Abstract
Aim
To determine the prevalence of latent tuberculosis infection (LTI) in a Spanish prison, analyze the main sociodemographic and clinical variables associated with this condition and estimate the percentage of individuals with LTI who have received chemoprophylactic treatment.
Materials and methods
Cross-sectional study including inmates hosted in the Madrid VI Prison on 16/07/2016. Exclusion criteria: history of tuberculosis; non-updated tuberculin test according to the Tuberculosis Prevention and Control Program in Prisons protocol. Information of the variables was collected from SANIT and SIP programs, and by checking the clinical records of inmates. Description of the participant population and comparison between the frequency of distribution of the independent variables in LTI present and absent groups were performed, the last calculating the p value with Ji2 and Mann-Whitney U tests. Bivariate and multivariate analysis have been carried out with a logistic regression model.
Results
936 individuals have been included. The prevalence of LTI in prison is 54.6%. This condition has been linked to the sociodemographic variables age, sex and nationality of origin, being age the one that has shown the strongest association. Among the other factors analyzed, only HCV infection behaves as a predictor of LTI. 30.3% of the individuals with LTI have completed or are receiving chemoprophylactic treatment in the moment of the study.
Discussion
LTI prevalence is high in the Spanish current prison population. The results of the study emphasize the relevance of the LTI screening in the prison setting, specially among high risk groups, and point out the need of a greater effort in the indication and completion of the chemoprophylactic treatment.
Keywords: latent tuberculosis, prevalence, risk factors, prisons, Mycobacterium tuberculosis, tuberculin, Public Health, Spain
Palabras clave: tuberculosis latente, prevalencia, factores de riesgo, prisiones, Mycobacterium tuberculosis, tuberculina, salud pública, España
Resumen
Objetivo
Determinar la prevalencia de infección tuberculosa latente (ITL) en un centro penitenciario tipo español, analizar las principales variables sociodemográficas y clínicas asociadas a este padecimiento, y estimar el porcentaje de individuos con ITL que han realizado tratamiento quimioprofiláctico.
Materiales y métodos
Estudio descriptivo transversal incluyendo a los internos registrados en el Centro Penitenciario Madrid VI a fecha de 16/07/2016. Criterios de exclusión: antecedente de enfermedad tuberculosa o no disponer de prueba de tuberculina actualizada conforme al Programa de Prevención y Control de Tuberculosis en el Medio Penitenciario. Recogida de las variables desde los programas SANIT, SIP y mediante revisión de los historiales clínicos de los internos. Descripción de la población participante y comparación de la frecuencia de distribución de las variables predictoras en los grupos de ITL presente y ausente, calculando el valor p mediante las pruebas de Chi cuadrado y U de Mann-Whitney. Análisis bivariante y multivariante mediante regresión logística.
Resultados
936 pacientes incluidos. La prevalencia de ITL es del 54,6%, y se ha relacionado con las variables edad, sexo y nacionalidad de procedencia, siendo la edad la que mayor fuerza de asociación ha demostrado. Entre el resto de los factores analizados, solo la infección por el virus de la hepatitis C se comporta como elemento predictor de ITL. El 30,3% de los individuos con ITL ha completado o se encuentra realizando tratamiento quimioprofiláctico en el momento del estudio.
Discusión
La prevalencia de ITL en la población penitenciaria española actual es alta. Los resultados refuerzan la importancia de su cribado en el medio penitenciario, especialmente en aquellos grupos de mayor riesgo, así como la necesidad de un mayor esfuerzo en la indicación y la cumplimentación del tratamiento quimioprofiláctico.
INTRODUCTION
Today tuberculosis (TB) is considered a major public health issue. According to the 2017 WHO Global Tuberculosis report, in 2016 1.3 million people died because of this condition. The estimated incidence of tuberculosis worldwide for that same year was 10.4 million cases, of which almost 4.700 were reported in our country 1 .
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis bacillus. The disease is spread when people who are sick with pulmonary TB (index case) expel bacteria into the air, to other people (contacts), therefore causing TB disease or latent tuberculous infection (LTI)- without clinical or radiologic evidence of active disease 2 . An estimated third of the world population currently presents LTI 1 and only between 5 and 10% will develop TB disease during their lifetime, although that proportion can climb up to 30% for patients with HIV 1 , 3 .
