Abstract
We report a 55-year-old female patient with refractory vasospastic angina and bronchial asthma treated successfully with corticosteroids. She was diagnosed with vasospastic angina by coronary angiography and the acetylcholine provocation test. Even after administration of oral vasodilators (benidipine, diltiazem, nicorandil, isosorbide mononitrate) she had recurrent chest pain with ST elevation. She had a history of bronchial asthma, so we added 30 mg/day of oral prednisolone. Her symptoms disappeared completely upon treatment. This case report suggests that corticosteroids are a therapeutic choice for patients with refractory vasospastic angina, especially for those with bronchial asthma.
<Learning objective: We report a 55-year-old female patient with refractory vasospastic angina and bronchial asthma. Even after administration of oral vasodilators, she had recurrent chest pain with ST elevation. She had a history of bronchial asthma, so we added 30 mg/day of oral prednisolone. Her symptoms disappeared completely upon treatment. This case report suggests that corticosteroids are a therapeutic choice for patients with refractory vasospastic angina, especially for those with bronchial asthma.>
Keywords: Vasospastic angina, Coronary spasm, Corticosteroid
Introduction
Vasospastic angina can cause not only angina pectoris but also myocardial infarction, and even sudden cardiac death with fatal arrhythmia 1, 2, 3, 4. Usually, it is controlled satisfactorily with oral vasodilators such as calcium antagonists and nitrates. However, some patients with vasospastic angina are resistant to conventional oral vasodilators. Those patients are recognized as having “refractory vasospastic angina” (RVA).
There are several treatments for RVA. Some case reports have shown the effectiveness of corticosteroids, especially in patients with allergic disease 3, 4. However, there is a paucity of data regarding the effectiveness of corticosteroids for vasospastic angina, as well as for the relationship between inflammation or allergic reactions and coronary vasospasm.
Here we describe a case of RVA with bronchial asthma treated successfully with corticosteroids in addition to oral vasodilators.
Case report
A 55-year-old female patient was referred to our hospital with a chief complaint of chest pain of 2-week duration. She complained of an increasing frequency of chest pain, especially in the morning and at rest. These findings were consistent with a diagnosis of worsening angina. She had a history of bronchial asthma, but no risk factors for coronary heart disease. She arrived at our hospital with no medication.
