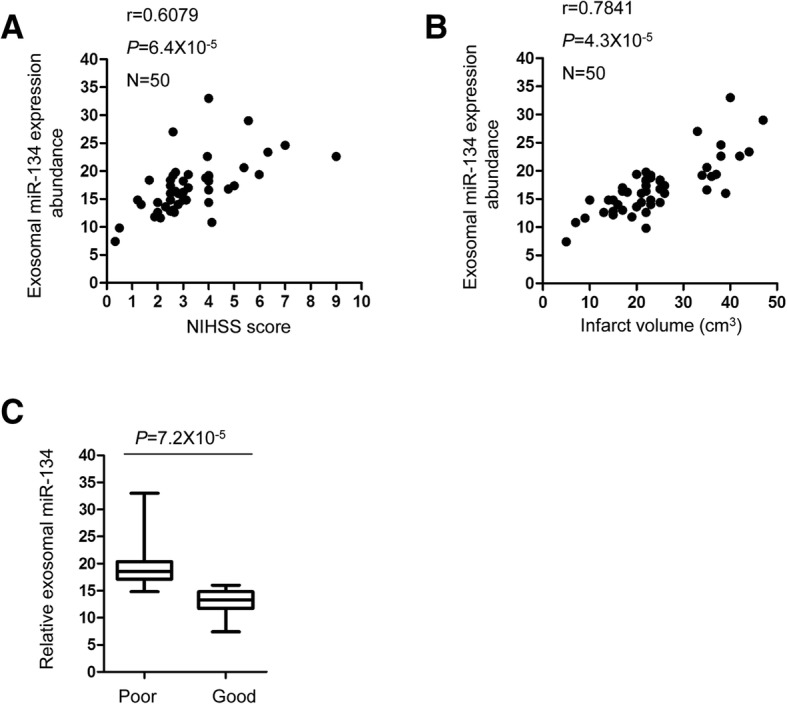
The correlation between the abundance of serum exosomal miR-134 with the NIHSS, infraction volume of AIS patients. a The correlation between exosomal level of miR-134 with the NIHSS score of the stroke patients was analyzed by the Person correlation test. N = 50. b The correlation between exosomal level of miR-134 with the infarction volume of the stroke patients was analyzed by the Person correlation test. N = 50. c The correlation between serum exosomal miR-134 with the outcome of AIS patients. The expression level of miR-134 in AIS patients with good prognosis (modified Rankin Scale (mRS) ≤ 2, n = 32) and poor prognosis ((mRS > 2, n = 18) was analyzed by the Student’s t test
The level of serum exosomal miR-134 was positively correlated with the serum level of IL-6 and plasma hs-CRP
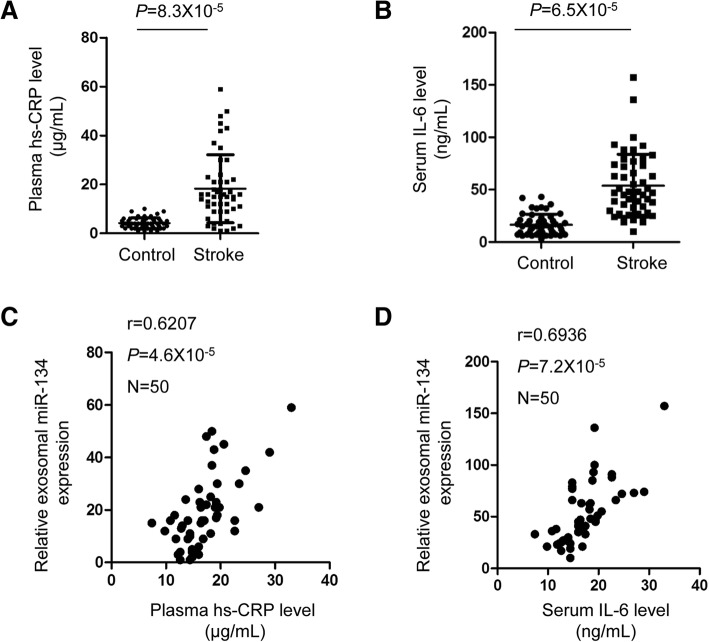
Increasing evidence suggested that inflammation plays critical roles in the development of cardiovascular diseases [32–34]. The pro-inflammatory cytokine IL-6 and hs-CRP was reported to reflect the degree of brain ischemic damage and stroke [35–41]. In this study, the levels of plasma hs-CRP and serum IL-6 were measured in AIS patients and control participants. The results showed that both plasma hs-CRP and serum IL-6 was significantly increased in the AIS patients in comparison with that of the control group (Fig. 5a and b). To further characterize the relationship between exosomal miR-134 and stroke, the correlation between the expressions of exosoma miR-134 and hs-CRP, IL-6 was analyzed, respectively. As shown in Fig. 5c and d, the level of miR-134 presented positive correlations with plasma hs-CRP and serum IL-6.
