Abstract
Background:
It has been shown that short-wavelength blue component of the visible light spectrum can alter the circadian rhythm and suppress the level of melatonin hormone. The short-wavelength light emitted by smartphones’ screens can affect the sleep quality of the people who use these devices at night through suppression of melatonin.
Objectives:
In this study, we examined the effects of covering the screens of smartphones with different filters (changing the effective wavelength of the light) on sleep delay time in 43 healthy students.
Materials and Methods:
Volunteer students were asked to go to bed at 23:00 and to use their mobile phones in bed for watching a natural life documentary movie for 60 minutes. No filter was used for one night while amber and blue filters were used for other 2 nights. Photospectrometry method was used to determine the output spectrum of the light passing through the filters used for covering the screens of the mobile phones. The order for utilizing amber or blue filters or using no filter was selected randomly. After 1 hour, the participants were asked to record their sleep delay time measured by a modified form of sleep time record sheet.
Results:
The mean sleep delay time for the “no-filter” night was 20.84±9.15 minutes, while the sleep delay times for the nights with amber and blue filters were 15.26±1.04 and 26.33±1.59 minutes, respectively.
Conclusion:
The findings obtained in this study support this hypothesis that blue light possibly suppresses the secretion of melatonin more than the longer wavelengths of the visible light spectrum. Using amber filter in this study significantly improved the sleep quality. Altogether, these findings lead us to this conclusion that blocking the short-wavelength component of the light emitted by smartphones’ screens improves human sleep.
Keywords: Smartphones , Mobile Phones , Blue Light , Sleep Quality , Display , Screen
Introduction
The retinal light exposure can affect sleep duration and biological parameters such as blood pressure [1]. As output of light-emitting electronic devices such as smartphones, tablets and laptops is mainly in the short wavelength component of the visible light spectrum, using these devices before sleep might cause sleep disorders. Some studies show that exposure to bright light at night suppresses melatonin secretion and, it has been revealed that human circadian system is susceptible to short-wavelength component of the visible light spectrum [2,3]. Some recent studies show that especially short wavelength blue light adversely affects the level of melatonin more than other wavelengths of the visible spectrum. On the other hand, for treatment of some types of mood disorders and sleep problems which are caused by circadian rhythm, blue wavelengths have been effectively used [4]. The disturbances of circadian rhythm are believed to be linked to the increased prevalence of sleep disorders and light therapy through regulation of the circadian system can be used to treat these sleep disorders [5]. The use of blue light in modern societies is rapidly increasing and it is estimated that a large proportion of the population of the world are exposed to artificial light at night [6]. Recent studies reveal that exposure to artificial light at night can be associated with increased risk of breast and prostate cancer [7]. Blue light has some well-known applications in different medical fields such as phototherapy [8,9]. or antibacterial treatment of plaque-induced periodontal pathologies [10]. As exposure to blue light is associated with some risks, it has been suggested to use LEDs with the emission peak of 470-480 nm instead of using LEDs with emission peaks below 450 nm [6]. Over the past several years, our laboratories at the Ionizing and Non-ionizing Radiation Protection Research Center (INIRPRC) have expanded their focus on studying the health effects of exposure to some common and/or occupational sources of electromagnetic fields (EMFs) such as cellular phones [11-19], mobile base stations [20], mobile phone jammers [21,23], laptop computers [24], radars [12], dentistry cavitrons [25], MRI [26,27], Wi-Fi routers [28] and different coils [29,30]. This study was aimed at assessing if blocking the short-wavelength component of the light emitted by smartphones’ screens could improve the sleep quality in university students.
Material and Methods
Participants
Forty-three healthy students (15 males and 28 females, mean age: 23.58 ± 8.78 years) participated in this study. Prior to the experiment, an oral explanation was given to all participants.
Ethical Issues
This study was approved by the INIRPRC and was carried out in accordance with the ethical guidelines of Shiraz University of Medical Sciences (SUMS). All participants were provided with written informed consent.