For the Prisons Department TB is also one of the most significant public health issues due to its higher incidence with regard to the general population 4 , 5 and to the fact that imprisonment itself is a risk factor for the development of TB disease 3 , 6 , 7 . In this regard, since 1991 the Department has implemented TB prevention and control programs which have been successful in reducing the incidence of the disease among the imprisoned population in our country 8 . These programs focus on the early the early diagnosis and directly observed therapy of new cases, the study of contacts and the detection and prioritization of treatment for LTI cases depending on concurrent risk factors 9 .
Latency is one of the main obstacles in the eradication of TB 10 since most of the cases of active TB are due to the reactivation of latent bacilli, which usually involves individuals with coexisting risk factors 11 . Available evidence suggests that age 12 and comorbidity (such as HIV 1 , rheumatoid arthritis 13 , asthma 10 or chronic kidney disease 14 ), are predictors for both LTI and TB disease. However, studies are controversial on whether social factors such as smoking, alcohol abuse and drug use should be considered 13 , 15 .
The identification of risk groups has become a challenge and a priority to achieve the control and eradication of the disease 16 , 17 . Nevertheless, there are few studies carried out in settings where the incidence is higher such as prisons, and the previously existing data can not be extrapolated to today's Spanish immate population 18 .
This study has a dual objective. On one hand, it intends to estimate the prevalence of LTI in a Spanish type prison (representative of penitentiary facilities built in Spain in the last 25 years) with a urban module structure and a capacity for hosting around 1000 inmates. On the other hand, the study analyses the role of factors traditionally associated to LTI as well as others which can be found among the imprisoned population such as the impact of severe mental illness, being under chronic psychotropic treatment or the inclusion in methadone rehabilitation programmes, which have still not been assessed.
Last, the proportion of LTI patients who have completed or are currently on chemoprophylactic treatment has been estimated.
MATERIAL AND METHODS
Design and subjects of the study
We have carried out a cross-sectional descriptive study in Madrid VI Prison. The target population is that of the correctional facility (Madrid VI). The inclusion criteria was the fact of being registered in this facility on 16/07/2016. 1090 individuals fulfilled this requirement. 154 individuals were excluded of the study: 5 due to a background of TB disease and 149 due to a lack of updated PPD test results according to the protocol of TB Prevention and Control in the Correctional Setting. This protocol establishes, among other recommendations, that PPD test should be repeated every six months in inmates with HIV and every year for HIV-negative patients, provided that there is no previous positive test 9 . The lack of information was due in 34 cases to the refusal of patients to undergo the test, in 69 cases they had already been scheduled for the test but not undergone it yet, and in the remaining 46 because of a delay of the healthcare staff to carry out the test or to transfer the results to the SANIT software.
Variables
Independent variables included in the study were the following: gender (male/female), age classified in 4 groups according to quartiles (under 31/31-38/ 39-47/over 47), nationality classified in 4 categories (Spain and other developed countries/Latin-America/Africa/Eastern Europe and the Middle East), a background of smoking (yes/no), previous methadone maintenance treatment (yes/no), being under chronic psychotropic treatment (yes/no), HIV infection (yes/no), active or resolved HCV infection (yes/no), severe mental disorder (yes/no) and previously completed or current chemoprophylactic treatment (yes/no). The dependent variable is LTI (present/absent). Variables PPD test result (positive, negative and unavailable) and previous TB disease (yes/no) were used to determine the excluded cases.
LTI was considered for those individuals with positive PPD test, measured as a swollen area (induration) of 5 mm or more or as the appearance of vesicles or necrosis 48-72 hours after the injection, regardless the vaccination status of patients. In all cases, active disease was ruled out. LTI was excluded in those cases without positive criteria after assessing the booster effect and discarding recent infectious processes.
The diagnosis of severe mental disorder was established in those patients with non-organic psychotic disorders and some cases with ongoing personality disorder for over 2 years, who also presented moderate to severe dysfunction in terms of work, social and family performance.
Collection of data and statistical analysis
Data on the variables gender, age and nationality were obtained by means of the SIP software (Prison Information System of restricted access). The infor mation on a background of psychotropic treatment, PPD results, HIV and HCV infections was collected by means of the SANIT software. In order to establish the background of TB disease, smoking, methadone maintenance treatment and previously completed or current chemoprophylaxis, paper medical records were consulted. With regard to the diagnosis of severe mental disorder, this was consulted in a computer-based record of the Madrid VI setting itself. The collection of data was carried out by a single investigor.
