Abstract
The diagnosis of multiple myeloma can be challenging, even for experienced physicians, and requires close collaboration between numerous disciplines (orthopedics, radiology, nuclear medicine, radiation therapy, hematology and oncology) before the final diagnosis of myeloma is made. The definition of multiple myeloma is based on the presence of clinical, biochemical, histopathological, and radiological markers of disease. Specific tests are needed both at presentation and during follow-up in order to reach the correct diagnosis and characterize the disease precisely. These tests can also serve prognostic purposes and are useful for follow-up of myeloma patients. Molecular analyses remain pivotal for defining high-risk myeloma and are used in updated patient stratifications, while minimal residual disease assessment via flow cytometry, molecular techniques and radiological approaches provides additional prognostic information on patients’ long-term outcome. This pivotal information will guide our future treatment decisions in forthcoming clinical trials. The European Myeloma Network group updated their guidelines on different diagnostic recommendations, which should be of value to enable appropriate use of the recommendations both at diagnosis and during follow-up.
Introduction
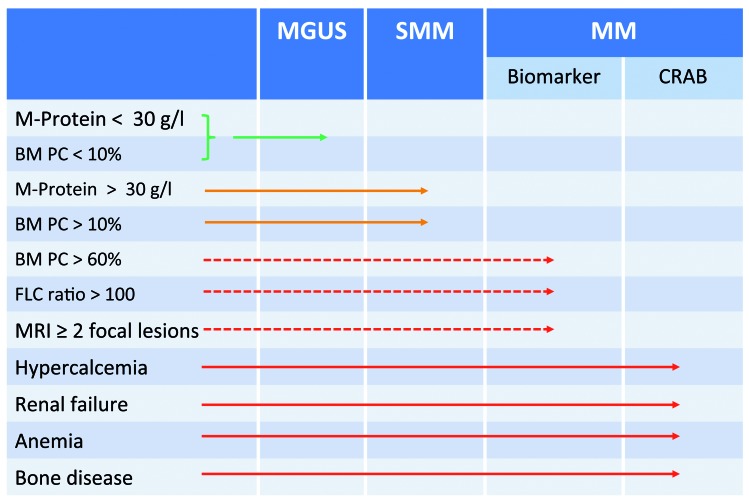
The classification and differential diagnosis of monoclonal gammopathies is based on clinical, biological and radiological criteria but remains challenging in certain cases. Multiple myeloma (MM) is the most common malignant gammopathy and is associated with a wide spectrum of signs and symptoms.1 In the past decade, the treatment options for patients with MM have increased considerably. Together with improved supportive care, these new regimens significantly prolong the survival of both younger and older patients.2 The 2014 revision of the diagnostic criteria for MM allows the initiation of treatment in patients defined only by biomarkers, annotated as SLIM criteria [bone marrow (BM) infiltration >60%, involved/uninvolved serum free light-chain (SFLC) ratio >100 or >1 focal lesion >5 mm as determined by magnetic resonance imaging (MRI)], without waiting for conventional CRAB criteria (hypercalcemia, renal impairment, anemia, bone disease) to occur.3,4 Both the SLIM biomarker and CRAB criteria are listed in Figure 1. Given the recent evolution in diagnosis and response assessment, members of the European Myeloma Network (EMN) agreed to review and recommend diagnostic and response criteria to allow their discriminating use in daily practice and current care of patients’.
Figure 1.
The differential diagnosis between monoclonal gammopathy of undetermined significance, smoldering myeloma and multiple myeloma. The discrimination between these monoclonal gammopathies is based on: (i) the plasma cell infiltration in the bone marrow, (ii) the presence of clinical symptoms related to myeloma disease and (iii) the existence of biomarkers of disease that allow initiation of treatment. MGUS: monoclonal gammopathy of undetermined significance; SMM: smoldering multiple myeloma; MM: multiple myeloma; BM: bone marrow; PC: plasma cells; FLC: free light chain; MRI: magnetic resonance imaging.
Methodology
These recommendations were developed by a panel of clinical experts on MM based on evidence of published data through August 2017. Expert consensus was used to suggest recommendations, where sufficient data were lacking. The final recommendations were classified based on the GRADE criteria,5 which incorporates the strength and quality of evidence (Online Supplementary Table S1). Based on discussions at the 2017 EMN Trialist meeting (Baveno, Italy) guidelines were prepared and circulated among all panel members. The manuscript subsequently underwent revision in three rounds until the EMN experts reached consensus. In line with the guidelines of the International Committee of Medical Journal Editors, authorship was based on active contribution during discussion, writing and revision of the guidelines.
European Myeloma Network recommendations
Diagnostic tools
Blood tests
A defining feature of plasma cell (PC) disorders is the secretion of monoclonal immunoglobulins, often referred to as a monoclonal M-protein, which can be used as a diagnostic marker, but also for the follow-up of the disease. Its heavy- and light-chain components can be identified by immunofixation and further quantified by serum protein electrophoresis and/or a serum free light-chain (SFLC) assay. It should be kept in mind that with persisting disease and possible de-differentiation of myeloma cells, the capacity to produce M-proteins may decrease or be completely lost (light-chain escape). In those patients, low M-protein levels, the presence of light chains only, or even complete absence of M-proteins and light chains may be mistaken as an ongoing or evolving response.6
Of note, immunofixation is approximately 10-fold more sensitive than serum protein electrophoresis and is required at diagnosis to characterize the phenotype of the M-protein, and for confirmation of a complete response, which is defined as being immunofixation-negative.7 Serum electrophoresis and immunofixation may not be able to detect light-chain aberrations in patients with oligo-secretory disease, such as light-chain MM. Due to their low molecular weight, these SFLC are rapidly cleared by the kidneys. In such cases, the monoclonal burden should be measured in a 24 h urine collection or in the serum by an automated SFLC immunoassay (Grade 1A), the latter having a higher sensitivity to detect and quantify the involved free light chains.7 In concordance with the International Myeloma Working Group (IMWG), we recommend the performance of serum immunofixation and electrophoresis on serum and urine samples and a SFLC assay for the diagnosis of a monoclonal PC disorder (Grade 1A).
Additional laboratory tests should be performed for the diagnosis and follow-up of MM patients, such as a complete blood count to evaluate possible cytopenias, blood smears to look for circulating PC and general biochemistry tests (renal and liver function tests, calcium, phosphate, uric acid, albumin, creatinine, lactate dehydrogenase, C-reactive protein, β2-microglobulin). Quantification of serum immunoglobulins by nephelometry enables an indirect measurement of the M-protein or the recognition of a secondary hypogammaglobinemia and is recommended for any patient presenting with a gammopathy (oligo-, poly- or monoclonal) (Grade 1A).
The HevyLite® immunoassay quantifies both the involved and uninvolved intact immunoglobulin chains and quantifies them separately (IgGκ/λ, IgAκ/λ, IgMκ/λ).8 This assay has prognostic value for progression-free and overall survival9 and seems particularly useful when the M-protein is difficult to measure via serum protein electrophoresis. This assay is not yet part of the routine workup of MM patients, but may be of value in the followup of patients and has been included in clinical trials.10
Urine analysis
Proteinuria should be assessed on urine samples from all patients at diagnosis and during the follow-up. If proteinuria is present, it should be quantified in a 24 h urine collection. Total 24 h protein and Bence-Jones proteinuria should be evaluated by densitometry, electrophoresis and immunofixation. To detect low amounts of monoclonal proteins, it is recommended that the urine is concentrated 200-fold.11 These 24 h urine collections are often inconsistently performed, resulting in incomplete urine collection. In addition, renal function can influence the accuracy of the results, a fact which should be taken into consideration when interpreting laboratory values. The SFLC assay can be used for the follow-up of patients with light-chain MM. A recent French study, focusing on patients with light-chain MM, demonstrated that the SFLC assay is superior to 24 h urine collection for: (i) identifying patients with measurable disease, (ii) following their response to initial therapy, and (iii) giving a prognostic indication of the patients’ response and overall survival.12 This study included 113 patients with light-chain MM, all of whom had an abnormal SFLC ratio and measurable disease parameters in serum, while only 64% patients had measurable M-proteins in the urine, as determined by urine protein electrophoresis. Similar results were found in 576 patients with light-chain MM from the UK Myeloma IX and XI trials. The disease burden of the patients with light-chain MM could be measured and monitored by urine protein electrophoresis in 80% of cases. Of the remaining patients 113 (97%) had involved free light chains >100 mg/L, which was sufficient to measure response to therapy.13 These two studies confirmed the importance of SFLC measurements to diagnose and monitor patients with light-chain or oligosecretory MM. The replacement of urine studies by the SFLC assay for all myeloma patients remains controversial, since an Eastern Cooperative Oncology Group study on 399 MM patients (of whom only a minority had light-chain MM disease) found only a weak correlation between results of the SFLC assay and 24 h protein analysis.14
In line with the IMWG guidelines,15 we recommend the SFLC assay for the diagnosis and monitoring of patients with oligosecretory disease (Grade 2B). However, for patients with measurable urinary M-proteins, MM should be monitored by 24 h urine collections. When albumin is the dominant protein found in the urine, a glomerulopathy (such as AL-amyloidosis or light-chain deposition disease) should be excluded. The 24 h urine collection remains important when results are discordant.
