Abstract
Background: Approximately 10% to 15% of lung cancer cases in the United States occur in never smokers, but there has been much debate about whether this rate is increasing. To determine whether the proportion of never smokers among lung cancer cases is increasing, we conducted a retrospective study using registries from The University of Texas Southwestern Medical Center, Parkland Hospital, and Vanderbilt University.
Methods: Registries were queried for demographic information from 1990 to 2013 including sex, age, stage, and self-reported smoking history. Ten thousand five hundred ninety-three non–small cell lung cancer (NSCLC) case patients and 1510 small cell lung cancer (SCLC) case patients were captured, and logistic regression analysis was performed. All statistical tests were two-sided.
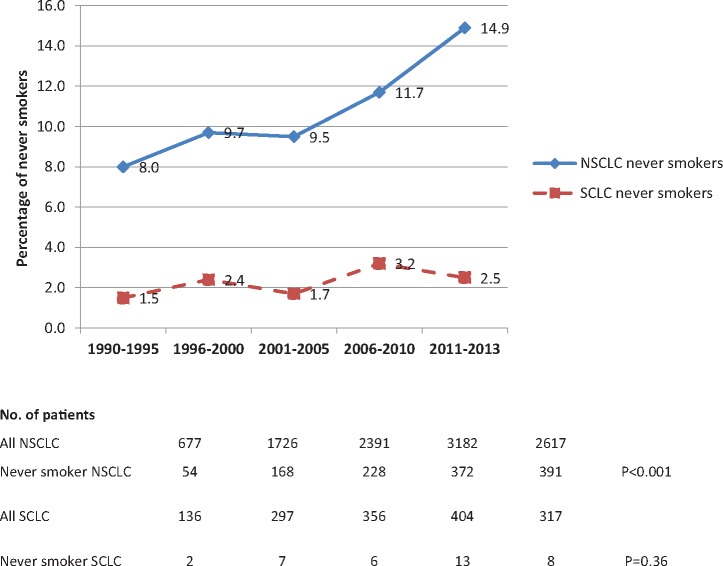
Results: The proportion of never-smoker NSCLC patients increased from 8.0% in the years 1990 to 1995 to 14.9% in 2011 to 2013 (P < .001). This increase was also observed using multivariable logistic regression after controlling for sex, stage at diagnosis, and race/ethnicity. The percentage of never smokers among SCLC case patients (1.5% in 1990–1995 to 2.5% in 2011–2013, P = .36) or squamous cell NSCLC case patients did not statistically significantly change during this period.
Conclusions: This study demonstrates an increasing proportion of NSCLC patients who have never smoked in a large, diverse patient population between 1990 and 2013. Given that this increase appears independent of sex, stage, and race/ethnicity and also occurred in our county hospital, this trend is unlikely due to changes in referral patterns and suggests that the actual incidence of lung cancer in never smokers is increasing.
Lung cancer is the second most common cancer and the leading cause of cancer-related mortality in the United States, with an estimated 224 390 new cases and 158 000 deaths anticipated in the United States in 2016 (1). An estimated 10% to 15% of lung cancer cases in the United States occur in never smokers (2). Lung cancer in never smokers has been associated with East Asian descent, female sex, and adenocarcinoma histology (3). The cause of lung cancer in these patients includes many possible factors such as exposure to secondhand smoke, radon, air pollution, cooking oil, etc. (4), but the precise cause in an individual case is often uncertain. Additionally, there has been much debate about whether the incidence of lung cancer in never smokers is increasing. This question has been difficult to address because of poorly recorded smoking histories in the past and accurately identifying the number of never smokers with lung cancer and total number of never smokers in a given population. Using cancer registry data from our three institutions, our objective was to test our hypothesis that the proportion of never smokers with lung cancer relative to smokers with lung cancer is increasing.
Methods
Database Queries
We conducted a retrospective study using lung cancer registry data from The University of Texas (UT) Southwestern Medical Center in Dallas (which includes both our private patient facilities and our large county charity care hospital Parkland Hospital/Health Care System in Dallas) and Vanderbilt University in Nashville. These registries were queried between 1990 and 2013 to identify and obtain information on all lung cancer patients registered, including diagnosis (NSCLC or SCLC), histology, stage at diagnosis, sex, age at diagnosis, race/ethnicity, and self-reported smoking history. These three institutions are all large centers for which registry data was available. UT Southwestern and Vanderbilt University hospitals are largely insured patient populations, whereas Parkland Hospital is a county charity care hospital where the patients are primarily under- or uninsured. The definition of never smoker in the registries was whether or not a patient had ever smoked and was answered by the patient as a “yes or no” question.
