Abstract
Recent evidence has extensively demonstrated the anticancer potential of nutraceuticals, including plant polyphenols. Polymeric nanocarrier systems have played an important role in improving the physicochemical and pharmacological properties of polyphenols, thus ameliorating their therapeutic effectiveness. This article summarizes the benefits and shortcomings of various polymeric systems developed for the delivery of polyphenols in cancer therapy and reveals some ideas for future work.
Keywords: cancer therapeutics, polymeric carriers, nanoparticles, polyphenols, cell lines
1. Introduction
A large number of food ingredients have beneficial effects on human health. In particular, during the last decade, polyphenols and antioxidants have been extensively investigated for their therapeutic effectiveness after their intravenous administration [1].
Polyphenols contain a minimum of one aromatic ring, as well as hydroxyl groups ranging from a minimum of one ring. They are different from each other on the basis of the number of aromatic rings and phenol groups [2] and can be grouped into two main classes: flavonoids and non-flavonoids [3]. The former contains 15 carbon atoms, comprising two aromatic rings connected by a three-carbon link, while the latter contains heterogeneous compounds with phenolic acids having between one and six carbon atoms. Quercetin, kaempferol, apigenin, and myricetin belong to flavonoid class, while resveratrol, vanillin, and ellagitannins are examples of non-flavonoids.
Polyphenols are biologically active compounds, having useful effects against various chronic diseases, including cancer [4]. The biological activities of polyphenols are generally attributed to their antioxidant potential [5]. However, a comprehensive explanation for the biological effects of polyphenols is still uncertain [6]. In addition, their effects are also believed to be modulated via distinct actions on the signaling pathways at a cellular level [7].
Clinical studies on cancer therapy have reported a significant decrease in the therapeutic effectiveness of conventional cytotoxic compounds. The reduced efficacy is not only attributed to their unsuitable physicochemical properties, such as lipophilicity, but also to inappropriate pharmacokinetic features, including multidrug resistance, poor penetration into tumor microenvironment, and toxicity to non-diseased cells [8,9,10]. A wide array of research activities has been conducted to decipher these issues by several approaches, including the investigation of alternative anticancer compounds, as well as the development of targeted nanotherapeutics.
2. Polyphenol-Loaded Polymeric Nanotherapeutics for Cancer Treatment
The pathophysiology of cancer involves molecular-level changes in biological processes. Thus, in recent years, approaches have emerged to develop nanodiagnostic and nanotherapeutic modalities, such as lipid nanoparticles, nanohybrids, and polymeric nanoparticles [11,12,13]. In preclinical and initial clinical trials, these nanocarriers have exhibited excellent performance as drug delivery vehicles [14,15,16]. Nano-sized drug delivery systems have several promising features, including improved stability, enhanced solubility, and increased surface area to volume ratio. In addition, the surface properties of such carriers can be modified to attain controllable pharmacological and physicochemical features, thereby reducing barriers to effective chemotherapy in cancer [17]. Additionally, an ameliorated therapeutic index and diminished toxicity to healthy cells are also achieved through the nanotherapeutic approach [17]. It is remarkable that active and passive targeting could be used to deliver drugs to specific sites. These properties are significantly important for typical biologically active compounds, such as polyphenols for their translation into useful therapeutic modalities. Regardless of the promising progress in basic cancer biology at the preclinical level, polyphenols have inappropriate pharmacological properties, such as low bioavailability due to inefficient systemic access, and thus require high doses for optimum therapeutic effect [18]. Although in vitro studies have proved the biological effectiveness of polyphenols, these findings could not be achieved in vivo due to their instability in the physiological conditions of temperature, pH, and enzyme system. Their stability and therapeutic effectiveness could be improved by developing polyphenol-loaded nanotherapeutics. Therefore, biologically active polyphenols could be combined with nano-sized carriers to overcome the drawbacks of conventional anticancer therapy and develop a clinically efficacious treatment for cancer.
2.1. Polymer-Based Nanovesicles
Polymeric vesicles are prepared using amphiphilic block copolymers, which contain a lipophilic and a hydrophilic segment. These self-assembled structures have variable shapes and sizes, such as polymersomes [19] and micelles [20]. These vesicular systems have drug delivery capabilities and offer specific benefits.
Polymersomes are bilayered vesicles, composed of high molecular weight amphiphiles. Thus, they allow slow permeability of drugs due to the strong mechanical properties of their membranes [21]. Additionally, the surface of polymersomes is modified by using shell-producing, water-soluble, flexible polymers to reduce polymersomes–macrophages interactions [22]. Moreover, polymeric micelles are composed of a lipophilic core and a hydrophilic shell, into which lipophilic and hydrophilic drugs can be loaded and delivered, respectively [21]. These vesicles exhibit a narrow size distribution, ranging between 20 and 80 nm, and are long-lasting in systemic circulation [23,24,25], but, due to their poor stability, they undergo premature drug leakage in the bloodstream, resulting in reduced therapeutic efficacy and enhanced undesired effects. Polyphenol-loaded polymersomes and micelles have been synthesized by using natural polymers, such as dextran, chitosan, gelatin, casein, and polyethylene glycols PEG, due to their biodegradable and biocompatible features Table 1 and Table 2.
Table 1.
Polyphenol-loaded polymersomes for the treatment of cancer.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model/In Vivo Model Promisingly Ttreated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Polyvinyl pyrrolidone–PEG | Emulsion evaporation | Plant polyphenols | Glioblastoma DBTRG-05MG | [28] |
| 2 | Keratin | Solvent evaporation | Curcumin | Cervical cancer HeLa | [29] |
| 3 | Gelatin | Solvent evaporation | Curcumin | Lung cancer H1299 | [30] |
| 4 | PEG–Oleic acid | Thin layer evaporation | Curcumin | Brain cancer U87MG | [42] |
PEG: polyethylene glycol.
Table 2.
Polyphenol-loaded polymeric micelles for the treatment of cancer.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model/In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Gelatin–Dextran | Self-assembly-Genipin-Crosslinking | Plant polyphenols | Breast cancer MCF-7 | [26] |
| 2 | Gelatin–Dextran | Self-assembly-Genipin-Crosslinking | Curcumin | Cervical cancer HeLa Healthy mice | [27] |
| 3 | Casein | Self-assembly | Curcumin | Cervical cancer HeLa | [32] |
| 4 | Zein–PEG | Self-assembly | Curcumin | Ovarian cancer NCI Healthy mice | [33] |
| 5 | Chitosan–Stearic acid | Self-assembly | Curcumin | Colon cancer Primary Xenograft mice | [34] |
| 6 | PEG–Polyanhydride esters | Solvent evaporation | Curcumin | Cervical cancer HeLa | [35] |
| 7 | PEG–Polylactic acid | Solvent evaporation | Curcumin + Doxorubicin | Breast cancer MCF-7 Xenograft mice | [36] |
| 8 | PEG–Polycaprolactone | Thin-layer evaporation | Curcumin | Ovarian cancer A2780t | [38] |
| 9 | PEG–Polycaprolactone | Thin-layer evaporation | Curcumin | Breast cancer MDA-MB-436 | [37] |
| 10 | PEG–Polycaprolactone | Self-assembly | Curcumin | Breast cancer 4T1–4T1 Xenograft mice | [40] |
| 11 | PEG–Polycaprolactone | Thin-layer evaporation | Curcumin | Cervical cancer HeLa Xenograft mice | [39] |
| 12 | PEG–Polycaprolactone | Thin-layer evaporation | Curcumin | Colon HT-29 | [39] |
| 13 | PEG–Polycaprolactone | Thin-layer evaporation | Curcumin + Doxorubicin | Lung cancer LL/2 Xenograft mice | [41] |
| 14 | Linoleic acid-PEG-Polycaprolactone | Self-assembly | Curcumin | Cervical cancer HeLa Healthy mice | [43] |
| 15 | Linoleic acid-PEG-Polycaprolactone | Self-assembly | Curcumin | Lung A549 | [43] |
| 16 | PEG -Palmitic acid | Self-assembly | Curcumin | Cervical cancer HeLa | [32] |
| 17 | PEG2000-DSPE | Thin-layer evaporation | Curcumin + Paclitaxel | Ovarian cancer SK-OV-3TR | [45] |
| 18 | PEG2000-DSPE | Thin-layer evaporation | Curcumin + Paclitaxel | Ovarian cancer NCI SK-OV-3TR Xenograft mice | [46] |
| 19 | PEG2000-DSPE | Thin-layer evaporation | Curcumin + Doxorubicin | Colon cancer HCT-116 Xenograft mice | [44] |
| 20 | PEG- Doxorubicin | Self-assembly | Curcumin + Doxorubicin | Cervical cancer HeLa HepG2 Xenograft mice | [47] |
| 21 | PEG-Doxorubicin | Self-assembly | Curcumin + Doxorubicin | Hepatic HepG2 | [47] |
| 22 | Poloxamers F127 F68 | Thin-layer evaporation | Curcumin | Cervical cancer HeLa | [48] |
| 23 | Poloxamers-PEG-Succinate | Solvent evaporation | Curcumin | Ovarian cancer NCI | [49] |
| 24 | Poloxamers F127 | Thin-layer evaporation | Resveratrol, Curcumin + Doxorubicin | Ovarian cancer SKOV-3 Healthy mice | [50] |
| 25 | Poloxamers F127 | Thin-layer evaporation | Resveratrol, Quercetin + Doxorubicin | Ovarian cancer SKOV-3 Healthy mice | [31] |
| 26 | Apolipoprotein-E3 | recombinant DNA | Resveratrol | Glioblastoma A-172 | [51] |
| 27 | Polycaprolactone-PEG-Succinate | Thin-layer evaporation | Resveratrol | Breast cancer MCF-7 | [52] |
| 28 | Casein | Self-assembly | Epigallocatechin gallate | Colon cancer HT-29 | [53] |
| 29 | Polylactic acid-PEG | Thin-layer evaporation | Epigallocatechin gallate | Pancreatic cancer MiaPaca-2 | [54] |
Note: PEG2000-DSPE—1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[methoxypolyethylene glycol-2000].
Gelatin–dextran micelles loaded with tea polyphenols were studied for their effect on breast cancer using MCF-7 cells and it was found that the encapsulated polyphenols had an enhanced efficacy compared with their free form [26]. Later on, this carrier was loaded with curcumin for the treatment of HeLa cancer cells. The results revealed an improvement in the pharmacokinetic and therapeutic properties of the encapsulated curcumin, compared with its control [27]. In addition, polyvinyl pyrrolidone–PEG conjugates were used to develop polymersomes loaded with Cotinus coggygria flavonoids for the treatment of glioblastoma [28]. Moreover, curcumin delivery systems were prepared by using protein-type polymers, such as gelatin, casein, and keratin [29,30,31,32,33]. In addition to their biocompatibility, these materials supported curcumin’s efficacy on cancerous cells of the lung and cervix [29,30]. Curcumin-loaded chitosan–stearic acid conjugates exhibited an improvement in the curcumin efficiency against colon cancer [34]. Curcumin polymersomes and micelles have been prepared with an aim of enhancing their anticancer activity. Owing to its stealth properties and biocompatible nature, PEG is extensively used in the fabrication of nanoparticulate systems. In vitro testing of PEG–polyanhydride esters and PEG–polylactic acid vehicles for curcumin and doxorubicin showed their synergism in HeLa and MCF-7 cancer cells. The polymer conjugates were prepared by a solvent evaporation technique [35,36]. The solvent evaporation-induced synthesis of curcumin-loaded micelles of polycaprolactone and PEG was aimed at the treatment of various cancers, such as breast [37] and ovarian [38] cancer cells in vitro, and colon [39], breast [40], and lung [41] in xenograft mouse models. The anticancer efficacy of these polycaprolactone–PEG–curcumin nanomicelles against lung and brain tumors was further enhanced through their modification by using different fatty acids, such as oleic acid, linoleic acid, and palmitic acid [42,43]. In some other studies, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[methoxypolyethylene glycol-2000] was employed for the synthesis of curcumin micelles to treat colon and ovarian cancers in vitro and in vivo, showing synergism with doxorubicin [44,45] and paclitaxel [46]. These in vitro and in vivo studies depict the promising characteristics of the polymeric polymersomes and micelles for delivering various polyphenols, including curcumin.
