Abstract
Cocaine toxicity can result in myocardial infarction from coronary vasospasm. The current treatment algorithm includes intravenous and/or intracoronary vasodilator administration with an expectantly quick resolution of symptoms and signs of ischemia. However, in situations in which myocardial injury persists, the optimal management is uncertain. We present a case in which extracorporeal membrane oxygenation effectively stabilized a patient with ongoing hemodynamic instability who experienced repeated episodes of myocardial injury and ventricular tachyarrhythmias due to cocaine toxicity.
<Learning objective: In many urban settings, cocaine-induced angina is not uncommon. The pathogenesis of its manifestation includes coronary artery vasospasm and decreased left ventricular function. Treatment typically involves systemic vasodilators, such as nitrates and calcium channel blockers. However, in patients with substantial hemodynamic instability, these agents might result in a worsening of systemic perfusion. Accordingly, extracorporeal membrane oxygenation should be considered in such cases to promote myocardial recovery.>
Keywords: Extracorporeal membrane oxygenation, Coronary artery vasospasm, Cocaine toxicity
Introduction
Cocaine toxicity is associated with significant cardiovascular morbidity and overall mortality. The primary mechanisms of this process include profound coronary vasospasm and tachycardia. Initial management typically involves vasodilators such as nitrates and dihydropyridine calcium channel blockers; however, in patients who develop cardiogenic shock, hemodynamic instability precludes their administration. Accordingly, we present a unique case in which extracorporeal membrane oxygenation (ECMO) was employed to stabilize a patient experiencing prolonged cardiovascular collapse due to cocaine intoxication and the effects of its metabolites.
Case report
A 52-year-old male with a history of cocaine use and hypertension presented to the emergency department (ED) with unrelenting angina following cocaine ingestion. The initial electrocardiogram (ECG) exhibited ST-segment elevations that did not resolve following administration of sublingual nitroglycerin. Shortly thereafter, the patient experienced ventricular fibrillation for which he underwent cardiopulmonary resuscitation, electrical cardioversion, and intubation with return of spontaneous circulation. He was taken urgently for cardiac catheterization, which revealed diffuse left-sided and distal right-sided coronary artery vasospasm without any correctable underlying atherosclerotic disease (Fig. 1). His coronary arteries responded to intracoronary administration of nitroglycerin.
Fig. 1.
Coronary angiogram upon admission. Images demonstrate diffuse vasospasm of the obtuse marginal (A), left anterior descending (B), and right coronary arteries (C).
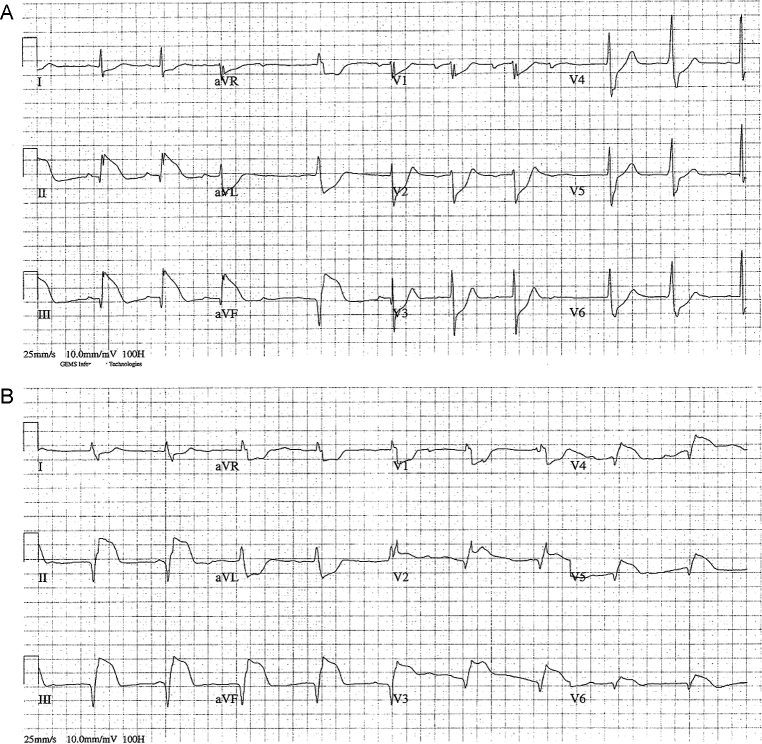
Several hours after admission while on intravenous nitroglycerin, the patient suffered a recurrent ventricular fibrillation arrest. Following resuscitation, the patient demonstrated profound inferior–posterior and right ventricular injury pattern on ECG and marked hemodynamic instability (Fig. 2). Due to his profound degree of cardiogenic shock, his vasodilator therapies were discontinued and an intra-aortic balloon pump was emergently placed. The patient continued to demonstrate significant hemodynamic instability with an ejection fraction of 10–15% on echocardiogram. Accordingly, the cardiac surgery service was consulted and the patient underwent emergent veno-arterial ECMO canulation via the right femoral artery and left femoral vein. There was an immediate improvement in the patient's mixed venous oxygenation (40–80%) and the degree of ST-segment elevation (Fig. 3).
