ABSTRACT
Patient safety depends on adequate staffing but the number of doctors required for safe staffing for medical emergencies is not known. We measured the duration of the admission process for patients seen by medical teams in emergency departments (EDs) and acute medical units. History taking and examination by a core medical trainee took 22 minutes for a patient referred from the ED and 21 minutes for a patient referred from primary care. A complete admission clerking with prescription and ordering of investigations ranged from a mean of 15 minutes for a consultant in acute medicine to a mean of 55 minutes for a foundation year 1 trainee. The duration of post-take ward rounds also showed significant variability.
Our data can be used to model staffing patterns if combined with information about admission numbers and local set up.
KEYWORDS: Acute medicine, junior doctor, workload, consultant, shifts
Introduction
Hospital staffing levels have recently been highlighted as a key ingredient for a safe care environment. Concerns were founded on observations of poor care delivered by overstretched staff as part of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Recommendations from the Francis report1 and the subsequent review by Don Berwick for the Department of Health into patient safety in the NHS have led to a renewed debate about safe staffing levels.2 The National Institute for Health and Care Excellence has commissioned the development of guidelines for safe levels of staffing.3
While there is some evidence for recommendations for safe levels of staffing for nurses,4 there is currently limited evidence available to suggest the number of doctors required to safely manage acute hospital care. The Royal College of Physicians (RCP) recommends a minimum standard for consultant presence on acute medical units (AMUs).5 Given that consultants are working increasingly as part of complex multidisciplinary teams, there is scope for further work in this area. Delays in patients being seen and workload increases have the potential to impact on mortality, morbidity and length of stay in hospital.6,7
In order to ascertain objective criteria for staffing requirements, there is a need to better understand the workload of doctors and the timing of processes involved in routine aspects of medical care. The admission process is a key part of the acute medical team’s role and the time requirements for this and related tasks will have implications on the staffing models and the overall efficiency of units.
We sought to observe the admission process of acutely unwell medical patients by doctors of different grades while examining factors that influence time requirements.
Methods
Setting
The study took place at Ysbyty Gwynedd, Bangor in 2013 and 2014. Ysbyty Gwynedd is a district general hospital in north Wales with 550 beds covering all major specialties, including a renal unit and a 13 bedded critical care unit.
The AMU has 29 beds and is complemented by an ambulatory care unit for low-risk admissions. The latter two units are co-located and take direct admissions from primary care only.
During the day shift (08:00 to 20:30), the on-call team consists of four doctors in training (a newly qualified foundation year 1 (FY1) doctor, two core medical trainees (CMTs) with 1–4 years of experience, and one medical registrar with 4 or more years of clinical experience and membership of the Royal College of Physicians) and an on-call consultant with a full specialist qualification. The sole task of the on-call team is the care of emergency admissions and emergencies of inpatients. All team members, except for the consultant, have the additional responsibility of being part of the cardiac arrest team. Patients seen by doctors in training are subsequently reviewed by a consultant in acute medicine (08:00–17:00) or otherwise by the on-call consultant as part of the post-take ward round. Out-of-hours take and general medical ward cover is provided by two CMTs and the medical registrar.
New admissions have blood and an electrocardiogram taken by a technician prior to being ‘clerked’ by doctors. Clerking involves taking a full history, a physical examination and documentation in the patient’s notes, including the documentation of a working diagnosis, differential diagnosis and care plan. Clerking is usually undertaken by doctors in training prior to senior review. In our unit, clerking is at times also undertaken by consultants. The selection of patients will depend usually on queuing with the sickest patients and those who have been waiting longest being seen by more senior doctors.
Patients are referred to the AMU from the hospital’s emergency department (ED) and directly from primary care. Referrals from the ED are first clerked by an ED doctor who completes the ED documentation and then clerked again by a doctor of the medical on-call team who completes a separate medical admissions pro forma (Fig 1).