Fig. 5.
The level of serum exosomal miR-134 was positively correlated with the serum level of IL-6 and plasma hs-CRP. a, b The levels of plasma hs-CRP and serum IL-6 were detected in AIS patients and control participants. Student’s t test. c, d The exosomal miR-134 was positively correlated with the concentration of plasma hs-CRP and serum IL-6 in AIS patients
Discussion
Aberrant expression of miRNAs is associated with the initiation and development of human diseases. Notably, the plasma exosomal miRNAs have been found as diagnosis biomarkers and potential therapeutic targets in some diseases, however, the expression of exosomal miRNAs in acute ischemic stroke and its correlation with the clinical characteristics of the stroke patients remain largely unknown. In this study, we isolated the exosomes from blood of AIS patients and found that exosomal miR-134 was highly expressed in the stroke patients compared with that of the control group. Additionally, miR-134 was positively correlated with the NIHSS score and poor prognosis of these patients. These findings suggested that potential involvement of exosomal miR-134 in AIS.
The intercellular communication is an essential process under both physiological and pathological conditions. It has been well documented that extracellular vesicles and exosomes are important platform to change the genetic information between cells [42]. The extraordinary value of exosomes in the diagnosis and treatment of stroke has drawn wide attention during recent years. The function of exosome in brain injury and neurondegenerative diseases has been demonstrated [43–48]. It has been reported that exosomes protected the brain tissues from ischemia-reperfusion injury after hypoxia precondition [49]. The protection role of exosomes secreted by the mesenchymal stem cells was achieved by delivering functional proteins or RNAs to neurons or astrocytes after ischemic injury [24, 50]. Previous study has showed that increased plasma microvesicles during cerebral ischemia [51, 52]. The number of microvesicles derived from endothelial cells was positively correlated with the occurrence of ischemic stroke [53, 54]. In the present study, increased exosomal miR-134 might indicate the enhanced production of exosomes in stroke patients, which responds to the intercellular brain injury. Further investigation is needed to explore the specific cell type or brain tissue where the exosome derived from.
MiRNAs have emerged as important regulators of cardiovascular physiological processes [55]. It has been documented that miR-21, miR-223 and miR-146b served as biomarkers for acute ischemic stroke [17, 56, 57]. Additionally, elevated serum expression of miR-15a, miR-16 and miR-17-5p was also found to be strongly associated with the AIS [58]. Recent findings showed that miR-134 regulated the ischemia injury-induced neuronal cell death [29]. In the present study, the exosomal miR-134 was significantly increased in AIS samples after stroke in comparison with that of the control group. No remarkable difference was observed for the level of exosomal miR-134 at the time point of 24-, 48- and 72 h after the stroke event. Further study is necessary to explore the alternation of exosomal miR-134 expression with relatively earlier time frame. In the present study, as blood samples of AIS patients were collected within 24 h after the stroke onset, we couldn’t rule out the possibility that the increase of exosomal miR-134 is due to the stroke event based on the present data. Therefore, more evidence is needed to confirm the conclusion that exosomal miR-134 is a potential independent risk factor in AIS. It might be helpful to detect the expression of exosomal miR-134 with normal subjects and follow the occurrence of AIS to establish the correlation between exosomal miR-134 and AIS. In principle, blocking the secretion and uptake of exosomes or inhibiting the expression of exosomal miR-134 might be necessary to investigate the involvement of exosomal miR-134 in the occurrence of AIS.
