Abstract
Systemic lupus erythematosus (SLE) is an autoimmune disease associated with widespread inflammation and tissue damage. It is more common and severe among Blacks, Hispanics, and Asians; with higher incidence in women. While the goals of medical treatment are to prevent flares and reduce organ damage, up to 50% of patients perceive their health to be suboptimal with unaddressed needs including fatigue and pain. Recent SLE treatment guidelines focus on improving quality of life. Yoga has shown improvements in quality-of-life and fatigue in various diagnoses. While there is growing evidence that yoga therapy may help osteoarthritis and rheumatoid arthritis symptoms, there is only one reference in the literature related to SLE.
Methods/Setting:
An adjunct study was undertaken to evaluate adapting the Yoga as Self Care for Arthritis in Minority Communities study for a bilingual population living with SLE in the Washington, DC area. Informants included 7 patients enrolled onto the study, and 3 yoga instructors living with SLE. Qualitative methods included journals and semi-structured interviews.
Results:
Enrolling patients clarified revisions for intake questionnaires, and symptoms that may impact class participation. Participants demonstrated increased balance, body awareness, and tolerated a faster-paced yoga class when compared to those in parent study. Yoga instructors’ recommendations included modifying the yoga based on energy levels and frequent changes in physical ability.
Conclusion:
This paper shares perspectives from various informants and affirms the feasibility of progressing to a larger study. It summarizes our findings and recommendations towards creating a randomized controlled trial, as there are currently none in the literature.
Keywords: yoga, systemic lupus erythematosus, minority, qualitative methods, bilingual, journals, narratives
1. Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease in which immune system dysregulation leads to widespread inflammation and tissue damage. Lupus is a chronic disease that causes inflammation affecting the skin, joints, kidneys, lungs, nervous system and/or other organs of the body [1–6]. Most often, lupus starts at ages 20–40, occurring ten times more often in women than men [4, 5, 7]. Minority patients tend to have more abrupt disease onset, more severe clinical manifestations, and worse disease activity [4, 8, 9]. Regardless of age and gender, Hispanic, African American, and Asian SLE patients tend to have more hematological, serosal, neurological, and renal manifestations [9, 10]. There is currently no cure [1, 4].
SLE is relatively uncommon and is not a reportable disease. Estimates from population-based lupus patient registries [11] suggests a prevalence of 161,000 with definite SLE and 322,000 with definite or probable SLE [12]. National incidence estimates range widely, from 1.8 to 7.6 cases per 100,000 persons per year in parts of the United States [13, 14]. Lupus flares vary from mild to serious and life threatening. Most patients have periods of disease activity (flares), followed by times when the symptoms are mostly quiet (remission) [1, 4]. In one study, nearly 60% of the patients had flares or persistently active disease per year [15]. The overall goal of standard medical treatment is to prevent flares, to reduce organ damage and other problems [16].
1.1. Physician Patient Disconnect
Discordance between physician and patient disease activity ratings may affect quality of care [9]. Clinical measures of disease activity and organ damage may be poor indicators of a patient’s overall health status. Even when clinical parameters show improvement, in some studies up to 50% of patients perceive their health to be suboptimal [17]. Results of two previous SLE Needs Questionnaire surveys revealed 94–100% of patients have at least one unaddressed need related to their illness, most commonly fatigue/tiredness and pain [17]. Because of better testing, earlier diagnosis, and optimal treatment the overall prognosis has changed. SLE patients now experience over a 90% survival rate at 5 years [5, 9]. However less favorable survival of ethnic minorities is possibly related to socioeconomic status and access to medical care [9, 10]. Quality of life can suffer because of symptoms like fatigue and joint pain. Recently published treatment guidelines focus on improving the quality of life of patients with SLE [18].
1.2. Yoga and Arthritis
Studies have shown exercise to be safe, reduce fatigue, and not aggravating to SLE disease activity [19–24]. However, willingness to participate in an exercise program or to continue regular exercise may be problem [24]. Complementary and integrative health (CIH) practices are increasingly common supplements to standard treatment and the details of their application in SLE are crucial for rheumatologists to understand [25]. While there is growing evidence that yoga therapy may help both osteoarthritis and rheumatoid arthritis [26], a literature search of ‘yoga and lupus (or SLE)’ performed using Pubmed, Scopus, CINAHL and Web of Science yielded no published articles only a meeting abstract [27]. Additional information about the same study, offered within another paper, indicated that it was implemented at the McGill University Health Centers Lupus Clinic in Montreal, Canada. Focus groups and participant surveys indicated perceived improvement of overall well-being, improved stress and pain management, healthier relationships, and better sleep. All participants wished to continue yoga but were hesitant to try programs not designed for SLE [28].
In the yogic literature, there are refereces regarding the potential for yogic practices to enhance muscular strength, body flexibility, reduce stress, depression, and chronic pain, improve sleep patterns, enhance overall well-being and quality of life [29]. Mind-body therapies, including yoga, call for simultaneous attention to the body, breathing, attentional and affective regulation and cognition. Previous studies have shown patients utilizing mind-body therapies such as yoga, reported a shift in their experience of negative emotions as well as the development of self-regulatory skills in dealing with pain, emotional regulation and re-appraisal of life situations [30]. Studies indicate that elements of yoga (gentle movement, slow breathing, meditation, and guided imagery) may lead to mental relaxation and influence aspects of the parasympathetic nervous system associated with a body when at rest [31–36].
