ABSTRACT
Having benign paroxysmal positional vertigo (BPPV) puts patients at a significantly higher risk of falling. It is poorly recognised and diagnosis is frequently delayed. BPPV has been studied in outpatient settings, but there have been no studies looking at the prevalence in patients admitted with falls. This study aims to establish how common BPPV is in these patients.
For a 4-month period, patients admitted on an unselected medical take were screened for an admission precipitated by a fall. Patients who consented were assessed for BPPV using the Dix-Hallpike manoeuvre. Patients who tested positive were treated using the Epley manoeuvre. The assessments were carried out by specialist physiotherapists who were experienced at assessing and diagnosing patients with peripheral vestibular disorders.
Out of the 111 patients initially identified, 37 (33%) were considered to be appropriate and consented to be part of the study. Of these, 20 patients (54%) had a positive Dix-Hallpike manoeuvre.
Of the patients included in the study, over half tested positive for BPPV. This merits further study. Potentially, there is a proportion of patients admitted with falls who have an easily treatable contributing factor that is not being identified with standard practice.
KEYWORDS: Falls, vertigo, BPPV
Introduction
Falls are an increasingly important issue for the NHS because they are a major cause of morbidity and mortality. The rate of falls is higher in older patients. Currently, there are 10 million people over the age of 65 in the UK; this number is set to increase to 19 million by 20501 and will likely be accompanied by an increase in the incidence of falls. Estimates put the cost of falls to the NHS at £2.3 billion per year.2
It has been well documented in previous studies that dizziness is a common symptom in older patients, with prevalence quoted as between 13% and 38%,3 rising to 50% in patients over the age of 85. Benign paroxysmal positional vertigo (BPPV) is thought to be the most common cause of dizziness in older patients and has a higher prevalence in women.4 BPPV is a ‘clinical syndrome characterised by recurrent, brief episodes of severe vertigo and rotatory nystagmus, precipitated by specific positions of the head relative to gravity’.4 It is often poorly recognised by non-specialists and, as such, is diagnosed late. There is a long delay between onset of symptoms and diagnosis, often with multiple healthcare contacts. One study found that the average time between first symptoms and diagnosis was 70 months, with an average of eight hospital visits.5
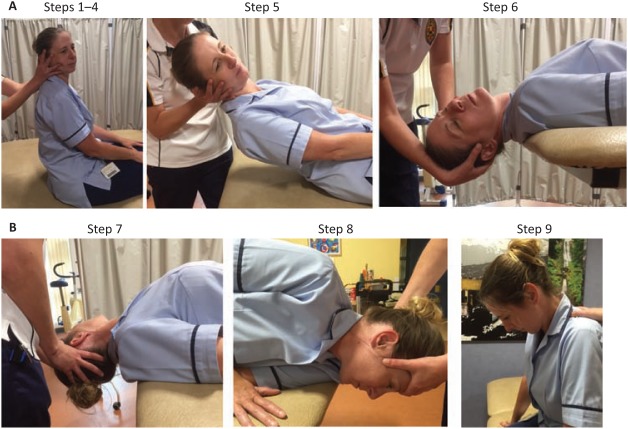
The symptoms of BPPV result in a significantly increased risk of falling.6,7 Although the diagnosis can be frequently delayed, once it is suspected, BPPV can be easily diagnosed using the Dix-Hallpike manoeuvre.8 Originally described in 1952, the Dix-Hallpike Manoeuvre can be performed in less than 5 minutes by trained staff and is comprised of the following steps (Fig 1a):
Sit the patient on an examination couch so that their shoulders are in line with the end of the couch when lying down.
Holding both sides of the patient’s head, turn the their head 45° towards the side of the vestibular system being tested.
Ask the patient to keep their eyes open and fix them on a point in front of them throughout the test.
Observe for nystagmus (continuous uncontrolled movement of the eyes).
Keeping the 45° position, hold the patients head and bring the patient rapidly backwards so the head hangs 15–20° below the horizontal plane beyond the edge of the examination couch.
Maintain the position for 30–60 seconds, observing for rotational nystagmus and symptoms of vertigo.9
Fig 1.
A – Dix-Hallpike manoeuvre. B – additional steps for the Epley manoeuvre.
Particle repositioning manoeuvres, for example the Epley manoeuvre, are the most effective and successful treatments available, curing 61.5–87% of patients.10–12 The Epley manoeuvre initially starts with a Dix-Hallpike procedure with the following additional steps (Fig 1b):
After 20 seconds in the final position of the Dix-Hallpike manoeuvre, turn the patient’s head to the opposite direction such that it is 45° from the midline in the opposite direction.