Physical examination findings were almost normal. Electrocardiography (ECG) and chest radiography did not reveal abnormal findings. Hematology showed a white blood cell count of 4100/μL (neutrophils, 44.9%; lymphocytes, 42.1%; monocytes, 6.6%; eosinophils, 5.9%; and basophils, 0.5%), a hemoglobin level of 13.4 g/dL, and a platelet count of 17.1 × 104/μL. Serum samples showed a negative level of troponin-T (0.006 ng/mL), slight elevation of the level of brain natriuretic peptide (BNP; 22.4 pg/mL), and a normal level of C-reactive protein (CRP; 0.15 mg/dL). Transthoracic echocardiography showed a normal size and contractility of the left ventricle. She was admitted to our hospital with a diagnosis of unstable angina.
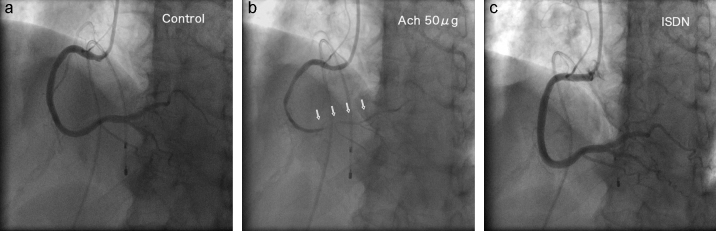
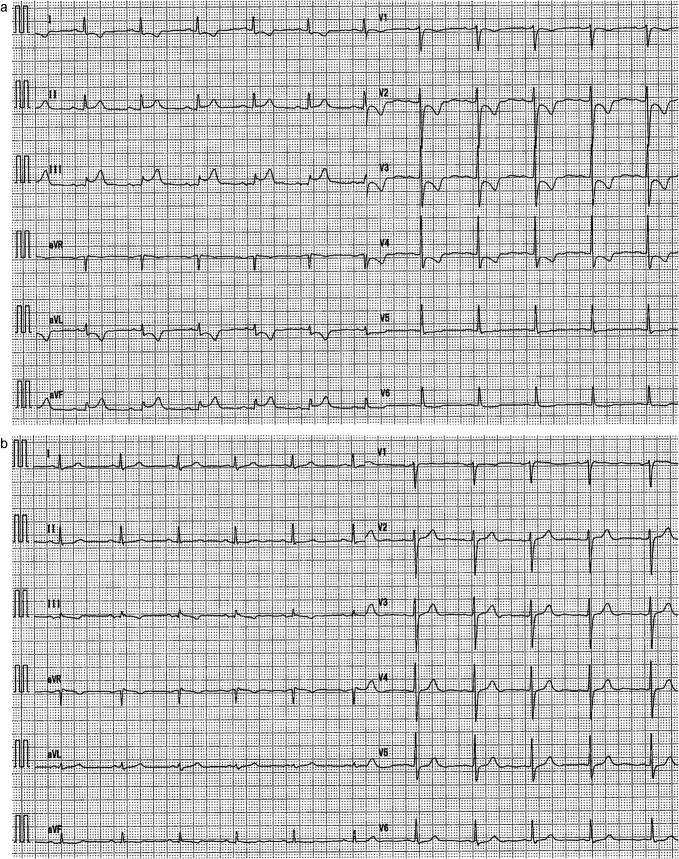
Diagnostic coronary angiography revealed no significant atherosclerotic stenosis in the coronary arteries. The acetylcholine provocation test was undertaken to investigate coronary vasospasm (Fig. 1a–c). A temporary pacemaker was inserted into the right ventricle via the right femoral vein in case of bradycardia. There was no clear evidence of severe coronary vasospasm in the left coronary artery with intracoronary infusion of acetylcholine (25, 50, and 100 μg). However, the right coronary artery was almost totally occluded upon provocation with acetylcholine (50 μg; Fig. 1b) with chest pain. ECG revealed ST elevation in leads II, III, and aVF, as well as ST depression in leads I, aVL, and V1–V4 (Fig. 2a). After intracoronary infusion of isosorbide dinitrate, coronary spasm was reversed (Fig. 1c) and the electrocardiographic changes were normalized (Fig. 2b). She was diagnosed with vasospastic angina.
Fig. 1.
Coronary angiography and the acetylcholine provocation test. Angiogram of the right coronary artery using 6-Fr Judkins right catheter (left anterior oblique and cranial view): (a) control angiogram, (b) angiogram after acetylcholine provocation (Ach), and (c) angiogram after intracoronary infusion of isosorbide dinitrate (ISDN).
Fig. 2.
Electrocardiography. (a) Electrocardiogram revealing ST elevation in leads II, III, and aVF as well as ST depression in leads I, aVL, and V1–V4 after acetylcholine provocation. (b) Electrocardiographic changes are normalized after intracoronary infusion of isosorbide dinitrate.
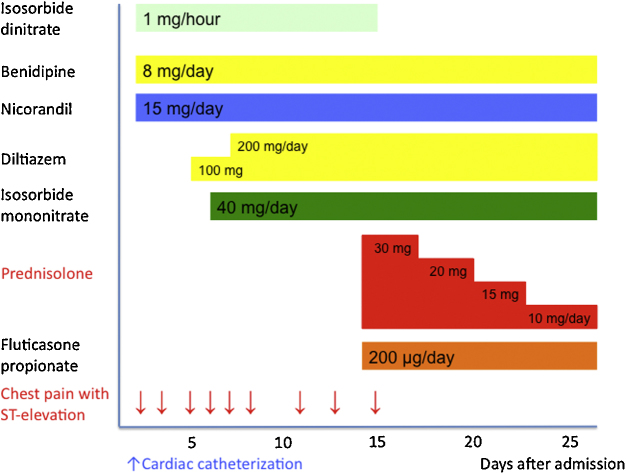
In addition to continuous intravenous administration of isosorbide dinitrate, we started oral vasodilators (8 mg/day of benidipine, 15 mg/day of nicorandil), but she had recurrent chest pain with ST elevation in leads II, III, and aVF in the morning (Fig. 3). Usually, her symptoms were relieved with sublingual nitroglycerin or a temporary bolus intravenous infusion of isosorbide dinitrate. We added 200 mg/day of diltiazem and 40 mg/day of isosorbide mononitrate. However, she had recurrent chest pain with ST elevation every day (especially early in the morning). Because she had RVA with a history of bronchial asthma, we added 30 mg/day of oral prednisolone. Simultaneously, we started inhalation of 200 μg/day of fluticasone propionate, because of her history of bronchial asthma.