Bone marrow studies
A BM aspirate enables quantification of infiltrating PC and cytogenetic studies on purified PC. Unfortunately, dilution by peripheral blood during aspiration or the presence of patchy disease (uneven distribution of MM cells throughout the BM) may result in an underestimation of tumor infiltration.16 We therefore recommend an additional BM trephine biopsy, which may generate complementary information (Grade 1B). A BM biopsy correctly identified MM disease in 95% of symptomatic patients with a low PC count on the initial BM smears.16 The correct quantification of BM PC is also important because of the 60% cut-off as a biomarker of malignancy. The IMWG earlier recommended retaining the highest PC infiltration in case of discrepancy. Finally, the monoclonality of PC in the diagnostic sample should be confirmed by multiparameter flow cytometry or by immunohistochemistry confirming light-chain restriction.
Flow cytometry of bone marrow cells
In cases of monoclonal gammopathies, the most relevant information provided by multiparameter flow cytometry is the identification and enumeration of neoplastic versus polyclonal BM PC. Regardless of the disease category, these neoplastic PC share similar immunophenotypic features, which are distinct from those of normal PC. Typically, CD38, CD138 and CD45 (together with light scatter characteristics) are the best backbone markers for the discrimination of PC. In addition, expression of CD19, CD56, CD117, CD20, CD28, CD27 and CD81, together with cytoplasmic immunoglobulin light-chain restriction, allows a clear discrimination between normal/reactive versus monoclonal PC17 and was used by the EuroFlow consortium to create a standardized panel allowing the quantification and immunophenotypic characterization of neoplastic PC.18
Due to dilution and the sometimes patchy disease distribution, multiparameter flow cytometry often underestimates the infiltration but remains important for detection of monoclonal PC in the peripheral blood and for the detection of minimal residual disease (MRD) in the BM. The Mayo Clinic group reported on the prognostic importance of circulating neoplastic cells in patients with newly diagnosed or relapsing MM.19,20 They recently monitored circulating MM cells at diagnosis and after induction therapy by multiparameter flow cytometry and confirmed inferior progression-free and overall survival for patients with persistent circulating MM cells before transplantation.21
Molecular studies
Cytogenetics
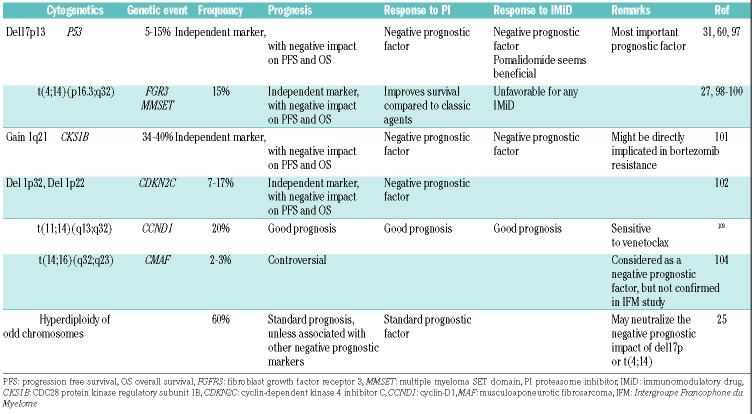
MM remains a heterogeneous disease with some patients progressing rapidly, while others survive more than 10 years. This clinical diversity is mainly driven by genetic abnormalities affecting the biological characteristics of MM cells.22 These alterations, summarized in Table 1, are important prognostic factors and can be divided into primary, disease-initiating abnormalities (hyperdiploidy and translocations involving the IGH locus) and secondary events, related to further progression of the disease.23 Fluorescence in situ hybridization on interphase cells, performed after purification of CD138+ cells or after counterstaining for the monoclonal light chains, is the technique required to detect these abnormalities.24 Alternative techniques that can be used are single-nucleotide polymorphism arrays, which are able to detect loss of heterozygosity and numerical chromosome abnormalities, and comparative genomic hybridization arrays, which mainly reveal numerical abnormalities.
Table 1.
Recommended cytogenetic studies with implicated gene alterations and related prognosis.
Up to 65% of patients with MM have translocations that involve the immunoglobulin heavy chain gene (IGH) on chromosome 14q32. The prevalence and prognostic impact of these IGH translocations vary according to the partner chromosome (Table 1). Hyperdiploidy generally consists of numerical gains (of the odd chromosomes) with a few structural changes, and is usually associated with longer overall survival. Not all trisomies have the same prognostic impact: trisomy 21 impairs, while trisomies 3 and 5 improve overall survival and may partially abrogate the negative impact of del17p and t(4;14).25
The most recurrent secondary alterations are deletion/monosomy of chromosome 13, deletion of chromosome 17p13, chromosome 1 abnormalities (1p deletions and 1q gains/amplifications), and C-MYC translocations. Deletion 17p13 is considered the most detrimental prognostic factor (due to short remission after high-dose therapy and an increased incidence of extramedullary disease) and is present in 8–10% of untreated patients.26 This deletion becomes clinically relevant when identified in the majority of PC. Different percentages (varying from 10%–60%) have been proposed to define a threshold that is associated with an impaired prognosis.27–29 The presence of a biallelic inactivation (i.e. by an additional mutation) of TP53 may particularly shorten overall survival.30 Aberrations of chromosome 1 (either 1q21 gains/amplifications or deletions of 1p32) are common and associated with shorter progression-free and overall survival, particularly the less frequent del(1p32).31 Patients with adverse cytogenetics may have additional aberrations: in the British MRC IX trial patients with two adverse cytogenetic lesions had a median overall survival of 2 years, while the survival of patients with three aberrations (an adverse IGH translocation, +1q21 and del17p13) was only 9 months.32 This inferior survival of patients with additional genetic abnormalities was also found in an Intergroupe Francophone du Myelome study that focused on patients with either del17p13 or t(4;14): for patients harboring t(4;14), multivariate analyses showed a shorter overall survival for patients with a combined del(13q14) or del(1p32). Among patients with del17p13, overall survival was shorter in those with del(1p32).33
Next-generation genome sequencing
Next-generation sequencing allows the detection of baseline clonal heterogeneity,34 clonal tiding35 and linear and branching evolution and contributes to a better understanding of MM disease biology.36 The availability of more than 2000 sequenced MM genomes has essentially defined the genomic landscape. These data revealed a high incidence of clinically relevant genomic aberrations, including oncogenic RAS mutations, but also a number of rarer and potentially actionable lesions, such as BRAF mutations.37,38 Of note, the vast majority of available genomic data in MM is still derived from samples obtained at diagnosis and does not, therefore, necessarily reflect the situation during disease progression. In addition, the clinical relevance of most mutations has not yet been determined and is undergoing investigation in large sequencing programs (CoMMpass, The Myeloma Genome Project and others).39,40 No mutation screening has yet been implemented in standard clinical workflows, but mutational analyses may help to identify potential therapeutic targets (such as BRAF mutations) and to stratify of patients in clinical trials.