Fig. 2.
12-lead (A) and right ventricular (B) electrocardiograms during initial arrest. Images demonstrate profound inferior–posterior and right ventricular injury pattern.
Fig. 3.
Initial and follow-up electrocardiogram. Note the ST-segment elevation in the inferior leads (II, III, and AVF) on admission (A) which improved following extracorporeal membrane oxygenation canulation (B).
Over the course of the ensuing 3 days, the patient experienced continued cardiovascular recovery. ECMO was gradually weaned to off without a substantial change in his cardiac indices or perfusion parameters and he was successfully separated from support. The remainder of his hospital course was notable for the discovery of multiple watershed cerebral infarcts, either secondary to transient episodes of hypoperfusion during his cardiac arrests or cerebral vasospasm. He was ultimately discharged to a skilled nursing facility for further neurologic rehabilitation.
Discussion
We present a case in which profound hemodynamic lability limited medical options in treating cocaine-induced coronary vasospasm, resulting in the initiation of ECMO therapy and subsequent recovery of cardiovascular function.
Cocaine-induced myocardial infarction occurs in approximately 6% of patients presenting to the ED with chest pain following cocaine ingestion [1]. The pathogenesis of this insult includes direct myocardial injury, diffuse coronary artery vasospasm, and plaque rupture with thrombosis, all related to heightened sympathetic activity 2, 3. Typical management for cocaine-induced coronary vasospasm includes administration of vasodilators, such as nitroglycerin and calcium channel blockers, and close observation 3, 4. These physiologic effects commonly last only 12 h as the vasospasm is quick to subside.
This patient's clinical course failed to improve following the initial injury. Despite intracoronary and systemic administration of coronary vasodilators, the patient had recurrent myocardial injury with ventricular fibrillation followed by profound cardiogenic shock. Recurrent arrhythmias due to cocaine toxicity have been attributed to ongoing ischemia, sodium channel blockade, or catecholamine excess [5]. Although the exact nidus in this case is unclear, the patient responded favorably to veno-arterial ECMO implementation with eventual stabilization of cardiac function.
Current treatment algorithms of cocaine-induced chest pain or myocardial infarction do not include temporary mechanical circulatory support as a component of management [1]. However, in patients with unstable hemodynamics and ongoing vasospasm, ECMO appears to be a safe option for myocardial recovery.
Conflicts of interest
There was no special funding obtained for this project. None of the authors has any relevant financial disclosures.
References
- 1.McCord J., Jneid H., Hollander J.E., de Lemos J.A., Cercek B., Hsue P., Gibler W.B., Ohman E.M., Drew B., Philippides G., Newby L.K. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008;117:1897–1907. doi: 10.1161/CIRCULATIONAHA.107.188950. [DOI] [PubMed] [Google Scholar]
- 2.Muscholl E. Effect of cocaine and related drugs on the uptake of noradrenaline by heart and spleen. Br J Pharmacol Chemother. 1961;16:352–359. doi: 10.1111/j.1476-5381.1961.tb01095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brogan W.C., 3rd, Lange R.A., Kim A.S., Moliterno D.J., Hillis L.D. Alleviation of cocaine-induced coronary vasoconstriction by nitroglycerin. J Am Coll Cardiol. 1991;18:581–586. doi: 10.1016/0735-1097(91)90617-i. [DOI] [PubMed] [Google Scholar]
- 4.Negus B.H., Willard J.E., Hillis L.D., Glamann D.B., Landau C., Snyder R.W., Lange R.A. Alleviation of cocaine-induced coronary vasoconstriction with intravenous verapamil. Am J Cardiol. 1994;73:510–513. doi: 10.1016/0002-9149(94)90684-x. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman R.S. Treatment of patients with cocaine-induced arrhythmias: bringing the bench to the bedside. Br J Clin Pharmacol. 2010;69:448–457. doi: 10.1111/j.1365-2125.2010.03632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]