Favorable disposition of curcumin and doxorubicin was achieved when these drugs were combined in PEG micelles for cervical and hepatic cancer [47]. Few studies have documented a profound toxicity of curcumin-loaded poloxamer nanocarriers towards HeLa [48] and ovarian cancer cells [49]. In addition, poloxamer nanoformulations containing resveratrol and doxorubicin exhibited a synergistic effect on ovarian cancer in mice [50]. A resveratrol–quercetin combination exhibited the same effect in ovarian tumors [51]. Moreover, resveratrol was encapsulated into PEG–polycaprolactone conjugate, and the resulting micelles were surface-modified with apolipoprotein and used for the treatment of glioblastoma [51] and breast cancer [52]. Lastly, some other studies reported epigallocatechin gallate delivery in colon cancer from PEG–polylactic acid [53] and in pancreas cancer from casein micelles [54]. The micelles of various polymers, such as PEG and polycaprolactone, showed an improved anticancer efficacy of the loaded polyphenols, such as quercetin, resveratrol, and curcumin.
2.2. Polymer-Based Nanoparticles
High stability, uniform particle size, excellent drug loading efficiency, and controlled release of drug are important characteristics of polymeric nanoparticles [55], which are spherical or irregular shaped, colloidal systems loaded with drugs [56]. A wide range of biocompatible, natural, and synthetic polymers have been utilized as polymeric nanoparticles to deliver anticancer drugs [57,58]. Table 3 illustrates the representative examples of polymers used as nanoparticles for the delivery of polyphenols. Due to their biocompatible and biodegradable features, chitosan and polylactic-co-glycolic acid PLGA have been extensively studied for polyphenol delivery [59]. To prevent the uptake of nanoparticles by macrophages, the surface functionalization of nanoparticles can be modified by using polyethylene glycol PEG and its derivatives [60]. The selection of the procedure for the fabrication of polymeric nanoparticles depends on various factors, such as the properties of the employed polymer, drug, and the desired end product to achieve the desired, controllable physicochemical and pharmacological performance in vitro and in vivo. Table 4 also depicts some extensively employed approaches, such as emulsion solvent removal, polymer interaction, and radical polymerization.
Table 3.
Polyphenol-loaded polymeric nanoparticles for the treatment of cancer in vitro.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Polylactic-co-glycolic acid PLGA–PEG | Emulsion solvent evaporation | Pomgranade polyphenols | Breast cancer MCF-7, Hs578T | [61] |
| 2 | Chitosan | Ionic gelation | Tea polyphenols | Hepatic cancer Hep G2 | [62] |
| 3 | Polycaprolactone | EXP | Plant polyphenols | Gastric cancer MNK28 | [63] |
| 4 | Alginate–Chitosan–Poloxamers F127 | Ionic gelation | Curcumin | Cervical cancer HeLa | [64] |
| 5 | Fibrinogen | CaCl2 Crosslinking | Curcumin | Prostate cancer PC3 | [65] |
| 6 | PLGA | Emulsion solvent evaporation | Curcumin | Breast cancer MCF-7 | [65] |
| 7 | PLGA | Emulsion solvent evaporation | Curcumin | Osteosarcoma U2OS | [66] |
| 8 | Chitin | Emulsion solvent evaporation | Curcumin | Melanoma A375 | [67] |
| 9 | Peptide | Ionic gelation | Curcumin | Medulloblastoma DAOY | [68] |
| 10 | N-Isopropylacrylamide-N-vinyl-2-pyrrolidone-Polyethylene glycol acrylate | Self-assembly | Curcumin | Pancreatic cancer Capan-1, MiaPaCa2, PL-5, PL-8, Su86.86, BxPC-3, PANC-1, E3LZ10.7 Healthy mice | [69] |
| 11 | PLGA–PEG | Nanoprecipitation | Curcumin | Colon cancer HT-29 Healthy mice | [70] |
| 12 | PLGA | Nanoprecipitation | Curcumin | Ovarian cancer A2780, A2780CP | [71] |
| 13 | Cellulose | Nanoprecipitation | Curcumin | Prostate cancer C4-2, PC-3, LNCaP, DU-145 | [72] |
| 14 | PLGA | Nanoprecipitation | Curcumin | Prostate cancer DU-145, PC-3 Xenograft mice | [73] |
| 15 | Human serum albumin | Emulsion solvent evaporation | Curcumin | Colon cancer HCT116 HCT116 Xenograft mice | [74] |
| 16 | Human serum albumin | Emulsion solvent evaporation | Curcumin | Pancreatic cancer MiaPaCa2 | [74] |
| 17 | Gelatin–Polyacryl-amidoglycolic acid | Emulsion polymerization | Curcumin | Colon cancer HCT-116 | [75] |
| 18 | Silk fibroin | Physical adsorption and coprecipitation | Curcumin | Human hepatocellular carcinoma Hep3B, human neuroblastoma Kelly cells, Human bone marrow-derived mesenchymal stem cells hBMSCs | [76] |
| 19 | Chitosan–Polybutyl cyanoacrylate | Emulsion polymerization | Curcumin + Doxorubicin | Breast cancer MCF-7 | [77] |
| 20 | PLGA | Emulsion solvent evaporation | Curcumin + 5-fluorouracil | Breast cancer MCF-7 | [78] |
| 21 | PLGA | Nanoprecipitation | Curcumin + Cisplatin | Ovarian cancer A2780CP | [79] |
| 22 | PLGA | Nanoprecipitation | Curcumin + Cisplatin | Breast cancer MDA-MB-231 | [79] |
| 23 | N-Isopropylacryl-amide-N-vinyl-2-pyrrolidone–Acrylic acid | Radical polymerization | Curcumin + Gemcitabine | Pancreatic cancer Pa03C Xenograft mice | [80] |
Table 4.
Polyphenol-loaded polymeric nanoparticles for the treatment of cancer in vitro.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Gelatin–Polyelectrolyte | Layer-by-layer | Epigallocatechin gallate | Breast cancer MBA-MD-231 | [81] |
| 2 | PLGA–PEG | Nanoprecipitation | Epigallocatechin gallate | Prostate cancer LNCaP | [82] |
| 3 | Casein-phospho-peptide–Chitosan | Genipin-Crosslinking | Epigallocatechin gallate | Hepatic cancer HepG2 | [83] |
| 4 | Casein-phospho-peptide–Chitosan | Genipin-Crosslinking | Epigallocatechin gallate | Gastric cancer BGC823 | [83] |
| 5 | Casein-phospho-peptide–Chitosan | Genipin-Crosslinking | Epigallocatechin gallate | Colon cancer Caco-2 | [84] |
| 6 | Hyaluronic acid | Self-assembly | Epigallocatechin gallate + Doxorubicin | Cancer of the external auditory canal | [85] |
| 8 | Chitosan | Ionic gelation | Epigallocatechin gallate | Prostate cancer 22R_1 Xenograft mice | [87] |
| 7 | Chitosan | Ionic gelation | Epigallocatechin gallate | Melanoma Mel928 Mel928 Xenograft mice | [88] |
| 9 | Chitosan–Gelatin–PEG | Ionic gelation | Epigallocatechin gallate | Gastric cancer Luc MKN45 Xenograft mice | [88] |
| 10 | PLGA | Nanoprecipitation | Epigallocatechin gallate + Cisplatin | Lung cancer A549 | [89] |
| 11 | PLGA | Nanoprecipitation | Epigallocatechin gallate + Cisplatin | Cervical cancer HeLA | [89] |
| 12 | PLGA | Nanoprecipitation | Theaflavin | Leukemia THP-1 | [89] |
| 13 | PLGA | Solvent evaporation | Epigallocatechin gallate + Cisplatin | Lung cancer A549 Ehrlich ascites carcinoma Xenograft mice | [90] |
| 14 | PLGA | Solvent evaporation | Epigallocatechin gallate | Cervical cancer HeLA | [90] |
| 15 | PLGA | Solvent evaporation | Theaflavin | Leukemia THP-1 | [90] |
| 16 | PLGA | Solvent evaporation | Theaflavin | Cancer of the external auditory canal | [90] |
| 17 | PLGA–PEG | Nanoprecipitation | Resveratrol | Prostate cancer DU-145, LNCaP | [91] |
| 18 | Bovine serum albumin | Nanoprecipitation | Resveratrol | Lung cancer NCI-H460 | [92] |
| 19 | Bovine serum albumin | Nanoprecipitation | Resveratrol | Ovarian cancer SKOV3 | [93] |
| 20 | PLGA | Emulsion method | Resveratrol | Breast cancer MCF-7 | [94] |
| 21 | Maleimide–PEG–Polylactic acid | Self-assembly | Resveratrol | Glioblastoma CT26, U87 CT26 Xenograft mice | [95] |
| 22 | Chitosan | Ionic gelation | Quercetin + 5-fluorouracil | Pancreas cancer MiaPaCa2 | [96] |
| 23 | PLGA | Emulsion solvent evaporation | Quercetin + Tamoxifen | Breast cancer MCF-7 Xenograft mice | [97] |
| 24 | PLGA | Emulsion solvent evaporation | Quercetin + Tamoxifen | Colon cancer Caco2 | [97] |
| 25 | Hyaluronic acid–Polybutyl cyanoacrylate–a-Tocopheryl–PEG–Succinate | Radical polymerization | Morin hydrate | Lung cancer A549 S180 Xenograft mice | [98] |
| 26 | Hyaluronic acid–Polybutyl cyanoacrylate –Tocopheryl–PEG–Succinate | Radical polymerization | Morin hydrate | Hepatic cancer L02 | [98] |
Compared with free polyphenols, polyphenol extracts loaded into chitosan, PLGA– polycaprolactone nanoparticles exhibited boosted apoptosis induction and cell internalization, resulting in the enhanced antiproliferative activity in various cell line studies [61,62,63].