Gene expression profiling
Based on microarrays to study mRNA expression, gene expression profiling gives a global snapshot of disease biology and may help clinicians to classify patients into separate groups with distinct outcomes. The University of Arkansas pioneered this technique to stratify MM patients and to characterize individuals’ disease at the molecular level.41 They identified gene expression profiling patterns that allowed MM patients to be grouped in seven disease classes. Further correlation of their microarray results with survival data of individual patients identified a list of 70 genes (GEP70) that had strong prognostic information.41 Similarly, the HOVON group identified a 92-gene signature (termed SKY92), based on the gene expression profiling results of the Hovon-65 trial.42,43 Other gene expression profiling-based risk models have been developed, such as the IFM-15 and MRC-IX-6 gene signatures44,45 Although not routinely determined in the majority of laboratories within or outside Europe, both the GEP70 and the SKY92 profiles are commercially available.
Imaging
Traditionally, osteolytic bone disease was investigated by conventional skeletal radiography. The 2014 IMWG disease criteria also considered small osteolytic lesions (≥5 mm), detected by computed tomography (CT) or combined 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET/CT) as symptoms of myeloma-induced bone disease.3 Taking into account these definitions, in 2015 the EMN proposed a relevant algorithm for guiding the choice of imaging technique.46,47 Different European centers have integrated CT into their diagnostic work-up based on its superior sensitivity and its ease of operation This choice was supported by the recent implementation as a national standard of care in the diagnostic workup of patients with suspected MM in the UK and elsewhere.48 Whole-body CT has also been integrated into the diagnostic work-up of the European Society of Medical Oncology49 and the upcoming IMWG guidelines.
The risk of pathological fractures or neurological complications should be assessed in patients with lytic lesions. In this regard, MRI is the preferred examination to detect spinal cord compression. If whole-body CT is not available, conventional radiographs can still be used but must be interpreted with their limited sensitivity in mind. In asymptomatic patients without lytic lesions, axial MRI or whole-body MRI should be considered to assess the presence of focal lesions (Grade 1B). Addition of dynamic contrast enhancement or diffusion weighted imaging to a whole-body MRI protocol provides additional information on BM vascularization, cellularity, and composition and improves the sensitivity of MRI.50,51 Two or more focal lesions on MRI are considered as a MM-defining biomarker.52 18F-FDG PET/CT can replace whole-body CT, if image acquisition of CT allows a detailed evaluation of the bone structures from vertex to knees, including both arms (Grade 1B).53 18F-FDG PET/CT is important to assess the presence of extramedullary disease, known to be an independent prognostic factor.54 The integration of MRI, PET-CT and whole-body CT always requires experience, interdisciplinary consensus and reflection and needs to be correlated with blood, urine and BM results. Finally, baseline 18F-FDG PET/CT scans enable post-treatment follow-up of hypermetabolic regions with a greater sensitivity than MRI.54,55 PET/CT is also useful in confirming MRD.56
European Myeloma Network recommendations for the diagnosis of multiple myeloma:
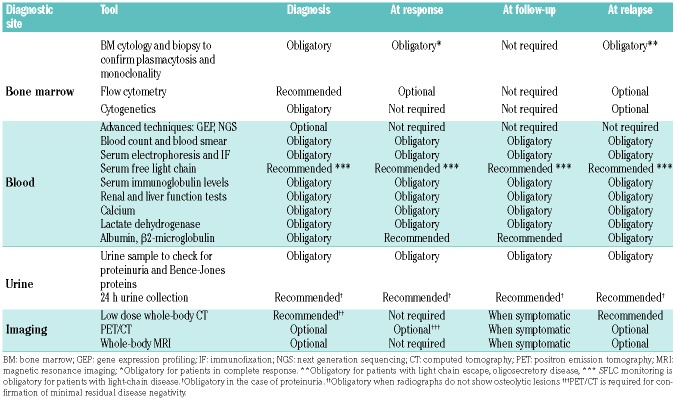
The initial work-up should include: complete blood count, kidney function tests, serum protein electrophoresis with immunofixation, serum albumin, β2-microglobulin, lactate dehydrogenase, C-reactive protein, calcium, serum free light chains (especially useful in the case of light-chain multiple myeloma), 24 h protein collection with protein quantification, electrophoresis and urine immunofixation, and bone marrow (aspiration only is acceptable) studies to quantify and characterize abnormal plasmacytosis (Table 2). The intervals between follow-up studies depend on the response obtained and the patients’ characteristics, as proposed in Table 3 (Grade 2C). After CD138+ plasma cell sorting, fluorescence in situ hybridization analysis should include at least t(4;14) and del17p; analysis of t(14;16), 1q21 gain and del(1p32) are also recommended. In addition, bone integrity needs to be evaluated with whole-body computed tomography and/or whole-body magnetic resonance imaging (at least axial). Quantification of the level of plasma cell infiltration, serum free light chains and magnetic resonance imaging assessment are required to assess the SLIM-CRAB biomarkers that define early active multiple myeloma. At relapse, the extent of myeloma-induced bone disease should be re-evaluated, especially if the relapse occurs late after the initial diagnosis.
Table 2.
Recommendations on further examinations at diagnosis, for response assessment, during follow-up and at relapse.
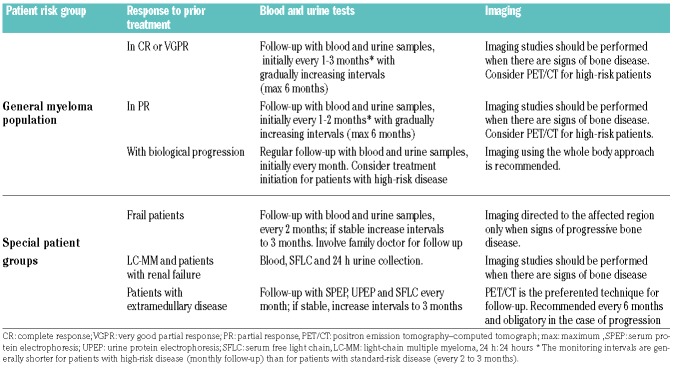
Table 3.
Follow-up of multiple myeloma patients according to response and patients’ characteristics (general strength of these recommendation GRADE 2C).
Staging and prognosis
Disease-specific prognostic scores
The variable outcome of MM patients depends on differences in disease biology, global disease burden and the health status of the patient. Researchers have developed clinical scoring systems in order to estimate individual prognosis. The degree of anemia, renal failure and osteolysis were the first disease-related prognostic biomarkers described in MM and were all included in the Salmon & Durie staging system. Subsequently, β2-microglobulin, albumin and C-reactive protein levels, and proliferative activity of MM cells were found to be additional prognostic factors, and albumin and β2-microglobulin levels were incorporated in the International Staging System (ISS) in 2005. Other biomarkers have been identified and include markers of tumor cell proliferation, cytokines, pro-angiogenic factors, indicators of bone remodeling, circulating (exosomal) miRNA and imaging abnormalities. Another promising biomarker is the serum level of shed B-cell maturation antigen, which correlates well with BM PC infiltration and declines according to tumor response.57 Follow-up of serum B-cell maturation antigen levels seems of interest in patients with non-secretory disease, for whom we lack reliable parameters in the blood; future studies are therefore warranted.
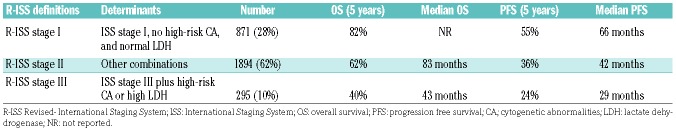
Apart from the often still reported Salmon & Durie staging system, the ISS and revised (R)-ISS are frequently used as staging systems; in the latter systems, the β2-microglobulin and albumin levels reflect patients’ tumor burden, turnover rate, presence of renal impairment, and nutritional and performance status.58 In order to improve the prognostic performance of the ISS score, the IMWG updated it, adding high-risk cytogenetics [t(4;14), t(14;16), and del17p determined by interphase fluorescence in situ hybridization] and elevated serum lactate dehydrogenase (Table 4).59 These factors had been previously identified as relevant risk factors for early progression after autologous transplantation.60 Of note, the ISS and R-ISS give prognostic information at diagnosis, but have not been validated in relapsed/refractory MM.
Table 4.