In regards to SLE, from a yogic perspective, during flare periods the body needs help to shift from the high-alert focus of the sympathetic nervous system to the quiet, immunity-supporting role of the parasympathetic nervous system. Recommendations include using restorative and gentle poses, breathing, and meditation to help manage chronic, painful conditions and calm a stressful mind until inflammation has subsided [37, 38]. When symptom free, a broader-based yoga practice focusing on proper alignment and putting the joints through a full range of motion can be useful; such as a beginning-level alignment-based yoga class along with a gentle vinyasa-type practice. Yoga nidra (a deep relaxation/meditation technique) is also recommended as a restorative practice during all lupus stages [37]. Because lupus affects each patient differently, yoga interventions can be individualized for the array of symptoms observed.
1.3. Study Objective
In 2014, the principal investigator (SH) for the Natural History of Systemic Lupus Erythematosus (Clinical trial# NCT00001372), requested to add patients to the current protocol and to consider creating a new protocol specific for SLE. The objective of this adjunct study was to determine the feasibility of adapting the pilot yoga protocol Yoga as Self Care for Arthritis in Minority Communities (ClinicalTrials.gov# NCT01617421) for persons with SLE. The pilot study was initiated to investigate the feasibility and acceptability of offering a therapeutic yoga intervention to minority patients diagnosed with rheumatoid arthritis (RA) and osteoarthritis (OA) being served by the National Institute of Arthritis and Musculoskeletal and Skin Disease (NIAMS) Community Health Center (CHC) [39]. This paper shares our experience exploring perspectives from patients, and yoga teachers; combined with observations from clinicians and researchers as a precursor to creating a larger study. It offers recommendations for a future randomized controlled trial (RCT) of yoga for SLE, as there are currently none in the literature.
2. METHODS
2.1. Formative work
The research group met with NIAMS rheumatologists and nurse practitioners to discuss psychosocial and clinical differences observed when caring for patients with RA/OA versus SLE. SLE makes up approximately 25% of the patients seen at the NIAMS CHC and is the third largest diagnosis group after RA and OA. Those with SLE tended to be younger, were more often employed, and offered more complaints of fatigue but reported less joint pain. As mentioned in the literature [40–42], clinicians expressed concerns that being diagnosed with a chronic illness at a young age coupled with the unpredictable nature of disease activity appeared to lead to overwhelming feelings and frustration within the NIAMS clinic population. A yoga intervention was being explored to determine the potential to improve quality of life and reduce reports of fatigue.
Additionally, to ascertain interest from the clinic population in yoga as part of a research protocol, bilingual (English/Spanish) informal interviews were conducted with twenty-eight patients from the National Institutes of Health (NIH) lupus clinic between August and September 2014. When given the choice of four options, stretching and relaxation were of greater interest than movement and stress reduction. Other reasons for willingness to try yoga included: increased energy, help with fatigue, sleep, stress, and flexibility.
2.2. Eligibility Criteria and Patient Recruitment
An amendment to add five SLE patients to test the acceptability/feasibility of the current study design for this new diagnosis was approved by National Institute of Diabetes and Digestive and Kidney Disease (NIDDK)/NIAMS intramural institutional review board (IRB) in July 2014. Research participants were recruited from English-speaking or Spanish-speaking patients receiving care from the NIAMS CHC located in the Washington DC metro region. Patients met enrollment criteria from the original protocol [39]; additional appropriateness for yoga was determined by rheumatology clinicians familiar with each patient’s medical history. Because this diagnosis was new for the pilot protocol, during enrollment, participants were encouraged to discuss their experience living with SLE.
2.3. Intervention and Participant Data Collection
The study used Hatha yoga and follows the format of the previous Yoga for Arthritis RCT conducted through Johns Hopkins University [26]. Bilingual yoga classes were held for 60 minutes biweekly, over eight weeks, at a yoga studio in Washington, DC. Classes included deep breathing, relaxation, meditation, poses for strength, flexibility, and balance. Additional details can be found in the protocol articles [39, 43, 44]. All participants received yoga equipment, bilingual manuals, and were encouraged to develop a home practice based on concepts taught during classes. Personal journals were used to record home practice and participant observations [43]. Bilingual semi-structured open-ended exit interviews were conducted to gather perceptions about yoga classes and the study design. Exit interviews were completed in the yoga studio following the last class, and lasted approximately 30 minutes. Field notes and observational data were also collected during the study.
2.4. Participant Qualitative Data Analysis
Participant journals were analyzed using content analysis techniques. An audit trail was maintained through written documentation of the group process. NVivo (version 10) electronic database was used to organize transcripts and assemble themes. Both data triangulation (using more than one source of data) and investigator triangulation (using several evaluators) were used to reduce potential bias [43].
Analyses and validation were conducted in three stages: 1) two researchers (SHM and GTA) each independently coded using inductive analysis, 2) using an iterative coding process, these two researchers met regularly with two additional researchers (KRM and MML) and themes were discussed until consensus and saturation of themes was reached, and 3) finally two additional researchers not involved in the original theme selection (GW and NF) evaluated suggested themes and related quotes for credibility and continuity. Suggestions from each stage were incorporated into selection of final themes.
Since exit interview responses, unlike journal entries, were from open-ended questions, these were analyzed using a cutting and sorting (card sort) method.[45] Responses were categorized as elaborating on survey questions, mapping to existing journal themes, or identifying unique themes. Field notes were added, when needed, to clarify participant comments.