Exposure to Light
All participants were requested to go to bed at 23:00 under dim light conditions. They were asked to use their mobile phones in bed for 60 minutes (to watch a life documentary movie). No filter was used on one night, while amber and blue filters were used on other 2 nights. The brightness of the screens was the same on these three nights. The output spectrum of the light passing through the filters used to cover the screens of the mobile phones was determined by spectrometric methods (Figure 1). The order for using amber or blue filters or using no filter was selected randomly. After 1 hour, the participants were asked to record their sleep delay time measured by a modified form of sleep time sheet. Furthermore, all participants were asked to complete a previously validated questionnaire about their routine exposures to different electromagnetic fields. Participants were instructed to keep the bedroom temperature at about 25°C and were ordered to maintain their regular sleep/wake up schedule (e.g. 24:00 to 08:00).
Figure1.
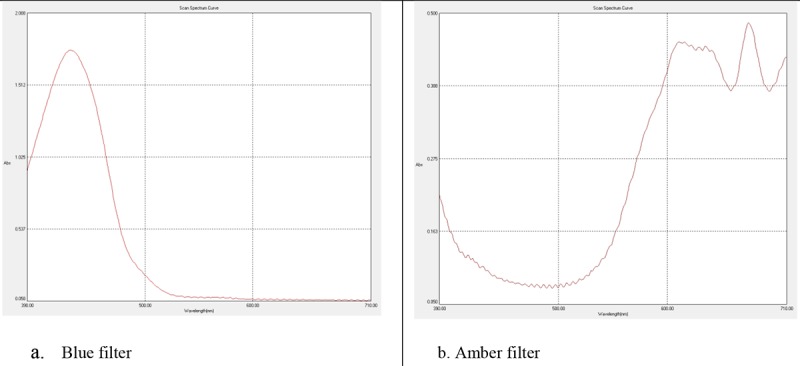
The output spectra of the light passing through the blue (panel a.) and amber (panel b) filters which covered the screens of the participants’ mobile phones.
Results
The mean age of the participants was 23.6 ± 8.8 years. The frequency of male participants was 15 students (34.9%), while 28 students (65.1%) were female. The majority of students who participated in this study were G.P., Ph.D. or M.D. students (24 students, 55.84%). Demographic characteristics of the participants are shown in Table 1.
Table 1.
Demographic characteristics of participants.
| Characteristics | |
|---|---|
| Age (Mean ±SD) (years) | 23.6 ± 8.8 |
| Sex | Frequency (%) |
| Male | 15 (34.9%) |
| Female | 28 (65.1%) |
| Education | Frequency (%) |
| College Students | 6 (14%) |
| BSc Students | 12 (27.9%) |
| MSc Students | 1 (2.3%) |
| GP, Ph.D., MD Students | 24 (55.84%) |
The mean sleep delay time for the “no filter” night was 20.84±9.15 minutes, while the sleep delay times for amber and blue filters were 15.26±1.04 and 26.33±1.59 minutes, respectively.
Discussion
Based on the findings obtained in our study, it was revealed that the mean sleep delay time for the amber filter was the shortest, while it was intermediate for “no filter” and the longest sleep delay time was observed for blue filters. These findings are generally in line with the results of the study conducted by Korean researchers who reported that fine control of blue light in smartphone displays could reduce the adverse health effects of blue light emitted from the displays of smartphones at night [31]. However, the shortcomings of the paper published by Oh et al. have been addressed previously [32]. As discussed by Mortazavi et al., the first shortcoming in their study was due to this point that the authors only focused on the visible component of the electromagnetic radiation spectrum and ignored the reports which indicated a significant association between exposure to RF-EMFs of mobile or cordless phones and sleep problems [33,34]. It is worth noting that exposure to electromagnetic fields can also affect the level of plasma melatonin [35,36]. Moreover, in contrast with Oh et al., we paid attention to the confounding factor of the very low sensitivity of human eye to short wavelengths in the visible spectrum and controlled the light intensity. It has long been known that both scotopic and photopic eye sensitivities depend on the wavelength of light and the highest eye sensitivity in the photopic vision occurs in yellow-green region [37].