The Revised-International Staging System is one of the best stratification methods; it is based on routinely available cytogenetic and biochemistry tests (Palumbo et al.).56
Frailty and co-morbidities
Once a treatment has started, adherence to the established protocol remains a major clinical concern in elderly and frail patients. This requires an individualized approach in which therapeutic decisions should be driven by both disease features and the patient’s characteristics. As in other malignancies, comprehensive geriatric assessments have been evaluated to assess patients’ functional, cognitive and mental status, comorbidities, nutrition and presence of geriatric symptoms. Palumbo and co-workers developed a retrospective simplified geriatric assessment, named the IMWG-Frailty Index, in which age, the Charlson Comorbidity Index, activities of daily living and instrumental activities of daily living were used to discriminate between fit, intermediate-fit and frail patients, showing different incidences of severe adverse events, progression-free survival and overall survival.61 Expectedly, more severe adverse events and treatment discontinuations were reported in frail patients. The most extensive retrospective and prospective tests and validation analyses were performed within the German study group, who prospectively assessed the IMWG-Frailty Index with the revised Myeloma Comorbidity Index (R-MCI) and other comorbidity indices.62 A second prospective German study including 801 MM patients determined that impaired renal and pulmonary function, poorer Karnofsky performance status, frailty and age were independent, multivariate risk factors for overall survival. Addition of cytogentic abnormalities resulted in the weighted revised Myeloma Comorbidity Index, which is able to assess patients’ physical condition accurately and is simple to apply in the clinic.63 Although not yet proven via randomized treatment algorithms, there is circumstantial evidence that limited induction therapy, careful dose modifications and reductions, sensible use of supportive care and watchful surveillance of unfit and frail patients may improve patients’ outcome further.64 The EMN insists on developing trials, specifically designed for frail patients, for further refinement of frailty-related diagnostics and best treatment selection.65
Drug-related biomarkers
While prognostic factors regarding disease evaluation are listed above, drug-related biomarkers are being assessed to predict response to treatment and, possibly, to facilitate optimal treatment while avoiding ineffective therapies and unnecessary toxicity. Recent pharmacogenomic studies revealed gene signatures that could predict the clinical outcome after treatments based on immunomodulatory drugs66 or bortezomib.67 The expression of cereblon, an intracellular binding partner of immunomodulatory drugs has been intensively studied as a biomarker and initial studies correlated cereblon levels with the outcome of MM patients receiving treatment with such drugs.68–71 These studies used quantitative real time PCR analysis, gene expression profiling or immunohistochemistry to quantify cereblon expression and showed that loss of cereblon expression was associated with resistance to immunomodulatory drugs. Further investigations revealed limitations of these assays, because both splice variants of cereblon and point mutations were described.72,73 When exploring predictors for tumor responses to daratumumab, higher CD38 expression was found on MM cells of responsive patients. However, good responses were also seen in patients with lower CD38 expression, an observation confirmed in a second study that showed that CD38 expression level was not necessarily predictive of response in advanced MM; nevertheless attempts to assess agents that keep CD38 upregulation increased, e.g., all-trans retinoic acid and histone deacetylase inhibitors, are being pursued pre-clinically and clinically.74,75
Finally, expression of anti-apoptotic proteins, BCL-2, BCL-XL or MCL-1, measured by quantitative real-time PCR, predict pharmacological responses to the bcl-2 inhibitor venetoclax, which is mostly active in patients harboring t(11,14) translocations.76
European Myeloma Network recommendations:
The International Staging System score and, whenever possible, the Revised International Staging System score, should be determined at diagnosis to assess prognosis. At least a minimal frailty assessment should be performed to aid the choice of induction therapy, dose amendments and supportive care. Although of interest due to their prognostic and predictive value, biomarkers, such as cereblon and CD38 protein expression, are not routinely assessed in daily multiple myeloma care, while fluorescence in situ hybridization for t(11;14) should be performed if treatment with venetoclax is a clinical option.
Response assessment
The implication of the results of an SFLC assay and MRD assessment prompted the IMWG to update MM response criteria.77 In 2011, two new categories, stringent complete response and very good partial response, were added. Correct disease assessment is not only crucial for reporting in clinical trials, it also indicates prognosis in individual cases.77,78 It is well known that patients who obtain a complete response following induction have improved progression-free and overall survival after intensive treatment.79
Patients should, therefore, be evaluated before initiation of each treatment cycle to determine their response to therapy. For MM patients with intact immunoglobulins, the recommended method for monitoring is quantification of serum and urinary M-protein. Whether all serum (and urine) parameters have to be checked after each cycle, rather than after every two or three cycles is left to the discretion of each physician, taking into account disease aggressiveness, organ (i.e. renal) impairment and various other factors. To confirm a stringent complete response, normalization of the SFLC values and disappearance of monoclonal PC infiltration in the BM should be added to negative immunofixation on serum and urine samples. The BM must be evaluated in order to confirm a complete response, but this can be done at some time after the end of treatment, allowing full recovery of the BM. Of note, BM infiltration can be heterogeneous with persisting focal lesions in an otherwise recovered BM (earlier referred to as patchy disease). The follow-up of patients with light-chain MM and measurable M-protein levels in urine should include 24 h urine collections. The SFLC assay generally allows response assessment in patients with oligosecretory disease with unmeasurable serum and urine M-protein levels [serum M-protein <1 g/dL (10 g/L) or urine M-protein <200 mg/24 h]. If the SFLC assay is not informative, BM plasmacytosis should be assessed.77
The definition of relapse applies to a patient in complete response who experiences reappearance of MM, while progression refers to patients with an increasing disease burden from a baseline or persistent residual disease. An additional assessment for confirmation is mandatory before initiating a new line of therapy. MM progression can be determined biochemically (increase in an existing monoclonal peak), or by radiological and clinical criteria. The interested reader can find the criteria for relapse and disease progression recently described by the IMWG.77 Response assessment can be challenging, especially in cases of deep response after the use of monoclonal antibodies, which may interfere with quantification of the M-protein and may require specific assays.80
Minimal residual disease
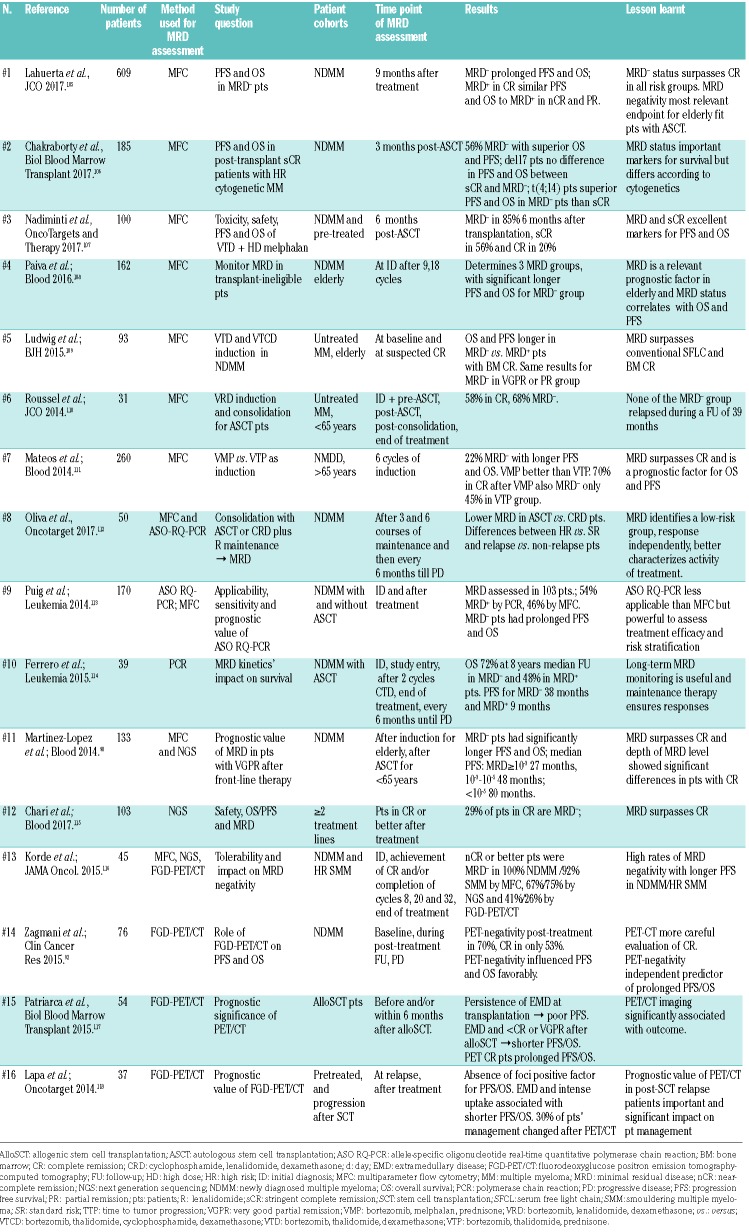
Current induction regimens, in association with autologous stem cell transplantation, achieve very high response rates and the responses are often deep. Unfortunately, however, MM often recurs due to residual MM cells, drug resistance and/or persistence of resistant dormant subclones.81 MRD can be assessed by multipara-meter flow cytometry, polymerase chain reaction (PCR)-based methods or next-generation sequencing to identify persistent clonal cells. Recent studies, listed in Table 5, confirmed the prognostic impact of MRD status as an independent variable for outcome.82 In the future, MRD will be more widely used in clinical trials to guide treatment choices and probably as a surrogate marker for progression-free and overall survival.56
Table 5.
