Abstract
Some pathogens might develop favorable global adaptation in response to certain stress treatments resulting in enhanced virulence and/or resistance to a different stress. β-lactam resistance, as well as ampC and ampG genes involved in this resistance, were studied to evaluate their possible role in Escherichia coli O157:H7 (E. coli) radioresistance. E. coli adapted to 25, 15 or 7 μg/mL of kanamycin or carbenicillin, were produced and treated with sensitization (0.4 kGy) or lethal (1.5 kGy) irradiation doses. In E. coli O157:H7, irradiation treatment at 0.4 kGy dose increased ampC and ampG expression respectively by 1.6 and 2-fold in the wild type strain (Wt) but up to by 2.4 and 3.4-fold when the strain was beforehand adapted to 25 μg/mL of carbenicillin (Carb25). Accordingly, ΔampC and ΔampG mutants and E. coli adapted to 25 μg/mL of kanamycin were more sensitive to 0.4 kGy treatment than Wt. While, E. coli Carb25 or overexpression of ampC and ampG provided complete resistance to 0.4 kGy and were even able to survive and grow after exposure to a normally lethal 1.5 kGy irradiation dose. We further noticed that these strains can tolerate other stresses like oxidative, cold and heat shocks. This demonstrates that carbenicillin adaptation promotes resistance to γ-irradiation and to other stresses, likely at least through increased AmpC and AmpG expression. These results are important for the food industry and particularly when considering the use of irradiation for food preservation of meat obtained directly from animals fed β-lactam antibiotics.
Keywords: Biotechnology, Microbiology, Molecular biology
1. Introduction
The bacterium E. coli serotype O157:H7 was identified in 1989 as a human pathogen that can produce one of several Shiga toxins known to cause haemorrhagic colitis and hemolytic uremic syndrome (Karmali et al., 1983). E. coli O157:H7, found in the feces of healthy cattle, can be acquired by direct contact with infected animals or people, by consumption of contaminated food (i.e. meat, fruits, vegetables and poultry), or by wastewater of slaughterhouses (Karmali et al., 1983; Phillips, 1999; Loukiadis et al., 2006). The emergence of antibiotic use in animal feed to treat, control and prevent clinical diseases or to enhance animal growth promotes bacterial resistance by natural selection of mutant population unresponsive to the antibiotics (Courvalin, 2008). Furthermore, spontaneous antibiotic-resistant E. coli O157:H7 strains are emerging, such as ampicillin and chloramphenicol resistant mutants of strain EDL933, which led to increased motility, altered sensitivity to phages, and altered generation time in vitro resulting in a rise in their virulence (Tóth et al., 2003; Carone et al., 2014). As a result, Canadian authorities have recognized that some antimicrobial drugs used in veterinary medicine, e.g. β-lactams, can promote the development of resistance and might have serious consequences on human health (Health Canada, 2002).
Bacterial resistance to β-lactam antibiotics induces SOS response, through RecA and DpiA, and is driven by either β-lactamases modifying penicillin-binding proteins (PBPs), or by increased active efflux or decreased permeability, dependent on permeases (Poole, 2004). In many Enterobacteriaceae and other Gram-negative bacteria, the expression of the β-lactamase gene ampC is inducible by various β-lactam antibiotics (Sanders Jr and Sanders Jr, 1986; Zeng and Lin, 2013). Some mutations can alter this inducibility, resulting in increased β-lactamases synthesis and consequently raised resistance to new β-lactam antibiotics (Sanders and Sanders Jr, 1983; Juan et al., 2006). AmpC belongs to the group I, class C of β-lactamases and it is expressed at very low levels in wild type strains. AmpC levels increase significantly in E. coli in the presence of certain β-lactam antibiotics (Livermore, 1995).
The expression of ampC is induced by several genes products leading to peptidoglycan recycling, required for cell growth and division (Normark, 1995; Park and Uehara, 2008). The peptidoglycan layer is composed of β-1,4-linked N-acetylglucosamine (GlcNAc) and N-acetylmuramic acid (MurNAc) residues. Peptidoglycan degradation, caused for instance by the action of β-lactam antibiotics, leads to the generation of a pool of GlcNAc-anhMurNAc-peptides which can be transported to the cytoplasm by the permease AmpG (Park and Uehara, 2008) and act as signals involved in ampC induction and metabolism through the transcriptional regulator AmpR and the repressor AmpD. Therefore, mutation in ampD or in ampR may lead to overproduction of AmpC beta-lactamase (Kaneko et al., 2005; Schmidtke and Hanson, 2008).
In several food industries, γ-irradiation is used to prolong shelf-life of food products and to reduce the growth of pathogens (Koutchma et al., 2009; Ben-Fadhel et al., 2016). At doses of 2–7 kGy, γ-irradiation can eliminate potentially pathogenic bacteria such as E. coli O157:H7. The microbial inactivation mechanism of γ-irradiation is explained by oxidative radicals resulting from the radiolysis of water, generating an oxidative stress that will cause damage to nucleic acids, proteins and whole cells (Farkas, 2006). The increase of these free radicals induces an oxidative stress response in the bacteria. However, many pathogens can develop physiological and molecular mechanisms of resistance that can disrupt the efforts of food industries to control food contamination and to insure food safety. Bacterial radioresistance is a complex phenomenon that is still poorly understood.
The aim of this study is to assess the impact of the resistance to antibiotics widely used in animal feed (β-lactams) on the radioresistance of E. coli O157:H7, more specifically by evaluating the effect of AmpC β-lactamase and of AmpG permease.
2. Materials and methods
2.1. Material
Isopropyl-β-D-thiogalactopyranoside (IPTG), N,N′-dimethyl-4,4′-bipyridinium dichloride (Paraquat) carbenicillin, ampicillin, piperacillin and kanamycin were obtained from Sigma Aldrich, Ontario, Canada. PureZOL was provided from Life Science Research, Ontario, Canada.
2.2. Bacterial strains, plasmids and growth conditions
E. coli strains and plasmids used in this study are listed in Table 1. Bacteria were cultivated overnight (O/N) in Tryptic Soy Broth (TSB, Difco, Becton Dickinson, Sparks, MD, USA) or on Tryptic Soy Agar plate (TSA, Difco, Becton Dickinson, Sparks, MD, USA). The media was supplemented with: (i) 100 μg/mL carbenicillin and incubated at 30 °C for E. coli O157:H7 (pKD46) (Wt and mutants) or at 37 °C for E. coli O157:H7 (Ptrc99A) (Wt and carrying ampC or ampG), (ii) 30 μg/mL kanamycin and incubated at 37 °C for E. coli O157:H7 without pKD46, or (iii) without antibiotics for strain K-12 (Wt and mutants). Transformed cells were recovered in 1 mL SOC medium (Thermo Fisher Scientific, Burlington, Ontario, Canada) (pKD46) or 1 mL TSB and incubated at 30 °C for 1 h. IPTG was added to TSB medium to obtain a final concentration of 1 mM for E. coli O157:H7 carrying pTRC99A plasmid. To reach the bacterial exponential phase, the O/N culture was diluted at 1/100th and incubated at 37 °C for 3–4 h until an OD600 ≈ 1 was obtained. OD600 for all cell cultures used in this work was measured with a Nanodrop ND-1000 spectrophotometer (Thermo Fisher Scientific, Burlington, Ontario, Canada) and a path length correction was applied by multiplying the given value by a factor of 10.
Table 1.