For the analysis of data, SPSS Statistics 23 programme was used. The description of qualitative variables and the estimation of LTI prevalence are depicted as absolute values and percentages. For the continuous quantitative variable age, the distribution of its values was assessed by means of the Kolmogov-Smirnov test, by considering central trend measures such as the median and inter-quartile ranges (IQR), due to its non-normal distribution. The frequency of distribution of independent variables in the LTI present or absent groups has been analyzed. To verify the differences between both groups p value has been calculated by means of Ji2 and Mann-Whitney U tests. Statistical significance was defined for p value of 0.05 or less. The magnitude of the association between different variables and the presence of LTI has been established by means of logistic-regression bivariate and multivariate analysis, therefore considering potential confusing factors. The calculated association measure has been the odds ratio with 95% confidence intervals.
Limitations of the study
The technique used to diagnose TB infection is PPD test, which after the injection of a purified protein derivate (PPD RT-23) shows previous hypersensitivity to that substance. PPD is highly sensitive for individuals with unaltered immune response. However, for HIV-positive patients its sensitivity drops to 70% 19 , 20 which can entail a significant proportion of false-negatives in this population group. Another drawback of PPD test is that proteins are non-specific for Mycobacterium tuberculosis, but common to other non-tuberculous mycobacteria and to Mycobacterium bovis (present in BCG vaccine), which further reduces the specificity of the test and can lead to false-positives.
RESULTS
A total of 936 patients were included in the study, with a mean age of 38 (IQR 31-47), among which 97.4% were males. The vast majority of inmates were originally Spanish (64%), while the remaining 36% were foreign (from 57 different nationalities). 75.4% had a background of smoking, 44.1% were under chronic psychotropic treatment and 13.4% had been on methadone maintenance treatment at some point. The prevalence of HIV infection was 5.6%. 17.4% of the individuals had a background of active or resolved HCV infection and 4.5% had some type of severe mental disorder. In the sample, 511 inmates had a positive PPD test, which entails a prevalence of LTI of 54.6% in this facility. Among patients with LTI, 155 (30.3%) had completed or were currently on chemoprophylactic treatment, while 69.7% were not.
When comparing inmates with and without LTI there are statistically significant differences with regard to the distribution of the following variables: gender (p=0.003), age (p under 0.001), prior or current treatment with methadone (p=0.001), chronic psychotropic treatment (p=0.010) and active or resolved HCV infection (p under 0.001) (see Table 1), unlike the variables smoking (p=0.317), HIV infection (p=0.454) and severe mental disorder (p=0.734). As for the stratified variable nationality, p value was 06.
Table 1. Sociodemographic and clinical features of individuals included in the study with regard to the presence or absence of LTI.
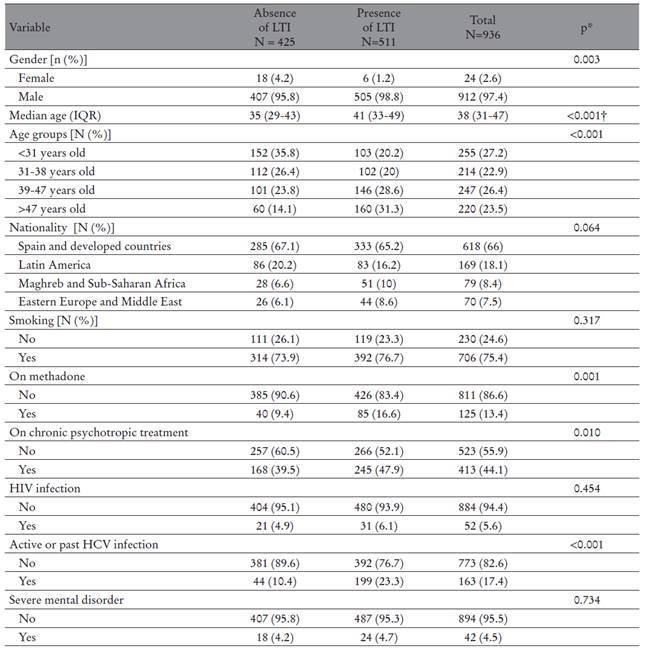
Note. LTI: latent tuberculosis infection; IQR: Inter-quartile range; HVI: human immunodeficiency virus; HCV: Hepatitis C Virus.