Curcumin is a pharmacologically active polyphenol with low water solubility. Therefore, many studies have been conducted to prepare its effective formulations. In this context, an important effort is the development of curcumin-loaded nanoparticles. Therapeutic studies involving various cancer cell lines, including cervical and prostate cells, osteoclasts, and melanocytes [64,65,66,67,68], revealed that these nanoparticles exhibited controlled release of curcumin, resulting in effective passive targeting. It is noteworthy that both free curcumin and curcumin-loaded nanoparticles have the same mechanism of action. In addition, curcumin-loaded nanoparticles have been synthesized by a free radical polymerization method using polyethylene glycol acrylate, N-isopropylacrylamide, and N-vinyl-2-pyrrolidone for the treatment of pancreatic cancer. These nanoparticles showed insignificant toxicity in mouse [69]. Another study reported the synthesis of curcumin-loaded nanoparticles by an emulsion polymerization method using chitosan and butyl-cyanoacrylate together for the treatment of hepatic cancer [69]. In addition, free curcumin and curcumin nanoparticles were compared in various cell lines, such as colon, prostate, and ovarian. The nanoparticles of curcumin induced cellular uptake and the apoptosis boosting resulting in the ameliorated anticancer activity than its free form [70,71,72]. PLGA nanoparticles containing PEG were fabricated to improve curcumin efficacy against prostate and colon cancer [73,74,75], while curcumin–silk fibroin nanoparticles have been shown to have a potential role in human hepatocellular carcinoma Hep3B, human neuroblastoma Kelly cells, and human bone marrow-derived mesenchymal stem cells hBMSCs [76]. Moreover, curcumin was encapsulated into pH-responsive nanogels to enhance its efficacy against colon cancer [75]. To achieve a synergistic effect, curcumin nanoparticles containing conventional anticancer drugs, such as doxorubicin [77] and 5-fluorouracil [78], have been employed for breast cancer treatment. For the treatment of ovarian cancer, a useful association between curcumin- and cisplatin-loaded nanoparticles has been noted [79]. Furthermore, curcumin combined with gemcitabine in nanoparticles, prepared by free radical polymerization using N-isopropylacrylamide, N-vinyl-2-pyrrolidone, and acrylic acid, exhibited a synergistic anticancer effect in animal models [80]. Thus, compared to that of free curcumin, curcumin nanoparticles induce cellular uptake, and the apoptosis boosting leads to increased anticancer activity in various cell lines, such as colon, prostate, and ovarian.
Using natural polymers, such as gelatin [81] and a PLGA–PEG combination [82], as well as synthetic polymers, including chitosan–casein–PEG derivatives [82], the synthesis of epigallocatechin gallate nanoparticles with improved stability and in vitro activity against various organs, such as prostate, alimentary canal, breast, and stomach [81,82,83,84], was achieved. Furthermore, epigallocatechin gallate nanoparticles containing doxorubicin were prepared which exhibited a synergistic anticancer effect against Ehrlich ascites cancer [85]. In vivo studies in xenograft mice have also proved the effective stability and activity of epigallocatechin gallate nanoparticles against stomach, prostate, and melanocyte carcinoma [86,87,88]. In addition, epigallocatechin gallate combined with cisplatin in a nanoparticulate formulation was developed as a new synergistic therapy for some invasive cancers [89,90].
Some studies reported the nanoencapsulation of resveratrol into bovine serum albumin [91], gelatin [92], PLGA [93], and PLGA–PEG derivatives [94], revealing an increase in resveratrol activity against cancer of various organs, such as prostate, ovaries, breasts, and lungs [91,92,93,94]. Resveratrol-loaded PLGA–PEG nanoparticles were surface-modified using transferrin for active targeting of glioma cancer cells in vivo [95].
Quercetin and 5-fluorouracil were co-encapsulated into chitosan, and the resulting nanoparticles showed a synergistic effect against pancreatic cells in vitro [96]. Another synergistic study described the promising potential of quercetin–tamoxifen loaded into PLGA nanoparticles for the treatment of breast cancer in model mice [97]. Lastly, a four-component system was formulated using poly-butyl cyanoacrylate, α-tocopherol, and PEG for the delivery of hyaluronic acid into liver cancerous cells in vitro [98]. The preparation of nanoparticles loaded with epigallocatechin gallate, resveratrol, quercetin, and 5-fluorouracil with improved stability and in vitro activity against various organs, such as stomach, prostate, ovaries, alimentary canal, and breast, can be achieved using various natural polymers, such as gelatin, PEG, and PLGA, alone and in combination with synthetic polymers, such as chitosan and casein.
2.3. Polymer-Based Conjugates
An important class of the emerging systems for the treatment of cancer is polymer-based conjugates, which consist of a drug molecule and a hydrophilic polymeric macromolecule covalently bonded to each other. In recent years, tremendous research has been conducted to explore new and functional therapeutic conjugates. Like nanoparticles, polymeric conjugates are also high molecular weight systems that affect a drug’s pharmacokinetics, toxicity, and efficacy [99].
Polymer–drug conjugate–a water-soluble system is composed of a drug-associating unit, another unit for linking an active targeting molecule, such as monoclonal antibody, and a portion for linking an element useful for the modulation of physicochemical features [100]. The therapeutic potential of polymeric conjugates is profoundly improved by using antioxidant polymers, which can be acquired either by the conjugation of polyphenol monomers with macromolecules or the polymerization of monomer units of polyphenols. High molecular weight antioxidants can be prepared by three different approaches, namely, enzymatic catalysis, condensation, and radical grafting [101].
Enzymatic catalysis refers to the catalyst-mediated chemical reaction between non-toxic reagents in milder reaction conditions of pH, temperature, and pressure, resulting in the synthesis of distinct structures having controlled chemical properties [102]. In general, a peroxidase or a tyrosinase is used as the catalyst in a coupling reaction.
In condensation reactions, the functional groups of an antioxidant molecule and a polymeric chain react with each other, producing well-defined products with specific mechanical and physical features. As a result of these reactions, the mechanical properties of the product are similar to those of the parent materials. Esterification and acetylation are two important examples of condensation reactions. Generally, these reactions take place in several steps.
Lastly, the radical grafting approach involves free radical coupling between the polyphenol unit and the polymeric moiety in the presence of mild reaction conditions [103], resulting in the synthesis of a characteristic product that retains chemical features of the parent polyphenols.
Polyphenol-loaded polymeric conjugates for the treatment of cancer are summarized in Table 5. For the treatment of pancreatic cancer, a curcumin–gemcitabine combination was loaded with PEG conjugates through a condensation reaction in the presence of carbodiimide [104]. Also, PEG conjugates containing just curcumin have also been prepared for prostate [105] and glioma cancer [106]. Through the same conjugation technique, synergistic cytotoxicity was achieved with resveratrol–bicalutamide–PEG conjugates in breast and cervical cancer cells [107] and quercetin–paclitaxel–carboxymethyl chitosan conjugates in hepatic cancer cells [108]. Another study reported the synthesis of curcumin–dithiopropionic acid copolymer, followed by conjugation with PEG [109]. PEG hydrogels containing triphosgene–curcumin conjugates showed an increased effect against proliferation in breast cancer cells [110].
Table 5.
Polyphenol-loaded polymeric conjugates for the treatment of cancer.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | PEG | Condensation method | Curcumin | Glioma C6 | [106] |
| 2 | PEG | Condensation method | Curcumin | Prostate cancer PC-3 | [105] |
| 3 | PEG | Condensation method | Curcumin + Gemcitabine | Pancreatic cancer MiaPaCa2, PANC-1, BxPC-3, AsPC-1 | [104] |
| 4 | PEG | Condensation method | Resveratrol + Bicalutamide | Cervical cancer HeLa | [107] |
| 5 | PEG | Condensation method | Resveratrol + Bicalutamide | Breast cancer MCF-7 | [107] |
| 6 | Carboxymethyl chitosan | Condensation method | Quercetin + Paclitaxel | Hepatic cancer HepG2 HepG2 Xenograft mice | [108] |
| 7 | PEG | Condensation method | Curcumin | Cervical cancer HeLa, Breast cancer EMT6 EMT6 Xenograft mice | [109] |
| 8 | PEG–Desaminotyrosyl-tyrosine ethyl ester | Condensation method | Curcumin | Breast cancer MDA-MB-231 | [110] |
| 9 | PEG | Condensation method | Catechin + Bortezomib | Breast cancer MDA-MB-231 | [111] |
| 10 | Hyaluronic acid–Polyethyleneimine | Condensation method | Epigallocatechin gallate + Granzyme B | Colon cancer HCT-116 | [112] |
| 11 | Dextran | Free radical grafting | Catechin | Pancreatic cancer MiaPaca-2, PL45 | [113] |
| 12 | Dextran | Free radical grafting | Catechin | Neuroblastoma IMR-32, IMR-32-CisRes, BE2-C Xenograft mice | [114] |
| 13 | Dextran | Enzyme laccase catalysis | Catechin | Neuroblastoma IMR-32 | [114] |
| 14 | Polymethacrylic acid | Free radical grafting | Quercetin | Cervical cancer HeLa | [115] |
| 15 | Gelatin | Free radical grafting | Gallic acid | Prostate cancer DU-145, PC-3 | [116] |
| 16 | Gelatin | Free radical grafting | Gallic acid | Renal cancer A498 | [116] |
Compared with the free forms of the tested polyphenols, the anticancer activity of PEG–catechin amides against breast cancer was synergistically increased in the presence of bortezomib [111]. Therapeutic synergism was also observed when hyaluronic acid–epigallocatechin gallate amides containing granzyme B were tested against colon cancer [112]. The therapeutic analysis of catechin–dextran conjugates showed the increased efficacy of catechin in pancreatic cancer cells [113] and in a neuroblastoma model animal [114]. Other studies showed an increase in the anticancer activity of quercetin-loaded polymethacrylic acid conjugates towards cervical cancer [115] and gallic acid-loaded gelatin conjugates towards cervical cancer [116]. All these conjugates were prepared by a free radical approach. For the treatment of hepatic, pancreatic, prostate, glioma, and breast cancer, curcumin, resveratrol, and quercetin in combination with standard anticancer agents, such as paclitaxel, gemcitabine, or bortezomib, have been successfully loaded to polymeric conjugates.
2.4. Carbon-Based Nanostructures and Nanohybrids
A class of nano-sized materials, known as carbon nanostructures, is extensively being investigated for its therapeutic applications [117]. The representative examples of this interesting group of compounds are graphene and carbon nanotubes because of their good permeability, cheap availability, excellent physicochemical features, and large surface area for the likely interaction with bioactive compounds [118,119].
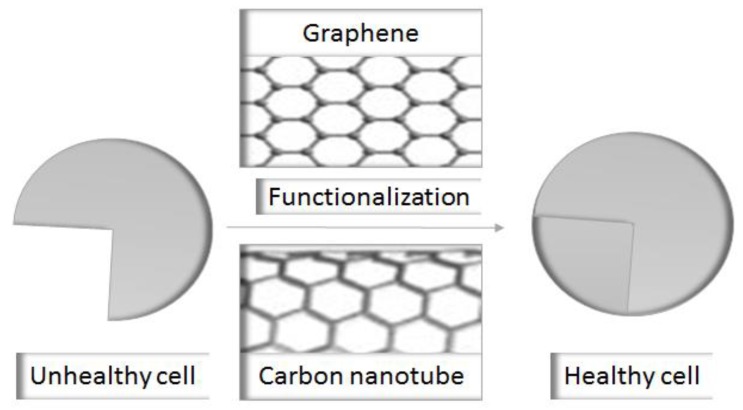
Graphene is a bidimensional honeycomb-like structure, consisting of a layer of six sp2 carbon atoms [120]. These bodies undergo cell internalization through endocytosis or active processes [121]. Graphene oxide, an oxidative product of graphene, is an efficient drug delivery vehicle, because it contains numerous functionalities, such as carboxylic and hydroxyl groups Figure 1 [122].
Figure 1.