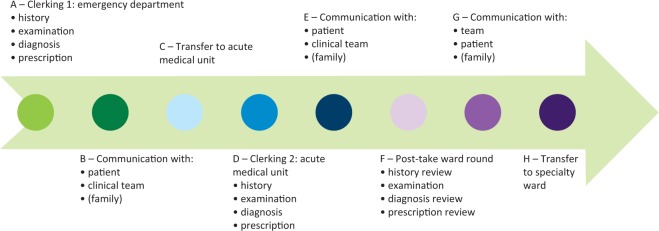
Fig 1.
High-level process map of the admission process for a medical emergency admission into hospital. For patients who are admitted directly to the acute medical unit after referral from primary care, the process starts with D. Study 1 measures clerking of patients admitted through the emergency department by a doctor in the emergency department (A) compared with a doctor from the medical on-call team (D). Study 2 measures the initial assessment by the medical on-call doctor (D and E). Study 3 measures the post-take ward round (F and G). B, C and H were not measured.
Study design
In order to determine the potential to optimise processes, we undertook three separate direct observation studies that timed workflow. Studies were approved by the audit department as service improvement projects. Doctors were aware that they were being observed and gave verbal consent to taking part in the project.
Study 1: direct observation of patients admitted after referral from the ED compared with those referred directly from primary care
A medical student screened potential medical admissions on arrival in the ED. The total time required for history and examination by ED doctors was recorded. This process was repeated when the patients had been referred for admission to hospital and subsequently had their history and examination taken by a member of the medical on-call team. Patients who were referred to a non-medical team or discharged from the ED were excluded.
Patients referred by a GP were seen in the AMU. The medical student observed and recorded the time taken by members of the on-call medical team to do a history and examination of patients referred directly from primary care to the AMU and compared it with the time taken for history and examination of patients admitted through the hospital’s ED.
Study 2: direct observation of clerking of patients directly admitted in the AMU after referral from primary care
The clerking of patients referred directly to the AMU from primary care was also reviewed by a medical student. Patient contacts were charted minute by minute against a pre-defined list of tasks (Fig 2), ie history taking, documentation and interruptions. One minute was the smallest measured time unit. For each time unit, more than one task could be performed simultaneously.
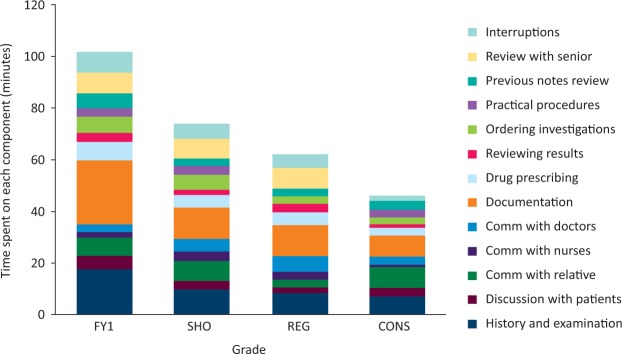
Fig 2.
Cumulative time units taken for tasks during clerking. The number of time units for concurrent tasks takes into account simultaneously performed tasks in pre-defined categories. The number of units is thus more than the time actually taken. Comm = communication; CONS = consultant; FY1 = foundation year 1 trainee; REG = registrar; SHO = senior house officer (includes foundation year 2 trainees and core medical trainees).
An interruption was defined as a request to deal with a matter not related to the patient currently being seen. ‘Concurrent tasks’ were defined as an individual handling more than one activity at the same time (ie communicating with a member of the team and documenting findings, or taking a history and examining the patient).
In order to capture case-mix, data was collected regarding the patient’s severity of illness as measured by the National Early Warning Score (NEWS) at the time of clerking and their dependency as measured by the Clinical Frailty Scale (CFS).8 Both parameters are routinely collected as part of the admissions process at Ysbyty Gwynedd.