*Chi-square. †Mann-Whitney U.
Table 2 depicts the results of bivariate and multivariate analysis, which show the magnitude of the association between the different variables analysed and the presence of LTI. Thus, after adjustment for confounding factors, multivariate analysis shows that there is a higher probability of suffering LTI between male individuals [OR 3.12 (95%CI 1.19-8.16)] and between individuals who are over 38 years old [OR 2.08 (95%CI 1.41-3.05) in the group of 38 to 47 years old with regard to the group of less than 31 years old, and OR 3.90 (95%CI 2.56-5.93) in the group over 47 years old with regard to the same reference group]. As far as nationality is concerned, coming from Eastern Europe or the Middle East was associated with over a two fold increase of the probability of suffering LTI in comparison with coming from Spain or other developed countries [OR 2.13 (95%CI 1.24-3.69)]. This probability is even higher in case of African origin [OR 2.69 (95%CI 1.59-4.55)]. Last, HCV infection was also associated to a higher risk of LTI [OR 1.96 (95%CI 1.22-3.16)].
Table 2. Factors associated to the presence of LTI: bivariate and multivariate analysis.
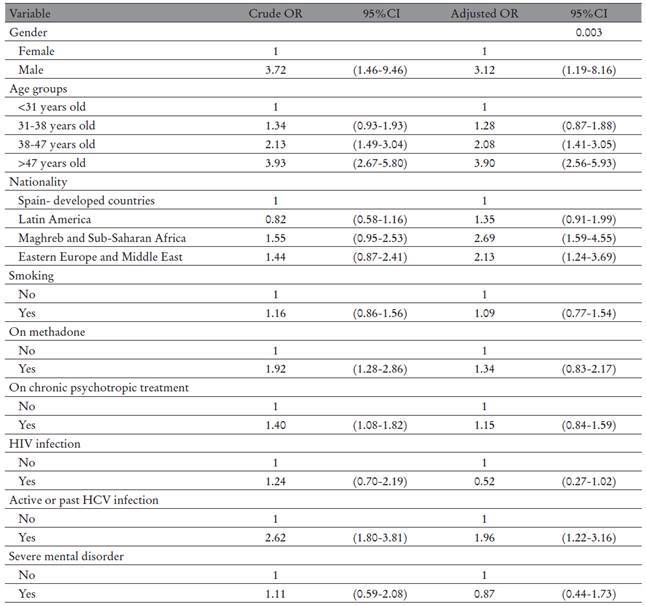
Note. 95%CI: confidence interval; OR: odds ratio.
Multivariate analysis has not shown association between the rest of variables and LTI.
DISCUSSION
This results are coherent with those concluded in the “Multi-centre study on the prevalence of latent TB infection among the population of Spanish prisons” 12 , based on data collected in 2008 from 341 individuals belonging to 18 Spanish correctional facilities. Therefore, in that study the prevalence of LTI was 50.4% (95%CI 45.0-55.9%), while ours was 54.6%. The difference between both figures could be due to the fact that the diagnostic criteria for LTI in that study was more restrictive, considering as positive the PPD test when the induration reached 5 mm or more in HIV-positive patients, and 10 mm or more in HIV-negative patients after 48.96 hours of injection, while our study considered a positive result an induration of 5 mm or more regardless the background of HIV infection. The prevalence of LTI was similar to that reported by other previous studies carried out on inmate population in our country 21 , 22 . These data significantly differ from the prevalence of LTI among the general population as noted by the WHO, which estimates it around 30% 1 , as well as by a study carried out in the general Spanish population which estimates it around 15% 23 .
With regard to LTI-associated factors, multivariate analysis reveals a higher probability of suffering this condition in males. This is coherent with the results of another study carried out in 2003 on the Spanish general population 23 . However, the result of our study lacks accuracy and it should be noted that only 24 women were included (2.6%). Thus, this result should be considered with precaution. The association between LTI and the variables age and nationality is also consistent with the previous literature 12 , 18 . This can be explained by the fact that the older the individual is, the higher risk of infection due to a more prolonged exposure time. On the other hand, a higher prevalence of LTI is found among individuals who come from countries where TB is still endemic.