A schematic representation showing the ameliorated effect of functionalization on the cytocompatibility of graphene and carbon nanotubes.
Carbon nanotubes are obtained by the condensation of benzene rings having a composition of sp2 carbons, prepared as tube-like structures with a single layer single-walled carbon nanotubes or multiple layers multiple-walled carbon nanotubes [123]. Carbon nanotubes have a strong affinity with different proteins and undergo spiraling movement, thus they are efficiently uptaken by cells, revealing their promising membrane permeability [124].
Graphene oxide and carbon nanotubes are suitable drug delivery vehicles due to their quick physiological distribution, accumulation in various organs, including liver, lungs, kidney, and stomach, and excretion through bile and urine [125,126,127]. In addition, graphene oxide is a biocompatible and cytotoxic substance [128,129]. However, carbon nanotubes could be toxic and produce inflammation, necrosis, fibrosis, and granuloma due to their reducing potential: this feature of carbon nanotubes may hinder their use in drug delivery [129].
These toxicity problems can be eliminated by combining these materials with biocompatible, water-soluble compounds, especially polymers, generating carbon nanohybrids [130].
Numerous studies have reported the successful application of graphene oxide and carbon nanotubes in drug delivery for cancer therapy [131]; however, only a few studies describe their role in the delivery of polyphenols. For instance, a promising modality describes the polyphenol-induced reduction of graphene oxide, resulting in the bond formation between polyphenols and graphene oxide [132]. In this regard, tea polyphenol extract nanohybrids exhibited an improved antiproliferative action in colon cancer cells [133]. Similarly, the proliferation was profoundly inhibited by resveratrol nanohybrids in ovarian cancer cells [134].
On the other hand, pristine carbon nanotubes have been used in some studies for the delivery of polyphenols [135]. Owing to their toxic features, carbon nanotubes have been made biologically compatible by coating with suitable polymers, including gelatin Table 6. In this context, multiple-walled carbon nanotubes were combined with polycaprolactone, resulting in the formation of nanohybrids. These nanohybrids loaded with tea polyphenol exhibited a promising therapeutic effect towards hepatic and lung cancer [136].
Table 6.
Polyphenol-loaded carbon-based nanohybrids for the treatment of cancer.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model/In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Graphene oxide | Reduction method | Tea polyphenols | Colon cancer HT29, SW48 | [133] |
| 2 | Graphene oxide | Reduction method | Resveratrol | Ovarian cancer A2780 | [134] |
| 3 | Polycapro-lactone–MWNT | Electrospinning | Tea polyphenols | Lung cancer A549 | [136] |
| 4 | Polycapro-lactone–MWNT | Electrospinning | Tea polyphenols | Hepatic HepG2 | [136] |
| 5 | Gelatin–MWNT | Coating | Catechin + Radiotherapy | Prostate cancer DY-145, PC-3, LNCap | [138] |
| 6 | Gelatin–MWNT | Coating | Catechin | Cervical cancer HeLa | [139] |
| 7 | Polymeth-acrylic acid–MWNT | Radical coupling | Quercetin | Cervical cancer HeLa | [137] |
| 8 | Polymeth-acrylic acid–MWNT | Radical coupling | Quercetin + Cisplatin | Neuroblastoma IMR-32 | [140] |
Note: MWNT—Multiple-walled carbon nanotubes.
Functional nanohybrids Table 6 have also been prepared by developing covalent bonds between the polyphenol and the polymer through a radical reaction. In this regard, catechin–gelatin conjugate [137,138] and quercetin–methacrylic acid conjugate [139,140] were used as the coating material for multi-walled carbon nanotubes. The obtained nanotherapeutics were found to have enhanced anticancer activity in HeLa cancer cells, compared with the free flavonoids [137,139]. It is remarkable that a synergistic anticancer effect can be achieved by using these flavonoid nanohybrids and radiotherapy together towards neuroblastoma [140] and prostate cancer treatment [138]. All these studies demonstrated that carbon nanotubes and graphene oxide could be successfully utilized for the delivery of the polyphenols, including quercetin and catechins, for the effective treatment of cancer, including hepatic, prostate, and lung cancer.
2.5. Magnetic Nanoparticles Manipulation of Nanoparticles Using Magnetic Field
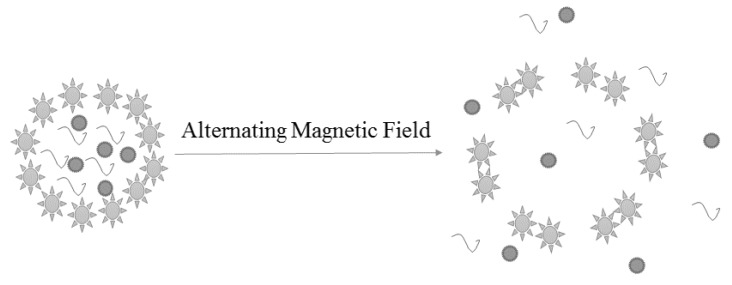
The nanoparticles modulated by a magnetic field, termed magnetic nanoparticles, are extensively studied drug delivery vehicles for the treatment of inflammation, cancer, and other chronic diseases [141,142]. In addition to remote actuation, an alternate magnetic field with high radiofrequency can be applied for the heating of nanoparticles Figure 2 to augment the microenvironment temperature and enhance the probability of synergism.
Figure 2.
A concept figure showing drug release from magnetic nanoparticles under the effect of alternating magnetic field.
In recent years, several studies Table 7 have reported the application of magnetic nanoparticle as a vehicle for the delivery of polyphenols for the treatment of tumors. It has been reported that curcumin conjugates possess profound cytotoxicity in Caco-2 cells, glioma [143], and breast cells [144]. Another study described the improved pharmacokinetics and cytotoxicity of curcumin–poloxamer nanoparticles, compared with curcumin alone [145]. Furthermore, magnetic nanoparticles coated with catechin–dextran conjugate exhibited an excellent anticancer activity towards pancreatic cancer [146]. A similar therapeutic outcome was observed when colon cancer cells were treated with epigallocatechin gallate–dextran conjugate [147]. The in vitro treatment of SMMC-7721 tumor cells with quercetin-loaded nickel nanoparticles exhibited synergism between the therapeutic effect and the permeability-enhancing effect of quercetin and nickel nanoparticles, respectively [148]. The nanocarriers for the delivery of polyphenols are studied in vivo to a limited extent, likely due to the fact that these nanoparticles, like any nano-sized drug delivery system, circulate for a short time in the blood as well as exhibit non-specific features. A representative study [147] reporting in vivo experiments on green tea-coated magnetic nanocrystals described their promising transport and uptake properties, suggesting their potential use in therapeutics and multimodal imaging.
Table 7.
Polyphenol-loaded magnetic nanoparticles for the treatment of cancer.
| No. | Components of Nanoparticles | Method of Preparation | Polyphenol + Synergistic Agent | Type of Cancer In Vitro Model/In Vivo Model Promisingly Treated with the Fabricated Nanotherapeutic Formulation | References |
|---|---|---|---|---|---|
| 1 | Hyaluronic acid–Iron | Layer-by-layer | Curcumin | Colon cancer Caco-2 | [143] |
| 2 | Polyvinyl pyrrolidone–Iron | Layer-by-layer | Curcumin | Glioma C6 | [143] |
| 3 | Iron–Poloxamers F127 | Nanopre-cipitation | Curcumin | Pancreatic cancer HPAF-II, Panc-1/Xenograft mice | [145] |
| Iron–Dextran | Solvation method | Catechin | Pancreatic cancer MIA Paca2 | [146] | |
| 4 | Iron | Reduction process | Epigallocatechin gallate | Colon cancer CT-26/Xenograft mice | [147] |
| 5 | Nickel | Electro-chemical deposition | Quercetin | Hepatic cancer SMMC-7721 | [148] |
3. Conclusions
In spite of extensive research struggles, the limitations to achieving effective cancer therapy are still unresolved. Similarly, natural products, including polyphenols, have been known for their anticancer effects for a long time, but their clinical use is still a dream. The above discussion reveals that the exclusive use of polyphenols as cancer therapy is inadequate for translation into therapeutic protocol; rather, due to the substantial synergism observed in study models, polyphenols can be suggested in combination with standard therapeutic modalities. Moreover, it is encouraging that a wide range of safe and effective polymeric nanoparticulate systems are available for the delivery of multiple compounds. Thus, polyphenols could be recommended for clinical use in the future.