2.5. Yoga Teachers Data Collection
All three yoga instructors had completed the 30 hour Yoga for Arthritis teacher training created for the Hopkins study and were familiar with the series of poses used in the protocol. Suggestions from yoga teachers living with lupus were collected via individual conversations and written submissions. Group consensus was obtained through a conference call with all three instructors.
3. RESULTS
3.1. Characterizing Research Participants
The accrual goal was set at 5 patients. Based on attrition from previous studies [44], 7 patients were enrolled. Baseline questionnaires and physical assessments were completed, then all 7 were waitlisted until a suitable cohort was formed. The start of the intervention was determined by attending the first yoga class, (n=3) met this criteria. Background information regarding those who participated in the 8-week yoga series from July–August 2015 are listed below.
Participant A was a 52 year old Hispanic, female from Honduras who worked part-time in a grocery store. She had been in the US for 11 years, and diagnosed with SLE for 2 years. Her body mass index (BMI) was 33.6 (obese), she reported moderate pain in 2 out of18 joints, and morning stiffness. She used four types of complementary and alternative medicine (CAM) (categories included vitamins, supplements and spirituality). During the rehab assessment, she complained of pain in lower back and right shoulder but reported no physical limitations. She attended 4 out of 16 classes, and practiced at home 2.5 days/week.
Participant B was a 37 year old Hispanic, female from El Salvador who worked at a grocery store as a cake decorator. She had been in the US for 13 years and diagnosed with SLE for 1 year. Her BMI was 31.4 (obese), she reported mild pain in 4 out 18 joints, and no morning stiffness. She reported using CAM (vitamins). During the rehab assessment, she reported occasional vigorous exercise, occasional low back pain, and no physical limitations. She attended 13 out of 16 classes, and practiced at home 2.4 days/week.
Participant C was a 44 year old Black/Hispanic female from Dominican Republic who worked as a web designer. She had been in the US for 7 years and diagnosed with SLE for 5 years. Her BMI was 23.5 (normal weight), she reported having 1 joint with mild pain and 4 with moderate pain out of 18 joints, and morning stiffness. She used nine types of CAM (categories: providers, diet, vitamins, rubs, movement, and spirituality). During the rehab assessment, she reported mild exercise, history of chronic pain in knees, shoulder and mid-back with a history of scoliosis; but no physical limitations. She attended 15 out of 16 classes, and practiced at home 1.3 days/week. Prior to SLE diagnosis, she reported having complete body stiffness with pain in neck, lower back, and two middle fingers; impaired sleep, and reduced energy. In 2010, she completely deteriorated with a face rash, hair loss, and toothaches (ulcers). From 2010–2013 she reported being seen monthly by a physician for various symptoms.
The SLE cohort (n=7) were all female and Hispanic. Most (85.7%) were employed and physically active (Table 1). The measure for balance (single-leg stance) showed statistically (ttest comparison p value=0.043) what researchers observed during yoga classes, the SLE cohort could hold balancing poses longer than the RA/OA cohort. Researchers also observed the SLE group appeared to have increased body awareness, willingness to attempt more challenging poses, and the ability to tolerate a faster paced yoga class.
Table 1:
Characterizing Participants
| Baseline Values | (n=7) |
|---|---|
| Employed (f/t or p/t) | 85.7% |
| Occasional/mild exercise | 85.7% |
| No painful joints | 67.5% |
| Mean values | |
| Age (years) | 43.9 |
| Duration of arthritis (years) | 5.2 |
| BMI | 30.7 |
| Pain intensity (possible range 0–10) | 5.6 |
| Self-rated health* | 3.9 |
| Self-Efficacy Exercise Regularly^ | 5.8 |
| Physical Function- Balance | |
| Single leg stance (seconds) left | 26.8 |
| right | 24.0 |
Self-rated health – “Would you say your health in general is 1-excellent, 2-very good, 3-good, 4-fair, or 5-poor?”)
Self-efficacy (1 (not at all confident) to 10 (totally confident)) in being able to exercise.