Statistical Analysis
Logistic regression analysis was performed to assess the association between never smokers with lung cancer and risk factors including sex, stage, and race/ethnicity. Exact Cochran-Armitage trend test was used to investigate if the proportion of never-smoker lung cancer patients increases over the years. Student's t tests were used to compare age between smokers and nonsmokers, and chi-square tests were used to compare sex between smokers and nonsmokers. Statistical significance cutoff was set at a P value of .05 or less. All statistical tests were two-sided. Proportion of never smokers with lung cancer was calculated as the number of lung cancer patients who self-reported as never smokers divided by the total number of lung cancer cases.
Results
Total Patients
A total of 10 593 NSCLC and 1510 SCLC case patients were identified: 3300 from UTSW (2900 NSCLC and 400 SCLC), 2915 from Parkland (2517 NSCLC and 398 SCLC), and 5888 from Vanderbilt (5176 NSCLC and 712 SCLC). The sex distribution of the NSCLC patients is shown in Table 1.
Table 1.
Non–small cell lung cancer patients by institution and sex during the 1990–2013 time periods
| Time period | University of Texas Southwestern, No |
Parkland, No. |
Vanderbilt, No. |
|||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| 1990–1995 | 315 | 226 | 13 | 18 | 84 | 21 |
| 1996–2000 | 214 | 200 | 313 | 209 | 506 | 284 |
| 2001–2005 | 285 | 238 | 386 | 271 | 710 | 501 |
| 2006–2010 | 371 | 353 | 427 | 322 | 985 | 724 |
| 2011–2013 | 354 | 344 | 310 | 248 | 761 | 600 |
Proportion of Lung Cancer Patients Who Have Never Smoked Among the Total Lung Cancer Population
As demonstrated in Figure 1, exact Cochran-Armitage trend test demonstrates an increasing percentage of never smokers with lung cancer among all NSCLC case patients from 8.0% in the years 1990 to 1995 to 14.9% in 2011 to 2013 (P < .001). By contrast, there was no statistically significant increase in never smokers among the population diagnosed histologically as SCLC during this time period (1.5% to 2.5%, respectively, P = .36). This trend was observed among all three institutions (Table 2). Because the captured case patients between 1990 and 1995 were relatively low compared with the other time periods, we re-analyzed the data excluding the 1990 to 1995 time period and observed no change in the trend (Exact Cochran-Armitage trend test P values were P < .001 for NSCLC and P = .55 for SCLC, respectively).
Figure 1.
Proportion of never-smoker non–small cell lung cancer (NSCLC) patients. The graph shows the proportion of never smokers among NSCLC patients over the time period. The table gives the numbers of NSCLC and SCLC patients for each five-year time period. P values were calculated using a two-sided exact Cochran-Armitage trend test. NSCLC = non–small cell lung cancer; SCLC = small cell lung cancer.
Table 2.
Percentage of never smokers among NSCLC and SCLC by institution over the time periods
| Time period | University of Texas Southwestern, % |
Parkland, % |
Vanderbilt, % |
|||
|---|---|---|---|---|---|---|
| NSCLC | SCLC | NSCLC | SCLC | NSCLC | SCLC | |
| 1990–1995 | 8.9 | 1.7 | 12.9 | 0.0 | 1.9 | – |
| 1996–2000 | 9.4 | 1.4 | 8.2 | 2.8 | 10.9 | 2.5 |
| 2001–2005 | 9.9 | 0 | 7.6 | 2.8 | 10.4 | 2.3 |
| 2006–2010 | 13.8 | 7.0 | 12.1 | 2.9 | 10.6 | 2.2 |
| 2011–2013 | 19.5 | 4.5 | 14.2 | 1.3 | 12.9 | 2.3 |
| P * | <.001 | .11 | <.001 | .61 | .008 | .89 |
Two-sided P value from exact Cochran-Armitage trend test. The endash indicates no case patients recorded during that period. NSCLC = non–small cell lung cancer; SCLC = small cell lung cancer.