Study 3: direct observation of the post-take ward round in the AMU
Timed observations of the post-take ward rounds were made by a core medical trainee. Patient contacts were charted minute by minute against the same pre-defined list of tasks as in study 2.
Results
Study 1: direct observation of patients admitted after referral from the ED compared with those referred directly from primary care
During May and June 2013, a total of 20 patient encounters were observed during the day shift of the on-call team in the working week. Half of these (10 patients) presented to the ED and were then admitted on to the AMU. The other ten patients were admitted directly to the AMU by their GP. Four of the ED referrals and three of the primary care referrals were seen by registrars. The remaining patients were seen by CMTs.
The mean time for a doctor to take a history and perform an examination of a patient in the ED was 19 minutes (standard deviation (SD), 4 minutes). For the medical on-call team, history and examination of patients referred from the ED took 22 minutes (SD 5 minutes), and 21 minutes (SD 2 minutes) for patients referred by their GPs. There was no significant difference in the time taken by ED doctors for patients admitted via ED compared with medical doctors or between the time taken by medical doctors to see ED versus primary care admissions. Time taken was not dependent on the level of illness as measured by NEWS (Median 2; IQR 1–3).
Study 2: direct observation of clerking of patients directly admitted in the AMU after referral from primary care
Demographics
In total, 40 patients were observed in January 2014: 9 were seen by FY1s, 10 by CMTs, 12 by registrars and 8 by acute medical consultants. Patients had a range of CFS scores with 18% of the cohort having a CFS score of 7 or 8 (severely frail or very severely frail) and 35% of the cohort having a CFS of 2 or 3 (well or managing well).
Overall time taken
FY1 doctors took a mean of 55 minutes (SD 6 minutes), CMTs a mean of 38 minutes (SD 16 minutes), medical registrars a mean of 32 minutes (SD 15 minutes) and consultants averaged 15 minutes (SD 5 minutes) to clerk a patient (Fig 3).
Fig 3.
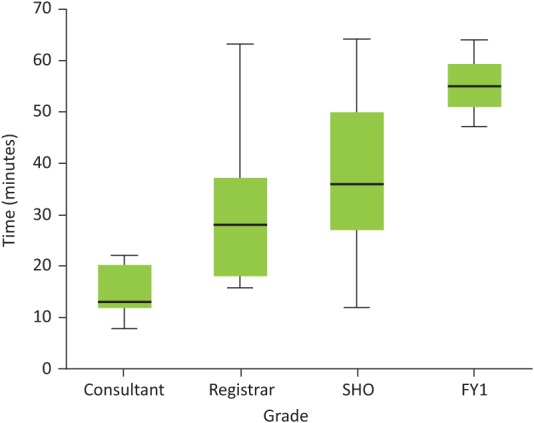
Time taken to clerk a patient in the acute medical unit according to seniority. FY1 = foundation year 1 trainee; SHO = senior house officer (includes foundation year 2 trainees and core medical trainees).
Individual components
The items with the highest time requirements for all grades of doctors were documentation (41%), history and examination (31%) and communication with relatives (19%). Fig 2 shows the breakdown of these components according to grade of doctor.
Interruptions
Interruptions took up a mean of 5 minutes (SD 5 minutes) per patient. FY1 doctors were interrupted more often and spent a mean of 8 minutes dealing with interruptions, while consultants spent a mean of only 2 minutes.
Impact of frailty and severity of illness
The length of the clerking process was related to the level of frailty of patients seen (Fig 4). Doctors spent a mean of 42 minutes (SD 17 minutes) with patients who were classified as severely or very severely frail (CFS 7/8, n=7). Patients with a CFS of 4 or 5 had a mean clerking time of 36 minutes (SD 18 minutes). The interaction with patients who were classified as well or managing well (CFS 2/3) took a mean of 29 minutes (SD 18 minutes).
Fig 4.