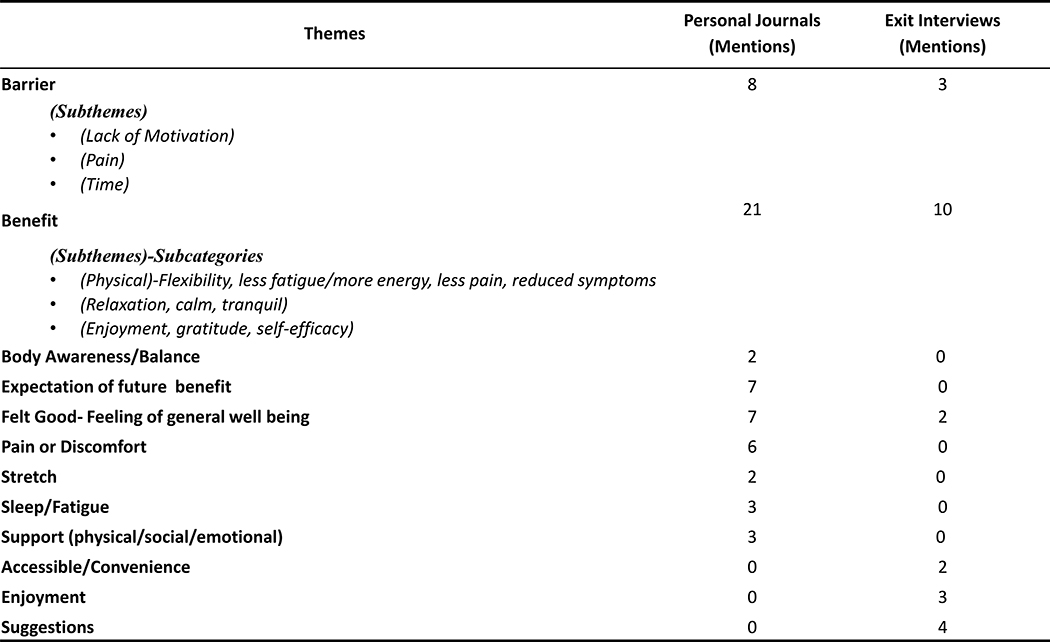
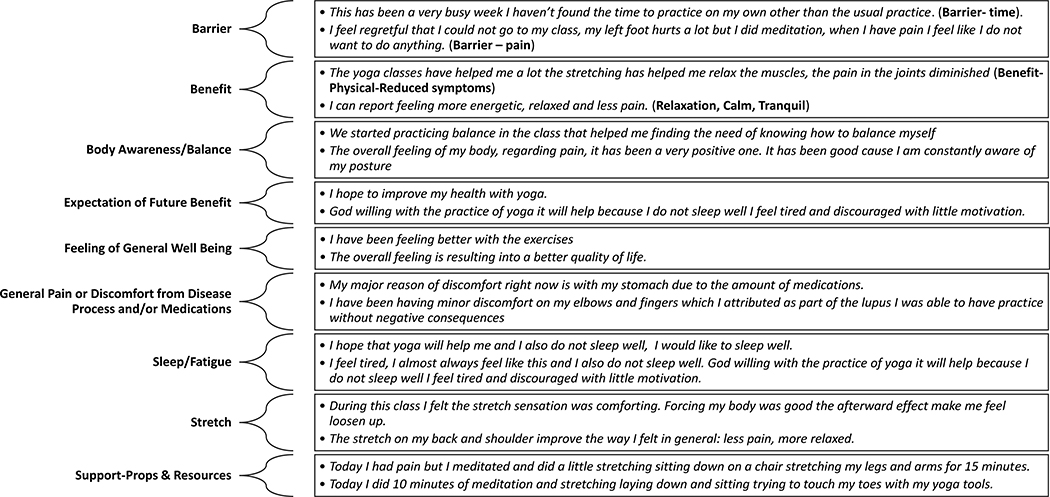
Figure 1 shows most frequently mentioned themes along with corresponding subthemes and subcategories predominantly related to benefits and barriers of learning yoga. Participant quotes related to selected themes are highlighted in figure 2. The matrix format shows similar themes were obtained from participant journals and when responding to open-ended exit interview questions.
Figure 1:
Matrix of Qualitative Themes by Data Collection Source
Figure 2:
Selected Participant Themes and Quotes (n=3)
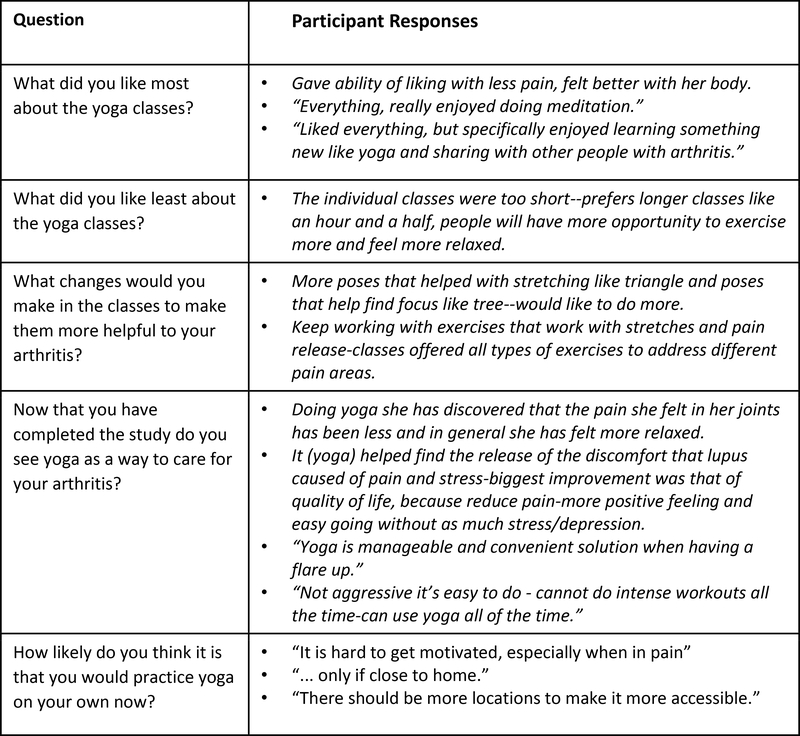
3.2. Exit interview comments
During one-on-one exit interviews, participants were encouraged to elaborate on open-ended options (listed in the original protocol appendix [39]). Exit interview responses (figure 3) provided additional information related a desire for longer classes, enjoyment of poses perceived as helpful for SLE, and potential barriers related to accessibility and convenience.