Sex and Age of Never Smokers With NSCLC
Men had a statistically significantly higher rate of smoking than women among NSCLC patients (93.1% compared with 82.5%. P < .001) (Table 3). Never smokers with NSCLC were more likely to be female 17.5% vs 6.9% male (P < .001) (Table 3). The number of never-smoker women with NSCLC increased from 10.2% to 22.1% (P < .001) and increased in men from 6.6% to 8.9% (P = .006) between 1990 and 2013 (data not shown). Never smokers with NSCLC were slightly younger than their smoking counterparts (60.6 +/- 16.7 years vs 63.4 +/- 12.9 years, P < .001) but there was no statistically significant difference in age for the SCLC patients (Table 3).
Table 3.
Age and sex of never smokers vs smokers at all three institutions
| Demographic | Smokers (n = 10 854 total NSCLC + SCLC) | Never smokers (n = 1249 total NSCLC + SCLC) | P* |
|---|---|---|---|
| Age, mean (SD), y | |||
| NSCLC | 63.4 (12.9) | 60.6 (16.7) | <.001 |
| SCLC | 61.7 (12.2) | 63.3 (14.7) | .44 |
| Sex, No. (% of NSCLC cases) | |||
| Female | 3761 (82.5) | 798 (17.5) | <.001 |
| Male | 5619 (93.1) | 415 (6.9) | |
Two-sided P value from Student’s t test for age and from chi-square test for sex. NSCLC = non–small cell lung cancer; SCLC = small cell lung cancer.
Stage of Diagnosis of Never Smokers With NSCLC
Though the magnitude of the increase over time suggests otherwise, to examine the possibility that the increasing numbers of never smokers among the NSCLC population was potentially due to the earlier or incidental diagnosis of early-stage or potentially “indolent disease,” we examined stage at diagnosis (Table 4). There was no statistically significant difference in the rates of nonmetastatic (stage I–III) disease at presentation over the years among NSCLC nonsmoking patients at UTSW (P = 1.00), Parkland (P = .42), or Vanderbilt (P = .28) by Exact Cochran-Armitage trend test. At Vanderbilt, there was a statistically significant decrease in stage III patients (P = .002) (data not shown), but this did not affect the overall proportion of stage I–III or the number of patients with stage IV disease.
Table 4.
Never smokers and stage: Absolute numbers and percentage of never smoker patients with nonmetastatic (stage I–III) NSCLC*
| Institution and time period | Total No. of never-smoking NSCLC patients | No. of never- smoking NSCLC patients with nonmetastatic (stage I–III) disease | % of never-smoking NSCLC patients with nonmetastatic (stage I–III) disease (95% CI)† |
|---|---|---|---|
| UTSW | |||
| 1990–1995 | 40 | 21 | 52.5 (36.13 to 68.49) |
| 1996–2000 | 29 | 15 | 51.7 (32.53 to 70.55) |
| 2001–2005 | 40 | 16 | 40.0 (24.86 to 56.67) |
| 2006–2010 | 84 | 48 | 57.1 (45.88 to 67.89) |
| 2011–2013 | 131 | 65 | 49.6 (40.77 to 58.48) |
| P‡ | 1.00 | ||
| Parkland | |||
| 1990–1995 | 4 | 3 | 75.0 (19.41 to 99.37) |
| 1996–2000 | 33 | 14 | 42.4 (25.48 to 60.78) |
| 2001–2005 | 43 | 15 | 34.9 (21.01 to 50.93) |
| 2006–2010 | 77 | 30 | 39.0 (28.05 to 50.75) |
| 2011–2013 | 68 | 25 | 36.8 (25.39 to 49.33) |
| P‡ | .42 | ||
| Vanderbilt | |||
| 1990–1995 | 0 | 0 | |
| 1996–2000 | 66 | 40 | 60.6 (47.81 to 72.42) |
| 2001–2005 | 90 | 45 | 50.0 (39.27 to 60.73) |
| 2006–2010 | 128 | 66 | 51.6 (42.57 to 60.48) |
| 2011–2013 | 128 | 64 | 50.0 (41.04 to 58.96) |
| P‡ | .28 | ||
The data are represented as the percentage of never-smoking non–small cell lung cancer (NSCLC) patients with nonmetastatic (stages I, II, and III combined) disease over the time periods. A change in nonmetastatic disease would indicate a corresponding change in metastatic (stage IV) disease. Of note, the absolute numbers of patients in this table do not necessarily add up to the overall totals of the study because while all patients counted in the study had smoking status documented, not all patients’ stage data were documented in the registries. CI = confidence interval; NSCLC = non–small cell lung cancer; UTSW = University of Texas Southwestern.