List of E. coli strains and plasmids used in this study.
| E. coli stains and plasmids | Description | Source or reference |
|---|---|---|
| O157:H7 str. EDL933 | Pathogenic strain isolated from Michigan ground beef | Provided by Pr. Charles Dozois (INRS-IAF) |
| K-12 | ||
| ΔampC | F-, Δ(araD-araB)567, ΔlacZ4787(::rrnB-3), λ-, rph-1, Δ(rhaD-rhaB)568, ΔampC777::kan, hsdR514 | Genetic stock center (Baba et al., 2006) |
| ΔampG | F-, Δ(araD-araB)567, ΔlacZ4787(::rrnB-3), ΔampG790::kan, λ-, rph-1, Δ(rhaD-rhaB)568, hsdR514 | Genetic stock center (Baba et al., 2006) |
| Plasmid | Sensitive plasmid | Genetic stock center |
| pKD46 | F-, λ-, rph-1, pKD46 | (Datsenko and Wanner, 2000) |
| pTrc99A | trcP vector, lacI promoter, pUCl8 EcoRI-SmaI, | Provided by Pr. Charles Dozois (INRS-IAF) |
2.3. Construction of mutants and complementation/overexpression vectors
Deletion mutants were derived using one-step PCR fragment-mediated lambda red recombination mutagenesis (Datsenko and Wanner, 2000). The pKD13 strain has been used to create KEIO mutants (Baba et al., 2006). Using primers listed in Table 2, the ampC::kan and ampG::kan alleles were amplified directly from K-12 mutant strains JW4111-2 (ΔampC::kan) and JW0423-1(ΔampG::kan) respectively, obtained from the Keio collection to generate ΔampC::kan and ΔampG::kan in O157:H7, a derivate of E. coli K-12 carrying pKD46 (Sabri et al., 2009). The purified PCR fragment was transformed into DH5α competent cells carrying pKD46 by heat shock. The extracted plasmid-Δgene (ampC or ampG) was transformed by electroporation (1800 volts, 200 ohms, 25 μF) into E. coli O157:H7 competent cells. The homologous recombination between pKD46 and chromosomic genes was then evaluated. E. coli O157:H7 mutants were verified by amplification and sequencing of ampC::kan or ampG::kan using primers cited in Table 2. Overexpression of ampC and ampG was achieved using the high-copy number inducible plasmid pTRC99A (Amann et al., 1988). These two genes were amplified using E. coli O157:H7 DNA as the template and the primers cited in Table 2 designed to have EcoRI and SmaI cohesive ends. The resulting PCR amplicon was digested by EcoRI and SmaI (New England Biolabs, Massachusetts, USA) and used for ligation to EcoRI-/SmaI-treated pTrc99A. The recombinant plasmid was transformed into DH5α competent cells by heat shock. After miniprep, it was transformed by electroporation (1800 volts, 200 ohms, 25 μF) into E. coli O157:H7 competent cells. Transformants carrying pTRC99A-gene or pTRC99A-without gene were selected on TSA plates supplemented with 100 μg/mL of carbenicillin. Plasmids were digested by EcoRI and migrated on 1% agarose gel to confirm gene insertion.
Table 2.
List of primers used in this study.
| Genes | Sequence (5′ to 3′) |
|---|---|
| Homologous primers | |
| ampC. Fwd | GAGCTTCATTGGTCGCGTAT |
| ampC. Rev | TTCACTCTGCTGCCACATTC |
| ampG. Fwd | ATATCGCCATCATCGCTACC |
| ampG. Rev | CAAAAGGGGAGTGCAGAAGA |
| Primers for overexpression | |
| ampC.over-EcoRI-Fwd | CTCTGAATTCTTTTCTACGGTCTGGCTGCT |
| ampC.over-SmaI-Rev | CTCTCCCGGGCAGGCGCATAAATGTTTCCT |
| ampG.over-EcoRI-Fwd | CTCTGAATTCTGCTGACCGATACCATCGCT |
| ampG.over-SmaI-Rev | CTCTCCCGGGGCTAAGCCGCACAAAAGAAC |
| Primers for verification | |
| ampC.over-Fwd | TTTTCTACGGTCTGGCTGCT |
| ampC.over-Rev | CAGGCGCATAAATGTTTCCT |
| ampG.over-Fwd | TGCTGACCGATACCATCGCT |
| ampG.over-Rev | GCTAAGCCGCACAAAAGAAC |
| Primers for qRT-PCR | |
| ampC. Fwd | CGCTAAGGAGTGCAACATGA |
| ampC. Rev | CGCAGCATGTAAAAGCGATA |
| ampG. Fwd | GCCGCCCTTAATTTTTCTTC |
| ampG. Rev | GCAATGGAAACGGTAAAAGC |
| rpoH Fwd | TCGTCAAAGTTGCGACCACCAAAG |
| rpoH rev | ATCGTCGTCGGAAGACAGGTCAAA |
2.4. Antibiotic susceptibility assays
The minimum inhibitory concentration (MIC) of the antibiotics was determined as recommended by the Clinical and Laboratory Standards Institute (Clinical and Laboratory Standards Institute, 2014). The evaluated antibiotics were carbenicillin, ampicillin, piperacillin and kanamycin. All antibiotics were prepared in distilled water to a final concentration of 50 μg/mL for kanamycin and 100 μg/mL for the others. A Blank Antimicrobial Susceptibility Disks (Thermo Ficher Scientific, Burlington, Ontario, Canada) imbibed with either 5 μL or 10 μL of one of the antibiotics, corresponding to 250 μg and 500 μg for kanamycin and 500 μg and 1000 μg for the other antibiotics, were used for the antibiotic susceptibility assays on E. coli O157:H7 mutants.
2.5. Development of antibiotic-adapted O157:H7 strains
E. coli O157:H7 was adapted to 25, 15 or 7 μg/mL of carbenicillin or kanamycin by successive passages (n = 4) in TSB supplemented with the respective antibiotic at the specified concentration. The selected concentrations of each antibiotic used in this study were enough to slow down the bacterial growth. After the adaptation step and for all following experiments, adapted bacteria were cultivated in TSB without antibiotic.
2.6. γ-Irradiation treatments
Cell cultures (all strains) from the exponential phase of growth (OD600 ≈ 1) were transferred into microfuge tubes and subjected to one of two different irradiation treatments: the sensitive dose of 0.4 kGy to only damage the cells or the lethal dose of 1.5 kGy (Caillet et al., 2005). The experiments were performed at room temperature (20 ± 1 °C) at the Canadian Irradiation Center, where samples were irradiated in a UC-15A irradiator (Nordion Inc., Kanata, ON, Canada) equipped with a 60Co source with a dose rate of 16.8 kGy/h.
2.7. Viability and growth study
All strains were evaluated immediately after irradiation treatment for their viability and growth. The obtained working cultures were serially diluted and plated on TSA plates and then incubated overnight at 37 °C. For the growth assays, the obtained working cultures were diluted in TSB to an OD600 = 0.05 and 200 μL of cell culture were distributed wells of sterile microtiter plates. This experiment was performed in a Bioscreen C apparatus (Growth Curves USA) where the cultures were incubated at 37 °C for 20 h and the OD600 growth measurements were performed every 30 minutes after a homogenization period of 30 seconds.
2.8. RNA preparation and quantitative real-time PCR (qRT-PCR)
E. coli O157: H7 Wt and Carb25 adapted bacteria were incubated in TSB at 37 °C and irradiated at the sensitive dose at the exponential phase of growth (OD600 ≈ 1). Control and irradiated cultures were incubated at 37 °C for 60 min and then RNA extraction was performed. Bacterial culture was centrifuged at 12,000 x g for 5 min and the cells were suspended in 1 mL PureZOL. RNA extraction was carried out as recommended by the supplier. The iScript reverse transcription kit (Life Science Research, Ontario, Canada) was used to synthesize cDNA from 50 ng of RNA and quantitative real-time PCR (qRT-PCR) was then performed using the SsoAdvanced™ Universal SYBR® Green Supermix reagent (Life Science Research, Bio-Rad) on a Rotor-Gene 6000 thermocycler (Corbett). Modulation of gene expression from qRT-PCR was normalized to the expression of the internal rpoH gene. The primers used in this study are listed in Table 2. The variation of gene expression was calculated using the -2ΔΔCt method of Livak and Schmittgen (2001). The relative expression of Wt was used as a reference to calculate the ampC and ampG expression levels.
2.9. Statistical analysis
Each experiment was done in triplicate (n = 3) and experimental values are presented as means +/- standard deviation. Statistical analysis was done using Prism5 (GraphPad Software, Inc.) and differences between means were considered significant when the confidence interval is lower than 5 % (***, P ≤ 0.001; **, P ≤ 0.01; *, P ≤ 0.05; student t test).