Figure 3:
Participant Exit Interview Feedback (n=3)
3.3. Yoga Instructors living with SLE
In order to obtain more information about the unique yoga needs of those with SLE, research team members met with three yoga instructors diagnosed with lupus. Each shared background details in order elucidate their experience of living with SLE:
Instructor C –
a 42 year old African American female who had been diagnosed with lupus for 14 years. She had practiced yoga for 14 years and had been a yoga instructor for 5 years. She began practicing yoga because she was “motivated to get her life back” and reduce the anxiety and fatigue from lupus. She began with a 45 minute ‘tape’ of gentle flow yoga and continued because she felt energized, she enjoyed poses that helped get her blood flowing and tune out chaos.
Instructor CC–
a 45 year old White female diagnosed with lupus for 7 years, she had been practicing yoga for 25 years and a yoga teacher for 2 years. She had lupus since a teenager but didn’t know due to constellation of symptoms. She reported having both lupus and arthritis flares. On good days, she enjoys a vigorous yoga practice, however, she stated she was aware of the uncertainty of her symptoms from day to day.
Instructor S –
a middle aged African American female and advanced yoga teacher. It took her 2 years to understand what aspects of yoga practice would help to manage lupus. Her body changes daily and she has to constantly adjust. When feeling well, her practice is to stretch muscles with long holds, slow transitions, and meditation to help keep mindful and calm. Before every practice she assesses what her body is capable of doing and makes modifications. Vinyasa-flow yoga after a flare helps her focus and reduce fatigue because of the pace.
Given their background with the class content, these instructors were asked to give suggestions to revise the 16-class yoga series for people living with SLE. They provided feedback on three subject areas: lupus flares, yoga practices, and contraindications.
Lupus flares –
Depending on the severity of symptoms, yoga practice may require no modification or only slight adjustments. Migraines, balance challenges, depressive symptoms, sore joints, and fatigue were all mentioned as features of lupus flares that impact yoga practice. Recommendations were made to accommodate these challenges since flares could feel discouraging and foster negativity; applying positive mantras may be additional useful strategies. Despite their many benefits, the up-and-down motions of sun salutations can trigger migraines. Moon salutations may be substituted, which can be done slowly and with less upand-down movement. During a flare, challenging balancing postures might be replaced with easier standing postures with shorter holds. To counter the inclination to remain curled up, chest openers as restoratives with props can help to combat fatigue and depression. Excess fatigue may result in a break from practice. When returning to practice, a slow vinyasa practice is suggested to foster mindfulness without fatigue.
Yoga practices (physical poses, meditation, restoratives, and breath work) –
It was suggested that participants start supine since this position is effortless, and then progress to more balancing and core strengthening poses. Beginning each class with meditation was a common suggestion, as it can support self-assessment and body attunement to guide yoga practice. Regarding breath-work (pranayama), cooling breath practices were recommended, to counter what is considered a ‘heat generating’ condition. Both meditation and breath work might be started in short intervals, especially for beginners who may be resistant.
There were mixed perspectives regarding restorative poses. It was suggested that 25–50% of class time should be dedicated to restorative postures because they provide centering and can be practiced during flares. One instructor reported that restoratives fostered mind chatter, which may be overcome by reducing long periods of silence.
Instructors agreed that when not having flares, a moderate level, fast-paced yoga practice (Vinyasa/flow) could help with overall fitness and building self-awareness. Instructors asserted sun salutations provide a challenging home practice, but are gentle enough not to cause pain during practice. There was a recommendation to substitute legs-up-the-wall or bridge poses instead of more challenging inversions. One instructor suggested the Iyengar model of practicing class rotation to encourage home practice for disease management since it is a “plug and play model”. This empowers the participant to adjust practice based on how they feel and may be less overwhelming than learning many postures. It is helpful to modify based on energy and ability at the time of practice.
Contraindications –
Despite the challenges of managing morning stiffness, instructors suggested morning classes when patients have more energy. Also, yoga instructors echoed the avoidance of balancing postures during flares due to ongoing fatigue and muscle weakness consistent with the disease. Instead, it would be easier to do standing postures (tree pose) while holding for less time than harder poses like warrior III or revolved half-moon.
4. DISCUSSION
Our study offers a unique perspective that addresses the feasibility of offering a modified yoga series to those with SLE but can also link these findings to our RA/OA feasibility/acceptability study [43, 44] and ultimately back to the Johns Hopkins’ Yoga for Arthritis efficacy study [26]. When designing future studies, our findings may help mitigate the assumption that those living with RA/OA would report more pain than SLE. While significance may not have been found on all measures due to the small sample size, our SLE cohort tended to more often be employed and to be more physically active. Interestingly, the measures for self-rated health and self-efficacy yielded similar results between the two groups. Additionally, several participants in both cohorts stated yoga helped them learn more about their bodies and to foster a positive outlook when living with a rheumatic disease.
Yoga is proposed to offer methods for regulation and resilience through the integrated practice of yamas and niyamas (ethical/intentional principles), asana (physical exercises), pranayama (breathing techniques) and meditation [30, 46]. The focus of yoga therapy on cultivating the connection to steadfast joy, eudaimonic well-being, meaning, and purpose highlights an important place for yoga therapy in caring for the ill client. When the practices of exercise, breathing, meditation, and ethical principles are rooted in yoga’s philosophical underpinnings and given within the proposed explanatory framework, they form a path toward meaning, purpose, and eudaimonic well-being. It has been found that such an integrated yoga practice, had a greater effect on anxiety-related symptoms and salivary cortisol than physical postures (asana) alone [46].