95% confidence interval is calculated using an exact binomial method.
Two-sided P value from exact Cochran-Armitage trend test.
Race/Ethnicity of Never Smokers Among the NSCLC Population
Asia has a higher rate of never-smoker lung cancer patients and more than 50% of Asian female patients are never smokers (5). NSCLC tumors in Asian and, based on some reports, Hispanic patients, have increased rates of particular genetic aberrations such as activating epidermal growth factor receptor (EGFR) mutations (6–8). Because such aberrations have not been routinely captured in our databases until very recently, to assess the possibility that the observed increase in never smokers among the NSCLC population during this period was just because of increased numbers of patients seeking clinical trials for EGFR and ALK-directed therapies, we examined race/ethnicity as a surrogate for mutation status with a focus on Asian and Hispanic patients. As demonstrated in Table 5, there was a statistically significant increase in the proportion of Asians over the years among all NSCLC patients at UTSW (P < .001) and Parkland (P = .001). Additionally, there was a statistically significant increase in the proportion of Hispanic patients over the years among all NSCLC patients at Parkland (P < .001) and Vanderbilt (P = .04). The numbers of Hispanic patients at UTSW and Asian patients at Vanderbilt were relatively low and did not statistically significantly change during this period. However, after controlling for race/ethnicity, there is still an increasing proportion of never smokers among the NSCLC population at UTSW (P < .001), Parkland (P = .03), Vanderbilt (P = .001), and for all three institutions combined (P < .001) (Supplementary Table 1, available online).
Table 5.
Asian and Hispanic patients among NSCLC patients at each of the three institutions as a surrogate for EGFR mutation status*
| Time period | UTSW |
Parkland |
Vanderbilt |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total No. of NSCLC patients | No. of Asian patients (%) | No. of Hispanic patients (%) | Total No. of NSCLC patients | No. of Asian patients (%) | No. of Hispanic patients (%) | Total No. of NSCLC patients | No. of Asian patients (%) | No. of Hispanic patients (%) | |
| 1990–1995 | 539 | 4 (0.7) | 17 (3.2) | 31 | 0 (0.0) | 1 (3.2) | 116 | 0 (0.0) | 0 (0.0) |
| 1996–2000 | 413 | 4 (1.0) | 13 (3.2) | 522 | 12 (2.3) | 51 (9.8) | 784 | 0 (0.0) | 2 (0.3) |
| 2001–2005 | 522 | 13 (2.5) | 25 (4.8) | 657 | 19 (2.9) | 86 (13.1) | 1199 | 3 (0.3) | 2 (0.2) |
| 2006–2010 | 723 | 18 (2.5) | 29 (4.0) | 749 | 27 (3.6) | 113 (15.1) | 1694 | 4 (0.2) | 9 (0.5) |
| 2011–2013 | 696 | 32 (4.6) | 25 (3.6) | 558 | 32 (5.7) | 105 (18.8) | 1355 | 6 (0.4) | 9 (0.7) |
| P† | <.001 | .59 | .001 | <.001 | .07 | .04 | |||
The absolute numbers of patients in this table do not necessarily add up to the overall totals of the study because while all patients counted in the study had smoking status documented, not all patients’ race/ethnicity data were documented in the registries. EGFR = epidermal growth factor receptor; NSCLC = non–small cell lung cancer; UTSW = University of Texas Southwestern.
Two-sided P value from exact Cochran-Armitage trend test.
Histology of Never Smokers With NSCLC
The number of never smokers with squamous histology was small (13 or fewer per five-year reporting time period per institution) (Table 6). Exact Cochran-Armitage trend test shows there was no statistically significant difference in the proportion of histology (nonsquamous vs squamous) over the years among NSCLC nonsmoking patients at UTSW (P = .64), Parkland (P = .15), or Vanderbilt (P = .11) (Table 6).
Table 6.