To evaluate the potential diagnostic value of exosomal miR-134 in AIS, receiver operating characteristic curve was analyzed and the data indicated that exosomal miR-134 might serve as a potential biomarker for distinguishing AIS from non-stroke control. Higher exosomal miR-134 expression may be an important indicator to be considered in medical examination, which might benefit the prevention and implement effective solutions to decrease the occurrence of AIS. To better provide the implication of this study, a larger sample size is necessary in the further investigation. Additionally, our data elucidated the positively correlation between the expression of exosomal miR-134 with the poor prognosis of AIS patients. Increasing evidence suggested that inflammation is involved in the progression of cerebrovascular diseases [59–62]. The plasma hs-CRP and serum IL-6 are important markers of inflammation and associated with the development of stroke. Consistently, our results found that serum exosomal miR-134 was significantly correlated with the increased expression of hs-CRP and IL-6 in AIS patients, which supported the conclusion that exosomal miR-134 was potential candidate for AIS prediction. As the function of miRNAs is achieved via modulating the expression of downstream target genes, further studies will be designed to explore the underlying molecular mechanism by which exosomal miR-134 in response to the ischemic stroke.
Conclusions
Our study demonstrated that the expression of exosomal miR-134 in AIS patients was significantly increased. Enhanced abundance of the exosomal miR-134 was significantly correlated with the poor prognosis of AIS. Due to the relative small sample sizes in this study, further large-scale prospective data and longer follow-up studies were quite necessary to confirm the specificity and accuracy of exosomal miR-134 as a biomarker in the diagnosis of AIS.
Acknowledgements
We would like to thank all the subjects who participate in this study.
Funding
None.
Availability of data and materials
The data of this study was available from the corresponding authors as requested.
Abbreviations
- AIS
Acute ischemic stroke
- ANOVA
One-way analysis of variance
- HRP
Horse radish peroxidase
- hs-CRP
High-sensitivity C relative protein
- IL-6
Interleukin 6
- miRNAs
microRNAs
- MRI
Magnetic resonance imaging
- NIHSS
National Institutes of Health Stroke Scale
- ROC
Receiver operating characteristic
- RT
Room temperature
- TEM
Transmission electron microscopy
- TOAST
Trial of Org 10,172 in Acute Stroke Treatment
Authors’ contributions
JXZ and LC designed the study and performed most of the experiments. BCC purified the exosomes and detected the exosomes with the electron microscopy. SZH and CSZ collected the samples and analyzed the baseline clinical characteristics of the AIS patients and normal controls, as well as the correlation between the expression of exosomal miR-134 and the risk of stroke. HRW and CC interpreted the data. FQL wrote the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the ethics committee of The Second Affiliated Hospital of Hainan Medical University. All the patients involved in this study were introduced with the collection and usage of the tissues when they were conscious and had the capacity of independent decision-making. Written consent was obtained directly from each participant that was approved by the ethics committee of The Second Affiliated Hospital of Hainan Medical University.
Consent for publication
Written informed consent for publication was received from all the patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jingxia Zhou, Email: zhoujingxiayisheng@qq.com.
Lin Chen, Email: linchen49@yahoo.com.
Bocan Chen, Email: bocan517@yahoo.com.
Shaozhu Huang, Email: shaozhu2000@qq.com.
Chaosheng Zeng, Email: zengyisheng88@qq.com.
Hairong Wu, Email: hairongyisheng00@qq.com.
Cong Chen, Email: conghappycong@aliyun.com.
Faqing Long, Email: drctorlong@aliyun.com.
References