According to our integrative medicine physician co-author (NF), the positive experiences reported by patients using mind-body therapies, such as yoga, may be explained by yoga’s influence on the vagus nerve, a component of the autonomic nervous system. During yoga practice vagal dominance occurs and there is a positive effect on autonomic regulation [34]. The interface between brain, immune system and inflammation is termed the classic inflammatory reflex [47]. The efferent response of this reflex is determined by activation of the vagus nerve. Vagal nerve activation leads to an acytelcholine receptor facilitated response in the spleen with subsequent inhibition of release of pro-inflammatory cytokines, such as TNF-alpha and IL-17. This vagal mediated response is in fact termed the cholinergic anti-inflammatory pathway. Impairment of this pathway has been proposed as a possible mechanism for systemic inflammation in chronic autoimmune conditions [48]. Studies have reported impaired vagus nerve activity in several rheumatological conditions, including SLE [49, 50].
4.1. Proposed modifications to the yoga series
Feedback from participants and yoga teachers for adapting the yoga intervention included offering vigorous paced (vinyasa flow) yoga classes for future SLE cohorts. Additional suggestions included starting each class supine, with meditation to cultivate body awareness and assess energy levels and teaching ‘cooling’ breaths. Restorative poses and deep breathing could be taught in every class to use as ‘gentle’ practice options when needed. Extending the class duration to 90 minutes would accommodate requests for holding some poses longer and slower transitions for going deeper into certain poses while maintaining an overall vinyasa-type flow. Next steps should include a Delphi study to solicit feedback from national and international yoga experts related to adapting the 16 class yoga series for persons living with SLE. The practicality of suggested changes should then be pilot tested by a cohort living with SLE before progressing to an RCT.
4.2. Potential changes to the study design
While yoga is adaptable, its multi-dimensional aspects make it challenging to draw comparisons across studies. For future studies it is recommended to use an objective tool such as the Essential Properties of Yoga Questionnaire, developed to allow researchers to link specific yoga components to health benefits [51]. Components of future yoga interventions that require further testing include capturing yoga dosage (count of classes, quality and duration home practice); possibly using an objective measure of physical activity (i.e. Fitbit).
Additional concepts to be tested include creating a study design that considers the frequency of flares and adaptability of classes with mixed ability. This would include adapting yoga classes for participants requiring different levels of yoga based upon body changes related to living with SLE. Levels of intensity could include:
high (vinyasa)
middle (gentle asana)
low (restoratives)
It is recommended for the yoga instructor to have a minimum training as a yoga therapist with prior experience with lupus, along with one assistant to help with positioning during restorative poses. Research is needed regarding methods to capture data for those experiencing too much pain or fatigue to attend class but able to practice yogic breathing, meditation, and restoratives at home. With the additional organ involvement associated with SLE, future studies may need to determine appropriate exclusions for some comorbidities.
5. CONCLUSION
Unlike RA and OA, SLE is systemic and associated with generalized body pain and most importantly, fatigue. In general, those living with lupus tend to be younger with a wider range of mobility. When feeling better they may prefer more rigor than during a flare. Our study offers further preliminary evidence that yoga appears to be a safe and adaptable to the needs of individuals with lupus. While those providing feedback during our study may have been a randomly more functional group, enrolling patients with SLE onto the study provided clarity on revisions to capture relevant information for the intake questionnaire. Additionally, interviewing yoga instructors with SLE gave clarity on possible adaptations to the current Yoga for Arthritis series.
Highlights.
Perspectives from those living with systemic lupus erythematosus (SLE), and researcher and clinician insights on a research population with SLE
Results from an adjunct study to the Yoga as Self Care for Arthritis in Minority Communities study for osteoarthritis and rheumatoid arthritis
Enrolling patients living with SLE clarified questionnaire revisions and lupus symptoms that could impact yoga class participation
Yoga instructors living with lupus highlighted yoga series modifications related to energy levels and frequent physical ability changes
This preliminary work affirms the feasibility of progressing to a larger study design
Acknowledgements –
The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). The authors wish to thank all study participants and yoga instructors who supported this research.
Funding source – All funding for this study is provided by the National Institutes of Health Clinical Center Intramural Research Program.
List of abbreviations
- SLE
systemic lupus erythematosus
- CAM
complementary and alternative medicine
- CIH
complementary and integrative health
- OA
osteoarthritis
- RA
rheumatoid arthritis
- NIAMS
National Institute of Arthritis and Musculoskeletal & Skin Disease
- CHC
community health clinic
- DC
District of Columbia
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- PI
principal investigator
- IRB
institutional review board
- NIH
National Institutes of Health
- BMI
body mass index
- RCT
randomized controlled trial
Footnotes
Trial Registration: ClinicalTrials.gov: NCT01617421
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kimberly R. Middleton, National Institutes of Health (NIH), Clinical Center, Nursing Research and Translational Science, 10 Center Drive, Room 2B-01, Bethesda, MD 20892, Phone: 301-496-9083, middletonk@cc.nih.gov.
Steffany Haaz Moonaz, Maryland University of Integrative Health, smoonaz@muih.edu.
Sarfaraz A. Hasni, National Institute of Arthritis and Musculoskeletal and Skin, Disease (NIAMS)/Staff Clinician, Bethesda, MD 20892, hasnisa@mail.nih.gov
Miriam Magaña López, UC Berkeley School of Public Health, Berkeley, CA 94720, miriam_magana@berkeley.edu.