Recent studies on minimal residual disease and the implications for progression-free and overall survival of patients with multiple myeloma.
Conventional flow-MRD approaches, based on multiple institutional non-standardized protocols, can reliably identify malignant PC and discriminate aberrantly expressed cell surface markers in approximately 90% of patients (with a sensitivity of detecting 10−4 atypical PC in normal BM). Recent studies conducted by Spanish and UK groups have shown that negative MRD by multiparameter flow cytometry is predictive for both progression-free survival and overall survival, even in patients who achieved a complete response.83,84 Recent technical advances have increased the sensitivity of next-generation flow cytometry protocols down to the 10−6 range.85
MRD analysis by PCR detects persistent residual tumor cells through the amplification of a tumor-specific molecular marker. The IGH rearrangement is used as a marker of clonality in various B-cell malignancies.86 Allele-specific oligonucleotide PCR with primers complementary to the heavy chain variable sequence remains one of the most sensitive approaches to detect residual malignant PC, reaching a sensitivity of 10−5.87 Unfortunately, it is a laborious, time-consuming approach that is not widely available because of its dependence on patient-specific primers and probes for quantitative PCR.
Next-generation sequencing of the IGH rearrangement segments provides insights into the architecture of the B-lineage repertoire with consensus primers. Since the B-lineage repertoire includes the malignant PC clone in BM, next-generation sequencing of IGH enables a quantitative determination of MRD, without per-patient customization, provided that the malignant clone was identified in a diagnostic sample or a sample taken during active disease.88 Results from next-generation sequencing are highly concordant with flow-based MRD detection, highly reproducible and reach a sensitivity of 10−6.89–91 A lack of standardization and limited commercial availability are the main restraints for next-generation sequencing. Flow cytometry and molecular techniques both require an appropriate BM sample. Heterogeneous BM infiltration and peripheral blood dilution can be major hurdles to the evaluation of MRD. Since neither of these techniques is able to detect extramedullary disease, they should be combined with imaging studies.
Imaging is a third approach to evaluate MRD in MM. Both PET/CT and MRI have been evaluated in this setting.53,55 Regarding PET/CT, two large studies assessed the prognostic value of negative PET/CT after induction and autologous stem cell transplantation.55,92 Both studies found that PET/CT-negative patients had a better progression-free and overall survival compared to PET/CT-positive patients (52 versus 38 months and 5-year estimates of 90% versus 71%, respectively).92 In the French IMAJEM study, MRD was evaluated in 86 patients via PET-CT and flow cytometry. Although the concordance between the two tests was low, progression-free survival was better in patients who were negative according to both techniques compared to those who were positive by PET and/or flow cytometry (3-year progression-free survival, 86.8% versus 52.9%), indicating that both techniques are complementary. A major advantage of PET/CT is its capacity to assess MRD outside the BM; its disadvantages are high cost and the lack of reimbursement in certain countries, insufficient standardization and reduced tracer uptake in some MM patients. Evaluation via PET/CT has been incorporated into the new IMWG MRD criteria.77 In the future, the increased capabilities of diffusion weighted MRI to detect small lesions and diffuse infiltration may offer advantages that merit prospective evaluation in MRD assessment studies.50
In addition, recent studies have demonstrated that circulating DNA fragments carrying tumor-specific sequence alterations can be detected and quantified in the blood of patients with solid tumors.93,94 In MM, various studies have provided evidence that - much like in solid tumors - MM-specific alterations (VDJ rearrangements or somatic genomic alterations) can also be identified and tracked in cell-free DNA circulating in blood.95,96
European Myeloma Network recommendations:
Response assessment is an essential part of myeloma management. Patients under treatment should be evaluated before the initiation of each cycle and according to international guidelines. Minimal residual disease testing is not currently recommended in routine follow-up of patients but is likely to be incorporated in standard response/progression evaluation soon. Valid options for the assessment of minimal residual disease are based on bone marrow cells (next-generation flow cytometry) or molecular analysis (next- generation sequencing), often also combined with an imaging-based evaluation. These methods require appropriate expertise.
Conclusion
While novel agents have certainly improved the outcomes of patients with myeloma, prompt diagnosis and close follow-up of MM patients remain highly relevant and contribute to better survival. In most cases, the diagnosis of MM is straightforward, being based on biological and radiological evidence when evocative clinical signs are present. During response assessment, the evaluation of MRD will become increasingly important and, within the next few years, will guide treatment choices in clinical trials and possibly also outside trial scenarios. International efforts are needed to standardize the different techniques that can be used to evaluate MRD. Guidelines on appropriate follow-up and patient-tailored monitoring have been updated in this EMN consensus paper and should help to improve the outcome and prognosis of our patients.
Supplementary Material
Acknowledgments
The authors thank distinguished IMWG, EMN, DSMM and GMMG experts for their advice and recommendations that have helped us to improve this paper. This work was supported by the Deutsche Krebshilfe (grants 1095969 and 111424 to ME), the Foundation against Cancer, the Fonds National de la Recherche Scientifique and the Fonds d’Investissement de Recherche Scientifique (FIRS) du CHU de Liège (grants to JC), the NIHR Imperial Biomedical Research Centre and the Cancer Research UK Imperial Centre (grants to HWA).