Histology in never smokers with non–small cell lung cancer*
| Time period | UTSW |
Parkland |
Vanderbilt |
|||
|---|---|---|---|---|---|---|
| Total No.of never-smoking NSCLC patients | No. of nonsquamous patients (%) | Total No.of never-smoking NSCLC patients | No. of nonsquamous patients (%) | Total No. of never-smoking NSCLC patients | No. of nonsquamous patients (%) | |
| 1990–1995 | 48 | 45 (93.8) | 2 | 2 (100.0) | 2 | 2 (100.0) |
| 1996–2000 | 39 | 38 (97.4) | 38 | 32 (84.2) | 68 | 59 (86.8) |
| 2001–2005 | 52 | 51 (98.1) | 32 | 27 (84.4) | 85 | 78 (91.8) |
| 2006–2010 | 100 | 90 (90.0) | 71 | 64 (90.1) | 141 | 128 (90.8) |
| 2011–2013 | 136 | 129 (94.9) | 62 | 58 (93.6) | 159 | 150 (94.3) |
| P† | .64 | .15 | .11 | |||
Absolute numbers and percentages of nonsquamous vs squamous histology in never smokers with non–small cell lung cancer (NSCLC). Of note, the absolute numbers of patients in this table do not necessarily add up to the overall totals of the study (Figure 1) because while all patients counted in the study had smoking status documented, not all patients’ subtype of NSCLC were documented in the registries. NSCLC = non–small cell lung cancer; UTSW = University of Texas Southwestern.
Two-sided P value from exact Cochran-Armitage trend test.
The number of never smokers with small cell histology was also small (Figure 1) and remained stable over time (P = .36). When we re-analyzed the data including unknown smoking status in the denominator, a trend toward an increase in the number of never smokers with small cell histology was observed (P = .03), but when the years 1990 to 1995 were also excluded (see above), no such trend was observed (P = .45).
Discussion
This multi-institution study demonstrates an increasing proportion of never smokers with NSCLC between 1990 and 2013 in a large, geographically and demographically diverse population. This increase was independent of sex, stage, or race/ethnicity.
A limitation of our study is that we measured the proportion of never smokers among lung cancer case patients over time and not incidence. We were unable to measure incidence because we do not have the total patients seen at these hospitals with their smoking statuses. However, that this increased proportion was independent of sex, stage at diagnosis, and race/ethnicity and did not occur in small cell lung cancer patients or squamous cell lung cancer patients suggests that the incidence of lung cancer cases in never smokers is increasing.
Other limitations of our study include our databases’ use of patient-reported smoking history as opposed to a more objective smoking status ascertainment using biochemical tests. However, we note the fact that rate of never smokers with SCLC remained relatively constant throughout the time period of our analysis and served as an internal control of smoking history in our databases. Additionally, race/ethnicity data was not necessarily self-reported. Also, we used race/ethnicity as a surrogate for molecular status (eg, EGFR mutation status) because these data were not available. The analyses of the subgroups by race/ethnicity, stage, etc., were descriptive and exploratory in nature. Because their numbers were too small, power calculations were not performed.
Whether or not the incidence of never smokers with NSCLC is increasing has been debated over the years, with some reports suggesting there has been an increase in rates and/or deaths from NSCLC in never smokers (9,10) and others suggesting that such rates have not been increasing (11,12). Our data from three demographically diverse institutions (one of which is a large county hospital for the uninsured and underinsured) demonstrates an increase in the proportion of never smokers among the NSCLC population that is not explained by any increase in earlier diagnoses of clinically indolent disease. Additionally, this trend is likely not due to changes in referral patterns resulting in a disproportionate number of never smokers coming to Parkland, UT Southwestern, and Vanderbilt for early-phase clinical trials of targeted therapies because there was still an increasing proportion of never smokers among the NSCLC population, even after controlling for race/ethnicity (a surrogate for mutation status). Additionally, Parkland is a county “safety net” hospital, and not a referral hospital. While lung cancer clinical trials are conducted at Parkland, it does not have the large clinical trial portfolios of the other two institutions’ university hospital systems, and patients are unlikely to be referred there for new and innovative therapies.
Interestingly, a group in London recently reported data in abstract form that demonstrates an increasing incidence of never smokers diagnosed with NSCLC at a tertiary care hospital in the United Kingdom between 2008 and 2014. In that study, the rate of never smokers with early-stage lung cancer increased from 13% to 28% over the time period (13).