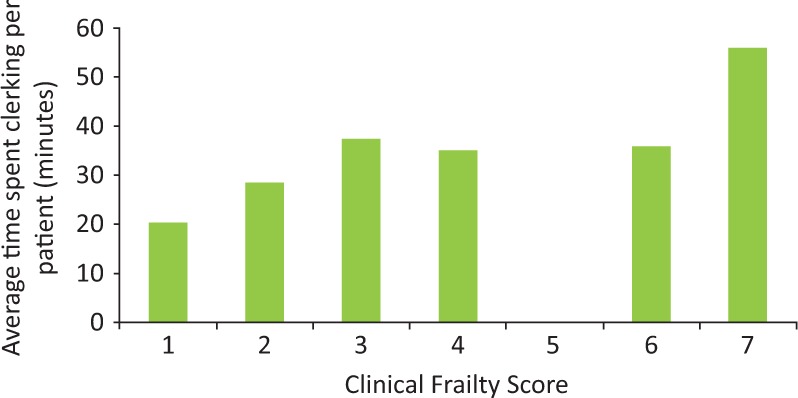
Mean clerking times in the acute medical unit for patients with different levels of frailty as measured by the Clinical Frailty Scale. The Clinical Frailty Scale scores denote: 1. Very fit, 2. Well, 3. Managing well, 4. Vulnerable, 5. Mildely frail, 6. Moderateley frail, 7. Severely frail, 8. Very severely frail, 9. Terminally ill. There were no patients with a score indicating mild frailty (5) in the cohort.
There was no correlation between NEWS score and the duration of clerking (p<0.68).
Study 3: direct observation of the post-take ward round in the AMU
In total, post-take ward rounds for 20 patients were observed. The mean duration of the post-take ward round per patient was 14 minutes (SD 4 minutes). The duration ranged from 7 minutes (a patient who had a stroke) to 23 minutes (a patient with a lower respiratory tract infection). The main tasks undertaken were history review and examination (mean 5.6 minutes, 27%), discussion with patients (mean 4.7 minutes, 22%) and communication within the nursing and medical team attending the round (mean 5.0 minutes, 24%). In 55% of the time units charted, consultants were performing predefined elements of the admission process concurrently rather than sequentially (eg obtaining aspects of the history from the patient while performing the examination).
Discussion
Modern hospitals are under huge pressure and their work practices are being forced to change. Traditionally, a junior doctor ‘clerked in’ a patient when they were admitted to hospital. This usually meant just doing a history and physical, inserting an intravenous line and taking a few preliminary blood samples. A definitive diagnosis and management plan was not agreed until the patient was reviewed by a senior physician. This review often did not take place until several hours, or even days, after the patient’s admission. Such a tardy approach to hospital care is no longer acceptable to patients, their relatives and, indeed, their physicians. Senior input into acute medical care as soon as possible has now become the accepted aspiration throughout the UK NHS. As a result, the admission process in hospitals has, over a period of years, been completely transformed.
It was clear from our results that the time required to undertake key tasks of the admission process reduces with increasing seniority: senior members of the team (consultants) were more able to perform elements of the admission process concurrently, whereas less experienced members (FY1s) did so sequentially. Patients clerked by consultants did not require time for senior review. In times of increased demand, consultants in our unit work in the same way as doctors in training, thus creating surge capacity and a flat hierarchy while being able to delegate some supporting tasks such as prescribing, documentation and requesting of investigations. While this might be positive for service, it creates a potential dilemma for training if the consultant service provision is at the expense of supervision and training of junior doctors.
Disappointingly, the review by an ED doctor did not seem to impact on the time it took for a doctor from the medical on-call team to review a patient. In order to understand the reasons for this, we reviewed case notes: matching terms from the documentation of ED doctors, documentation of medical on-call doctors and records of AMU nurses showed a large overlap in recorded data items. For one patient, 67 of 82 words in the ED clerking for history of presenting complaint were repeated verbatim in the medical unit documentation suggesting that this repeat clerking is a ‘futile clinical cycle’ that provides limited or no benefit.20
Previous studies have shown that doctors spend most of their time on indirect tasks and administrative duties and only 23% on direct care for patients.9 A study in a Dundee ED demonstrated that senior house officers showed a significant rise in performance between the first and last month of their attachment.10 Our results support the notion that junior doctors need to be allowed the time to gain the experience and knowledge to allow them to progress.