3. Results
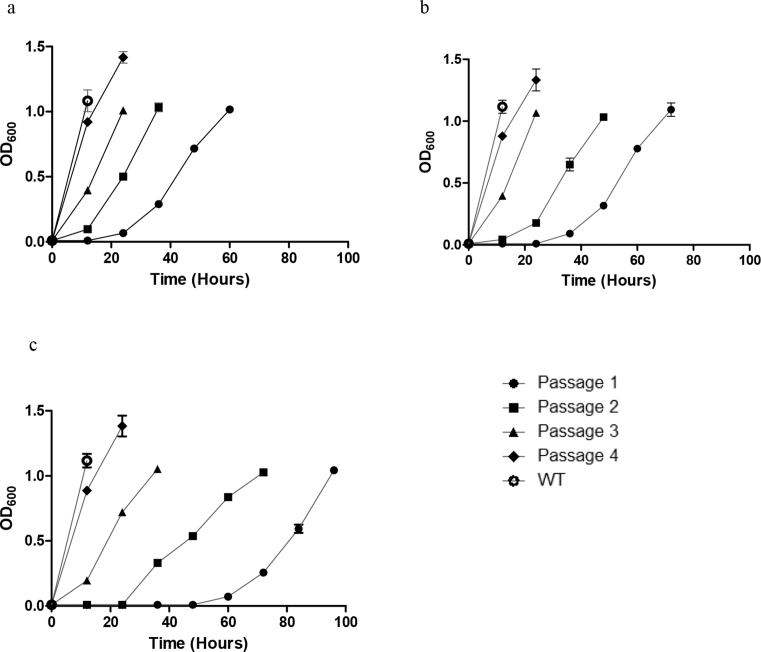
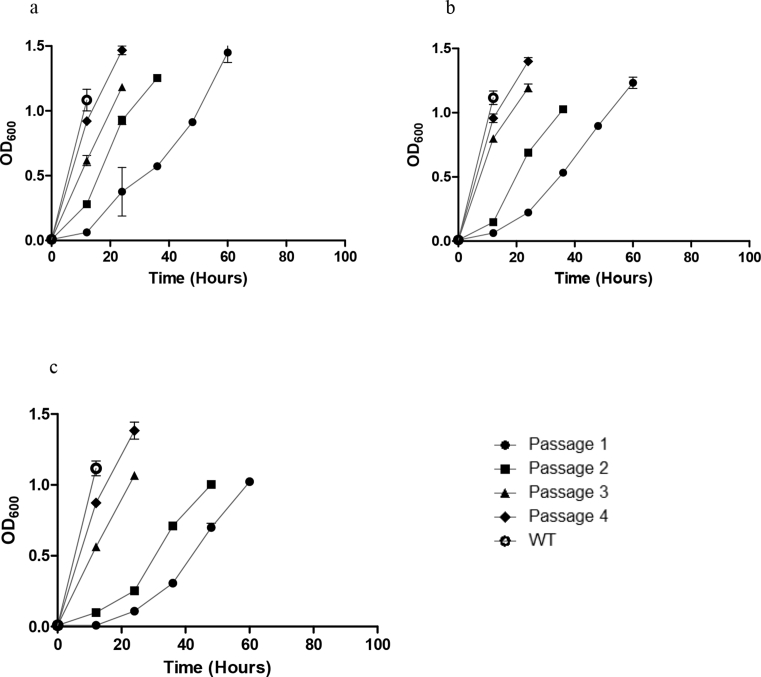
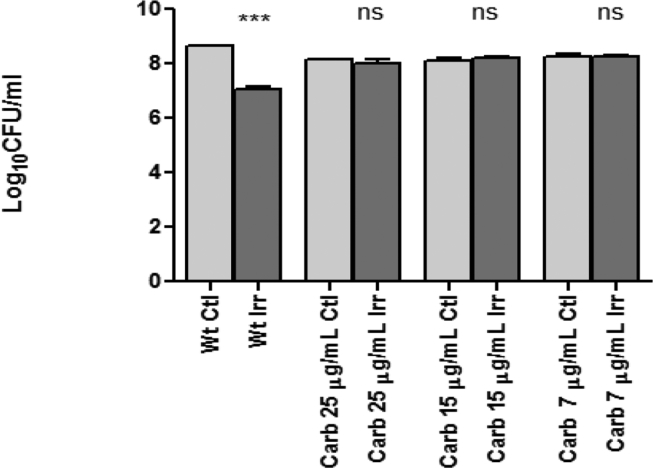
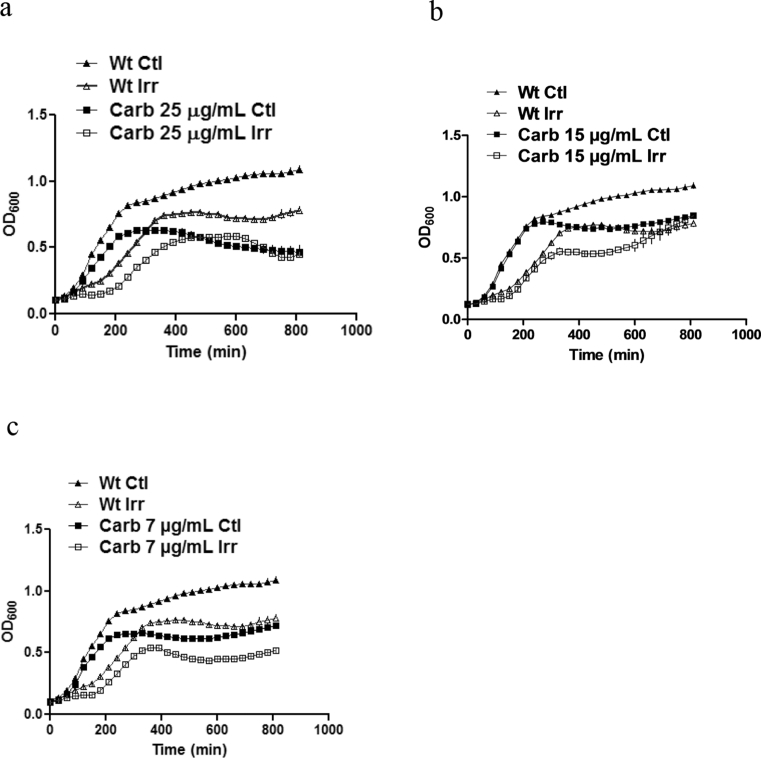
Two populations of E. coli O157:H7 were subcultured four times on various concentrations of carbenicillin (Carb25, Carb15 and Carb7) or kanamycin (Kan25, Kan15 and Kan7) until adaptation. Once these adapted bacteria were obtained, all remaining experiments were performed without antibiotic treatment. The bacterial growth rate increased according the number of passages and to the antibiotic concentration. O157:H7 was more easily adapted to kanamycin than to carbenicillin (Figs. 1 and 2). Adapted subpopulations were cultivated in TSB medium O/N at 37 °C, diluted at 1/100th and incubated at 37 °C until OD600 ≈ 1. The viability was then tested vs the Wt strain immediately following γ-irradiation treatment with 0.4 kGy (Fig. 3). As expected, irradiation significantly (P ≤ 0.001) reduced the counts of viable Wt bacteria (1.6 log reduction as compared to the control). The growth rate was also affected. In contrast, the same treatment had no significant effect on the survival (P > 0.05) of the carbenicillin-adapted subpopulations (Fig. 3). However, irradiation seems to have little effect on their growth (Fig. 4); and after 400 min and 600 min post-irradiation, respectively Carb25 and Carb15 were completely resistant (Fig. 4a and b).
Fig. 1.
Growth of carbenicillin-adapted E. coli O157:H7 strains to 7 μg/mL (a), 15 μg/mL (b) or 25 μg/mL (c) of carbenicillin by successive passages in TSB supplemented with antibiotic at the specified concentration (n = 4). Bacteria were incubated at 37 °C and 1/100th dilution was carried out from the culture at OD600 ≈ 1 and then sub-cultured for the next passage. 200 μL of each cell culture were used for growth monitoring.
Fig. 2.
Growth of kanamycin-adapted E. coli O157:H7 strains to 7 μg/mL (a), 15 μg/mL (b) or 25 μg/mL (c) of kanamycin by successive passages in TSB supplemented with antibiotic at the specified concentration (n = 4). Bacteria were incubated at 37 °C and 1/100th dilution was carried out from the culture at OD600 ≈ 1 and then sub-cultured for the next passage. 200 μL of each cell culture were used for growth monitoring.
Fig. 3.
Viability of E. coli O157:H7 (Wt or carbenicillin-adapted subpopulations) treated or not with irradiation at 0.4 kGy. Immediately after irradiation treatment, five μL of each cell culture were used. Results are represented by log10 of CFU/mL. Carb: carbenicillin adapted bacteria; Ctl: control non-irradiated; Irr: irradiated.
Fig. 4.
Growth of E. coli O157:H7, wild type and subpopulations -adapted to (a) 25 μg/mL, (b) 15 μg/mL or (c) 7 μg/mL carbenicillin, then treated or not with irradiation at 0.4 kGy. 200 μL of each cell culture were used. Carb: carbenicillin adapted bacteria; Ctl: control non-irradiated; Irr: irradiated.