Author Contributions
H.-Y.C. and G.M. conceived and designed the study. U.E., H.-Y.C., M.-J.X., Y.D.T., R.R. and G.M. executed the study. U.E. and G.M. analyzed the data. U.E., H.-Y.C., M.-J.X. and Y.D.T. contributed analysis tools. U.E., H.-Y.C., M.-J.X., Y.D.T., M.H.H.B.A., R.R., G.M. wrote the paper.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Cirillo G., Curcio M., Vittorio O., Lemma F., Restuccia D., Spizzirri U.G., Puoci F., Picci N. Polyphenol conjugates and human health: A perspective review. Crit. Rev. Food Sci. Nutr. 2016;56:326–337. doi: 10.1080/10408398.2012.752342. [DOI] [PubMed] [Google Scholar]
- 2.Nichenametla S.N., Taruscio T.G., Barney D.L., Exon J.H. A review of the effects and mechanisms of polyphenolics in cancer. Crit. Rev. Food Sci. Nutr. 2006;46:161–183. doi: 10.1080/10408390591000541. [DOI] [PubMed] [Google Scholar]
- 3.Del Rio D., Rodriguez-Mateos A., Spencer J.P.E., Tognolini M., Borges G., Crozier A. Dietary polyphenolics in human health, structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid. Redox. Signal. 2013;18:1818–1892. doi: 10.1089/ars.2012.4581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams R.J., Spencer J.P.E., Rice-Evans C. Flavonoids, antioxidants or signalling molecules? Free. Radic. Biol. Med. 2004;36:838–849. doi: 10.1016/j.freeradbiomed.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Yao L.H., Jiang Y.M., Shi J., Tomás-Barberán F.A., Datta N., Singanusong R., Chen S.S. Flavonoids in food and their health benefits. Plant Foods Hum. Nutr. 2004;59:113–122. doi: 10.1007/s11130-004-0049-7. [DOI] [PubMed] [Google Scholar]
- 6.Spencer J.P.E., Schroeter H., Crossthwaithe A.J., Kuhnle G., Williams R.J., Rice-Evans C. Contrasting influences of glucuronidation and O-methylation of epicatechin on hydrogen peroxide-induced cell death in neurons and fibroblasts. Free. Radic. Biol. Med. 2001;31:1139–1146. doi: 10.1016/S0891-5849(01)00704-3. [DOI] [PubMed] [Google Scholar]
- 7.Kong A.N.T., Yu R., Chen C., Mandlekar S., Primiano T. Signal transduction events elicited by natural products, role of MAPK and caspase pathways in homeostatic response and induction of apoptosis. Arch. Pharmacal. Res. 2000;23:1–16. doi: 10.1007/BF02976458. [DOI] [PubMed] [Google Scholar]
- 8.Luo Y., Prestwich G.D. Cancer-targeted polymeric drugs. Curr. Cancer Drug Targets. 2002;2:209–226. doi: 10.2174/1568009023333836. [DOI] [PubMed] [Google Scholar]
- 9.Luo J., Solimini N.L., Elledge S.J. Principles of cancer therapy, oncogene and non-oncogene addiction. Cell. 2009;136:823–837. doi: 10.1016/j.cell.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jemal A., Siegel R., Xu J., Ward E. Cancer statistics, 2010. CA Cancer J. Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 11.Gharpure K.M., Wu S.Y., Li C., Lopez-Berestein G., Sood A.K. Nanotechnology, future of oncotherapy. Clin. Cancer Res. 2015;21:3121–3130. doi: 10.1158/1078-0432.CCR-14-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pacardo D.B., Ligler F.S., Gu Z. Programmable nanomedicine, synergistic and sequential drug delivery systems. Nanoscale. 2015;7:3381–3391. doi: 10.1039/C4NR07677J. [DOI] [PubMed] [Google Scholar]
- 13.Stylianopoulos T., Jain R.K. Design considerations for nanotherapeutics in oncology. Nanomed. Nanotechnol. Biol. Med. 2015;11:1893–1907. doi: 10.1016/j.nano.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eetezadi S., Ekdawi S.N., Allen C. The challenges facing block copolymer micelles for cancer therapy, in vivo barriers and clinical translation. Adv. Drug Deliv. Rev. 2015;91:7–22. doi: 10.1016/j.addr.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes E., Ferreira J.A., Andreia P., Luís L., Barroso S., Sarmento B., Santos L.L. New trends in guided nanotherapies for digestive cancers, a systematic review. J. Control Release. 2015;209:288–307. doi: 10.1016/j.jconrel.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Johnstone T.C., Suntharalingam K., Lippard S.J. The next generation of platinum drugs, targeted PtII agents, nanoparticle delivery, and PtIV prodrugs. Chem. Rev. 2016;116:3436–3486. doi: 10.1021/acs.chemrev.5b00597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumari P., Ghosh B., Biswas S. Nanocarriers for cancer-targeted drug delivery. J. Drug Target. 2016;24:179–191. doi: 10.3109/1061186X.2015.1051049. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui I.A., Adhami V.M., Chamcheu C.J., Mukhtar H. Impact of nanotechnology in cancer, emphasis on nanochemoprevention. Int. J. Nanomed. 2012;7:591–605. doi: 10.2147/IJN.S26026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinkhuis R.P., Rutjes F.P.J.T., Van Hest J.C.M. Polymeric vesicles in biomedical applications. Polym. Chem. 2011;2:1449–1462. doi: 10.1039/c1py00061f. [DOI] [Google Scholar]
- 20.Discher B.M., Hammer D.A., Bates F.S., Discher D.E. Polymer vesicles in various media. Curr. Opin. Colloid Interface Sci. 2000;5:125–131. doi: 10.1016/S1359-0294(00)00045-5. [DOI] [Google Scholar]
- 21.Onaca O., Enea R., Hughes D.W., Meier W. Stimuli-responsive polymersomes as nanocarriers for drug and gene delivery. Macromol. Biosci. 2009;9:129–139. doi: 10.1002/mabi.200800248. [DOI] [PubMed] [Google Scholar]
- 22.Broz P., Benito S.M., Saw C., Burger P., Heider H., Pfisterer M., Marsch S., Meier W., Hunziker P. Cell targeting by a generic receptor-targeted polymer nanocontainer platform. J. Control. Release. 2005;102:475–488. doi: 10.1016/j.jconrel.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Tong R., Cheng J. Anticancer polymeric nanomedicines. Polym. Rev. 2007:345–381. doi: 10.1080/15583720701455079. [DOI] [Google Scholar]
- 24.Torchilin V.P. Micellar nanocarriers, pharmaceutical perspectives. Pharm. Res. 2007;24:1–16. doi: 10.1007/s11095-006-9132-0. [DOI] [PubMed] [Google Scholar]
- 25.Lu Y., Park K. Polymeric micelles and alternative nanonized delivery vehicles for poorly soluble drugs. Int. J. Pharm. 2013;453:198–214. doi: 10.1016/j.ijpharm.2012.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou H., Sun X., Zhang L., Zhang P., Li J., Liu Y.N. Fabrication of biopolymeric complex coacervation core micelles for efficient tea polyphenol delivery via a green process. Langmuir. 2012;28:14553–14561. doi: 10.1021/la303062j. [DOI] [PubMed] [Google Scholar]
- 27.Zhang L., Qi Z., Huang Q., Zeng K., Sun X., Li J., Liu Y.N. Imprinted-like biopolymeric micelles as efficient nanovehicles for curcumin delivery. Colloids Surf. B Biointerfaces. 2014;123:15–22. doi: 10.1016/j.colsurfb.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 28.Wang G., Wang J.J., To T.S.S., Zhao H.F., Wang J. Role of SIRT1-mediated mitochondrial and Akt pathways in glioblastoma cell death induced by Cotinus coggygria flavonoid nanoliposomes. Int. J. Nanomed. 2015;10:5005–5023. doi: 10.2147/IJN.S82282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Curcio M., Blanco-Fernandez B., Diaz-Gomez L., Concheiro A., Alvarez-Lorenzo C. Hydrophobically modified keratin vesicles for GSH-responsive intracellular drug release. Bioconjug. Chem. 2015;26:1900–1907. doi: 10.1021/acs.bioconjchem.5b00289. [DOI] [PubMed] [Google Scholar]
- 30.Curcio M., Cirillo G., Vittorio O., Umile G.S., Francesca L., Nevio P. Hydrolyzed gelatin-based polymersomes as delivery devices of anticancer drugs. Eur. Polym. J. 2015;67:304–313. doi: 10.1016/j.eurpolymj.2015.03.058. [DOI] [Google Scholar]
- 31.Cote B., Carlson L.J., Rao D.A., Alani A.W.G. Combinatorial resveratrol and quercetin polymeric micelles mitigate doxorubicin induced cardiotoxicity in vitro and in vivo. J. Control Release. 2015;213:128–133. doi: 10.1016/j.jconrel.2015.06.040. [DOI] [PubMed] [Google Scholar]
- 32.Sahu A., Kasoju N., Bora U. Fluorescence study of the curcumincasein micelle complexation and its application as a drug nanocarrier to cancer cells. Biomacromolecules. 2008;9:2905–2912. doi: 10.1021/bm800683f. [DOI] [PubMed] [Google Scholar]
- 33.Podaralla S., Averineni R., Alqahtani M., Perumal O. Synthesis of novel biodegradable methoxy polyethylene glycol-zein micelles for effective delivery of curcumin. Mol. Pharm. 2012;9:2778–2786. doi: 10.1021/mp2006455. [DOI] [PubMed] [Google Scholar]
- 34.Wang K., Zhang T., Liu L., Wang X., Wu P., Chen Z., Ni C., Zhang J., Hu F., Huang J. Novel micelle formulation of curcumin for enhancing antitumor activity and inhibiting colorectal cancer stem cells. Int. J. Nanomed. 2012;7:4487–4497. doi: 10.2147/IJN.S34702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lv L., Shen Y., Li M., Xu X., Li M., Guo S., Huang S. Novel 4-arm polyethylene glycolblock-polyanhydride-esters amphiphilic copolymer micelles loading curcumin, preparation, characterization, and in vitro evaluation. BioMed. Res. Int. 2013;2013 doi: 10.1155/2013/507103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lv L., Qiu K., Yu X., Chen C., Qin F., Shi Y., Ou J., Zhang T., Zhu H., Wu J., et al. Amphiphilic copolymeric micelles for doxorubicin and curcumin co-delivery to reverse multidrug resistance in breast cancer. J. Biomed. Nanotechnol. 2016;12:973–985. doi: 10.1166/jbn.2016.2231. [DOI] [PubMed] [Google Scholar]
- 37.Zhu W., Song Z., Wei P., Meng N., Teng F., Yang F., Liu N., Feng R. Y-shaped biotinconjugated poly ethylene glycol-poly epsilon-caprolactone copolymer for the targeted delivery of curcumin. J. Colloid Interface Sci. 2015;443:1–7. doi: 10.1016/j.jcis.2014.11.073. [DOI] [PubMed] [Google Scholar]