- 1.Fargeot G, Stefanizzi S, Depuydt S, Klapczynski F, Ameri A. Association between ischemic stroke and Erdheim-Chester disease: a case report and review of literature. J Stroke Cerebrovasc Dis. 2017;26:e153–e155. doi: 10.1016/j.jstrokecerebrovasdis.2017.04.029. [DOI] [PubMed] [Google Scholar]
- 2.Pires da Rosa G, Libanio D, Filipe Azevedo L. Analysis of the Cochrane Review: Fibrates for secondary prevention of cardiovascular disease and stroke. Rev Port Cardiol. 2017;36:55–58. doi: 10.1016/j.repc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Stefanidis Kayla B., Askew Christopher D., Greaves Kim, Summers Mathew J. The Effect of Non-Stroke Cardiovascular Disease States on Risk for Cognitive Decline and Dementia: A Systematic and Meta-Analytic Review. Neuropsychology Review. 2017;28(1):1–15. doi: 10.1007/s11065-017-9359-z. [DOI] [PubMed] [Google Scholar]
- 4.Sterne JA, Bodalia PN, Bryden PA, Davies PA, Lopez-Lopez JA, Okoli GN, Thom HH, Caldwell DM, Dias S, Eaton D, et al. Oral anticoagulants for primary prevention, treatment and secondary prevention of venous thromboembolic disease, and for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol Assess. 2017;21:1–386. doi: 10.3310/hta21090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang H, Guo W, Li J, Cao S, Zhang J, Pan J, Wang Z, Wen P, Shi X, Zhang S. Leptin concentration and risk of coronary heart disease and stroke: a systematic review and meta-analysis. PLoS One. 2017;12:e0166360. doi: 10.1371/journal.pone.0166360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, et al. Global and regional burden of stroke during 1990-2010: findings from the global burden of disease study 2010. Lancet. 2014;383:245–254. doi: 10.1016/S0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SY, Senatorov VV, Jr, Morrissey CS, Lippmann K, Vazquez O, Milikovsky DZ, Gu F, Parada I, Prince DA, Becker AJ, et al. TGFbeta signaling is associated with changes in inflammatory gene expression and perineuronal net degradation around inhibitory neurons following various neurological insults. Sci Rep. 2017;7:7711. doi: 10.1038/s41598-017-07394-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Zhang X, Cui L, Chen R, Zhang Y, Zhang C, Zhu X, He T, Shen Z, Dong L, et al. Salvianolic acids enhance cerebral angiogenesis and neurological recovery by activating JAK2/STAT3 signaling pathway after ischemic stroke in mice. J Neurochem. 2017;143:87–99. doi: 10.1111/jnc.14140. [DOI] [PubMed] [Google Scholar]
- 9.Okabe N, Narita K, Miyamoto O. Axonal remodeling in the corticospinal tract after stroke: how does rehabilitative training modulate it? Neural Regen Res. 2017;12:185–192. doi: 10.4103/1673-5374.200792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian X, Sun L, Feng D, Sun Q, Dou Y, Liu C, Zhou F, Li H, Shen H, Wang Z, Chen G. HMGB1 promotes neurovascular remodeling via rage in the late phase of subarachnoid hemorrhage. Brain Res. 2017;1670:135–145. doi: 10.1016/j.brainres.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Mizuguchi Y, Takizawa T, Yoshida H, Uchida E. Dysregulated miRNA in progression of hepatocellular carcinoma: a systematic review. Hepatol Res. 2016;46:391–406. doi: 10.1111/hepr.12606. [DOI] [PubMed] [Google Scholar]
- 12.Wen MM. Getting miRNA therapeutics into the target cells for neurodegenerative diseases: a mini-review. Front Mol Neurosci. 2016;9:129. doi: 10.3389/fnmol.2016.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma H, Wu Y, Yang H, Liu J, Dan H, Zeng X, Zhou Y, Jiang L, Chen Q. MicroRNAs in oral lichen planus and potential miRNA-mRNA pathogenesis with essential cytokines: a review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:164–173. doi: 10.1016/j.oooo.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Gambari R, Brognara E, Spandidos DA, Fabbri E. Targeting oncomiRNAs and mimicking tumor suppressor miRNAs: Nuew trends in the development of miRNA therapeutic strategies in oncology (review) Int J Oncol. 2016;49:5–32. doi: 10.3892/ijo.2016.3503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/S0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 16.Xiao S, Ma Y, Zhu H, Sun H, Yin Y, Feng G. miRNA functional synergistic network analysis of mice with ischemic stroke. Neurol Sci. 2015;36:143–148. doi: 10.1007/s10072-014-1904-4. [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Song Y, Huang J, Qu M, Zhang Y, Geng J, Zhang Z, Liu J, Yang GY. Increased circulating Exosomal miRNA-223 is associated with acute ischemic stroke. Front Neurol. 