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/103/11/1772
References
- 1.Kumar SK, Rajkumar V, Kyle RA, et al. Multiple myeloma. Nat Rev Dis Primers. 2017;3:17046. [DOI] [PubMed] [Google Scholar]
- 2.Kumar SK, Dispenzieri A, Lacy MQ, et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 2014;28(5):1122–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–548. [DOI] [PubMed] [Google Scholar]
- 4.Caers J, Fernández de Larrea C, Leleu X, et al. The changing landscape of smoldering multiple myeloma: a European perspective. Oncologist. 2016;21(3):333–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. [DOI] [PubMed] [Google Scholar]
- 6.Kuhnemund A, Liebisch P, Bauchmuller K, et al. ‘Light-chain escape-multiple myeloma’-an escape phenomenon from plateau phase: report of the largest patient series using LC-monitoring. J Cancer Res Clin Oncol. 2009;135(3):477–484. [DOI] [PubMed] [Google Scholar]
- 7.Jenner E. Serum free light chains in clinical laboratory diagnostics. Clin Chim Acta. 2014;427:15–20. [DOI] [PubMed] [Google Scholar]
- 8.Bradwell AR, Harding SJ, Fourrier NJ, et al. Assessment of monoclonal gammopathies by nephelometric measurement of individual immunoglobulin κ/λratios. Clin Chem. 2009;55(9):1646–1655. [DOI] [PubMed] [Google Scholar]
- 9.Ludwig H, Milosavljevic D, Berlanga O, et al. Suppression of the noninvolved pair of the myeloma isotype correlates with poor survival in newly diagnosed and relapsed/refractory patients with myeloma. Am J Hematol. 2016;91(3):295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greil C, Ihorst G, Gaiser F, et al. The serum heavy/light chain immunoassay: a valuable tool for sensitive paraprotein assessment, risk, and disease monitoring in monoclonal gammopathies. Eur J Haematol. 2017;99(5):449–458. [DOI] [PubMed] [Google Scholar]
- 11.Katzmann JA, Kyle RA, Benson J, et al. Screening panels for detection of monoclonal gammopathies. Clin Chem. 2009;55(8): 1517–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dejoie T, Corre J, Caillon H, et al. Serum free light chains, not urine specimens, should be used to evaluate response in light-chain multiple myeloma. Blood. 2016;128(25):2941–2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heaney JLJ, Campbell JP, Griffin AE, et al. Diagnosis and monitoring for light chain only and oligosecretory myeloma using serum free light chain tests. Br J Haematol. 2017;178(2):220–230. [DOI] [PubMed] [Google Scholar]
- 14.Dispenzieri A, Zhang L, Katzmann JA, et al. Appraisal of immunoglobulin free light chain as a marker of response. Blood. 2008;111(10):4908–4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dispenzieri A, Kyle R, Merlini G, et al. International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia. 2008;23(2):215–224. [DOI] [PubMed] [Google Scholar]
- 16.Lee N, Moon SY, Lee JH, et al. Discrepancies between the percentage of plasma cells in bone marrow aspiration and BM biopsy: impact on the revised IMWG diagnostic criteria of multiple myeloma. Blood Cancer J. 2017;7:e530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rawstron AC, Orfao A, Beksac M, et al. Report of the European Myeloma Network on multiparametric flow cytometry in mul tiple myeloma and related disorders. Haematologica. 2008;93(3):431–438. [DOI] [PubMed] [Google Scholar]
- 18.van Dongen JJM, Lhermitte L, Bottcher S, et al. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenotyping of normal, reactive and malignant leukocytes. Leukemia. 2012;26(9):1908–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gonsalves WI, Rajkumar SV, Gupta V, et al. Quantification of clonal circulating plasma cells in newly diagnosed multiple myeloma: implications for redefining high-risk myeloma. Leukemia. 2014;28(10):2060–2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonsalves WI, Morice WG, Rajkumar V, et al. Quantification of clonal circulating plasma cells in relapsed multiple myeloma. Br J Haematol. 2014;167(4):500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakraborty R, Muchtar E, Kumar SK, et al. Serial measurements of circulating plasma cells before and after induction therapy has an independent prognostic impact in patients with multiple myeloma undergoing upfront autologous transplantation. Haematologica. 2017;102(8):1439–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robiou du Pont S, Cleynen A, Fontan C, et al. Genomics of multiple myeloma. J Clin Oncol. 2017;35(9):963–967. [DOI] [PubMed] [Google Scholar]
- 23.Kuehl WM, Bergsagel PL. Molecular pathogenesis of multiple myeloma and its premalignant precursor. J Clin Invest. 2012;122(10):3456–3463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross FM, Avet-Loiseau H, Ameye G, et al. Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders. Haematologica. 2012;97(8):1272–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chretien M-L, Corre J, Lauwers-Cances V, et al. Understanding the role of hyperdiploidy in myeloma prognosis: which trisomies really matter? Blood. 2015;126(25):2713–2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Billecke L, Murga Penas EM, May AM, et al. Cytogenetics of extramedullary manifestations in multiple myeloma. Br J Haematol. 2013;161(1):87–94. [DOI] [PubMed] [Google Scholar]
- 27.Avet-Loiseau H, Leleu X, Roussel M, et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol. 2010;28(30):4630–4634. [DOI] [PubMed] [Google Scholar]
- 28.Neben K, Lokhorst HM, Jauch A, et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 2012;119(4):940–948. [DOI] [PubMed] [Google Scholar]
- 29.Merz M, Hielscher T, Seckinger A, et al. Baseline characteristics, chromosomal alterations, and treatment affecting prognosis of deletion 17p in newly diagnosed myeloma. Am J Hematol. 2016;91(11):E473–E477. [DOI] [PubMed] [Google Scholar]
- 30.Thanendrarajan S, Tian E, Qu P, et al. The level of deletion 17p and bi-allelic inactivation of TP53 has a significant impact on clinical outcome in multiple myeloma. Haematologica. 2017;102(9):e364–e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avet-Loiseau H, Attal M, Campion L, et al. Long-term analysis of the IFM 99 trials for myeloma: cytogenetic abnormalities [t(4;14), del(17p), 1q gains] play a major role in defining long-term survival. J Clin Oncol. 2012;30(16):1949–1952. [DOI] [PubMed] [Google Scholar]
- 32.Boyd KD, Ross FM, Chiecchio L, et al. A novel prognostic model in myeloma based on co-segregating adverse FISH lesions and the ISS: analysis of patients treated in the MRC Myeloma IX trial. Leukemia. 2012;26(2):349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hebraud B, Magrangeas F, Cleynen A, et al. Role of additional chromosomal changes in the prognostic value of t(4;14) and del(17p) in multiple myeloma: the IFM experience. Blood. 2015;125(13):2095–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keats JJ, Chesi M, Egan JB, et al. Clonal competition with alternating dominance in multiple myeloma. Blood. 2012;120(5):1067–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Egan JB, Shi C-X, Tembe W, et al. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood. 2012;120(5):1060–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melchor L, Brioli A, Wardell CP, et al. Single-cell genetic analysis reveals the composition of initiating clones and phylogenetic patterns of branching and parallel evolution in myeloma. Leukemia. 2014;28(8):1705–1715. [DOI] [PubMed] [Google Scholar]
- 37.Lohr Jens G, Stojanov P, Carter Scott L, et al. Widespread genetic heterogeneity in multiple myeloma: implications for targeted therapy. Cancer Cell. 25(1):91–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bolli N, Avet-Loiseau H, Wedge DC, et al. Heterogeneity of genomic evolution and mutational profiles in multiple myeloma. Nat Commun. 2014;5:2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bolli N, Li Y, Sathiaseelan V, et al. A DNA target-enrichment approach to detect mutations, copy number changes and immunoglobulin translocations in multiple myeloma. Blood Canc J. 2016;6:e467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson DC, Weinhold N, Mitchell JS, et al. Genome-wide association study identifies variation at 6q25.1 associated with survival in multiple myeloma. Nat Commun. 2016;7:10290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaughnessy JD, Zhan F, Burington BE, et al. A validated gene expression model of high-risk multiple myeloma is defined by deregulated expression of genes mapping to chromosome 1. Blood. 2007;109(6):2276–2284. [DOI] [PubMed] [Google Scholar]
- 42.Kuiper R, Broyl A, de Knegt Y, et al. A gene expression signature for high-risk multiple myeloma. Leukemia. 2012;26(11):2406–2413. [DOI] [PubMed] [Google Scholar]
- 43.Kuiper R, van Duin M, van Vliet MH, et al. Prediction of high- and low-risk multiple myeloma based on gene expression and the International Staging System. Blood. 2015;126(17):1996–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Decaux O, Lodé L, Magrangeas F, et al. Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiploid signatures in low-risk patients: a study of the Intergroupe Francophone du Myélome. J Clin Oncol. 2008;26(29):4798–4805. [DOI] [PubMed] [Google Scholar]