- 38.Gou Q., Liu L., Wang C., Wu Q., Sun L., Yang X., Xie Y., Li P., Gong C. Polymeric nanoassemblies entrapping curcumin overcome multidrug resistance in ovarian cancer. Colloids Surf. B Biointerfaces. 2015;126:26–34. doi: 10.1016/j.colsurfb.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 39.Mikhail A.S., Eetezadi S., Ekdawi S.N., Stewart J., Allen C. Image-based analysis of the size-and time-dependent penetration of polymeric micelles in multicellular tumor spheroids and tumor xenografts. Int. J. Pharm. 2014;464:168–177. doi: 10.1016/j.ijpharm.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 40.Liu L., Sun L., Wu Q., Guo W., Li L., Chen Y., Li Y., Gong C., Qian Z., Wei Y. Curcumin loaded polymeric micelles inhibit breast tumor growth and spontaneous pulmonary metastasis. Int. J. Pharm. 2013;443:175–182. doi: 10.1016/j.ijpharm.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 41.Wang B.L., Shen Y.M., Zhang Q.W., Li Y.L., Luo M., Liu Z., Li Y., Qian Z.Y., Gao X., Shi H.S. Codelivery of curcumin and doxorubicin by MPEG-PCL results in improved efficacy of systemically administered chemotherapy in mice with lung cancer. Int. J. Nanomed. 2013;8:3521–3531. doi: 10.2147/IJN.S45250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Erfani-Moghadam V., Nomani A., Zamani M., Yazdani Y., Najafi F., Sadeghizadeh M. A novel diblock copolymer of monomethoxy poly [ethylene glycol]-oleate with a small hydrophobic fraction to make stable micelles/polymersomes for curcumin delivery to cancer cells. Int. J. Nanomed. 2014;9:5541–5554. doi: 10.2147/IJN.S63762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Song Z., Zhu W., Liu N., Yang F., Feng R. Linolenic acid-modified PEG-PCL micelles for curcumin delivery. Int. J. Pharm. 2014;471:312–321. doi: 10.1016/j.ijpharm.2014.05.059. [DOI] [PubMed] [Google Scholar]
- 44.Abouzeid A.H., Patel N.R., Rachman I.M., Senn S., Torchilin V.P. Anti-cancer activity of anti-GLUT1 antibody-targeted polymeric micelles co-loaded with curcumin and doxorubicin. J. Drug Target. 2013;21:994–1000. doi: 10.3109/1061186X.2013.840639. [DOI] [PubMed] [Google Scholar]
- 45.Abouzeid A.H., Patel N.R., Sarisozen C., Torchilin V.P. Transferrin targeted polymeric micelles co-loaded with curcumin and paclitaxel, efficient killing of paclitaxel-resistant cancer cells. Pharm. Res. 2014;31:1938–1945. doi: 10.1007/s11095-013-1295-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarisozen C., Abouzeid A.H., Torchilin V.P. The effect of codelivery of paclitaxel and curcumin by transferrin-targeted PEG-PEbased mixed micelles on resistant ovarian cancer in 3-D spheroids and in vivo tumors. Eur. J. Pharm. Biopharm. 2014;88:539–550. doi: 10.1016/j.ejpb.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Y., Yang C., Wang W., Liu J., Liu Q., Huang F., Chu L., Gao H., Li C., Kong D., et al. Co-delivery of doxorubicin and curcumin by pH-sensitive prodrug nanoparticle for combination therapy of cancer. Sci. Rep. 2016;6:21225. doi: 10.1038/srep21225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sahu A., Kasoju N., Goswami P., Bora U. Encapsulation of curcumin in Pluronic block copolymer micelles for drug delivery applications. J. Biomater. Appl. 2011;25:619–639. doi: 10.1177/0885328209357110. [DOI] [PubMed] [Google Scholar]
- 49.Saxena V., Hussain M.D. Polymeric mixed micelles for delivery of curcumin to multidrug resistant ovarian cancer. J. Biomed. Nanotechnol. 2013;9:1146–1154. doi: 10.1166/jbn.2013.1632. [DOI] [PubMed] [Google Scholar]
- 50.Carlson L.J., Cote B., Alani A.W., Rao D.A. Polymeric micellar codelivery of resveratrol and curcumin to mitigate in vitro doxorubicin induced cardiotoxicity. J. Pharm. Sci. 2014;103:2315–2322. doi: 10.1002/jps.24042. [DOI] [PubMed] [Google Scholar]
- 51.Kim S.H., Adhikari B.B., Cruz S., Schramm M.P., Vinson J.A., Narayanaswami V. Targeted intracellular delivery of resveratrol to glioblastoma cells using apolipoprotein E-containing reconstituted HDL as a nanovehicle. PLoS ONE. 2015;10:e013. doi: 10.1371/journal.pone.0135130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang S., Chen R., Morott J., Repka M.A., Wang Y., Chen M. MPEG-b-PCL/TPGS mixed micelles for delivery of resveratrol in overcoming resistant breast cancer. Expert Opin. Drug Deliv. 2015;12:361–373. doi: 10.1517/17425247.2014.951634. [DOI] [PubMed] [Google Scholar]
- 53.Haratifar S., Meckling K.A., Corredig M. Antiproliferative activity of tea catechins associated with casein micelles, using HT29 colon cancer cells. J. Dairy Sci. 2014;97:672–678. doi: 10.3168/jds.2013-7263. [DOI] [PubMed] [Google Scholar]
- 54.Sun L., Zhang C., Li P. Copolymeric micelles for delivery of EGCG and cyclopamine to pancreatic cancer cells. Nutr. Cancer. 2014;66:896–903. doi: 10.1080/01635581.2014.904908. [DOI] [PubMed] [Google Scholar]
- 55.Hu C.M.J., Aryal S., Zhang L. Nanoparticle-assisted combination therapies for effective cancer treatment. Ther. Deliv. 2010;1:323–334. doi: 10.4155/tde.10.13. [DOI] [PubMed] [Google Scholar]
- 56.Pe´rez-Herrero E., Ferna´ndez-Medarde A. Advanced targeted therapies in cancer, drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015;93:52–79. doi: 10.1016/j.ejpb.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 57.Tsouris V., Joo M.K., Kim S.H., Kwon I.C., Won Y.Y. Nanocarriers that enable codelivery of chemotherapy and RNAi agents for treatment of drugresistant cancers. Biotechnol. Adv. 2014;32:1037–1050. doi: 10.1016/j.biotechadv.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 58.Estanqueiro M., Amaral M.H., Conceicao J., Sousa Lobo J.M. Nanotechnological carriers for cancer chemotherapy, the state of the art. Colloids Surf. B Biointerfaces. 2015;126:631–648. doi: 10.1016/j.colsurfb.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 59.Danhier F., Ansorena E., Silva J.M., Coco R., Le Breton A., Préat V. PLGA-based nanoparticles, an overview of biomedical applications. J. Control Release. 2012;161:505–522. doi: 10.1016/j.jconrel.2012.01.043. [DOI] [PubMed] [Google Scholar]
- 60.Dong H., Tang M., Li Y., Li Y., Qian D., Shi D. Disulfide-bridged cleavable PEGylation in polymeric nanomedicine for controlled therapeutic delivery. Nanomedicine. 2015;10:1941–1958. doi: 10.2217/nnm.15.38. [DOI] [PubMed] [Google Scholar]
- 61.Shirode A.B., Bharali D.J., Nallanthighal S., Coon J.K., Mousa S.A., Reliene R. Nanoencapsulation of pomegranate bioactive compounds for breast cancer chemoprevention. Int. J. Nanomed. 2015;10:475–484. doi: 10.2147/IJN.S65145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liang J., Li F., Fang Y., Yang W., An X., Zhao L., Xin Z., Cao L., Hu Q. Cytotoxicity and apoptotic effects of tea polyphenol-loaded chitosan nanoparticles on human hepatoma HepG2 cells. Mater. Sci. Eng. C. 2014;36:7–13. doi: 10.1016/j.msec.2013.11.039. [DOI] [PubMed] [Google Scholar]
- 63.Kim Y.J., Park M.R., Kim M.S., Kwon O.H. Polyphenol-loaded polycaprolactone nanofibers for effective growth inhibition of human cancer cells. Mater. Chem. Phys. 2012;133:674–680. doi: 10.1016/j.matchemphys.2012.01.050. [DOI] [Google Scholar]
- 64.Das R.K., Kasoju N., Bora U. Encapsulation of curcumin in alginate-chitosan-pluronic composite nanoparticles for delivery to cancer cells. Nanomed. Nanotechnol. Biol. Med. 2010;6:e15360. doi: 10.1016/j.nano.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 65.Sanoj Rejinold N., Muthunarayanan M., Chennazhi K.P., Nair S.V., Jayakumar R. Curcumin loaded fibrinogen nanoparticles for cancer drug delivery. J. Biomed. Nanotechnol. 2011;7:521–534. doi: 10.1166/jbn.2011.1320. [DOI] [PubMed] [Google Scholar]
- 66.Peng S.F., Lee C.Y., Hour M.J., Tsai S.C., Kuo D.H., Chen F.A., Shieh P.C., Yang J.S. Curcumin-loaded nanoparticles enhance apoptotic cell death of U2OS human osteosarcoma cells through the Akt-Bad signaling pathway. Int. J. Oncol. 2014;44:238–246. doi: 10.3892/ijo.2013.2175. [DOI] [PubMed] [Google Scholar]
- 67.Mangalathillam S., Rejinold N.S., Nair A., Lakshmanan V.K., Nair S.V., Jayakumar R. Curcumin loaded chitin nanogels for skin cancer treatment via the transdermal route. Nanoscale. 2012;4:239–250. doi: 10.1039/C1NR11271F. [DOI] [PubMed] [Google Scholar]
- 68.Altunbas A., Lee S.J., Rajasekaran S.A., Schneider J.P., Pochan D.J. Encapsulation of curcumin in self-assembling peptide hydrogels as injectable drug delivery vehicles. Biomaterials. 2011;32:5906–5914. doi: 10.1016/j.biomaterials.2011.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bisht S., Feldmann G., Soni S., Ravi R., Karikar C., Maitra A., Maitra A. Polymeric nanoparticleencapsulated curcumin ‘‘nanocurcumin’’, a novel strategy for human cancer therapy. J. Nanobiotechnol. 2007;5:3. doi: 10.1186/1477-3155-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li L., Xiang D., Shigdar S., Yang W., Li Q., Lin J., Liu K., Duan W. Epithelial cell adhesion molecule aptamer functionalized PLGA-lecithin-curcumin-PEG nanoparticles for targeted drug delivery to human colorectal adenocarcinoma cells. Int. J. Nanomed. 2014;9:1083–1096. doi: 10.2147/IJN.S59779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yallapu M.M., Gupta B.K., Jaggi M., Chauhan S.C. Fabrication of curcumin encapsulated PLGA nanoparticles for improved therapeutic effects in metastatic cancer cells. J. Colloid Interface Sci. 2010;351:19–29. doi: 10.1016/j.jcis.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 72.Yallapu M.M., Dobberpuhl M.R., Maher D.M., Jaggi M., Chauhan S.C. Design of curcumin loaded cellulose nanoparticles for prostate cancer. Curr. Drug Metab. 2012;13:120–128. doi: 10.2174/138920012798356952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yallapu M.M., Khan S., Maher D.M., Ebeling M.C., Sundram V., Chauhan N., Ganju A., Balakrishna S., Gupta B.K., Zafar N., et al. Anti-cancer activity of curcumin loaded nanoparticles in prostate cancer. Biomaterials. 2014;35:8635–8648. doi: 10.1016/j.biomaterials.2014.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim T.H., Jiang H.H., Youn Y.S., Park C.W., Tak K.K., Lee S., Kim H., Jon S., Chen X., Lee K.C. Preparation and characterization of water-soluble albumin-bound curcumin nanoparticles with improved antitumor activity. Int. J. Pharm. 2011;403:285–291. doi: 10.1016/j.ijpharm.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 75.Madhusudana Rao K., Krishna Rao K.S., Ramanjaneyulu G., Ha C.S. Curcumin encapsulated pH sensitive gelatin based interpenetrating polymeric network nanogels for anticancer drug delivery. Int. J. Pharm. 2015;478:788–795. doi: 10.1016/j.ijpharm.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 76.Montalbán M.G., Coburn J.M., Lozano-Pérez A.A., Cenis J.L., Víllora G., Kaplan D.L. Production of Curcumin-Loaded Silk Fibroin Nanoparticles for Cancer Therapy. Nanomaterials. 2018;8:26. doi: 10.3390/nano8020126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Duan J., Mansour H.M., Zhang Y., Deng X., Chen Y., Wang J., Pan Y., Zhao J. Reversion of multidrug resistance by co-encapsulation of doxorubicin and curcumin in chitosan/polybutyl cyanoacrylate nanoparticles. Int. J. Pharm. 2012;426:193–201. doi: 10.1016/j.ijpharm.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 78.Balasubramanian S., Ravindran Girija A., Nagaoka Y., Iwai S., Suzuki M., Kizhikkilot V., Yoshida Y., Maekawa T., Nair S.D. Curcumin and 5-Fluorouracil-loaded, folate-and transferrin-decorated polymeric magnetic nanoformulation, a synergistic cancer therapeutic approach, accelerated by magnetic hyperthermia. Int. J. Nanomed. 2014;9:437–459. doi: 10.2147/IJN.S49882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yallapu M.M., Maher D.M., Sundram V., Bell M.C., Jaggi M., Chauhan S.C. Curcumin induces chemo/radio-sensitization in ovarian cancer cells and curcumin nanoparticles inhibit ovarian cancer cell growth. J. Ovarian. Res. 2010;3:11. doi: 10.1186/1757-2215-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bisht S., Mizuma M., Feldmann G., Ottenhof N.A., Hong S.M., Pramanik D., Chenna V., Karikari C., Sharma R., Goggins M.G., et al. Systemic administration of polymeric nanoparticle-encapsulated curcumin NanoCurc blocks tumor growth and metastases in preclinical models of pancreatic cancer. Mol. Cancer Ther. 2010;9:2255–2264. doi: 10.1158/1535-7163.MCT-10-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shutava T.G., Balkundi S.S., Vangala P. Layer-by-layercoated gelatin nanoparticles as a vehicle for delivery of natural polyphenols. ACS Nano. 2009;3:1877–1885. doi: 10.1021/nn900451a. [DOI] [PubMed] [Google Scholar]