2017;8:57. doi: 10.3389/fneur.2017.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabour S. The diagnostic value of serum miRNA-221-3p, miRNA-382-5p, and miRNA-4271 in ischemic stroke: methodological issue to avoid misinterpretation. J Stroke Cerebrovasc Dis. 2017;26:1161. doi: 10.1016/j.jstrokecerebrovasdis.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Ma Z, Kan P, Zhang B. The diagnostic value of serum miRNA-221-3p, miRNA-382-5p, and miRNA-4271 in ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26:1055–1060. doi: 10.1016/j.jstrokecerebrovasdis.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 20.Madhavan B, Yue S, Galli U, Rana S, Gross W, Muller M, Giese NA, Kalthoff H, Becker T, Buchler MW, Zoller M. Combined evaluation of a panel of protein and miRNA serum-exosome biomarkers for pancreatic cancer diagnosis increases sensitivity and specificity. Int J Cancer. 2015;136:2616–2627. doi: 10.1002/ijc.29324. [DOI] [PubMed] [Google Scholar]
- 21.Valencia K, Luis-Ravelo D, Bovy N, Anton I, Martinez-Canarias S, Zandueta C, Ormazabal C, Struman I, Tabruyn S, Rebmann V, et al. miRNA cargo within exosome-like vesicle transfer influences metastatic bone colonization. Mol Oncol. 2014;8:689–703. doi: 10.1016/j.molonc.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ge Q, Zhou Y, Lu J, Bai Y, Xie X, Lu Z. miRNA in plasma exosome is stable under different storage conditions. Molecules. 2014;19:1568–1575. doi: 10.3390/molecules19021568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yentrapalli R, Merl-Pham J, Azimzadeh O, Mutschelknaus L, Peters C, Hauck SM, Atkinson MJ, Tapio S, Moertl S. Quantitative changes in the protein and miRNA cargo of plasma exosome-like vesicles after exposure to ionizing radiation. Int J Radiat Biol. 2017;93:569–580. doi: 10.1080/09553002.2017.1294772. [DOI] [PubMed] [Google Scholar]
- 24.Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 25.Bam M, Yang X, Sen S, Zumbrun EE, Dennis L, Zhang J, Nagarkatti PS, Nagarkatti M. Characterization of dysregulated miRNA in peripheral blood mononuclear cells from ischemic stroke patients. Mol Neurobiol. 2018;55:1419–1429. doi: 10.1007/s12035-016-0347-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li DB, Liu JL, Wang W, Li RY, Yu DJ, Lan XY, Li JP. Plasma Exosomal miR-422a and miR-125b-2-3p serve as biomarkers for ischemic stroke. Curr Neurovasc Res. 2017;14:330–337. doi: 10.2174/1567202614666171005153434. [DOI] [PubMed] [Google Scholar]
- 27.Yang J, Zhang X, Chen X, Wang L, Yang G. Exosome mediated delivery of miR-124 promotes neurogenesis after ischemia. Mol Ther Nucleic Acids. 2017;7:278–287. doi: 10.1016/j.omtn.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schratt GM, Tuebing F, Nigh EA, Kane CG, Sabatini ME, Kiebler M, Greenberg ME. A brain-specific microRNA regulates dendritic spine development. Nature. 2006;439:283–289. doi: 10.1038/nature04367. [DOI] [PubMed] [Google Scholar]
- 29.Huang W, Liu X, Cao J, Meng F, Li M, Chen B, Zhang J. miR-134 regulates ischemia/reperfusion injury-induced neuronal cell death by regulating CREB signaling. J Mol Neurosci. 2015;55:821–829. doi: 10.1007/s12031-014-0434-0. [DOI] [PubMed] [Google Scholar]
- 30.Liu C, Peng Z, Zhang N, Yu L, Han S, Li D, Li J. Identification of differentially expressed microRNAs and their PKC-isoform specific gene network prediction during hypoxic pre-conditioning and focal cerebral ischemia of mice. J Neurochem. 2012;120:830–841. doi: 10.1111/j.1471-4159.2011.07624.x. [DOI] [PubMed] [Google Scholar]
- 31.Liu W, Wu J, Huang J, Zhuo P, Lin Y, Wang L, Lin R, Chen L, Tao J. Electroacupuncture regulates hippocampal synaptic plasticity via miR-134-mediated LIMK1 function in rats with ischemic stroke. Neural Plast. 2017;2017:9545646. doi: 10.1155/2017/9545646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Libby P. Fanning the flames: inflammation in cardiovascular diseases. Cardiovasc Res. 2015;107:307–309. doi: 10.1093/cvr/cvv188. [DOI] [PubMed] [Google Scholar]