Hold this position for 20 seconds then turn the patient’s body 90° in the new direction of the head, ie the patient has gone from lying on their back to lying on their side with their head looking towards the ground.
After 20 seconds in this position, sit the patient up.12
Particle repositioning manoeuvres as treatment for BPPV mean that pharmacological treatments, which themselves may pose a falls risk by causing sedation, are not necessary.13
BPPV assessment and treatment has been integrated into outpatient falls clinics, as well as pre-existing ear, nose and throat dizziness clinics.14 However, a literature search failed to provide the prevalence of BPPV among those who are admitted with falls. The aim of this study was to assess the prevalence of BPPV in older people admitted to hospital with falls that would potentially otherwise go undiagnosed.
Methods
Every weekday between 17 March 2014 and 27 July 2014, the medical admissions list was reviewed. This included reviewing patients admitted over the weekTheyend on a Monday. Patients with a reason for admission that may be consistent with falls, including ‘falls’, ‘dizzy’, ‘collapse’ and ‘off legs’, were selected. These selection criteria were chosen as the admission reason on the admission list was at times non-specific, and as a team we were trying to include all patients who had fallen.
Medical notes were then screened to assess their suitability for the study. Patients were included if they were over the age of 65. were excluded if they lacked capacity to consent to the study, or were too unwell to participate.
Those meeting the criteria then met with a specialist physiotherapist who explained the project. Subjects were provided with an information leaflet and given time to consider involvement. They had a further consultation with the physiotherapist where those wishing to be included were given further opportunity to ask questions and then sign a consent form.
After providing consent, patients were tested using the Dix-Hallpike manoeuvre to diagnose BPPV. If this was positive, they were subsequently treated for BPPV and followed up as they normally would be for this diagnosis. The medical team caring for the subject as an inpatient and the patient’s GP were informed of their involvement in the study and the results of testing.
This study received ethical approval on 30 January 2014 from the National Institute for Social Care and Health Research (NISCHR), Research Ethics Service (REC Reference 14/WA/0006).
Results
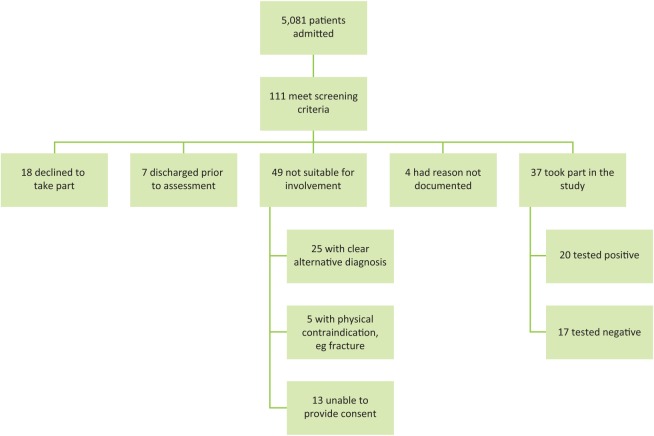
During the study period, 5,081 patients were admitted to the acute medical wards. Of these, 111 patients were identified as potentially suitable for assessment from the admissions list. Following a review of the patients’ case notes and discussion with the patients themselves, 18 patients declined to take part in the study, 7 were discharged prior to assessment, and 49 were determined to be unsuitable for assessment. The reasons for this inability to assess patients are summarised in Fig 2.
Fig 2.
Results breakdown
The mean age of the patients assessed was 82.4 years (range: 65–96 years). More women than men were assessed: 68% of the patients were female.
In total, 37 patients were tested for BPPV. Of those who were assessed, 20 were positive for BPPV (54%) and 17 patients were negative. The patients who tested positive were treated and followed up by the specialist physiotherapist team.
Discussion
Although we have attained only a small data set, we found that 54% of patients that participated in our study were positive for BPPV. Prior to initiating this project, there was a possibility that these patients may have been discharged without the consideration of BPPV as a contributor to their falls. Many other contributing factors may have been assessed and treated; however, this lack of assessment means that an easily treatable risk factor for falls may have been missed.
BPPV is a well-recognised risk factor for falling. Our study found that there is likely to be a cohort of patients who are admitted with falls that have BPPV as a contributing factor to their falls. This has not been identified in previous studies.
Firstly, it is important to note that many of the patients initially identified for the study were not appropriate for assessment for BPPV (Fig 2). Many of the reasons that patients were not able to be assessed may have precipitated their falls, eg septicaemia or stroke. Unfortunately, many patients who were admitted with falls lacked capacity, mainly as a result of delirium or dementia. Because they were not able to consent to participation, they were excluded from the study.