The association between LTI and HCV had been previously noted by a case-control study on inmates in the USA 13 , despite the fact that other studies have been unable to reach that same conclusion 12 . Our result could be due to the fact that HCV infection in the correctional setting is associated to intravenous drug use, and thus to socially disadvantaged populations who are traditionally at higher risk of LTI.
As for HIV, we have found a higher frequency of LTI among individuals with HIV infection. Nevertheless, multivariate analysis shows an OR of 0.52 with a CI including the null value. Therefore this result should be carefully considered since it could be influenced by other factors, such as the possibility of PPD false negative results.
Last, the percetage of individuals with LTI who had completed or were under chemoprophylactic treatment was 30.3%. That proportion is low and its below the data of 48% pointed out by a study conducted in 1999 on the Spanish inmate population 22 . Our study has not taken into account the reasons why a high proportion of inmates have not completed that treatment (refusal or abandon, medical contraindication or lack of prescription).
CONCLUSIONS
The prevalence of LTI in today’s Spanish inmate population is still high, being above that of the general population. In penitentiary facilities, LTI is associated to male gender, an older age, and the origin from countries where TB is endemic, being age the variable most strongly associated. Among the rest of variables under study, only HCV infection acts as a predictor for LTI. These results reinforce the relevance of LTI screening in prisons, especially among those groups with more risk factors; and they suggest that further effort should be made in prescribing and completing chemoprophylactic treatment, as measures needed to reduce the development of TB disease and prevent its transmission.
BIBLIOGRAPHIC REFERENCES
- 1.World Health Organization Global tuberculosis report. 2017 Available from: http://www.who.int/tb/publications/global_report/en/
- 2.Young KH, Ehman M, Reves R, Peterson Maddox BL, Khan A, Chorba TL, et al. Tuberculosis Contact Investigations - United States, 2003-2012. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1369–1374. doi: 10.15585/mmwr.mm6450a1. [DOI] [PubMed] [Google Scholar]
- 3.Nogueira P, Abrahao R, Galesi V. Tuberculosis and latent tuberculosis in prison inmates. Rev Saúde Pública. 2012;46:119–127. doi: 10.1590/s0034-89102011005000080. [DOI] [PubMed] [Google Scholar]
- 4.Kamarulzaman A, Reid SE, Schwitters A, Wiessing L, El-Bassel N, Dolan K, et al. Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet. 2016;388(10049):1115–1126. doi: 10.1016/S0140-6736(16)30769-3. [DOI] [PubMed] [Google Scholar]
- 5.Rueda ZV, Arroyave L, Marin D, Lopez L, Keynan Y, Giraldo MR, et al. High prevalence and risk factors associated with latent tuberculous infection in two Colombian prisons. Int J Tuberc Lung Dis. 2014;18(10):1166–1171. doi: 10.5588/ijtld.14.0179. [DOI] [PubMed] [Google Scholar]
- 6.O'Grady J, Maeurer M, Atun R, Abubakar I, Mwaba P, Bates M, et al. Tuberculosis in prisons: anatomy of global neglect. Eur Respir J. 2011;38(4):752–754. doi: 10.1183/09031936.00041211. [DOI] [PubMed] [Google Scholar]
- 7.Baussano I, Williams BG, Nunn P, Beggiato M, Fedeli U, Scano F. Tuberculosis incidence in prisons: a systematic review. PLoS Med. 2010;7(12):e1000381. doi: 10.1371/journal.pmed.1000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Secretaría General de Instituciones Penitenciarias. Subdirección General de Coordinación de Sanidad Penitenciaria Casos de tuberculosis en Instituciones Penitenciarias. 2013 Available from: http://www.institucionpenitenciaria.es/web/export/sites/default/datos/descargables/saludpublica/Tuberculosis_en_IIPP_2013.pdf.
- 9.Secretaría General de Instituciones Penitenciarias. Coordinación de Sanidad Penitenciaria Programa de Prevención y Control de Tuberculosis en el Medio Penitenciario. (3) 2011 Available from: http://www.institucionpenitenciaria.es/web/export/sites/default/datos/descargables/publicaciones/Programa_de_Prevencion_y_Control_de_la_Tuberculosis.pdf.