Our findings are generally in line with the findings obtained in a study conducted on sleep quality and the level of melatonin in 12 adults who used either blue-light shield or control eyewear two hours before sleep while using a self-luminous portable device. This study demonstrated significantly better sleep efficacy and sleep latency for users of the blue-light shield. Interestingly, individuals who used blue-light shield showed a higher level of sleepiness during portable device use [38].
These findings demonstrate that exposure to blue light may lead to sleep problems, while amber filter was capable of improving the sleep quality through decreasing the sleep delay time. These findings are generally in line with the growing body of evidence which shows blue light can suppress the secretion of melatonin, a hormone that controls the circadian rhythms.
Acknowledgement
This study was supported by the Ionizing and Non-ionizing Radiation Protection Research Center (INIRPRC), Shiraz University of Medical Sciences (SUMS), Shiraz, Iran.
Conflict of Interest:None Declared.
References
- 1.Ichikawa K. Changes in blood pressure and sleep duration in patients with blue light-blocking/yellow-tinted intraocular lens (CHUKYO study) Hypertens Res. 2014;37:659–64. doi: 10.1038/hr.2014.50. [DOI] [PubMed] [Google Scholar]
- 2.Kozaki T, Kubokawa A, Taketomi R, Hatae K. Light-induced melatonin suppression at night after exposure to different wavelength composition of morning light. Neurosci Lett. 2016;616:1–4. doi: 10.1016/j.neulet.2015.12.063. [DOI] [PubMed] [Google Scholar]
- 3.Figueiro MG, Plitnick BA, Lok A, Jones GE, Higgins P, Hornick TR, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527–37. doi: 10.2147/CIA.S68557. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alkozei A, Smith R, Killgore WD. Exposure to blue wavelength light modulates anterior cingulate cortex activation in response to ‘uncertain’ versus ‘certain’ anticipation of positive stimuli. Neurosci Lett. 2016;616:5–10. doi: 10.1016/j.neulet.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 5.Figueiro MG, Plitnick B, Rea MS. Pulsing blue light through closed eyelids: effects on acute melatonin suppression and phase shifting of dim light melatonin onset. Nat Sci Sleep. 2014;6:149–56. doi: 10.2147/NSS.S73856. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Mol Vis. 2016;22:61–72. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 7.Smolensky MH, Sackett-Lundeen LL, Portaluppi F. Nocturnal light pollution and underexposure to daytime sunlight: Complementary mechanisms of circadian disruption and related diseases. Chronobiol Int. 2015;32:1029–48. doi: 10.3109/07420528.2015.1072002. [DOI] [PubMed] [Google Scholar]
- 8.Ebbesen F, Vandborg PK, Madsen PH, Trydal T, Jakobsen LH, Vreman HJ. Effect of phototherapy with turquoise vs. blue LED light of equal irradiance in jaundiced neonates. Pediatr Res 2016;79:308–12. doi: 10.1038/pr.2015.209. [DOI] [PubMed] [Google Scholar]
- 9.Uchida Y, Morimoto Y, Uchiike T, Kamamoto T, Hayashi T, Arai I, et al. Phototherapy with blue and green mixed-light is as effective against unconjugated jaundice as blue light and reduces oxidative stress in the Gunn rat model. Early Hum Dev. 2015;91:381–5. doi: 10.1016/j.earlhumdev.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Mahdi Z, Habiboallh G, Mahbobeh NN, Mina ZJ, Majid Z, Nooshin A. Lethal effect of blue light-activated hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers on the viability of Porphyromonas gingivalis and Fusobacterium nucleatum. Laser Ther. 2015;24:103–11. doi: 10.5978/islsm.15-OR-09. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mortazavi SM, Motamedifar M, Namdari G, Taheri M, Mortazavi AR, Shokrpour N. Non-linear adaptive phenomena which decrease the risk of infection after pre-exposure to radiofrequency radiation. Dose Response. 2014;12:233–45. doi: 10.2203/dose-response.12-055.Mortazavi. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mortazavi SM, Taeb S, Dehghan N. Alterations of visual reaction time and short term memory in military radar personnel. Iran J Public Health. 2013;42:428–35. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 13.Mortazavi SM, Rouintan MS, Taeb S, Dehghan N, Ghaffarpanah AA, Sadeghi Z, et al. Human short-term exposure to electromagnetic fields emitted by mobile phones decreases computer-assisted visual reaction time. Acta Neurol Belg. 2012;112:171–5. doi: 10.1007/s13760-012-0044-y. [DOI] [PubMed] [Google Scholar]
- 14.Mortazavi S, Mosleh-Shirazi M, Tavassoli A, Taheri M, Mehdizadeh A, Namazi S, et al. Increased Radioresistance to Lethal Doses of Gamma Rays in Mice and Rats after Exposure to Microwave Radiation Emitted by a GSM Mobile Phone Simulator. Dose Response. 2013;11:281–92. doi: 10.2203/dose-response.12-010.Mortazavi. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mortazavi S, Mosleh-Shirazi M, Tavassoli A, Taheri M, Bagheri Z, Ghalandari R, et al. A comparative study on the increased radioresistance to lethal doses of gamma rays after exposure to microwave radiation and oral intake of flaxseed oil. Iranian Journal of Radiation Research. 2011;9:9–14. [Google Scholar]
- 16.Mortavazi S, Habib A, Ganj-Karami A, Samimi-Doost R, Pour-Abedi A, Babaie A. Alterations in TSH and Thyroid Hormones following Mobile Phone Use. Oman Med J. 2009;24:274–8. doi: 10.5001/omj.2009.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mortazavi SM, Daiee E, Yazdi A, Khiabani K, Kavousi A, Vazirinejad R, et al. Mercury release from dental amalgam restorations after magnetic resonance imaging and following mobile phone use. Pak J Biol Sci. 2008;11:1142–6. doi: 10.3923/pjbs.2008.1142.1146. [DOI] [PubMed] [Google Scholar]
- 18.Mortazavi SM, Ahmadi J, Shariati M. Prevalence of subjective poor health symptoms associated with exposure to electromagnetic fields among university students. Bioelectromagnetics. 2007;28:326–30. doi: 10.1002/bem.20305. [DOI] [PubMed] [Google Scholar]
- 19.Mortazavi S, Motamedifar M, Namdari G, Taheri M, Mortazavi A. Counterbalancing immunosuppression-induced infections during long-term stay of humans in space. Journal of Medical Hypotheses and Ideas. 2013;7:8–10. doi: 10.1016/j.jmhi.2012.12.001. [DOI] [Google Scholar]
- 20.Mortazavi S. Safety issue of mobile phone base stations. J Biomed Phys Eng. 2013;3:1–2. [PMC free article] [PubMed] [Google Scholar]
- 21.Mortazavi S, Parsanezhad M, Kazempour M, Ghahramani P, Mortazavi A, Davari M. Male reproductive health under threat: Short term exposure to radiofrequency radiations emitted by common mobile jammers. J Hum Reprod Sci. 2013;6:124–8. doi: 10.4103/0974-1208.117178. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rafati A, Rahimi S, Talebi A, Soleimani A, Haghani M, Mortazavi SM. Exposure to Radiofrequency Radiation Emitted from Common Mobile Phone Jammers Alters the Pattern of Muscle Contractions: an Animal Model Study. J Biomed Phys Eng. 2015;5:133–42. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 23.Shekoohi*Shooli F, Mortazavi SA, Jarideh S, Nematollahii S, Yousefi F, Haghani M, et al. Short-Term Exposure to Electromagnetic Fields Generated by Mobile Phone Jammers Decreases the Fasting Blood Sugar in Adult Male Rats. J Biomed Phys Eng. 2016;6:27–32. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 24.Mortazavi SMJ, Tavassoli A, Ranjbari F, Moammaiee P. Effects of laptop computers’ electromagnetic field on sperm quality. Journal of Reproduction & Infertility. 2010;11(4) [Google Scholar]