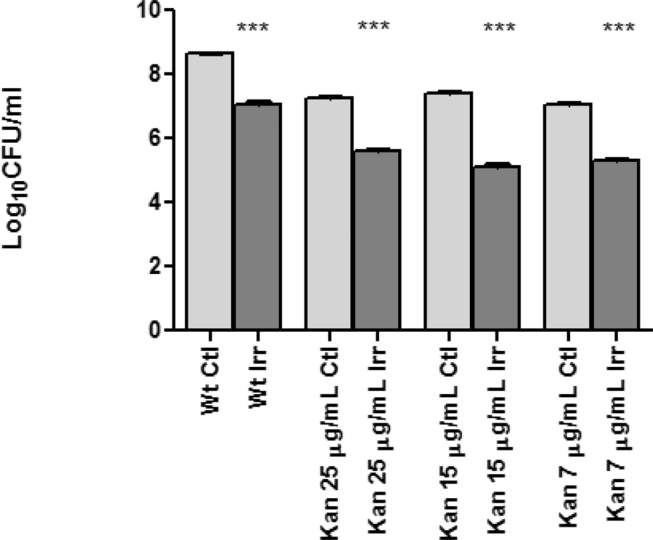
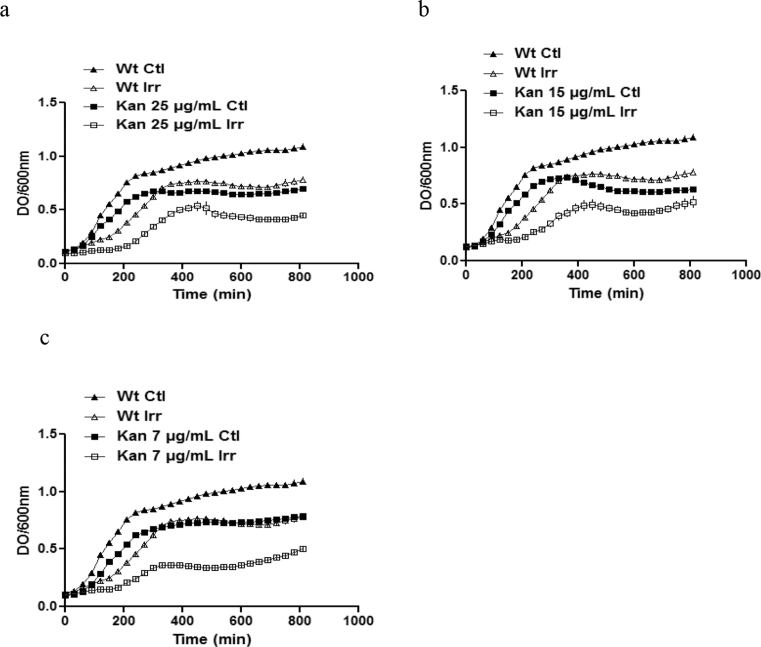
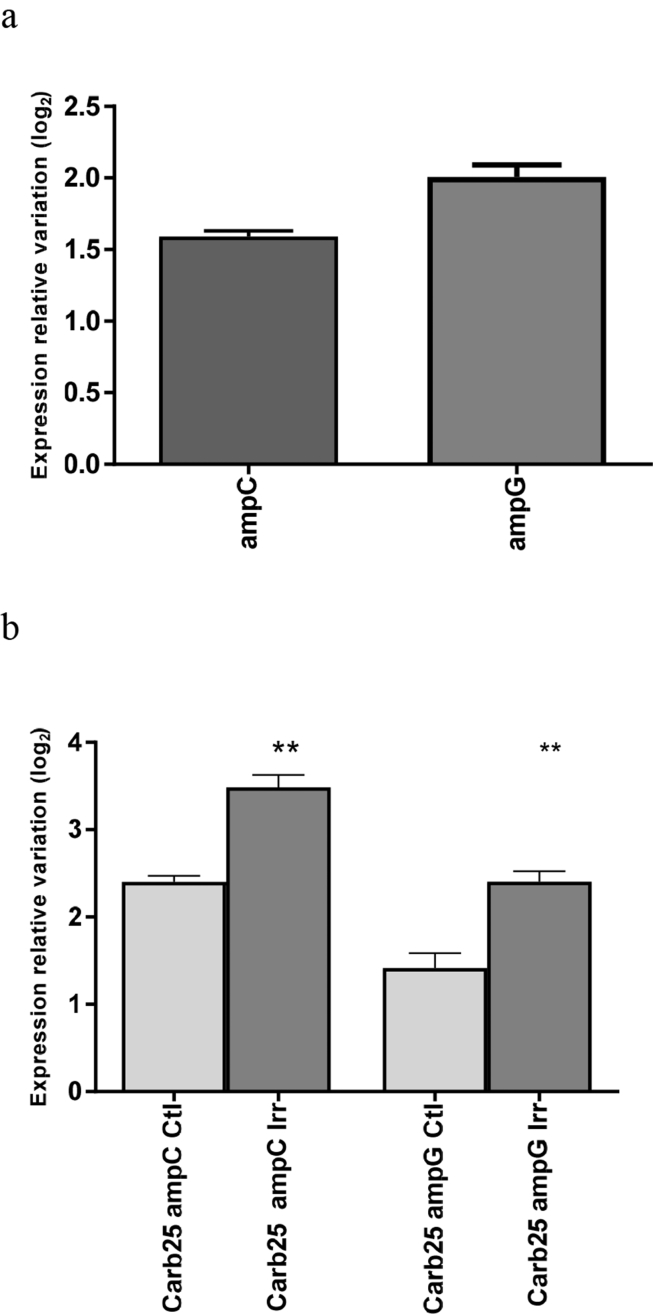
These observations show that bacterial adaptation to high concentrations of carbenicillin (i.e. ≥15 μg/mL) confers resistance to γ-irradiation. In contrast to carbenicillin, the adaptation of E. coli O157:H7 to different concentrations of kanamycin did not increase its radioresistance and a significant difference was observed between irradiated and non-irradiated cells adapted to the three concentrations of kanamycin (Figs. 5 and 6). The reduction level was 1.4, 1.8, 2 and 1.6 log10 CFU/mL for Wt and adapted E. coli to 7, 15 and 25 μg/mL, respectively (Fig. 5). These results were confirmed by evaluating E. coli growth after treatment (Fig. 6). A significant difference was observed throughout the whole experimental period between irradiated and non-irradiated E. coli cells adapted to the three concentrations of kanamycin. These results indicate that kanamycin has no effect on the development of resistance to 0.4 kGy irradiation treatment in E. coli O157:H7. The transcription of ampC and ampG was assessed by qRT-PCR 60 min after irradiation at 0.4 kGy. The results (Fig. 7a) demonstrate that irradiation treatment of E. coli led to a significant increase (P ≤ 0.01) in the expression of ampC and ampG, showing respectively an increase of 1.6 and 2-fold at 60 min post-treatment compared to the non-irradiated control. Interestingly, even without irradiation treatment, the expression of ampC was 2.4-fold higher in Carb25 than in the Wt. No significant difference (P > 0.01) was observed on the ampG expression. Moreover, irradiation treatment at 0.4 kGy further increased the expression of both ampC and ampG genes by 1 log2 in Carb25 bacteria (Fig. 7b). Sequencing of the Carb25 ampC and ampG genes revealed no mutation, compatible with an adaptation to carbenicillin promoted by modifications in gene expression.
Fig. 5.
Viability of E. coli O157:H7 (wild type and kanamycin adapted type) treated or not with irradiation at 0.4 kGy. 5 μL of each cell culture were used. Results are represented by log10 of CFU in 1 mL. Kan: kanamycin adapted bacteria; Ctl: control non-irradiated; Irr: irradiated.
Fig. 6.
Growth of E. coli O157:H7, wild type and kanamycin adapted type to (a) 25 μg/mL (b) 15 μg/mL and (c) 7 μg/mL treated or not with irradiation at 0.4 kGy. 200 μL of each cell culture were used. Kan: kanamycin adapted bacteria; Ctl: control non-irradiated; Irr: irradiated.
Fig. 7.
Effect of γ-irradiation on ampC and ampG expression of E. coli O157:H7; (a): in wild type bacteria. (b): in 25 μg/mL carbenicillin adapted bacteria (Carb25). Relative gene expression represents the change in transcription in bacteria 60 minutes after irradiation treatment at a dose of 0.4 kGy. Results are represented by log2 RNA expression using −2ΔΔCt. The difference was considered as significant when the expression relative variation ≥1.5 log2. Carb25: 25 μg/mL carbenicillin adapted bacteria, NI: not irradiated and Irr: irradiated.