Documentation takes up the largest proportion of time, no matter what grade the doctor is. Our study showed that 41% of time is spent on documentation, which is more than previous studies have shown in EDs and other countries.11–14 This may reflect the use of a detailed pro forma on our medical admission unit.
A large proportion of the time taken on clinical encounters is spent on communication with patients and their relatives. This is essential to establish the good doctor–patient relationships required for compassionate and effective care and cannot be compromised.
There was a high frequency of interruptions, particularly for the most junior doctors. This may reflect the culture of hierarchy, where staff feel it is more acceptable to interrupt the more junior members of the team. Such interruptions are potentially dangerous because they have been shown to lead to clinical errors.15
Our study is limited by its sample size. However, this does not invalidate the principle of the work. In order to improve resource optimisation (and possibly patient experience) it is necessary to measure processes. The duration of these processes will depend on local context, such as the layout of a unit, the quality of the IT support and the availability of old records. Documentation is the part of the admission process that takes the most time and it is possibly amenable to intervention: electronic records are, in theory, able to pre-populate many data fields from previous encounters and this might cut down on pure clerical tasks. In order to calculate optimised local team sizes these factors and the skill-mix of the team need to be taken into account. In order to generate optimised distribution of staff shifts, fluctuations in workload and the application of principles of queuing theory need to be understood.16
Timings might have been influenced by the ‘Hawthorne effect’.17 We are unable to estimate whether unobserved encounters would be slower or faster. Additionally, we might not have captured data for tasks done for a particular patient that were performed significantly later than the observed time (eg reviewing and acting upon delayed results). Limited senior reviews were captured but this may reflect a bigger problem with team structures.18
Workload distribution and staffing might have a serious impact on clinical outcomes. Increased consultant presence has been shown to be associated with reduced case-adjusted mortality rates in at least one publication.19
From our work, two principles of workload distribution are clear:
Senior doctors might take less time, but taking less time does not necessarily equate with greater accuracy or quality of the clerking. At the same time, trainees need to be allowed time to gain experience and develop into safe and efficient senior doctors in the future. One way to improve efficiency may be for consultants to focus their time on patients who might potentially have a quick turnaround and be discharged from the unit the same day.
It is possible to derive estimates for the size of a workforce that is needed to run a unit from observation of existing work practice. When considering staffing levels on AMUs, it is important to take into consideration the local set up and additional on-call responsibilities. Adopting a ‘supply and demand’ method of determining clinical staffing needs may be useful20 but this requires units to understand their own local processes rather than performing repeated ‘futile cycles’ with little or no added value.21 While the temptation might be to use minimum staffing numbers based on mathematical models, it is also clear that safe systems need redundancy to handle unexpected surges in demand from within the medical admissions unit and from crisis on general wards. This is not something we have studied in this piece of work.
Conclusion
Staffing requirements for acute units are affected by complex factors. Assessment of the workload and review of care processes are key to identifying areas for improvement and helping staff to work in a safe, efficient manner. We have established some building blocks to help develop optimum staffing levels in our unit but further work is required. Increased usage of data and modeling of workflow is needed to improve performance and patient safety while maintaining service sustainability.
Conflicts of interest
The authors declare no conflicts of interests.