Fig. 3.
Time-course of treatment. She had recurrent chest pain with ST elevation after oral administration of vasodilators. Finally, her symptoms disappeared upon treatment with 30 mg/day of oral prednisolone and inhalation of 200 μg/day of fluticasone propionate.
Her symptoms disappeared completely, and intravenous administration of isosorbide dinitrate was discontinued (Fig. 3). Prednisolone was decremented by 5 mg/day every 3 days. She was discharged from hospital with vasodilators (8 mg/day of benidipine, 15 mg/day of nicorandil, 200 mg/day of diltiazem, 40 mg/day of isosorbide mononitrate) and 10 mg/day of prednisolone. At the time of hospital discharge, hematology showed a white blood cell count of 3300/μL (neutrophils, 71.6%; lymphocytes, 19.3%; monocytes 7.3%; eosinophils 1.8%; and basophils 0.0%), a hemoglobin level of 13.1 g/dL, a platelet count of 12.5 × 104/μL, a BNP level of 16.9 pg/mL, and a CRP level of <0.10 mg/dL.
After discharge from hospital, prednisolone was decremented by 1 mg/day every 2 weeks. Finally, we prescribed 4 mg/day of prednisolone as maintenance therapy. The patient remained free of anginal symptoms during 12-month follow-up.
Discussion
Vasospastic angina is more common in Japan compared with Western countries [5]. The mechanism of action and pathophysiology of coronary spasm is not clear, but endothelial dysfunction and alternation of autonomic nervous tone are considered to be major factors [6]. Vasospastic angina is usually well controlled with oral vasodilators such as calcium antagonists and nitrates, and it is rare for patients with vasospastic angina to be refractory to conventional vasodilators.
We had prescribed 8 mg/day of benidipine, 15 mg/day of nicorandil, 200 mg/day of diltiazem, and 40 mg/day of isosorbide mononitrate, but our patient continued to have recurrent chest pain with appreciable ST elevation (Fig. 3). Therefore, additional therapy was needed to control angina and to prevent adverse events such as myocardial infarction or sudden cardiac death.
There are invasive and non-invasive choices for the treatment of RVA. β1 receptor agonists, vitamin E, and endothelin antagonists are non-invasive methods. Current guidelines state that use of corticosteroids is only a class-IIb indication for the treatment of vasospastic angina [7]. However, some case reports have demonstrated the effectiveness of corticosteroids for the treatment of RVA, especially in patients with allergic disease (e.g. bronchial asthma, chronic thyroiditis, Raynaud phenomenon, eosinophilia) 3, 4. Our case report is, in general, consistent with those reports. Other case reports reported focal infiltration of inflammatory cells in the coronary arteries of patients with vasospastic angina [8]. Therefore, local inflammation of the coronary artery may be associated with coronary vasospasm. The mechanism of action explaining the effectiveness of corticosteroids for coronary vasospasm is not clear, but case reports as well as the present study suggest that anti-inflammatory effects may contribute to control vasospastic angina. In our case, although there was no clear evidence of eosinophilia or elevation of inflammatory markers, blood tests showed that the number of eosinophils and levels of CRP decreased after oral administration of prednisolone. Takagi et al. [3] reported that corticosteroids were effective for patients with RVA with active and non-active bronchial asthma. Bronchial asthma was not active in our patient, but corticosteroids can suppress inflammation and hyper-reactivity in the coronary arteries, which can lead to vasospastic angina 3, 4. The initial dose of oral prednisolone for the treatment of RVA is controversial, because there are no guidelines for the volume used for such therapy. Case reports have suggested that the initial dose of oral prednisolone should be 20–40 mg/day 3, 4. In accordance to those case reports, we started with 30 mg/day of oral prednisolone as an initial dose of 0.5 mg/kg/day because her body weight was approximately 60 kg.
Conversely, it has been reported that corticosteroids are not effective for the treatment of atherosclerotic coronary artery disease. Azar et al. [9] reported that anti-inflammatory therapy with methylprednisolone did not improve the short-term outcomes of patients with unstable angina, whereas this therapy significantly decreased serum levels of CRP. Roberts et al. [10] reported the deleterious effects of methylprednisolone in patients with myocardial infarction. In addition, long-term administration of corticosteroids can lead to adverse side effects such as hypertension, corticosteroid-induced diabetes mellitus, congestive heart failure, susceptibility to infection, osteoporosis, and gastroduodenal ulcers. Therefore, the use of corticosteroids should be considered in carefully selected patients with RVA with allergic disease.