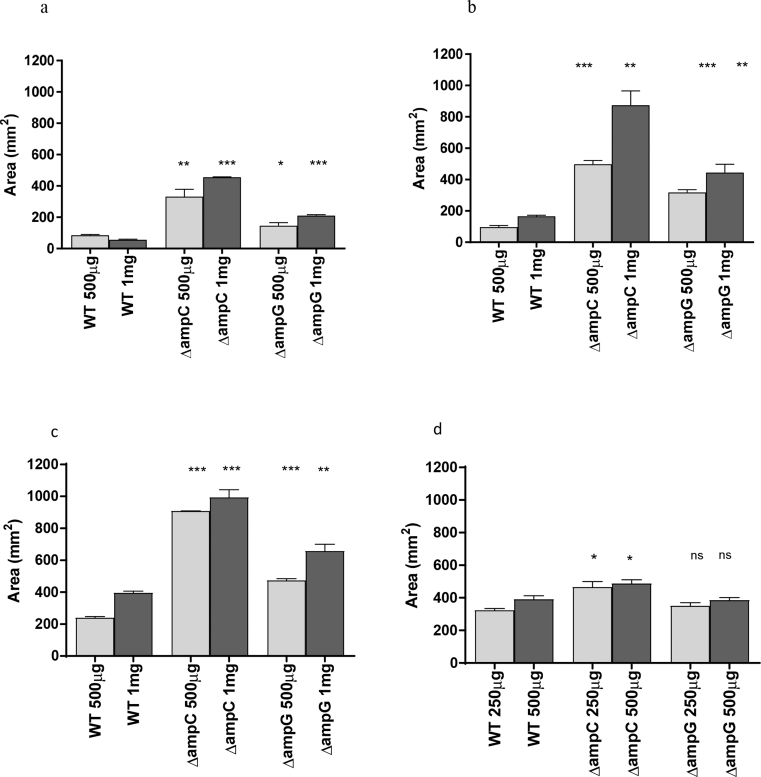
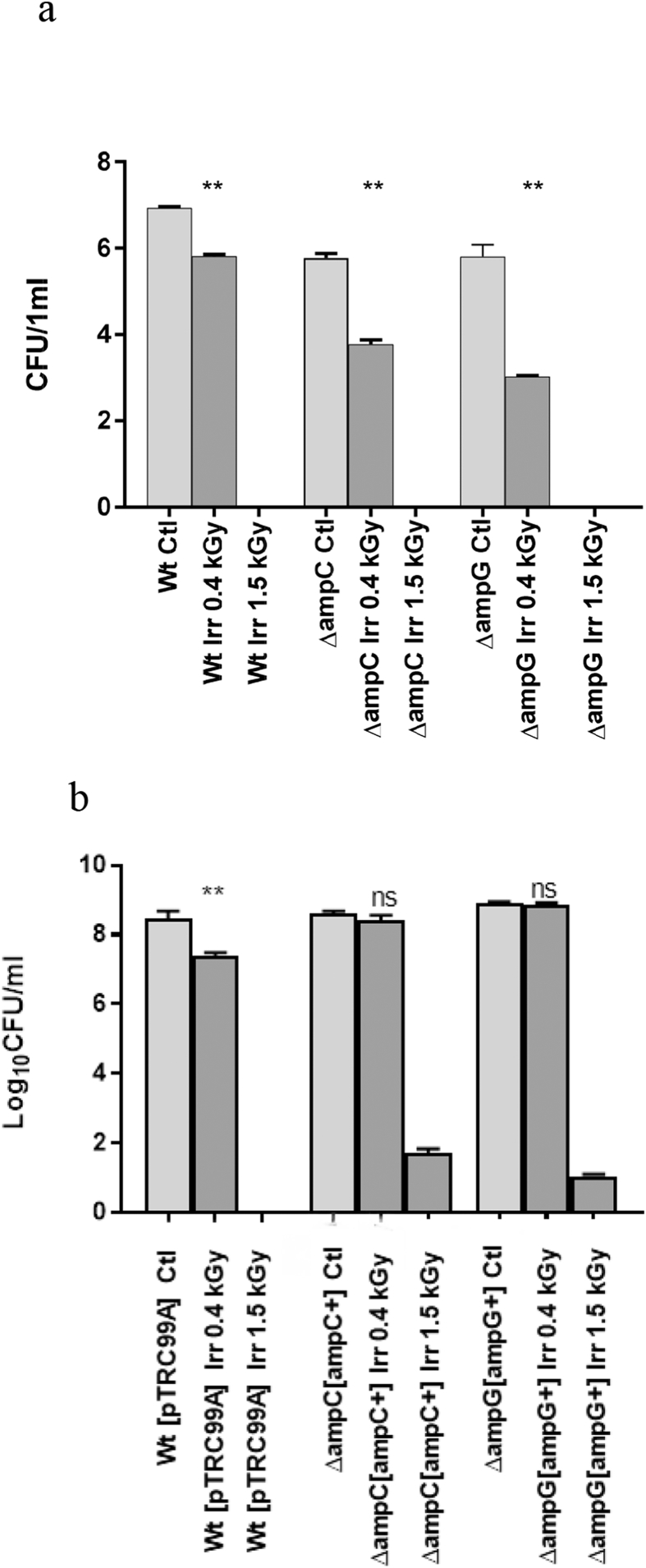
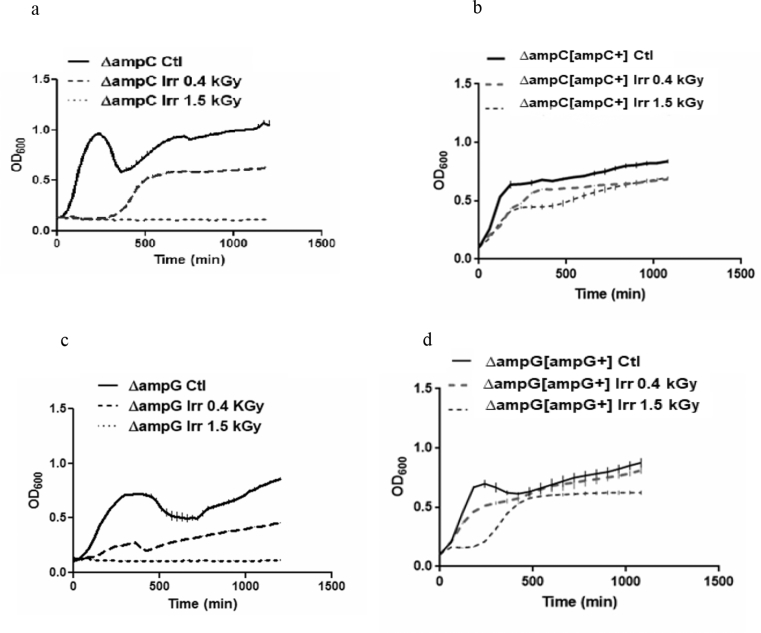
To further investigate the effect of these genes on the radioresistance of E. coli O157:H7, mutants in these genes were generated. As expected, the antibiogram results showed that ΔampC and ΔampG mutants are very sensitive to β-lactam antibiotics (ampicillin, piperacillin and carbenicillin) (Fig. 8 a,b,c). This sensitivity is dose-dependent and was higher with carbenicillin compared to the other antibiotics. In contrast, no significant effect of kanamycin on the ΔampG mutant and only a little effect on the ΔampC mutant were observed (Fig. 8d). Since the carbenicillin-adapted subpopulations were more resistant to γ-irradiation treatments, we tested whether the mutants with more sensitivity to β-lactam antibiotics would behave the opposite way. The effects of γ-irradiation at sensitization dose of 0.4 kGy and lethal dose of 1.5 kGy on the viability and the growth of E. coli ΔampC and ΔampG mutants are shown in Figs. 9a and 10a. The data demonstrate that inactivation of ampC and ampG increased the sensitivity of the cells to irradiation treatment at a dose of 0.4 kGy. Viability was reduced by 2 and 2.8 log10 CFU/mL in ΔampC and ΔampG mutants, respectively, as compared to only 1.1 log10 CFU/mL reduction in the Wt. To verify the effect of ampC and ampG deletion in radiosensitivity, E. coli ΔampC and ΔampG mutants were complemented respectively, by ampC and ampG genes on pTRC99A plasmid which is inducible by IPTG. Irradiation response of ΔampC overexpressing ampC (ΔampC[ampC+]) and ΔampG overexpressing ampG (ΔampG[ampG+]) was compared to Wt[pTRC99A] as a control. Very interestingly, the complemented mutants overexpressing the corresponding gene (ΔampC[ampC+] and ΔampG[ampG+]) became completely resistant to irradiation at the sensitization dose (Fig. 9) with only a limited growth difference with the Wt (Fig. 10). Even more, these overexpressing mutants were able to survive and grow after irradiation treatment at a dose of 1.5 kGy which is completely lethal for ΔampC and ΔampG mutants and for Wt O157:H7 (Figs. 9 and 10). Our findings suggest that AmpC and AmpG may intervene in the radioresistance of E. coli O157:H7.