- 82.Sanna V., Pintus G., Roggio A.M. Targeted biocompatible nanoparticles for the delivery of -epigallocatechin 3-gallate to prostate cancer cells. J. Med. Chem. 2011;54:1321–1332. doi: 10.1021/jm1013715. [DOI] [PubMed] [Google Scholar]
- 83.Hu B., Xie M., Zhang C., Zeng X. Genipin-structured peptide-polysaccharide nanoparticles with significantly improved resistance to harsh gastrointestinal environments and their potential for oral delivery of polyphenols. J. Agric. Food Chem. 2014;62:12443–12452. doi: 10.1021/jf5046766. [DOI] [PubMed] [Google Scholar]
- 84.Hu B., Wang Y., Xie M., Guanlan H., Fengguang A., Xiaoxiong Z. Polymer nanoparticles composed with gallic acid grafted chitosan and bioactive peptides combined antioxidant, anticancer activities and improved delivery property for labile polyphenols. J. Funct. Foods. 2015;15:593–603. doi: 10.1016/j.jff.2015.04.009. [DOI] [Google Scholar]
- 85.Ray L., Kumar P., Gupta K.C. The activity against Ehrlich’s ascites tumors of doxorubicin contained in self assembled, cell receptor targeted nanoparticle with simultaneous oral delivery of the green tea polyphenol epigallocatechin-3-gallate. Biomaterials. 2013;34:3064–3076. doi: 10.1016/j.biomaterials.2012.12.044. [DOI] [PubMed] [Google Scholar]
- 86.Lin Y.H., Chen Z.R., Lai C.H., Hsieh C.H., Feng C.L. Active targeted nanoparticles for oral administration of gastric cancer therapy. Biomacromolecules. 2015;16:3021–3032. doi: 10.1021/acs.biomac.5b00907. [DOI] [PubMed] [Google Scholar]
- 87.Khan N., Bharali D.J., Adhami V.M., Siddiqui I.A., Cui H., Shabana S.M., Mousa S.A., Mukhtar H. Oral administration of naturally occurring chitosan-based nanoformulated green tea polyphenol EGCG effectively inhibits prostate cancer cell growth in a xenograft model. Carcinogenesis. 2014;35:415–423. doi: 10.1093/carcin/bgt321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Siddiqui I.A., Bharali D.J., Nihal M., Adhami V.M., Khan N., Chamcheu J.C., Khan M.I., Shabana S., Mousa S.A., Mukhtar H. Excellent antiproliferative and pro-apoptotic effects of -epigallocatechin-3gallate encapsulated in chitosan nanoparticles on human melanoma cell growth both in vitro and in vivo. Nanomed Nanotechnol. Biol. Med. 2014;10:1619–1626. doi: 10.1016/j.nano.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 89.Singh M., Bhatnagar P., Srivastava A.K., Kumar P., Shukla Y., Gupta K.C. Enhancement of cancer chemosensitization potential of cisplatin by tea polyphenols polylactide-co-glycolide nanoparticles. J. Biomed. Nanotechnol. 2011;7:202. doi: 10.1166/jbn.2011.1268. [DOI] [PubMed] [Google Scholar]
- 90.Singh M., Bhatnagar P., Mishra S., Kumar P., Shukla Y., Gupta K.C. PLGA-encapsulated tea polyphenols enhance the chemotherapeutic efficacy of cisplatin against human cancer cells and mice bearing Ehrlich ascites carcinoma. Int. J. Nanomed. 2015;10:6789–6809. doi: 10.2147/IJN.S79489. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 91.Guo L., Peng Y., Li Y., Jingping Y., Guangmei Z., Jie C., Jing W., Lihua S. Cell death pathway induced by resveratrol-bovine serum albumin nanoparticles in a human ovarian cell line. Oncol. Lett. 2015;9:1359–1363. doi: 10.3892/ol.2015.2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Karthikeyan S., Hoti S.L., Prasad N.R. Resveratrol loaded gelatin nanoparticles synergistically inhibits cell cycle progression and constitutive NF-kappa B activation, and induces apoptosis in non-small cell lung cancer cells. Biomed. Pharmacother. 2015;70:274–282. doi: 10.1016/j.biopha.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 93.Kumar S., Lather V., Pandita D. A facile green approach to prepare core–shell hybrid PLGA nanoparticles for resveratrol delivery. Int. J. Biol. Macromol. 2016;84:380–384. doi: 10.1016/j.ijbiomac.2015.12.036. [DOI] [PubMed] [Google Scholar]
- 94.Sanna V., Siddiqui I.A., Sechi M., Mukhtar H. Resveratrol-loaded nanoparticles based on polyepsiloncaprolactone and polyd,l-lacticco-glycolic acid-polyethylene glycol blend for prostate cancer treatment. Mol. Pharm. 2013;10:3871–3881. doi: 10.1021/mp400342f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Guo W., Li A., Jia Z., Yuan Y., Dai H., Li H. Transferrin modified PEG-PLA resveratrol conjugates, in vitro and in vivo studies for glioma. Eur. J. Pharmacol. 2013;718:41–47. doi: 10.1016/j.ejphar.2013.09.034. [DOI] [PubMed] [Google Scholar]
- 96.David K.I., Jaidev L.R., Sethuraman S., Krishnan U.M. Dual drug loaded chitosan nanoparticles–sugar-coated arsenal against pancreatic cancer. Colloids Surf. B Biointerfaces. 2015;135:689–698. doi: 10.1016/j.colsurfb.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 97.Jain A.K., Thanki K., Jain S. Co-encapsulation of tamoxifen and quercetin in polymeric nanoparticles, implications on oral bioavailability, antitumor efficacy, and drug-induced toxicity. Mol. Pharm. 2013;10:3459–3474. doi: 10.1021/mp400311j. [DOI] [PubMed] [Google Scholar]
- 98.Abbad S., Waddad A.Y., Lv H., Zhou J. Preparation, in vitro and in vivo evaluation of Polymeric nanoparticles based on hyaluronic acid Polybutyl cyanoacrylate and D-alpha-tocopheryl Polyethylene glycol 1000 succinate for tumor-targeted delivery of Morin hydrate. Int. J. Nanomed. 2015;10:305–320. doi: 10.2147/IJN.S73971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sirova M., Kabesova M., Kovar L., Etrych T., Strohalm J., Ulbrich K., Rihova B. HPMA copolymer-bound doxorubicin induces immunogenic tumor cell death. Curr. Med. Chem. 2013;20:4815–4826. doi: 10.2174/09298673113206660281. [DOI] [PubMed] [Google Scholar]
- 100.Sobczak M., Debek C., Oledzka E., Kozłowski R. Polymeric systems of antimicrobial peptides-strategies and potential applications. Molecules. 2013;18:14122–14137. doi: 10.3390/molecules181114122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Spizzirri U.G., Cirillo G., Picci N., Iemma F. Recent development in the synthesis of eco-friendly polymeric antioxidants. Curr. Org. Chem. 2014;18:2912–2927. doi: 10.2174/1385272819666140923221142. [DOI] [Google Scholar]
- 102.Nyanhongo G.S., Nugroho Prasetyo E., Herrero Acero E., Guebitz G.M. Engineering strategies for successful development of functional polymers using oxidative enzymes. Chem. Eng. Technol. 2012;35:1359–1372. doi: 10.1002/ceat.201100590. [DOI] [Google Scholar]
- 103.Oliver S., Vittorio O., Cirillo G., Boyer C. Enhancing the therapeutic effects of polyphenols with macromolecules. Polym. Chem. 2016;7:1529–1544. doi: 10.1039/C5PY01912E. [DOI] [Google Scholar]
- 104.Li J., Wang Y., Yang C., Wang P., Oelschlager D.K., Zheng Y., Tian D.A., Grizzle W.E., Buchsbaum D.J., Wan M. Polyethylene glycosylated curcumin conjugate inhibits pancreatic cancer cell growth through inactivation of Jab1. Mol. Pharmacol. 2009;76:81–90. doi: 10.1124/mol.109.054551. [DOI] [PubMed] [Google Scholar]
- 105.Safavy A., Raisch K.P., Mantena S., Sanford L.L., Sham S.W., Krishna N.R., Bonner J.A. Design and development of water-soluble curcumin conjugates as potential anticancer agents. J. Med. Chem. 2007;50:6284–6288. doi: 10.1021/jm700988f. [DOI] [PubMed] [Google Scholar]
- 106.Dey S., Ambattu L.A., Hari P.R., Rekha M.R., .Sreenivasan K. Glutathione-bearing fluorescent polymer–curcumin conjugate enables simultaneous drug delivery and label-free cellular imaging. Polym. UK. 2015;75:25–33. doi: 10.1016/j.polymer.2015.08.020. [DOI] [Google Scholar]
- 107.Wang W., Zhang L., Le Y., Chen J.F., Wang J., Yun J. Synergistic effect of PEGylated resveratrol on delivery of anticancer drugs. Int. J. Pharm. 2016;498:134–141. doi: 10.1016/j.ijpharm.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 108.Wang X., Chen Y., Dahmani F.Z., Yin L., Zhou J., Yao J. Amphiphilic carboxymethyl chitosan–quercetin conjugate with P-gp inhibitory properties for oral delivery of paclitaxel. Biomaterials. 2014;35:7654–7665. doi: 10.1016/j.biomaterials.2014.05.053. [DOI] [PubMed] [Google Scholar]
- 109.Lv L., Guo Y., Shen Y., Liu J., Zhang W., Zhou D., Guo S. Intracellularly degradable, self-assembled amphiphilic block copolycurcumin nanoparticles for efficient in vivo cancer chemotherapy. Adv. Heal. Mater. 2015;4:1496–1501. doi: 10.1002/adhm.201500075. [DOI] [PubMed] [Google Scholar]
- 110.Shpaisman N., Sheihet L., Bushman J., Winters J., Kohn J. One-step synthesis of biodegradable curcumin-derived hydrogels as potential soft tissue fillers after breast cancer surgery. Biomacromolecules. 2012;13:2279–2286. doi: 10.1021/bm300518e. [DOI] [PubMed] [Google Scholar]
- 111.Su J., Chen F., Cryns V.L., Messersmith P.B. Catechol polymers for pH-responsive, targeted drug delivery to cancer cells. J. Am. Chem. Soc. 2011;133:11850–11853. doi: 10.1021/ja203077x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liang K., Ng S., Lee F., Lim J., Chung J.E., Lee S.S., Kurisawa M. Targeted intracellular protein delivery based on hyaluronic acid-green tea catechin nanogels. Acta Biomater. 2016;33:142–152. doi: 10.1016/j.actbio.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 113.Vittorio O., Cirillo G., Iemma F., Di Turi G., Jacchetti E., Curcio M., Barbuti S., Funel N., Parisi O.I., Puoci F., et al. Dextran-catechin conjugate, a potential treatment against the pancreatic ductal adenocarcinoma. Pharm. Res. 2012;29:2601–2614. doi: 10.1007/s11095-012-0790-9. [DOI] [PubMed] [Google Scholar]