- 33.Gregersen I, Holm S, Dahl TB, Halvorsen B, Aukrust P. A focus on inflammation as a major risk factor for atherosclerotic cardiovascular diseases. Expert Rev Cardiovasc Ther. 2016;14:391–403. doi: 10.1586/14779072.2016.1128828. [DOI] [PubMed] [Google Scholar]
- 34.Sallam N, Laher I. Exercise modulates oxidative stress and inflammation in aging and cardiovascular diseases. Oxidative Med Cell Longev. 2016;2016:7239639. doi: 10.1155/2016/7239639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waje-Andreassen U, Krakenes J, Ulvestad E, Thomassen L, Myhr KM, Aarseth J, Vedeler CA. IL-6: an early marker for outcome in acute ischemic stroke. Acta Neurol Scand. 2005;111:360–365. doi: 10.1111/j.1600-0404.2005.00416.x. [DOI] [PubMed] [Google Scholar]
- 36.Cojocaru IM, Cojocaru M, Tanasescu R, Iliescu I, Dumitrescu L, Silosi I. Expression of IL-6 activity in patients with acute ischemic stroke. Rom J Intern Med. 2009;47:393–396. [PubMed] [Google Scholar]
- 37.Kwan J, Horsfield G, Bryant T, Gawne-Cain M, Durward G, Byrne CD, Englyst NA. IL-6 is a predictive biomarker for stroke associated infection and future mortality in the elderly after an ischemic stroke. Exp Gerontol. 2013;48:960–965. doi: 10.1016/j.exger.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 38.Sand PG. IL-6 variants in ischemic stroke. Ann Neurosci. 2016;23:60–61. doi: 10.1159/000443558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang XF, Zou W, Yang Y. Effects of IL-6 and cortisol fluctuations in post-stroke depression. J Huazhong Univ Sci Technolog Med Sci. 2016;36:732–735. doi: 10.1007/s11596-016-1653-0. [DOI] [PubMed] [Google Scholar]
- 40.Sun SL, Xie YM, Zhang Y, Wang ZF, Yang J, Wang DQ, Jiao Y, Chen J, Tao YH. Study on relationship between constitution and syndrome of MMP-9, IL-6 and MTHFR gene in patients with ischemic stroke. Zhongguo Zhong Yao Za Zhi. 2017;42:3602–3612. doi: 10.19540/j.cnki.cjcmm.2017.0139. [DOI] [PubMed] [Google Scholar]
- 41.Chaudhuri JR, Mridula KR, Umamahesh M, Swathi A, Balaraju B, Bandaru VC. High sensitivity C-reactive protein levels in acute ischemic stroke and subtypes: a study from a tertiary care center. Iran J Neurol. 2013;12:92–97. [PMC free article] [PubMed] [Google Scholar]
- 42.Hao S, Moyana T, Xiang J. Review: cancer immunotherapy by exosome-based vaccines. Cancer Biother Radiopharm. 2007;22:692–703. doi: 10.1089/cbr.2007.368-R. [DOI] [PubMed] [Google Scholar]
- 43.Wan J, Yourshaw M, Mamsa H, Rudnik-Schoneborn S, Menezes MP, Hong JE, Leong DW, Senderek J, Salman MS, Chitayat D, et al. Mutations in the RNA exosome component gene EXOSC3 cause pontocerebellar hypoplasia and spinal motor neuron degeneration. Nat Genet. 2012;44:704–708. doi: 10.1038/ng.2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Basso M, Pozzi S, Tortarolo M, Fiordaliso F, Bisighini C, Pasetto L, Spaltro G, Lidonnici D, Gensano F, Battaglia E, et al. Mutant copper-zinc superoxide dismutase (SOD1) induces protein secretion pathway alterations and exosome release in astrocytes: implications for disease spreading and motor neuron pathology in amyotrophic lateral sclerosis. J Biol Chem. 2013;288:15699–15711. doi: 10.1074/jbc.M112.425066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Richard P, Feng S, Manley JL. A SUMO-dependent interaction between Senataxin and the exosome, disrupted in the neurodegenerative disease AOA2, targets the exosome to sites of transcription-induced DNA damage. Genes Dev. 2013;27:2227–2232. doi: 10.1101/gad.224923.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamlett Eric D., Ledreux Aurélie, Potter Huntington, Chial Heidi J., Patterson David, Espinosa Joaquin M., Bettcher Brianne M., Granholm Ann-Charlotte. Exosomal biomarkers in Down syndrome and Alzheimer's disease. Free Radical Biology and Medicine. 2018;114:110–121. doi: 10.1016/j.freeradbiomed.2017.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tofaris George K. A Critical Assessment of Exosomes in the Pathogenesis and Stratification of Parkinson’s Disease. Journal of Parkinson's Disease. 2017;7(4):569–576. doi: 10.3233/JPD-171176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang Shan, Ge Xintong, Yu Jinwen, Han Zhaoli, Yin Zhenyu, Li Ying, Chen Fanglian, Wang Haichen, Zhang Jianning, Lei Ping. Increased miR-124-3p in microglial exosomes following traumatic brain injury inhibits neuronal inflammation and contributes to neurite outgrowth via their transfer into neurons. The FASEB Journal. 2018;32(1):512–528. doi: 10.1096/fj.201700673R. [DOI] [PubMed] [Google Scholar]