Fig. 8.
Antibiotics susceptibility assays on E. coli O157:H7 ampC, ampG or ampR mutants. The disk containing 500 μg or 1 mg of (a) ampicillin, (b) piperacillin and (c) carbenicillin or 250 or 500 μg of (D) kanamycin was placed onto the surface of the agar plates. Inhibition area = (R2 × π).
Fig. 9.
Viability of E. coli strains: a: viability of ΔampC and ΔampG. E. coli. b: viability of ΔampC[ampC+] and ΔampG[ampG+]. E. coli. 5 μL of each cell culture were used. Results are represented by log10 of CFU in 1 mL. Ctl: control non-irradiated; Irr: irradiated; 0.4 kGy: sensitive dose; 1.5 kGy: lethal dose.
Fig. 10.
Growth after γ-irradiation of E. coli O157:H7 ΔampC (a), ΔampC-ampC (b), ΔampG (c) or ΔampG-ampG (d). 200 μL of each cell culture were used. Ctl: control non-irradiated; Irr: irradiated; 0.4 kGy: sensitive dose; 1.5 kGy: lethal dose.
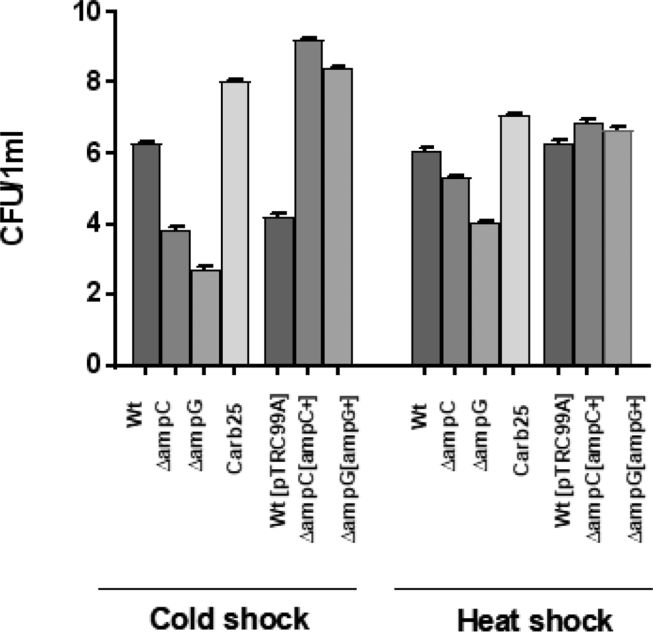
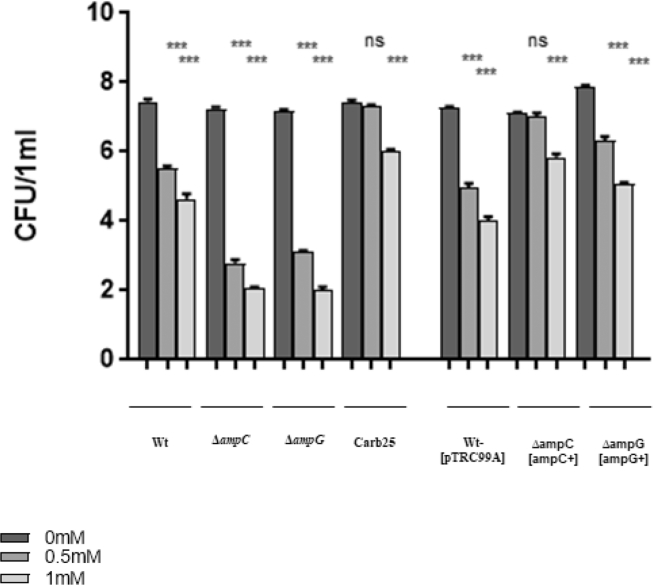
Since response mechanisms to stresses are often redundant, we also evaluated the effect of these two genes in the response to other stress like oxidative (paraquat), heat and cold stress. Interestingly, in contrast with the Wt and the ampC and ampG mutants, Carb25, ΔampC[ampC+], and ΔampG[ampG+] strains were all able to survive and grow after incubation at 50 °C for 2 h or 1 week at 4 °C and in presence of 0.5 mM or 1 mM paraquat, metabolic generator of superoxide (Figs.11 and 12).
Fig. 11.
Viability of E. coli O157:H7 strains under thermal stress: The bacteria at the exponential phase of growth (OD600 ≈ 1) are cultured in TSB and incubated at 50 °C for 2h (heat shock) or at 4 °C for 1 week (cold shock). 5 μL of each cell culture were used. Results are represented by log10 of CFU.
Fig. 12.
Viability of E. coli O157:H7 strains under paraquat stress: The bacteria at the exponential phase of growth (OD600 ≈ 1) are cultured in TSB supplemented with 0.5 or 1mM of paraquat and incubated at 37 °C for 40 min. 5 μL of each cell culture were used. Results are represented by log10 of CFU.
4. Discussion
In the present study, we have demonstrated that the resistance of E. coli O157:H7 to some antibiotic types could reduce its sensitivity to irradiation treatment at a dose that is normally lethal. In fact, our results show that an E. coli O157:H7 subpopulation adapted to carbenicillin recovered growth faster than wild type bacteria following an irradiation treatment at the sensitization dose (Figs. 3 and 4). This was not the case for a subpopulation of E. coli O157:H7 adapted to kanamycin (Figs. 5 and 6). We also demonstrated that the viability and the growth of the adapted bacteria were affected as compared to the Wt. This could be the result of a trade-off phenomenon, which is a negative correlation between stress resistance/adaptation and growth bacteria like pathogenic E. coli (Basra et al., 2018). These findings suggest that the acquisition of radioresistance after a bacterial adaptation to antibiotics depends on the class of antibiotic.
Wesche et al. (2009) reported that microorganisms that survive a given stress could gain resistance to that stress or another one. This phenomenon is attributable to the cross-protection mechanisms found in the bacteria and has an important impact on the industrial process conditions and food safety. While there is an increasing evidence of a relationship between different stress resistances, few studies have focused on the evaluation of the effect of bacterial resistance to a given stress on radioresistance. Collectively, it is possible that resistance to β-lactam antibiotics is responsible for some mechanism of resistance to an irradiation treatment at a dose of 0.4 kGy.
Peptidoglycan turnover and recycling are among the most important processes in bacterial life cycle. These mechanisms are involved in the regulation of virulence and the resistance response (Folkesson et al., 2005; Boudreau et al., 2012). The β-lactamase AmpC, produced by some Gram-negative bacteria, can interact with many β-lactam antibiotics including ampicillin, carbenicillin, penicillin and piperacillin (Sanders Jr and Sanders Jr, 1986). One of the regulators of this protein is the permease AmpG which imports peptidoglycan-derived product, named muropeptide, to the cytoplasm where it activates the transcription of ampC (Korfmann and Sanders, 1989; Yang et al., 2013).
To evaluate the impact of the β-lactam resistance on the E. coli O157:H7 radioresistance, we assessed the expression of two genes required for β-lactamase activity in E. Coli (i.e. ampC and ampG) under γ-irradiation treatment. These marker genes were selected based on RNA-seq results demonstrating that their expression increases in E. Coli O157:H7 following 0.4 kGy irradiation treatment (unpublished data). We have showed that the expression of both genes was significantly increased (Fig. 7) confirming our RNA-seq results. Collectively, these findings indicate that AmpC and AmpG could be related to E. coli O157:H7 radioresistance. In addition, ΔampC and ΔampG mutants in strain O157:H7 showed an important sensitivity towards different β-lactam antibiotics (Figs. 9a and 10a), consistent with previous studies that have reported a role of these genes in the resistance of other E. Coli strains to β-lactams (Sanders, 1987; Lindquist et al., 1993).