We reached different conclusions than Thun et al., who found that “these comprehensive analyses…contradict assertions that risk is increasing or that women have a higher incidence rate than men” (12). It is difficult to compare different studies directly, and the conclusions regarding temporal trends in Samet et al. and Thun et al. are largely based on data from Cancer Prevention Study I and II covering 1959 to 1972 and 1982 to 2000, respectively, and may not apply to more recent trends. Indeed, based on our data, the steepest rate of increase occurred after 2000 (Figure 1). If in fact the incidence of lung cancer in the never-smoking population is on the rise, it will be very important to identify environmental risk factors that play a role in the etiology of never-smoking lung cancer. Environmental risk factors will need to be integrated with detailed mutational characterization of such tumors to provide new insights as to the reasons behind this rising incidence (14–16). In fact, Samet et al. concluded from their study (related to the Thun et al. study) that “a large fraction of lung cancers occurring in never smokers cannot be definitively associated with established environmental risk factors, highlighting the need for additional epidemiologic research in this area” (11). We demonstrated that the proportion of lung cancer patients who reported themselves as “never smokers” is increasing at three diverse institutions. Given that this increase is not related to sex, stage, or race/ethnicity and was not seen in small cell lung cancer, these results suggest that the incidence of lung cancer arising in the never-smoking population is likely increasing. If this is verified in multiple other databases, it signals an urgent need to perform combined and integrated epidemiology and tumor molecular analyses to identify potential environmental lung cancer–causing carcinogens that will clearly impact prevention and treatment.
Funding
This work was supported in part by the Simmons Comprehensive Cancer Center (P30CA142543), Lung Cancer SPORE (P50CA70907), and the Margot Johnson Foundation.
Notes
The funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
We thank Judith Roberts, RHIT, CTR, for excellent assistance with tumor registry data.
Supplementary Material
References
- 1. Siegel RL, Miller KD, Jemal A.. Cancer statistics, 2016. CA Cancer J Clin. 2016;661:7–30. [DOI] [PubMed] [Google Scholar]
- 2. The Health Consequences of Smoking: A report of the Surgeon General. 2004. [PubMed]
- 3. Thu KL, Vucic EA, Chari R, et al. Lung adenocarcinoma of never smokers and smokers harbor differential regions of genetic alteration and exhibit different levels of genomic instability. PLoS One. 2012;73:e33003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alberg AJ, Brock MV, Ford JG, et al. Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 suppl):e1S–e29S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou W, Christiani DC.. East meets West: Ethnic differences in epidemiology and clinical behaviors of lung cancer between East Asians and Caucasians. Chin J Cancer. 2011;305:287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arrieta O, Ramirez-Tirado LA, Baez-Saldana R, et al. Different mutation profiles and clinical characteristics among Hispanic patients with non-small cell lung cancer could explain the “Hispanic paradox.” Lung Cancer. 2015;902:161–166. [DOI] [PubMed] [Google Scholar]
- 7. Shigematsu H, Lin L, Takahashi T, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;975:339–346. [DOI] [PubMed] [Google Scholar]
- 8. Zhang W, McQuitty EB, Olsen R, et al. EGFR mutations in US Hispanic versus non-Hispanic white patients with lung adenocarcinoma. Arch Pathol Lab Med. 2014;1384:543–545. [DOI] [PubMed] [Google Scholar]
- 9. Enstrom JE. Rising lung cancer mortality among nonsmokers. J Natl Cancer Inst. 1979;624:755–760. [PubMed] [Google Scholar]
- 10. Forastiere F, Perucci CA, Arca M, et al. Indirect estimates of lung cancer death rates in Italy not attributable to active smoking. Epidemiology. 1993;46:502–510. [DOI] [PubMed] [Google Scholar]
- 11. Samet JM, Avila-Tang E, Boffetta P, et al. Lung cancer in never smokers: Clinical epidemiology and environmental risk factors. Clin Cancer Res. 2009;1518:5626–5645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Thun MJ, Hannan LM, Adams-Campbell LL, et al. Lung cancer occurrence in never-smokers: An analysis of 13 cohorts and 22 cancer registry studies. PLoS Med. 2008;59:e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Proli C, Cufari ME, Phull H. et al. Increasing Incidence of Non-Smoking Lung Cancer: Presentation of Patients with Early Disease to a Tertiary Institution in the UK. 16th World Conference on Lung Cancer. 2015.
- 14. Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature. 2013;5007463:415–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Deciphering signatures of mutational processes operative in human cancer. Cell Rep. 2013;31:246–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Swanton C, McGranahan N, Starrett GJ, et al. APOBEC enzymes: Mutagenic fuel for cancer evolution and heterogeneity. Cancer Discov. 2015;57:704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.