- 49.Vicencio JM, Yellon DM, Sivaraman V, Das D, Boi-Doku C, Arjun S, Zheng Y, Riquelme JA, Kearney J, Sharma V, et al. Plasma exosomes protect the myocardium from ischemia-reperfusion injury. J Am Coll Cardiol. 2015;65:1525–1536. doi: 10.1016/j.jacc.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 50.Simpson RJ, Lim JW, Moritz RL, Mathivanan S. Exosomes: proteomic insights and diagnostic potential. Expert Rev Proteomics. 2009;6:267–283. doi: 10.1586/epr.09.17. [DOI] [PubMed] [Google Scholar]
- 51.Colombo E, Borgiani B, Verderio C, Furlan R. Microvesicles: novel biomarkers for neurological disorders. Front Physiol. 2012;3:63. doi: 10.3389/fphys.2012.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ji Q, Ji Y, Peng J, Zhou X, Chen X, Zhao H, Xu T, Chen L, Xu Y. Increased brain-specific MiR-9 and MiR-124 in the serum exosomes of acute ischemic stroke patients. PLoS One. 2016;11:e0163645. doi: 10.1371/journal.pone.0163645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jung KH, Chu K, Lee ST, Park HK, Bahn JJ, Kim DH, Kim JH, Kim M, Kun Lee S, Roh JK. Circulating endothelial microparticles as a marker of cerebrovascular disease. Ann Neurol. 2009;66:191–199. doi: 10.1002/ana.21681. [DOI] [PubMed] [Google Scholar]
- 54.Kuriyama N, Nagakane Y, Hosomi A, Ohara T, Kasai T, Harada S, Takeda K, Yamada K, Ozasa K, Tokuda T, et al. Evaluation of factors associated with elevated levels of platelet-derived microparticles in the acute phase of cerebral infarction. Clin Appl Thromb Hemost. 2010;16:26–32. doi: 10.1177/1076029609338047. [DOI] [PubMed] [Google Scholar]
- 55.Nouraee N, Mowla SJ. miRNA therapeutics in cardiovascular diseases: promises and problems. Front Genet. 2015;6:232. doi: 10.3389/fgene.2015.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen Z, Wang K, Huang J, Zheng G, Lv Y, Luo N, Liang M, Huang L. Upregulated serum MiR-146b serves as a biomarker for acute ischemic stroke. Cell Physiol Biochem. 2018;45:397–405. doi: 10.1159/000486916. [DOI] [PubMed] [Google Scholar]
- 57.Xiang Y, Guo J, Peng YF, Tan T, Huang HT, Luo HC, Wei YS. Association of miR-21, miR-126 and miR-605 gene polymorphisms with ischemic stroke risk. Oncotarget. 2017;8:95755–95763. doi: 10.18632/oncotarget.21316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu J, Du K, Lu X. Elevated expressions of serum miR-15a, miR-16, and miR-17-5p are associated with acute ischemic stroke. Int J Clin Exp Med. 2015;8:21071–21079. [PMC free article] [PubMed] [Google Scholar]
- 59.Becker KJ. Inflammation and the silent sequelae of stroke. Neurotherapeutics. 2016;13:801–810. doi: 10.1007/s13311-016-0451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gibbs WS, Weber RA, Schnellmann RG, Adkins DL. Disrupted mitochondrial genes and inflammation following stroke. Life Sci. 2016;166:139–148. doi: 10.1016/j.lfs.2016.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jimenez MC, Rexrode KM, Kotler G, Everett BM, Glynn RJ, Lee IM, Buring JE, Ridker PM, Sesso HD. Association between markers of inflammation and Total stroke by hypertensive status among women. Am J Hypertens. 2016;29:1117–1124. doi: 10.1093/ajh/hpw050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang X, Chappell FM, Valdes Hernandez M, Lowe G, Rumley A, Shuler K, Doubal F, Wardlaw JM. Endothelial function, inflammation, thrombosis, and basal ganglia perivascular spaces in patients with stroke. J Stroke Cerebrovasc Dis. 2016;25:2925–2931. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of this study was available from the corresponding authors as requested.