In the current study, we have also demonstrated that γ-irradiation up-regulates ampC and ampG expression of both Wt and Carb25 O157:H7 (Fig. 7). This could be explained by the response of E. coli to muropeptides distribution by increasing ampC and ampG expression, which then promotes resistance. In fact, Caillet et al. (2005) reported that irradiation treatment affects the peptidoglycan recycling by modification of the distribution of muropeptides on E. coli, probably as a result of modification to the glycan-binding peptides. Peptidoglycan recycling is important for cell growth and division (Park and Uehara, 2008). The AmpG permease can transport GlcNAc-anhMurNAc-peptides, a peptidoglycan degradation product, to the cytoplasm where it is lysed by the β-glucosaminidase NagZ to produce anhMurNAc-peptides, which are then metabolized to UDPMurNAc-pentapeptides or by ampD to generate GlcNAc, anhMurNAc, murein tripeptide, and D-Ala. Murein tripeptide is ligated to UDP-MurNAc, therefore returning it to the murein synthesis pathway. In absence of β-lactam, UDPMurNAc-pentapeptide binds AmpR and converts it into a repressor of ampC transcription. In presence of a β-lactam, anhMurNAc-peptides accumulate and bind AmpR which then leads to the activation of ampC transcription (Dietz et al., 1997; Jacobs et al., 1997). The inactivation of ampG results in non-inducible and micro-constitutive β-lactamase phenotypes to the bacterial cell, correlating peptidoglycan recycling and β-lactamase induction (Korfmann and Sanders, 1989; Lindquist et al., 1993).
On the other hand, ΔampC[ampC+] and ΔampG[ampG+] strains overproducing AmpC and AmpG respectively and of Carb25 were paraquat resistant (Fig. 11). In fact, sub-lethal concentrations of ampicillin or norfloxacin were associated with ROS-induced mutagenesis in E. coli and Staphylococcus aureus (S. Aureus) (Cuirolo et al., 2009; Kohanski et al., 2010). In addition, β-lactam-induced clinical hetero-resistant S. aureus is associated with oxidative stress via increasing ROS production and DNA damage, both factors responsible of SOS response induction (Rosato et al., 2014). This suggests that carbenicillin, similarly to ampicillin, leads to this mutagenesis induced by ROS and activates genes involved in the SOS response. Consequently, when E. coli O157:H7 was irradiated, it had all the resistance machinery already activated, which may have contributed to its radioresistance when adapted to carbenicillin, not to kanamycin (Figs. 3 and 6).
Also, in E. coli O157:H7, we see that overexpression of ampC or ampG promotes heat and cold stress resistance (Fig. 12), maybe because AmpR effect on thermic tolerance, is similar to what is observed in Pseudomonas aeruginosa and this by increasing the expression of DnaJ-DnaK-GrpE Hsp70 system, involved in heat stress response (Balasubramanian et al., 2014) and by controlling cold stress response. On the basis of these observations, it appears that the type of stress applied on E. coli O157:H7 affects the response to other types of stress.
Gene ampR is involved in the oxidative stress response of Pseudomonas aeruginosa (Balasubramanian et al., 2014). In the present study, the ΔampC and ΔampG mutants were more sensitive to irradiation treatment compared to the Wt. In the ΔampG mutant, anhMurNAc-peptides probably accumulate in the periplasm, resulting in no production of UDPMurNAc-pentapeptide. It is thus possible that UDPMurNAc-pentapeptide plays a role in the activation of the oxidative stress response by its interaction with ampR. In this context, E. coli becomes less resistant to an irradiation treatment when there is no interaction. These observations suggest that AmpC may be involved in E. coli O157:H7 radioresistance by a direct ROS genes synthesis control or interaction with ampR (Figs. 9-a-10b). Moreover, different growth profiles of ΔampC and ΔampG mutants were observed (Fig. 10). This could be related to the perturbation in peptidoglycan recycling caused by the absence of ampC or ampG, thus affecting cell growth and division (Park and Uehara, 2008).
In E. coli, various mutations in the ampC promoter/attenuator region, in ampG, in ampD or in ampR genes may lead to constitutive overproduction of AmpC beta-lactamases (Kopp et al., 1993; Caroff et al., 1999; Kuga et al., 2000). We have amplified and sequenced the ampC and ampG genes of Carb25 adapted bacteria and no mutation was detected in ampC promoter region, in ampC gene or in ampG genes, suggesting that carbenicillin adaptation leads to AmpC overproduction (Fig. 7b) by mutation in other regulatory elements, such as ampR or ampD but not in ampG. In this case, we can suppose that in Carb25 adapted bacteria, irradiation stress is important to induce the positive regulatory mechanism involving AmpG. In absence of this stress, AmpC overexpression maybe is favored especially by AmpR and/or AmpD.
In conclusion, the results of this study clearly demonstrate that in addition to their contribution in antibiotic resistance, ampC and ampG genes modulate the resistance of E. coli O157:H7 to γ-irradiation and may be to other stress like oxidative, cold and heat stress. Transcriptomic studies of ΔampC and sequencing of Carb25 complete genome could be assessed to confirm respectively the hypothesis of the role of ampC in inducing radioresistance by the control of the peptidogycan recycling and to determine the genes involved in carbenicillin adaptation in E. coli O157:H7. These results can be of great interest to the food industry and especially for irradiation treatment of meat from β-lactam treated animals, which could affect the efficiency of irradiation treatment. Since kanamycin did not show any effect on the radioresistance, it will be important to investigate the effects of additional antibiotic classes currently used in animal production to verify their effects on the radioresistance or resistance to other stress of E. coli O157:H7.
Declarations
Author contribution statement
Ghizlane Gaougaou, Yosra Ben-Fadhel: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Eric Deziel, Monique Lacroix: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This work was supported by the Natural Science and Engineering Research Council of Canada (NSERC, Discovery program).
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We thank Nordion for performing the irradiation treatment. Pr. Charles Dozois for providing bacterial strain and Sébastien Houle, Marie-Christine Groleau and Gabrielle Gendron-Lepage for their technical help.
References
- Amann E., Ochs B., Abel K.-J. Tightly regulated tac promoter vectors useful for the expression of unfused and fused proteins in Escherichia coli. Gene. 1988;69(2):301–315. doi: 10.1016/0378-1119(88)90440-4. [DOI] [PubMed] [Google Scholar]
- Baba T., Ara T., Hasegawa M., Takai Y., Okumura Y., Baba M., Datsenko K.A., Tomita M., Wanner B.L., Mori H. Construction of Escherichia coli K-12 in-frame, single-gene knockout mutants: the Keio collection. Mol. Syst. Biol. 2006;2(1) doi: 10.1038/msb4100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian D., Kumari H., Jaric M., Fernandez M., Turner K.H., Dove S.L., Narasimhan G., Lory S., Mathee K. Deep sequencing analyses expands the Pseudomonas aeruginosa AmpR regulon to include small RNA-mediated regulation of iron acquisition, heat shock and oxidative stress response. Nucleic Acids Res. 2014;42(2):979–998. doi: 10.1093/nar/gkt942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basra P., Alsaadi A., Bernal-Astrain G., O’Sullivan M.L., Hazlett B., Clarke L.M., Schoenrock A., Pitre S., Wong A. Fitness tradeoffs of antibiotic resistance in extraintestinal pathogenic Escherichia coli. Genome Biol. Evol. 2018;10(2):667–679. doi: 10.1093/gbe/evy030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Fadhel Y., Leroy V., Dussault D., St-Yves F., Lauzon M., Salmieri S., Jamshidian M., Vu D.K., Lacroix M. Combined effects of marinating and γ-irradiation in ensuring safety, protection of nutritional value and increase in shelf-life of ready-to-cook meat for immunocompromised patients. Meat Sci. 2016;118:43–51. doi: 10.1016/j.meatsci.2016.03.020. [DOI] [PubMed] [Google Scholar]
- Boudreau M.A., Fisher J.F., Mobashery S. Messenger functions of the bacterial cell wall-derived muropeptides. Biochemistry. 2012;51(14):2974. doi: 10.1021/bi300174x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caillet S., Shareck F., Lacroix M. Effect of gamma radiation and oregano essential oil on murein and ATP concentration of Escherichia coli O157: H7. J. Food Protect. 2005;68(12):2571–2579. doi: 10.4315/0362-028x-68.12.2571. [DOI] [PubMed] [Google Scholar]