A large proportion of the patients that were assessed had a positive Dix-Hallpike manoeuvre and, as such, they were diagnosed with BPPV. It has previously been found that 13% of patients in a falls clinic had a diagnosis of BPPV.15 Patients involved in this previous outpatient study had a mean age of 64 years, compared with 82.4 years in ours. This may represent the difference in the populations of those admitted because of falls as opposed to those assessed as an outpatient.
A smaller number of men than women were included in the study and a higher proportion of women tested positive for BPPV than men. This is consistent with previous research showing that BPPV is more common in women.
It is clear from this data that patients admitted with falls, in the absence of an acute medical illness, could benefit from assessment for BPPV. This is even more important when considering the fact that BPPV is an easily treatable contributor to falls.
Key Points
BPPV is a commonly missed, and easily treatable, risk factor for falls.
Assessment for BPPV is currently integrated into falls clinics; however, no previous research has looked at patients admitted with falls.
This study found that 54% of patients admitted with falls that were suitable for assessment had BPPV.
We would suggest that all patients admitted with falls are assessed for BPPV to minimise their risks of further falls.
Exclusion criteria means that many of those with BPPV go undetected.
Conflicts of interests
The authors declare no conflicts of interests.
References
- 1.Cracknell R. The ageing population. In: Mellows-Facer A, editor. Key issues for the new parliament 2010. London:: House of Commons Library; 2010. p. 45. [Google Scholar]
- 2.National Institute for Health and Care Excellence Falls in older people: assessing risk and prevention. London:: NICE; p. 2013. NICE clinical guideline 161. [PubMed] [Google Scholar]
- 3.Alrwaily M. Whitney SL. Vestibular rehabilitation of older patients with dizziness. Otolaryngol Clin North Am. 2011;44:473–96. doi: 10.1016/j.otc.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Van der Velde GM. Benign paroxysmal positional vertigo part 1: background and clinical presentation. J Can Chiropract Assoc. 1999;43:31–40. [Google Scholar]
- 5.Wang H. Yu D. Song N. Su K. Yin S. Delayed diagnosis and treatment of benign paroxysmal positional vertigo associated with current practice. Eur Arch Otorhinolaryngol. 2014;271:261–4. doi: 10.1007/s00405-012-2333-8. [DOI] [PubMed] [Google Scholar]
- 6.Gananca FF. Gazzola JM. Gananca CF, et al. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2010;76:113–20. doi: 10.1590/S1808-86942010000100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barin K. Dodson EE. Dizziness in the elderly. Otolaryngol Clin North Am. 2011;44:437–54. doi: 10.1016/j.otc.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Dix MR. Hallpike CS. The pathology, symptomatology, and thediagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45:341–54. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.British Society of Audiology Recommended procedure for Hallpike manoeuvre. Bathgate:: BSA; 2001. Available at www.thebsa.org.uk/wp-content/uploads/2014/04/HM.pdf. [Accessed 29 April 2016] [Google Scholar]
- 10.Maslovara S. Soldo SB. Puksec M. Balaban B. Penavic IP. Benign paroxysmal positional vertigo (BPPV): influence of pharmacotherapy and rehabilitation therapy on patients’ recovery rate and life quality. NeuroRehabilitation. 2012;31:435–41. doi: 10.3233/NRE-2012-00814. [DOI] [PubMed] [Google Scholar]
- 11.Appiani GC. Gagliardi M. Urbani L. Luccertini M. The Epley maneuver for the treatment of benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol. 1996;253:31–4. doi: 10.1007/BF00176699. [DOI] [PubMed] [Google Scholar]
- 12.Bahadir C. Diracoglu D. Kurtulus D. Garipoglu I. Efficacy of canalith repositioning maneuvers for benign paroxysmal positional vertigo. Clinical Chiropractic. 2009;12:95–100. [Google Scholar]
- 13.Sacco RR. Burmeister DB. Rupp VA. Greenbery MR. Management of benign paroxysmal positional vertigo: a randomised control trial. J Emerg Med. 2014;46:575–81. doi: 10.1016/j.jemermed.2013.08.116. [DOI] [PubMed] [Google Scholar]
- 14.Lawson J. Johnson I. Bamiou DE. Newton JL. Benign paroxysmal positional vertigo: clinical characteristics of dizzy patients referred to a falls and syncope unit. Q J Med. 2005;98:357–64. doi: 10.1093/qjmed/hci057. [DOI] [PubMed] [Google Scholar]
- 15.Lawson J. Bamiou DE. Cohen HS. Newton J. Positional vertigo in a falls service. Age Ageing. 2008;37:585–8. doi: 10.1093/ageing/afn151. [DOI] [PubMed] [Google Scholar]