- 114.Vittorio O., Brandl M., Cirillo G., Kimpton K., Hinde E., Gaus K., Yee E., Kumar N., Duong H., Fleming C., et al. Dextran–catechin, an anticancer chemically-modified natural compound targeting copper that attenuates neuroblastoma growth. Oncotarget. 2016;7:47479–47493. doi: 10.18632/oncotarget.10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Puoci F., Morelli C., Cirillo G., Curcio M., Parisi O.I., Maris P., Sisci D., Picci N. Anticancer activity of a quercetin-based polymer towards HeLa cancer cells. Anticancer Res. 2012;32:2843–2847. [PubMed] [Google Scholar]
- 116.Cirillo G., Kraemer K., Fuessel S., Puoci F., Curcio M., Spizzirri U.G., Altimari I., Iemma F. Biological activity of a gallic acid–gelatin conjugate. Biomacromolecules. 2010;11:3309–3315. doi: 10.1021/bm100760x. [DOI] [PubMed] [Google Scholar]
- 117.Bhattacharya K., Mukherjee S.P., Gallud A., Burkert S.C., Bistarelli S., Bellucci S., Bottini M., Star A., Fadeel B. Biological interactions of carbon-based nanomaterials, from coronation to degradation. Nanomed. Nanotechnol. Biol. Med. 2016;12:333–351. doi: 10.1016/j.nano.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bianco A., Kostarelos K., Partidos C.D., Prato M. Biomedical applications of functionalized carbon nanotubes. Chem. Commun. 2005;5:571–577. doi: 10.1039/b410943k. [DOI] [PubMed] [Google Scholar]
- 119.Feng L., Liu Z. Graphene in biomedicine, opportunities and challenges. Nanomed. Lond. 2011;6:317–324. doi: 10.2217/nnm.10.158. [DOI] [PubMed] [Google Scholar]
- 120.Wang Y., Li Z., Wang J., Jinghong L., Yuehe L. Graphene and graphene oxide, biofunctionalization and applications in biotechnology. Trends Biotechnol. 2011;29:205–212. doi: 10.1016/j.tibtech.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Peng C., Hu W., Zhou Y., Fan C., Huang Q. Intracellular imaging with a graphene-based fluorescent probe. Small. 2010;6:1686–1692. doi: 10.1002/smll.201000560. [DOI] [PubMed] [Google Scholar]
- 122.Makharza S., Cirillo G., Bachmatiuk A., Imad I., Nicholas I., Barbara T., Silke H., Mark H.R. Graphene oxidebased drug delivery vehicles, functionalization, characterization, and cytotoxicity evaluation. J. Nanopart Res. 2013;15:2099. doi: 10.1007/s11051-013-2099-y. [DOI] [Google Scholar]
- 123.Lin Y., Taylor S., Li H., Shiral K.A.F., Liangwei Q., Wei W., Lingrong G., Bing Z., Ya-Ping S. Advances toward bioapplications of carbon nanotubes. J. Mater. Chem. 2004;14:527–541. doi: 10.1039/b314481j. [DOI] [Google Scholar]
- 124.Zhang Y., Petibone D., Xu Y., Mahmood M., Karmakar A., Casciano D., Ali S., Biris A.S. Toxicity and efficacy of carbon nanotubes and graphene, the utility of carbon-based nanoparticles in nanomedicine. Drug Metab. Rev. 2014;46:232–246. doi: 10.3109/03602532.2014.883406. [DOI] [PubMed] [Google Scholar]
- 125.Wang H., Wang J., Deng X., Un H., Shi Z., Gu Z., Liu Y., Zhao Y. Biodistribution of carbon single-wall carbon nanotubes in mice. J. Nanosci. Nanotechnol. 2004;4:1019–1024. doi: 10.1166/jnn.2004.146. [DOI] [PubMed] [Google Scholar]
- 126.Chaudhuri P., Soni S., Sengupta S. Single-walled carbon nanotube-conjugated chemotherapy exhibits increased therapeutic index in melanoma. Nanotechnology. 2010;21:025102. doi: 10.1088/0957-4484/21/2/025102. [DOI] [PubMed] [Google Scholar]
- 127.Kiew S.F., Kiew L.V., Lee H.B., Imae T., Chung L.Y. Assessing biocompatibility of graphene oxide-based nanocarriers, a review. J. Control. Release. 2016;226:217–228. doi: 10.1016/j.jconrel.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 128.Bagri A., Mattevi C., Acik M., Chabal Y.J., Chhowalla M., Shenoy V.B. Structural evolution during the reduction of chemically derived graphene oxide. Nat. Chem. 2010;2:581–587. doi: 10.1038/nchem.686. [DOI] [PubMed] [Google Scholar]
- 129.Ambrosi A., Chua C.K., Khezri B., Sofer Z., Webster R.D., Pumera M. Chemically reduced graphene contains inherent metallic impurities present in parent natural and synthetic graphite. Proc. Natl. Acad. Sci. USA. 2012;109:12899–12904. doi: 10.1073/pnas.1205388109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Spizzirri U.G., Hampel S., Cirillo G., Maria V.M., Orazio V., Paolina C., Cristina G., Manuela C., Nevio P., Francesca L. Functional gelatin–carbon nanotubes nanohybrids with enhanced antibacterial activity. Int. J. Polym. Mater. Polym. Biomater. 2015;64:439–447. doi: 10.1080/00914037.2014.958833. [DOI] [Google Scholar]
- 131.Spizzirri U.G., Curcio M., Cirillo G., Spataro T., Vittorio O., Picci N., Hampel S., Iemma F., Nicoletta F.P. Recent advances in the synthesis and biomedical applications of nanocomposite hydrogels. Pharmaceutics. 2015;7:413–437. doi: 10.3390/pharmaceutics7040413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kim S.J., Lee J.M., Kumer R.A., Park S.Y., Kim S.C., In I. Environmentally friendly synthesis of P-doped reduced graphene oxide with high dispersion stability by using red table wine. Chem. Asian J. 2015;10:1192–1197. doi: 10.1002/asia.201500010. [DOI] [PubMed] [Google Scholar]
- 133.Abdolahad M., Janmaleki M., Mohajerzadeh S., Akhavan O., Abbasi S. Polyphenols attached graphene nanosheets for high efficiency NIR mediated photodestruction of cancer cells. Mater. Sci. Eng. C. 2013;33:1498–1505. doi: 10.1016/j.msec.2012.12.052. [DOI] [PubMed] [Google Scholar]
- 134.Gurunathan S., Han J.W., Kim E.S., Park J.H., Kim J.H. Reduction of graphene oxide by resveratrol, a novel and simple biological method for the synthesis of an effective anticancer nanotherapeutic molecule. Int. J. Nanomed. 2015;10:2951–2969. doi: 10.2147/IJN.S79879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cirillo G., Hampel S., Klingeler R., Puoci F., Iemma F., Curcio M., Parisi O.I., Spizzirri U.G., Picci N., Leonhardt A., et al. Antioxidant multiwalled carbon nanotubes by free radical grafting of gallic acid, new materials for biomedical applications. J. Pharm. Pharmacol. 2011;63:179–188. doi: 10.1111/j.2042-7158.2010.01211.x. [DOI] [PubMed] [Google Scholar]
- 136.Shao S., Li L., Yang G., Li J., Luo C., Gong T., Zhou S. Controlled green tea polyphenols release from electrospun PCL/MWCNTs composite nanofibers. Int. J. Pharm. 2011;421:310–320. doi: 10.1016/j.ijpharm.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 137.Cirillo G., Vittorio O., Hampel S., Spizzirri U.G., Picci N., Iemma F. Incorporation of carbon nanotubes into a gelatin-catechin conjugate, innovative approach for the preparation of anticancer materials. Int. J. Pharm. 2013;446:176–182. doi: 10.1016/j.ijpharm.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 138.Castro Nava A., Cojoc M., Peitzsch C., Cirillo G., Kurth I., Fuessel S., Erdmann K., Kunhardt D., Vittorio O., Hampel S., et al. Development of novel radiochemotherapy approaches targeting prostate tumor progenitor cells using nanohybrids. Int. J. Cancer. 2016;137:2492–2503. doi: 10.1002/ijc.29614. [DOI] [PubMed] [Google Scholar]
- 139.Cirillo G., Vittorio O., Hampel S., Iemma F., Parchi P., Cecchini M., Puoci F., Picci N. Quercetin nanocomposite as novel anticancer therapeutic, improved efficiency and reduced toxicity. Eur. J. Pharm. Sci. 2013;49:359–365. doi: 10.1016/j.ejps.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 140.Vittorio O., Brandl M., Cirillo G., Umile G.S., Nevio P., Maria K., Francesca L., Silke H. Novel functional cisplatin carrier based on carbon nanotubes-quercetin nanohybrid induces synergistic anticancer activity against neuroblastoma in vitro. RSC Adv. 2014;4:31378–31384. doi: 10.1039/C4RA03331K. [DOI] [Google Scholar]
- 141.Riggio C., Calatayud M.P., Giannaccini M., Sanz B., Torres T.E., Fernández-Pacheco R., Ripoli A., Ibarra M.R., Dente L., Cuschieri A., et al. The orientation of the neuronal growth process can be directed via magnetic nanoparticles under an applied magnetic field. Nanomed. Nanotechnol. Biol. Med. 2014;10:1549–1558. doi: 10.1016/j.nano.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 142.Ası´n L., Goya G.F., Tres A., Ibarra M.R. Induced cell toxicity originates dendritic cell death following magnetic hyperthermia treatment. Cell. Death Dis. 2013;4:e596. doi: 10.1038/cddis.2013.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Manju S., Sreenivasan K. Enhanced drug loading on magnetic nanoparticles by layer-by-layer assembly using drug conjugates, blood compatibility evaluation and targeted drug delivery in cancer cells. Langmuir. 2011;27:14489–14496. doi: 10.1021/la202470k. [DOI] [PubMed] [Google Scholar]
- 144.Wani K.D., Kitture R., Ahmed A., Choudhari AS., Koppikar SJ., Kale SN., Kaul-Ghanekar R. Synthesis, characterization and in vitro study of curcumin-functionalized citric acid-capped magnetic CCF nanoparticles as drug delivery agents in cancer. J. Bionanosci. 2011;5:59–65. doi: 10.1166/jbns.2011.1041. [DOI] [Google Scholar]
- 145.Yallapu M.M., Ebeling M.C., Khan S., Sundram V., Chauhan N., Gupta B.K., Puumala S.E., Jaggi M., Chauhan S.C. Novel curcumin-loaded magnetic nanoparticles for pancreatic cancer treatment. Mol. Cancer Ther. 2013;12:1471–1480. doi: 10.1158/1535-7163.MCT-12-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Vittorio O., Voliani V., Faraci P., Karmakar B., Iemma F., Hampel S., Kavallaris M., Cirillo G. Magnetic catechin-dextran conjugate as targeted therapeutic for pancreatic tumour cells. J. Drug Target. 2014;22:408–415. doi: 10.3109/1061186X.2013.878941. [DOI] [PubMed] [Google Scholar]
- 147.Xiao L., Mertens M., Wortmann L., Kremer S., Valldor M., Lammers T., Kiessling F., Mathur S. Enhanced in vitro and in vivo cellular imaging with green tea coated water-soluble iron oxide nanocrystals. ACS Appl. Mater. Interfaces. 2015;7:6530–6540. doi: 10.1021/am508404t. [DOI] [PubMed] [Google Scholar]
- 148.Guo D., Wu C., Li J., Guo A., Li Q., Jiang H., Chen B., Wang X. Synergistic effect of functionalized nickel nanoparticles and quercetin on inhibition of the SMMC-7721 cells proliferation. Nanoscale Res. Lett. 2009;4:1395–1402. doi: 10.1007/s11671-009-9411-x. [DOI] [PMC free article] [PubMed] [Google Scholar]