- Caroff N., Espaze E., Berard I., Richet H., Reynaud A. Mutations in the ampC promoter of Escherichia coli isolates resistant to oxyiminocephalosporins without extended spectrum β-lactamase production. FEMS Microbiol. Lett. 1999;173(2):459–465. doi: 10.1111/j.1574-6968.1999.tb13539.x. [DOI] [PubMed] [Google Scholar]
- Carone B.R., Xu T., Murphy K.C., Marinus M.G. High incidence of multiple antibiotic resistant cells in cultures of in enterohemorrhagic Escherichia coli O157: H7. Mutat. Res. Fund. Mol. M. 2014;759:1–8. doi: 10.1016/j.mrfmmm.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical and Laboratory Standards Institute . 2014. Performance Standards for Antimicrobial Susceptibility Testing Twenty-fourth Informational Supplement. [Google Scholar]
- Courvalin P. Predictable and unpredictable evolution of antibiotic resistance. J. Intern. Med. 2008;264(1):4–16. doi: 10.1111/j.1365-2796.2008.01940.x. [DOI] [PubMed] [Google Scholar]
- Cuirolo A., Plata K., Rosato A.E. Development of homogeneous expression of resistance in methicillin-resistant Staphylococcus aureus clinical strains is functionally associated with a β-lactam-mediated SOS response. J. Antimicrob. Chemother. 2009;64(1):37–45. doi: 10.1093/jac/dkp164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datsenko K.A., Wanner B.L. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. 2000;97(12):6640–6645. doi: 10.1073/pnas.120163297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz H., Pfeifle D., Wiedemann B. The signal molecule for beta-lactamase induction in Enterobacter cloacae is the anhydromuramyl-pentapeptide. J. Antimicrob. Chemother. 1997;41(10):2113–2120. doi: 10.1128/aac.41.10.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas J. Irradiation for better foods. Trends Food Sci. Technol. 2006;17(4):148–152. [Google Scholar]
- Folkesson A., Eriksson S., Andersson M., Park J.T., Normark S. Components of the peptidoglycan-recycling pathway modulate invasion and intracellular survival of Salmonella enterica serovar Typhimurium. Cell Microbiol. 2005;7(1):147–155. doi: 10.1111/j.1462-5822.2004.00443.x. [DOI] [PubMed] [Google Scholar]
- Health Canada . Veterinary Drugs Directorate HC. 2002. Uses of antimicrobials in food animals in Canada: impact on resistance and human health. [Google Scholar]
- Jacobs C., Frère J.-M., Normark S. Cytosolic intermediates for cell wall biosynthesis and degradation control inducible β-lactam resistance in gram-negative bacteria. Cell. 1997;88(6):823–832. doi: 10.1016/s0092-8674(00)81928-5. [DOI] [PubMed] [Google Scholar]
- Juan C., Moyá B., Pérez J.L., Oliver A. Stepwise upregulation of the Pseudomonas aeruginosa chromosomal cephalosporinase conferring high-level β-lactam resistance involves three AmpD homologues. Antimicrob. Agents Chemother. 2006;50(5):1780–1787. doi: 10.1128/AAC.50.5.1780-1787.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaneko K., Okamoto R., Nakano R., Kawakami S., Inoue M. Gene mutations responsible for overexpression of AmpC β-lactamase in some clinical isolates of Enterobacter cloacae. J. Clin. Microbiol. 2005;43(6):2955–2958. doi: 10.1128/JCM.43.6.2955-2958.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karmali M., Petric M., Steele B., Lim C. Sporadic cases of haemolytic-uraemic syndrome associated with faecal cytotoxin and cytotoxin-producing Escherichia coli in stools. Lancet. 1983;321(8325):619–620. doi: 10.1016/s0140-6736(83)91795-6. [DOI] [PubMed] [Google Scholar]
- Kohanski M.A., DePristo M.A., Collins J.J. Sublethal antibiotic treatment leads to multidrug resistance via radical-induced mutagenesis. Mol. Cell. 2010;37(3):311–320. doi: 10.1016/j.molcel.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopp U., Wiedemann B., Lindquist S., Normark S. Sequences of wild-type and mutant ampD genes of Citrobacter freundii and Enterobacter cloacae. Antimicrob. Agents Chemother. 1993;37(2):224–228. doi: 10.1128/aac.37.2.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korfmann G., Sanders C. ampG is essential for high-level expression of AmpC beta-lactamase in Enterobacter cloacae. Antimicrob. Agents Chemother. 1989;33(11):1946–1951. doi: 10.1128/aac.33.11.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutchma T., Forney L.J., Moraru C.I. CRC Press; 2009. Ultraviolet Light in Food Technology: Principles and Applications. [Google Scholar]
- Kuga A., Okamoto R., Inoue M. ampR gene mutations that greatly increase class C β-lactamase activity in Enterobacter cloacae. Antimicrob. Agents Chemother. 2000;44(3):561–567. doi: 10.1128/aac.44.3.561-567.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindquist S., Weston-Hafer K., Schmidt H., Pul C., Korfmann G., Erickson J., Sanders C., Martin H.H., Normark S. AmpG, a signal transducer in chromosomal β-lactamase induction. Mol. Microbiol. 1993;9(4):703–715. doi: 10.1111/j.1365-2958.1993.tb01731.x. [DOI] [PubMed] [Google Scholar]
- Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Livermore D.M. beta-Lactamases in laboratory and clinical resistance. Clin. Microbiol. Rev. 1995;8(4):557–584. doi: 10.1128/cmr.8.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loukiadis E., Kerouredan M., Oswald E., Brugere H. Virulence factors of enterohemorrhagic Escherichia coli (EHEC) in sewage of French slaughterhouses and environmental risk for public health. Epidemiology. 2006;17(6):S236. [Google Scholar]
- Normark S. β-Lactamase induction in gram-negative bacteria is intimately linked to peptidoglycan recycling. Microb. Drug Resist. 1995;1(2):111–114. doi: 10.1089/mdr.1995.1.111. [DOI] [PubMed] [Google Scholar]
- Park J.T., Uehara T. How bacteria consume their own exoskeletons (turnover and recycling of cell wall peptidoglycan) Microbiol. Mol. Biol. Rev. 2008;72(2):211–227. doi: 10.1128/MMBR.00027-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips C.A. The epidemiology, detection and control of Escherichia coli O157. J. Sci. Food Agric. 1999;79(11):1367–1381. [Google Scholar]
- Poole K. Resistance to β-lactam antibiotics. Cell. Mol. Life Sci. 2004;61(17):2200–2223. doi: 10.1007/s00018-004-4060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosato R.R., Fernandez R., Paz L.I., Singh C.R., Rosato A.E. TCA cycle-mediated generation of ROS is a key mediator for HeR-MRSA survival under β-lactam antibiotic exposure. PloS One. 2014;9(6) doi: 10.1371/journal.pone.0099605. e99605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabri M., Houle S., Dozois C.M. Roles of the extraintestinal pathogenic Escherichia coli ZnuACB and ZupT zinc transporters during urinary tract infection. Infect. Immun. 2009;77(3):1155–1164. doi: 10.1128/IAI.01082-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders C. Chromosomal cephalosporinases responsible for multiple resistance to newer β-lactam antibiotics. Annu. Rev. Microbiol. 1987;41(1):573–594. doi: 10.1146/annurev.mi.41.100187.003041. [DOI] [PubMed] [Google Scholar]
- Sanders C.C., Sanders W.E., Jr. Emergence of resistance during therapy with the newer β-lactam antibiotics: role of inducible β-lactamases and implications for the future. Rev. Infect. Dis. 1983;5(4):639–648. doi: 10.1093/clinids/5.4.639. [DOI] [PubMed] [Google Scholar]
- Sanders C.C., Jr., Sanders W.E., Jr. Type I β-lactamases of gram-negative bacteria: interactions with β-lactam antibiotics. J. Infect. Dis. 1986;154(5):792–800. doi: 10.1093/infdis/154.5.792. [DOI] [PubMed] [Google Scholar]
- Schmidtke A.J., Hanson N.D. Role of ampD homologs in overproduction of AmpC in clinical isolates of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2008;52(11):3922–3927. doi: 10.1128/AAC.00341-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tóth I., Csík M., Emçdy L. Spontaneous antibiotic resistance mutation associated pleiotropic changes in Escherichia coli O157: H7. Acta Vet. Hung. 2003;51(1):29–44. doi: 10.1556/AVet.51.2003.1.3. [DOI] [PubMed] [Google Scholar]
- Wesche A.M., Gurtler J.B., Marks B.P., Ryser E.T. Stress, sublethal injury, resuscitation, and virulence of bacterial foodborne pathogens. J. Food Protect. 2009;72(5):1121–1138. doi: 10.4315/0362-028x-72.5.1121. [DOI] [PubMed] [Google Scholar]
- Yang T.-C., Chen T.-F., Tsai J.J., Hu R.-M. AmpG is required for BlaXc beta-lactamase expression in Xanthomonas campestris pv. campestris str. 17. FEMS Microbiol. Lett. 2013;340(2):101–108. doi: 10.1111/1574-6968.12071. [DOI] [PubMed] [Google Scholar]
- Zeng X., Lin J. Beta-lactamase induction and cell wall metabolism in Gram-negative bacteria. Front. Microbiol. 2013;4:128. doi: 10.3389/fmicb.2013.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]