- 45.Dickens NJ, Walker BA, Leone PE, et al. Homozygous deletion mapping in myeloma samples identifies genes and an expression signature relevant to pathogenesis and outcome. Clin Cancer Res. 2010;16(6):1856–1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Terpos E, Kleber M, Engelhardt M, et al. European Myeloma Network guidelines for the management of multiple myeloma-related complications. Haematologica. 2015;100(10):1254–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hillengass J, Moulopoulos LA, Delorme S, et al. Whole-body computed tomography versus conventional skeletal survey in patients with multiple myeloma: a study of the International Myeloma Working Group. Blood Canc J. 2017;7:e599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Excellence NIfHaC. Myeloma: diagnosis and management 2016 [cited; Available from: https://www.nice.org.uk/guidance/ng35/resources/myeloma-diagnosis-and-management-pdf-1837394042821
- 49.Moreau P, San Miguel J, Sonneveld P, et al. Multiple myeloma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv52–iv61. [DOI] [PubMed] [Google Scholar]
- 50.Messiou C, Kaiser M. Whole body diffusion weighted MRI – a new view of myeloma. Br J Haematol. 2015;171(1):29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hillengass J, Bauerle T, Bartl R, et al. Diffusion-weighted imaging for non-invasive and quantitative monitoring of bone marrow infiltration in patients with monoclonal plasma cell disease: a comparative study with histology. Br J Haematol. 2011;153(6):721–728. [DOI] [PubMed] [Google Scholar]
- 52.Hillengass J, Fechtner K, Weber M-A, et al. Prognostic significance of focal lesions in whole-body magnetic resonance imaging in patients with asymptomatic multiple myeloma. J Clin Oncol. 2010;28(9):1606–1610. [DOI] [PubMed] [Google Scholar]
- 53.Cavo M, Terpos E, Nanni C, et al. Role of 18F-FDG PET/CT in the diagnosis and management of multiple myeloma and other plasma cell disorders: a consensus statement by the International Myeloma Working Group. Lancet Oncol. 2017;18(4):e206–e217. [DOI] [PubMed] [Google Scholar]
- 54.Zamagni E, Patriarca F, Nanni C, et al. Prognostic relevance of 18-F FDG PET/CT in newly diagnosed multiple myeloma patients treated with up-front autologous transplantation. Blood. 2011;118(23):5989–5995. [DOI] [PubMed] [Google Scholar]
- 55.Moreau P, Attal M, Caillot D, et al. Prospective evaluation of magnetic resonance imaging and [18F]fluorodeoxyglucose positron emission tomography-computed tomography at diagnosis and before maintenance therapy in symptomatic patients with multiple myeloma included in the IFM/DFCI 2009 trial: results of the IMAJEM Study. J Clin Oncol. 2017;35(25):2911–2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anderson KC, Auclair D, Kelloff GJ, et al. The role of minimal residual disease testing in myeloma treatment selection and drug development: current value and future applications. Clin Cancer Res. 2017;23(15):3980–3993. [DOI] [PubMed] [Google Scholar]
- 57.Sanchez E, Li M, Kitto A, et al. Serum B-cell maturation antigen is elevated in multiple myeloma and correlates with disease status and survival. Br J Haematol. 2012;158(6):727–738. [DOI] [PubMed] [Google Scholar]
- 58.Greipp PR, San Miguel J, Durie BG, et al. International Staging System for multiple myeloma. J Clin Oncol. 2005;23(15):3412–3420. [DOI] [PubMed] [Google Scholar]
- 59.Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863–2869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moreau P, Cavo M, Sonneveld P, et al. Combination of International Scoring System 3, high lactate dehydrogenase, and t(4;14) and/or del(17p) identifies patients with multiple myeloma (MM) treated with front-line autologous stem-cell transplantation at high risk of early MM progression– related death. J Clin Oncol. 2014;32(20): 2173–2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Palumbo A, Bringhen S, Mateos MV, et al. Geriatric assessment predicts survival and toxicities in elderly myeloma patients: an International Myeloma Working Group report. Blood. 2015;125(13):2068–2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Engelhardt M, Dold SM, Ihorst G, et al. Geriatric assessment in multiple myeloma patients: validation of the International Myeloma Working Group (IMWG) score and comparison with other common comorbidity scores. Haematologica. 2016;101(9): 1110–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Engelhardt M, Domm A-S, Dold SM, et al. A concise revised Myeloma Comorbidity Index as a valid prognostic instrument in a large cohort of 801 multiple myeloma patients. Haematologica. 2017;102(5):910–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mateos MV, Oriol A, Martinez-Lopez J, et al. Outcomes with two different schedules of bortezomib, melphalan, and prednisone (VMP) for previously untreated multiple myeloma: matched pair analysis using long-term follow-up data from the phase 3 VISTA and PETHEMA/GEM05 trials. Ann Hematol. 2016;95(12):2033–2041. [DOI] [PubMed] [Google Scholar]
- 65.Larocca A, Dold SM, Zweegman S, et al. Patient-centered practice in elderly myeloma patients: an overview and consensus from the European Myeloma Network (EMN). Leukemia. 2018. April 25 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 66.Bhutani M, Zhang Q, Friend R, et al. Investigation of a gene signature to predict response to immunomodulatory derivatives for patients with multiple myeloma: an exploratory, retrospective study using microarray datasets from prospective clinical trials. Lancet Haematol. 2017;4(9):e443–e451. [DOI] [PubMed] [Google Scholar]
- 67.Van Vliet MH, Kuiper R, Broijl A, Van Duin M, et al. Proteasome inhibitor treatment response can be predicted by gene expression profiling in multiple myeloma. Haematologica. 2014;99(S1):494. [Google Scholar]
- 68.Broyl A, Kuiper R, van Duin M, et al. High cereblon expression is associated with better survival in patients with newly diagnosed multiple myeloma treated with thalidomide maintenance. Blood. 2013;121(4):624–627. [DOI] [PubMed] [Google Scholar]
- 69.Heintel D, Rocci A, Ludwig H, et al. High expression of cereblon (CRBN) is associated with improved clinical response in patients with multiple myeloma treated with lenalidomide and dexamethasone. Br J Haematol. 2013;161(5):695–700. [DOI] [PubMed] [Google Scholar]
- 70.Schuster SR, Kortuem KM, Zhu YX, et al. The clinical significance of cereblon expression in multiple myeloma. Leuk Res. 2014;38(1):23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhu YX, Braggio E, Shi C-X, et al. Identification of cereblon-binding proteins and relationship with response and survival after IMiDs in multiple myeloma. Blood. 2014;124(4):536–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gandhi AK, Mendy D, Waldman M, et al. Measuring cereblon as a biomarker of response or resistance to lenalidomide and pomalidomide requires use of standardized reagents and understanding of gene complexity. Br J Haematol. 2014;164(2):233–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kortüm KM, Mai EK, Hanafiah NH, et al. Targeted sequencing of refractory myeloma reveals a high incidence of mutations in CRBN and Ras pathway genes. Blood. 2016;128(9):1226–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nijhof IS, Casneuf T, van Velzen J, et al. CD38 expression and complement inhibitors affect response and resistance to daratumumab therapy in myeloma. Blood. 2016;128(7):959–970. [DOI] [PubMed] [Google Scholar]
- 75.Pick M, Vainstein V, Goldschmidt N, et al. Daratumumab resistance is frequent in advanced-stage multiple myeloma patients irrespective of CD38 expression and is related to dismal prognosis. Eur J Haematol. 2018;100(5):494–501. [DOI] [PubMed] [Google Scholar]
- 76.Punnoose EA, Leverson JD, Peale F, et al. Expression profile of BCL-2, BCL-XL, and MCL-1 predicts pharmacological response to the BCL-2 selective antagonist venetoclax in multiple myeloma models. Mol Cancer Ther. 2016;15(5):1132–1144. [DOI] [PubMed] [Google Scholar]
- 77.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–e346. [DOI] [PubMed] [Google Scholar]
- 78.Durie BGM, Harousseau JL, Miguel JS, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006;20(9): 1467–1473. [DOI] [PubMed] [Google Scholar]
- 79.Lahuerta JJ, Mateos MV, Martínez-López J, et al. Influence of pre- and post-transplantation responses on outcome of patients with multiple myeloma: sequential improvement of response and achievement of complete response are associated with longer survival. J Clin Oncol. 2008;26(35):5775–5782. [DOI] [PubMed] [Google Scholar]
- 80.van de Donk Niels WCJ, Otten Henny G, El Haddad O, et al. Interference of daratumumab in monitoring multiple myeloma patients using serum immunofixation electrophoresis can be abrogated using the daratumumab IFE reflex assay (DIRA). Clin Chem Lab Med, 2016:1105. [DOI] [PubMed] [Google Scholar]