References
- 1.Department of Health Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London:: Department of Health; 2013. Available online at www.midstaffspublicinquiry.com/report. [22 June 2016]. [Google Scholar]
- 2.Department of Health Berwick review into patient safety. London:: Department of Health; 2013. [Google Scholar]
- 3.National Institute for Health and Care Excellence Safe staffing for nursing in adult inpatient wards in acute hospitals. London:: NICE; 2014. Safe staffing guideline No 1. [Google Scholar]
- 4.Sabin J. Subbe CP. Vaughan L, et al. Safety in numbers: lack of evidence to indicate the number of physicians needed to provide safe acute medical care. Clin Med. 2014;14:462–7. doi: 10.7861/clinmedicine.14-5-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Royal College of Physicians Acute care toolkit 4: Delivering a 12-hour, 7-day consultant presence on the acute medical unit. London:: RCP; 2012. [Google Scholar]
- 6.Bell D. Lambourne A. Percival F. Laverty AA. Ward DK. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS One. 2013;8:e61476. doi: 10.1371/journal.pone.0061476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mueller SK. Call SA. McDonald FS, et al. Impact of resident workload and handoff training on patient outcomes. Am J Med. 2012;125:104–10. doi: 10.1016/j.amjmed.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Rockwood K. Song X. MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tipping MD. Forth VE. Magill DB. Englert K. Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med. 2010;5:353–9. doi: 10.1002/jhm.647. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong PA. White AL. Thakore S. Senior house officers and foundation year doctors in emergency medicine: do they perform equally? A prospective observational study. Emerg Med J. 2008;25:725–7. doi: 10.1136/emj.2008.059154. [DOI] [PubMed] [Google Scholar]
- 11.Ghazanfar MN. Honore PH. Nielsen TR. Andersen SE. Rasmussen M. Hospital admission interviews are time-consuming with several interruptions. Dan Med J. 2012;59:A4534. [PubMed] [Google Scholar]
- 12.Westbrook JI. Ampt A. Kearney L, et al. All in a day’s work: an observational study to quantify how and with whom doctors on hospital wards spend their time. Med J Aust. 2008;188:506–9. doi: 10.5694/j.1326-5377.2008.tb01762.x. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell J. Hayhurst C. Robinson SM. Can a senior house officer’s time be used more effectively? Emerg Med J. 2004;21:545–7. doi: 10.1136/emj.2003.007088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ammenwerth E. Spötl HP. The time needed for clinical documentation versus direct patient care. A work-sampling analysis of physicians’ activities. Methods Inf Med. 2009;48:84–91. [PubMed] [Google Scholar]
- 15.Coiera EW. Jayasuriya RA. Hardy J, et al. Communication loads on clinical staff in the emergency department. Med J Aust. 2002;176:415–8. doi: 10.5694/j.1326-5377.2002.tb04482.x. [DOI] [PubMed] [Google Scholar]
- 16.Green LV. Soares J. Giglio JF. Green RA. Using queueing theory to increase the effectiveness of emergency department provider staffing. Acad Emerg Med. 2006;13:61–8. doi: 10.1197/j.aem.2005.07.034. [DOI] [PubMed] [Google Scholar]
- 17.Wickstray G. Bendix T. The “Hawthorne effect”– what did the original Hawthorne studies actually show? Scand J Work Environ Health. 2000;26:363–7. [PubMed] [Google Scholar]
- 18.Chaponda M. Borra M. Beeching NJ, et al. The value of the post-take wardround: are new working patterns compromising junior doctor education? Clin Med. 2009;9:323–6. doi: 10.7861/clinmedicine.9-4-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bell D. Lambourne A. Percival F. Laverty AA. Ward DK. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS One. 2013;8:e61476. doi: 10.1371/journal.pone.0061476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Jeune IR. Simmonds MJ. Poole L. Patient need at the heart of workforce planning: the use of supply and demand analysis in a large teaching hospital’s acute medical unit. Clin Med. 2012;12:312–6. doi: 10.7861/clinmedicine.12-4-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buist MD. How I nearly MET my maker: a story of clinical futile cycles and survival. Jt Comm J Qual Patient Saf. 2010;36:334–6. doi: 10.1016/s1553-7250(10)36050-8. [DOI] [PubMed] [Google Scholar]