Gladys Tataw-Ayuketah, NIH - Clinical Manager/Metabolic Program of Care, Tatawayuketahg@mail.nih.gov.
Nicole Farmer, NIH Clinical Center, nicole.farmer@nih.gov.
Gwenyth Wallen, NIH CC Nursing Department, NIH, Clinical Center, gwallen@cc.nih.gov.
References:
- 1.Ginzler E and Tayar J Systemic Lupus Erythematosus (Lupus). 2013. [cited 2018 February 6]; Available from: https://www.rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Systemic_Lupus_Erythematosus_(Lupus)/.
- 2.Frieri M, Mechanisms of disease for the clinician: systemic lupus erythematosus. Ann Allergy Asthma Immunol, 2013. 110(4): p. 228–32. [DOI] [PubMed] [Google Scholar]
- 3.Gurevitz SL, et al. , Systemic lupus erythematosus: a review of the disease and treatment options. Consult Pharm, 2013. 28(2): p. 110–21. [DOI] [PubMed] [Google Scholar]
- 4.Kiriakidou M, et al. , Systemic lupus erythematosus. Ann Intern Med, 2013. 159(7): p. Itc4–1. [DOI] [PubMed] [Google Scholar]
- 5.Lam NC, Ghetu MV, and Bieniek ML, Systemic Lupus Erythematosus: Primary Care Approach to Diagnosis and Management. Am Fam Physician, 2016. 94(4): p. 28494. [PubMed] [Google Scholar]
- 6.Tsokos GC, Systemic lupus erythematosus. N Engl J Med, 2011. 365(22): p. 2110–21. [DOI] [PubMed] [Google Scholar]
- 7.Ginzler E.a.T., Jean, Lupus, Rheumatology A.C.o., Editor. 2013. [Google Scholar]
- 8.Lau CS, Yin G, and Mok MY, Ethnic and geographical differences in systemic lupus erythematosus: an overview. Lupus, 2006. 15(11): p. 715–719. [DOI] [PubMed] [Google Scholar]
- 9.Pons-Estel GJ, et al. , Understanding the Epidemiology and Progression of Systemic Lupus Erythematosus. Seminars in Arthritis and Rheumatism, 2010. 39(4): p. 257–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward MM, Pyun E, and Studenski S, Long-term survival in systemic lupus erythematosus. Patient characteristics associated with poorer outcomes. Arthritis Rheum, 1995. 38(2): p. 274–83. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Lupus Detailed Fact Sheet. 2018. [cited 2018 February 6]; Available from: https://www.cdc.gov/lupus/facts/detailed.html#previnc.
- 12.Helmick CG, et al. , Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum, 2008. 58(1): p. 15–25. [DOI] [PubMed] [Google Scholar]
- 13.Rus V, Hajeer A, and Hochberg MC, Epidemiology of the Rheumatic Disease, in Systemic lupus erythematosus, Silman AJ HM, Editor. 2001, Oxford University Press: New York. [Google Scholar]
- 14.McCarty DJ, et al. , Incidence of systemic lupus erythematosus race and gender differences. Arthritis & Rheumatism, 1995. 38(9): p. 1260–1270. [DOI] [PubMed] [Google Scholar]
- 15.Nikpour M, et al. , Frequency and determinants of flare and persistently active disease in systemic lupus erythematosus. Arthritis Care & Research, 2009. 61(9): p. 1152–1158. [DOI] [PubMed] [Google Scholar]
- 16.National Institute of Arthritis and Musculosketal and Skin Diseases (NIAMS). Systemic Lupus Erythematosus (Lupus) 2016. [cited 2018 February ]; Available from: http://www.niams.nih.gov/Health_Info/Lupus/lupus_ff.asp.
- 17.Schmeding A and Schneider M, Fatigue, health-related quality of life and other patient-reported outcomes in systemic lupus erythematosus. Best Practice & Research Clinical Rheumatology, 2013. 27(3): p. 363–375. [DOI] [PubMed] [Google Scholar]
- 18.van Vollenhoven RF, et al. , Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Annals of the Rheumatic Diseases, 2014. 73(6): p. 958–967. [DOI] [PubMed] [Google Scholar]
- 19.Robb-Nicholson LC, et al. , Effects of aerobic conditioning in lupus fatigue: a pilot study. Br J Rheumatol, 1989. 28(6): p. 500–5. [DOI] [PubMed] [Google Scholar]
- 20.Carvalho MR, et al. , Effects of supervised cardiovascular training program on exercise tolerance, aerobic capacity, and quality of life in patients with systemic lupus erythematosus. Arthritis Rheum, 2005. 53(6): p. 838–44. [DOI] [PubMed] [Google Scholar]
- 21.Daltroy LH, et al. , Effectiveness of minimally supervised home aerobic training in patients with systemic rheumatic disease. Br J Rheumatol, 1995. 34(11): p. 1064–9. [DOI] [PubMed] [Google Scholar]
- 22.Ramsey-Goldman R, et al. , A pilot study on the effects of exercise in patients with systemic lupus erythematosus. Arthritis Care Res, 2000. 13(5): p. 262–9. [DOI] [PubMed] [Google Scholar]
- 23.Tench CM, et al. , Fatigue in systemic lupus erythematosus: a randomized controlled trial of exercise. Rheumatology (Oxford), 2003. 42(9): p. 1050–4. [DOI] [PubMed] [Google Scholar]
- 24.Yuen HK and Cunningham MA, Optimal management of fatigue in patients with systemic lupus erythematosus: a systematic review. Ther Clin Risk Manag, 2014. 10: p. 775–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haija AJ and Schulz SW, The Role and Effect of Complementary and Alternative Medicine in Systemic Lupus Erythematosus. Rheumatic Disease Clinics of North America, 2011. 37(1): p. 47–62. [DOI] [PubMed] [Google Scholar]