- 81.Paiva B, Corchete LA, Vidriales M-B, et al. Phenotypic and genomic analysis of multiple myeloma minimal residual disease tumor cells: a new model to understand chemoresistance. Blood. 2016;127(15):1896–1906. [DOI] [PubMed] [Google Scholar]
- 82.de Tute RM, Rawstron AC, Gregory WM, et al. Minimal residual disease following autologous stem cell transplant in myeloma: impact on outcome is independent of induction regimen. Haematologica. 2016;101(2): e69–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Paiva B, Martinez-Lopez J, Vidriales M-B, et al. Comparison of immunofixation, serum free light chain, and immunophenotyping for response evaluation and prognostication in multiple myeloma. J Clin Oncol. 2011;29(12):1627–1633. [DOI] [PubMed] [Google Scholar]
- 84.Rawstron AC, Child JA, de Tute RM, et al. Minimal residual disease assessed by multi-parameter flow cytometry in multiple myeloma: impact on outcome in the Medical Research Council Myeloma IX study. J Clin Oncol. 2013;31(20):2540–2547. [DOI] [PubMed] [Google Scholar]
- 85.Flores-Montero J, Sanoja-Flores L, Paiva B, et al. Next generation flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia. 2017;31:2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tonegawa S. Somatic generation of antibody diversity. Nature. 1983;302(5909):575–581. [DOI] [PubMed] [Google Scholar]
- 87.van der Velden VHJ, Cazzaniga G, Schrauder A, et al. Analysis of minimal residual disease by Ig//TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia. 2007;21(4):604–611. [DOI] [PubMed] [Google Scholar]
- 88.Logan AC, Gao H, Wang C, et al. High-throughput VDJ sequencing for quantification of minimal residual disease in chronic lymphocytic leukemia and immune reconstitution assessment. Proc Natl Acad Sci. 2011;108(52):21194–21199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martinez-Lopez J, Fernández-Redondo E, García-Sánz R, et al. Clinical applicability and prognostic significance of molecular response assessed by fluorescent-PCR of immunoglobulin genes in multiple myeloma. Results from a GEM/PETHEMA study. Br J Haematol. 2013;163(5):581–589. [DOI] [PubMed] [Google Scholar]
- 90.Martinez-Lopez J, Lahuerta JJ, Pepin F, et al. Prognostic value of deep sequencing method for minimal residual disease detection in multiple myeloma. Blood. 2014;123(20): 3073–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Avet-Loiseau H, Corre J, Lauwers-Cances V, et al. Evaluation of minimal residual disease (MRD) by next generation sequencing (NGS) is highly predictive of progression free survival in the IFM/DFCI 2009 Trial. Blood. 2015;126(23):191–191. [Google Scholar]
- 92.Zamagni E, Nanni C, Mancuso K, et al. PET/CT improves the definition of complete response and allows to detect otherwise unidentifiable skeletal progression in multiple myeloma. Clin Cancer Res. 2015;21(19):4384–4390. [DOI] [PubMed] [Google Scholar]
- 93.Dawson S-J, Tsui DWY, Murtaza M, et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med. 2013;368(13):1199–1209. [DOI] [PubMed] [Google Scholar]
- 94.Diehl F, Schmidt K, Choti MA, et al. Circulating mutant DNA to assess tumor dynamics. Nat Med. 2008;14(9):985–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Oberle A, Brandt A, Voigtlaender M, et al. Monitoring multiple myeloma by next-generation sequencing of V(D)J rearrangements from circulating myeloma cells and cell-free myeloma DNA. Haematologica. 2017;102(6):1105–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mithraprabhu S, Khong T, Ramachandran M, et al. Circulating tumour DNA analysis demonstrates spatial mutational heterogeneity that coincides with disease relapse in myeloma. Leukemia. 2017;31(8):1695–1705. [DOI] [PubMed] [Google Scholar]
- 97.Leleu X, Karlin L, Macro M, et al. Pomalidomide plus low-dose dexamethasone in multiple myeloma with deletion 17p and/or translocation (4;14): IFM 2010-02 trial results. Blood. 2015;125(9):1411–1417. [DOI] [PubMed] [Google Scholar]
- 98.Avet-Loiseau H, Attal M, Moreau P, et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myélome. Blood. 2007;109(8):3489–3495. [DOI] [PubMed] [Google Scholar]
- 99.An G, Acharya C, Deng S, et al. Cytogenetic and clinical marks for defining high-risk myeloma in the context of bortezomib treatment. Exp Hematol. 2015;43(3):168–176.e162. [DOI] [PubMed] [Google Scholar]
- 100.Klein U, Jauch A, Hielscher T, et al. Chromosomal aberrations +1q21 and del(17p13) predict survival in patients with recurrent multiple myeloma treated with lenalidomide and dexamethasone. Cancer. 2011;117(10):2136–2144. [DOI] [PubMed] [Google Scholar]
- 101.Nahi H, Våtsveen TK, Lund J, et al. Proteasome inhibitors and IMiDs can overcome some high-risk cytogenetics in multiple myeloma but not gain 1q21. Eur J Haematol. 2016;96(1):46–54. [DOI] [PubMed] [Google Scholar]
- 102.Hebraud B, Leleu X, Lauwers-Cances V, et al. Deletion of the 1p32 region is a major independent prognostic factor in young patients with myeloma: the IFM experience on 1195 patients. Leukemia. 2014;28(3):675–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lakshman A, Moustafa MA, Rajkumar SV, et al. Natural history of t(11;14) multiple myeloma. Leukemia. 2018;32(1):131–138. [DOI] [PubMed] [Google Scholar]
- 104.Avet-Loiseau H, Malard F, Campion L, et al. Translocation t(14;16) and multiple myeloma: is it really an independent prognostic factor? Blood. 2011;117(6):2009–2011. [DOI] [PubMed] [Google Scholar]
- 105.Lahuerta JJ, Paiva B, Vidriales MB, et al. Depth of response in multiple myeloma: a pooled analysis of three PETHEMA/GEM clinical trials. J Clin Oncol. 2017;35(25): 2900–2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chakraborty R, Muchtar E, Kumar SK, et al. Impact of post-transplant response and minimal residual disease on survival in myeloma with high-risk cytogenetics. Biol Blood Marrow Transplant. 2017;23(4):598–605. [DOI] [PubMed] [Google Scholar]
- 107.Nadiminti K, Singh Abbi KK, Mott SL, et al. VTD-melphalan is well tolerated and results in very high rates of stringent CR and MRD-negative status in multiple myeloma. Onco Targets Ther. 2017;10:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Paiva B, Cedena M-T, Puig N, et al. Minimal residual disease monitoring and immune profiling in multiple myeloma in elderly patients. Blood. 2016;127(25):3165–3174. [DOI] [PubMed] [Google Scholar]
- 109.Ludwig H, Greil R, Masszi T, et al. Bortezomib, thalidomide and dexamethasone, with or without cyclophosphamide, for patients with previously untreated multiple myeloma: 5-year follow-up. Br J Haematol. 2015;171(3):344–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Roussel M, Lauwers-Cances V, Robillard N, et al. Front-line transplantation program with lenalidomide, bortezomib, and dexamethasone combination as induction and consolidation followed by lenalidomide maintenance in patients with multiple myeloma: a phase II study by the Intergroupe Francophone du Myélome. J Clin Oncol. 2014;32(25):2712–2717. [DOI] [PubMed] [Google Scholar]
- 111.Mateos M-V, Oriol A, Martínez-López J, et al. GEM2005 trial update comparing VMP/VTP as induction in elderly multiple myeloma patients: do we still need alkylators? Blood. 2014;124(12):1887–1893. [DOI] [PubMed] [Google Scholar]
- 112.Oliva S, Gambella M, Gilestro M, et al. Minimal residual disease after transplantation or lenalidomide-based consolidation in myeloma patients: a prospective analysis. Oncotarget. 2017;8(4):5924–5935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Puig N, Sarasquete ME, Balanzategui A, et al. Critical evaluation of ASO RQ-PCR for minimal residual disease evaluation in multiple myeloma. A comparative analysis with flow cytometry. Leukemia. 2014;28(2):391–397. [DOI] [PubMed] [Google Scholar]
- 114.Ferrero S, Ladetto M, Drandi D, et al. Long-term results of the GIMEMA VEL-03-096 trial in MM patients receiving VTD consolidation after ASCT: MRD kinetics’ impact on survival. Leukemia. 2015;29(3):689–695. [DOI] [PubMed] [Google Scholar]
- 115.Chari A, Suvannasankha A, Fay JW, et al. Daratumumab plus pomalidomide and dexamethasone in relapsed and/or refractory multiple myeloma. Blood. 2017;130(8):974–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Korde N, Roschewski M, Zingone A, et al. Treatment with carfilzomib-lenalidomide-dexamethasone with lenalidomide extension in patients with smoldering or newly diagnosed multiple myeloma. JAMA Oncol. 2015;1(6):746–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Patriarca F, Carobolante F, Zamagni E, et al. The role of positron emission tomography with 18F-fluorodeoxyglucose integrated with computed tomography in the evaluation of patients with multiple myeloma undergoing allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21(6):1068–1073. [DOI] [PubMed] [Google Scholar]
- 118.Lapa C, Luckerath K, Malzahn U, et al. 18 FDG-PET/CT for prognostic stratification of patients with multiple myeloma relapse after stem cell transplantation. Oncotarget. 2014;5(17):7381–7391. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.