- 25.Mortazavi SM, Vazife-Doost S, Yaghooti M, Mehdizadeh S, Rajaie-Far A. Occupational exposure of dentists to electromagnetic fields produced by magnetostrictive cavitrons alters the serum cortisol level. J Nat Sci Biol Med. 2012;3:60–4. doi: 10.4103/0976-9668.95958. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mortazavi SM, Neghab M, Anoosheh SM, Bahaeddini N, Mortazavi G, Neghab P, et al. High-field MRI and mercury release from dental amalgam fillings. Int J Occup Environ Med. 2014;5:101–5. [PMC free article] [PubMed] [Google Scholar]
- 27.Mortazavi SM, Daiee E, Yazdi A, Khiabani K, Kavousi A, Vazirinejad R, et al. Mercury release from dental amalgam restorations after magnetic resonance imaging and following mobile phone use. Pak J Biol Sci. 2008;11:1142–6. doi: 10.3923/pjbs.2008.1142.1146. [DOI] [PubMed] [Google Scholar]
- 28.Mahmoudi R, Mortazavi S, Safari S, Nikseresht M, Mozdarani H, Jafari M, et al. Effects of microwave electromagnetic radiations emitted from common Wi-Fi routers on rats’ sperm count and motility. Int J Radiat Res. 2015;13:363–8. [Google Scholar]
- 29.Haghnegahdar A, Khosrovpanah H, Andisheh-Tadbir A, Mortazavi G, Saeedi Moghadam M, Mortazavi S, et al. Design and fabrication of helmholtz coils to study the effects of pulsed electromagnetic fields on the healing process in periodontitis: preliminary animal results. J Biomed Phys Eng. 2014;4:83–90. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 30.Paknahad M, Shahidi S, Mortazavi SMJ, Mortazavi G, Moghadam MS, Nazhvani AD. The Effect of Pulsed Electromagnetic Fields on Microleakage of Amalgam Restorations: An in Vitro Study. Shiraz E-Medical Journal. 2016;17(2) [Google Scholar]
- 31.Oh JH, Yoo H, Park HK, Do YR. Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep. 2015;5:11325. doi: 10.1038/srep11325. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MortazaVI SMJ, Mortazavi SA, Habibzadeh P, Mortazavi G. Is it Blue Light or Increased Electromagnetic Fields which Affects the Circadian Rhythm in People who Use Smartphones at Night. Iranian journal of public health. 2016;45:405–6. [PMC free article] [PubMed] [Google Scholar]
- 33.Yogesh S, Abha S, Priyanka S. Mobile usage and sleep patterns among medical students. Indian J Physiol Pharmacol. 2014;58:100–3. [PubMed] [Google Scholar]
- 34.Redmayne M, Smith E, Abramson MJ. The relationship between adolescents’ well-being and their wireless phone use: a cross-sectional study. Environ Health. 2013;12:90. doi: 10.1186/1476-069X-12-90. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh S, Mani KV, Kapoor N. Effect of occupational EMF exposure from radar at two different frequency bands on plasma melatonin and serotonin levels. Int J Radiat Biol. 2015;91:426–34. doi: 10.3109/09553002.2015.1004466. [DOI] [PubMed] [Google Scholar]
- 36.El-Helaly M, Abu-Hashem E. Oxidative stress, melatonin level, and sleep insufficiency among electronic equipment repairers. Indian J Occup Environ Med. 2010;14:66–70. doi: 10.4103/0019-5278.75692. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh KC. Basic Physics: PHI Learning Pvt. Ltd . 2009. p. 424. [Google Scholar]
- 38.Ayaki M, Hattori A, Maruyama Y, Nakano M, Yoshimura M, Kitazawa M, et al. Protective effect of blue-light shield eyewear for adults against light pollution from self-luminous devices used at night. Chronobiol Int. 2016;33:134–9. doi: 10.3109/07420528.2015.1119158. [DOI] [PubMed] [Google Scholar]