- 10.Barrios-Payan JA, Castanon-Arreola M, Flores-Valdez MA, Hernandez-Pando R. Biological, clinical and epidemiological aspects of latent tuberculosis. Salud Publica Mex. 2010;52(1):70–78. doi: 10.1590/s0036-36342010000100011. [DOI] [PubMed] [Google Scholar]
- 11.Gómez Rodríguez F, Bernal Bermúdez J, García Egido A. Evaluación y tratamiento de la tuberculosis latente en el adulto. Med Clin. 2001;117(3):111–114. doi: 10.1016/s0025-7753(01)72031-3. [DOI] [PubMed] [Google Scholar]
- 12.García-Guerrero J, Marco Mouriño A, Sáiz de la Hoya Zamácola P, Vera-Remartínez EJ, Grupo de estudio PREVALHEP de prisiones Estudio multicéntrico de prevalencia de infección tuberculosa latente en los internados en prisiones españolas. Rev Esp Sanidad Penit. 2010;12(3):79–85. doi: 10.4321/S1575-06202010000300003. [DOI] [PubMed] [Google Scholar]
- 13.Weant TE, Turner AN, Murphy-Weiss M, Murray DM, Wang SH. Can social history variables predict prison inmates' risk for latent tuberculosis infection? Tuberc Res Treat. 2012;2012:132406. doi: 10.1155/2012/132406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foster R, Ferguson TW, Rigatto C, Lerner B, Tangri N, Komenda P. A retrospective review of the two-step tuberculin skin test in dialysis patients. Can J Kidney Health Dis. 2016;3:28 doi: 10.1186/s40697-016-0119-4. -016-0119-4. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamani M, Mahmudian H, Majzoobi MM, Poorolajal J. Prevalence and incidence rates of latent tuberculous infection in a large prison in Iran. Int J Tuberc Lung Dis. 2016;20(8):1072–1077. doi: 10.5588/ijtld.15.0857. [DOI] [PubMed] [Google Scholar]
- 16.Dara M, Grzemska M, Kimberling M, Reyes H, Zagorskiy A. Guidelines for control of tuberculosis in prisons. United States Agency for International Development. 2009. Available from: http://pdf.usaid.gov/pdf_docs/PNADP462.pdf. [Google Scholar]
- 17.DiNardo AR, Guy E. Reactivation tuberculosis: role of surveillance. Expert Rev Anti Infect Ther. 2016;14(5):501–509. doi: 10.1586/14787210.2016.1173541. [DOI] [PubMed] [Google Scholar]
- 18.Marco A, Sole N, Orcau A, Escribano M, del Bano L, Quintero S, et al. Prevalence of latent tuberculosis infection in inmates recently incarcerated in a men's prison in Barcelona. Int J Tuberc Lung Dis. 2012;16(1):60–64. doi: 10.5588/ijtld.11.0007. [DOI] [PubMed] [Google Scholar]
- 19.Ai JW, Ruan QL, Liu QH, Zhang WH. Updates on the risk factors for latent tuberculosis reactivation and their managements. Emerg Microbes Infect. 2016;5:e10. doi: 10.1038/emi.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arias Guillén M. Avances en el diagnóstico de la infección tuberculosa. Arch Bronconeumol. 2011;47:521–530. doi: 10.1016/j.arbres.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 21.Sole N, Marco A, Escribano M, Orcau A, Quintero S, Del Bano L, et al. Prevalence of latent tuberculosis infection amongst immigrants entering prison. Rev Esp Sanid Penit. 2012;14(1):12–18. doi: 10.1590/S1575-06202012000100003. [DOI] [PubMed] [Google Scholar]
- 22.Martín V, Brugos M, Valcarcel I. Prevalencia de tratamiento de la infección tuberculosa en una prisión provincial. Rev Esp Salud Publica. 2000;74(4):361–366. [PubMed] [Google Scholar]
- 23.Alcaide Megias J, Altet Gomez MN, Canela-Soler J, Pina Gutierrez JM, Mila Auge C, de Souza Galvao ML, et al. A study of the tuberculous infection in adults. Rev Clin Esp. 2003;203(7):321–328. doi: 10.1157/13048022. [DOI] [PubMed] [Google Scholar]