Stent implantation is also a treatment for refractory focal vasospastic angina [2]. However, stenting does not work in patients with diffuse or multivessel coronary spasm [2]. In our case, stent implantation was not an option because coronary vasospasm occurred diffusely in the distal segment of the right coronary artery (Fig. 1c). In addition, some studies reported that implantation of drug-eluting stents was associated with vascular endothelial dysfunction and coronary vasospasm [6]. Furthermore, there are the problems of restenosis and continuous antiplatelet therapy to prevent stent thrombosis after stent implantation [2]. Therefore, stent implantation should be carried out in carefully selected patients with RVA.
Brachytherapy and sympathectomy are also therapeutic choices for RVA [1], but are invasive. Our patient had a history of bronchial asthma, so corticosteroids in addition to conventional oral vasodilators were the most appropriate and least invasive therapy for RVA.
In summary, our case report suggests that corticosteroids are a therapeutic choice for patients with RVA, especially for those with bronchial asthma. Further investigation involving a larger cohort is necessary to evaluate the effect of corticosteroids for the treatment of RVA.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Abbate A., Hamza M., Cassano A.D., Melchior R., Roberts C., Grizzard J., Shah K., Hastillo A., Kasirajan V., Crea F., Lanza G.A., Vetrovec G.W. Sympathectomy as a treatment for refractory coronary artery spasm. Int J Cardiol. 2012;161:e7–e9. doi: 10.1016/j.ijcard.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Marti V., Ligero C., Garcia J., Kastanis P., Guindo J., Dominguez de Rozas J.M. Stent implantation in variant angina refractory to medical treatment. Clin Cardiol. 2006;29:530–533. doi: 10.1002/clc.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takagi S., Goto Y., Hirose E., Terashima M., Sakuragi S., Suzuki S., Tsutsumi Y., Miyazaki S., Nonogi H. Successful treatment of refractory vasospastic angina with corticosteroids: coronary arterial hyperactivity caused by local inflammation? Circ J. 2004;68:17–22. doi: 10.1253/circj.68.17. [DOI] [PubMed] [Google Scholar]
- 4.Asano T., Kobayashi Y., Ohno M., Nakayama T., Kuroda N., Komuro I. Multivessel coronary artery spasm refractory to intensive medical treatment. Angiology. 2007;58:636–639. doi: 10.1177/0003319707303583. [DOI] [PubMed] [Google Scholar]
- 5.Sueda S., Ochi N., Kawada H., Matsuda S., Hayashi Y., Tsuruoka T., Uraoka T. Frequency of provoked coronary vasospasm in patients undergoing coronary arteriography with spasm provocation test of acetylcholine. Am J Cardiol. 1999;83:1186–1190. doi: 10.1016/s0002-9149(99)00057-0. [DOI] [PubMed] [Google Scholar]
- 6.Kim J.W., Suh S.Y., Choi C.U., Na J.O., Kim E.J., Rha S.W., Park C.G., Seo H.S., Oh D.J. Six-month comparison of coronary endothelial dysfunction associated with sirolimus-eluting stent versus paclitaxel-eluting stent. JACC Cardiovasc Interv. 2008;1:65–71. doi: 10.1016/j.jcin.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010;74:1745–1762. doi: 10.1253/circj.cj-10-74-0802. [DOI] [PubMed] [Google Scholar]
- 8.Kohchi K., Takebayashi S., Hiroki T., Nobuyoshi M. Significance of adventitial inflammation of the coronary artery in patients with unstable angina: results at autopsy. Circulation. 1985;71:709–716. doi: 10.1161/01.cir.71.4.709. [DOI] [PubMed] [Google Scholar]
- 9.Azar R.R., Rinfret S., Theroux P., Stone P.H., Dakshinamurthy R., Feng Y.J., Wu A.H., Range G., Waters D.D. A randomized placebo-controlled trial to assess the efficacy of antiinflammatory therapy with methylprednisolone in unstable angina (MUNA trial) Eur Heart J. 2000;21:2026–2032. doi: 10.1053/euhj.2000.2475. [DOI] [PubMed] [Google Scholar]
- 10.Roberts R., DeMello V., Sobel B.E. Deleterious effects of methylprednisolone in patients with myocardial infarction. Circulation. 1976;53:I204–I206. [PubMed] [Google Scholar]