- 26.Moonaz SH, et al. , Yoga in Sedentary Adults with Arthritis: Effects of a Randomized Controlled Pragmatic Trial. The Journal of Rheumatology, 2015. 42(7): p. 1194–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mill C, et al. , Yoga in Systemic Lupus Erythematosus: Qualitative Results of a Pragmatic Pilot Trial. Journal of Rheumatology, 2013. 40(6): p. 963–963. [Google Scholar]
- 28.Bartlett SJ, et al. , Yoga in rheumatic diseases. Curr Rheumatol Rep, 2013. 15(12): p. 387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woodyard C, Exploring the therapeutic effects of yoga and its ability to increase quality of life. International Journal of Yoga, 2011. 4(2): p. 49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan MB, et al. , Yoga Therapy and Polyvagal Theory: The Convergence of Traditional Wisdom and Contemporary Neuroscience for Self-Regulation and Resilience. Frontiers in Human Neuroscience, 2018. 12(67). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Streeter CC, et al. , Effects of yoga on the autonomic nervous system, gammaaminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses, 2012. 78(5): p. 571–9. [DOI] [PubMed] [Google Scholar]
- 32.Toschi-Dias E, et al. , Sudarshan Kriya Yoga improves cardiac autonomic control in patients with anxiety-depression disorders. J Affect Disord, 2017. 214: p. 74–80. [DOI] [PubMed] [Google Scholar]
- 33.Telles S, et al. , Heart rate variability in chronic low back pain patients randomized to yoga or standard care. BMC Complement Altern Med, 2016. 16(1): p. 279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyagi A and Cohen M, Yoga and heart rate variability: A comprehensive review of the literature. Int J Yoga, 2016. 9(2): p. 97–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khattab K, et al. , Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evid Based Complement Alternat Med, 2007. 4(4): p. 511–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarang P and Telles S, Effects of two yoga based relaxation techniques on heart rate variability (HRV). International Journal of Stress Management, 2006. 13(4): p. 460–475. [Google Scholar]
- 37.Editors Y Yoga and Lupus. Yoga Journal 2012. [cited 2018 July]; Available from: https://www.yogajournal.com/lifestyle/yoga-and-lupus.
- 38.Bell B Lupus Solution. Yoga Journal 2007. [cited 2018 July]; Available from: https://www.yogajournal.com/practice/lupus-solution.
- 39.Middleton KR, et al. , A pilot study of yoga as self-care for arthritis in minority communities. Health Qual Life Outcomes, 2013. 11(55). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beckerman NL, Auerbach C, and Blanco I, Psychosocial dimensions of SLE: implications for the health care team. J Multidiscip Healthc, 2011. 4: p. 63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rinaldi S, et al. , Influence of coping skills on health-related quality of life in patients with systemic lupus erythematosus. Arthritis Rheum, 2006. 55(3): p. 427–33. [DOI] [PubMed] [Google Scholar]
- 42.Mcelhone K, Abbott J, and Teh L-S, A review of health related quality of life in systemic lupus erythematosus. Lupus, 2006. 15(10): p. 633–643. [DOI] [PubMed] [Google Scholar]
- 43.Middleton KR, et al. , A qualitative approach exploring the acceptability of yoga for minorities living with arthritis: ‘Where are the people who look like me?’. Complement Ther Med, 2017. 31: p. 82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Middleton KR, et al. , Feasibility and assessment of outcome measures for yoga as selfcare for minorities with arthritis: a pilot study. Pilot and Feasibility Studies, 2018. 4(1): p. 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ryan GW and Bernard HR, Techniques to Identify Themes. Field Methods, 2003. 15(1): p. 85–109. [Google Scholar]
- 46.Sullivan MB, et al. , Toward an Explanatory Framework for Yoga Therapy Informed by Philosophical and Ethical Perspectives. Altern Ther Health Med, 2018. 24(1): p. 38–47. [PubMed] [Google Scholar]
- 47.Tracey KJ, The inflammatory reflex. Nature, 2002. 420(6917): p. 853–9. [DOI] [PubMed] [Google Scholar]
- 48.Mathis KW, An impaired neuroimmune pathway promotes the development of hypertension in systemic lupus erythematosus. Am J Physiol Regul Integr Comp Physiol, 2015. 309(9): p. R1074–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lagana B, et al. , Heart rate variability and cardiac autonomic function in systemic lupus erythematosus. Lupus, 1996. 5(1): p. 49–55. [DOI] [PubMed] [Google Scholar]
- 50.Koopman FA, et al. , Restoring the balance of the autonomic nervous system as an innovative approach to the treatment of rheumatoid arthritis. Mol Med, 2011. 17(9–10): p. 937–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Groessl EJ, et al. , The Essential Properties of Yoga Questionnaire: Development and Methods. Int J Yoga Therap, 2015. 25(1): p. 51–9. [DOI] [PMC free article] [PubMed] [Google Scholar]