Abstract
Background and Objective
Aboriginal peoples are at a higher risk of many chronic respiratory diseases compared to the general Canadian population. Patients with asthma-COPD overlap (ACO), a disease newly described in 2015, are associated with frequent exacerbations, rapid decline in lung function, poor quality of life, high mortality, and disproportionate utilization of health-care resources than patients with asthma and COPD alone. The objective was to investigate the prevalence and risk factors of ACO in Aboriginal peoples.
Methods
Data from the 2012 Aboriginal Peoples Survey (APS) were used for this study. The ACO definition was based on the respondent giving positive responses to both of the following questions “Do you/Does (name) have Asthma diagnosed by a health professional?” and “Do you/Does (name) have chronic bronchitis, emphysema or chronic pulmonary obstructive disease or COPD diagnosed by a health professional?” Results. Aboriginal peoples older than 45 years, women, widowed, separated, or divorced, having a total personal income below $20,000 were associated with a significant risk of ACO. Residing in Ontario, being a daily smoker, living in a rented dwelling, dwelling in need of major repairs, having diabetes, and working more than 40 hrs a week were also significantly associated with increased risk of ACO.
Conclusion
The results from this study will provide information to aid the development of prevention and intervention strategies for Aboriginal communities.
1. Introduction
Aboriginal peoples are at a higher risk of many chronic respiratory diseases compared to the general Canadian population [1–3]. A recent Canadian survey showed that approximately 15% of Aboriginal peoples had been diagnosed with at least one of the chronic respiratory diseases (chronic obstructive pulmonary disease (COPD), chronic bronchitis (CB), emphysema, and asthma) compared to 10% for non-Aboriginal peoples in Canada [4]. Inequalities in health status often result from social, cultural, economic, environmental, and political factors. Education level, occupation, income, rurality, accessibility to health care, and possible interplays between these determinants of health can lead to disparities. A higher prevalence of chronic respiratory diseases in Aboriginal peoples has been associated with many factors including higher smoking rate, poor housing, poor schooling, low household income, and lack of timely access to health care [5].
Obstructive airway diseases including asthma and COPD have been associated with social, economic, and health impact on individuals, families, and society in general [6]. In a US study, the prevalence of adult asthma was reported to be 7.7% in those aged 35–64 years, while the prevalence of COPD was between 6.6% and 9.2% across the age group of 45 to 64 years, and even higher from 11.6% to 12.1% across age 65 years and older [7, 8]. Recently, a new obstructive airway disease, the asthma-COPD overlap (ACO) was described, with its first treatment and management guidelines reported in 2015 [9]. However, little information is currently available including the prevalence of ACO and its associated risk factors. A recent study from Finland suggested that the prevalence of ACO was about 27% in asthma patients with a smoking history [10]. Another study suggested that about 10 to 20% of patients with COPD may have ACO [11].
Patients with ACO experience a greater health burden including worse respiratory symptoms, poorer health-related quality of life (QOL), frequent exacerbations leading to more emergency visits, comorbidities, and higher doses of medications, as compared to asthma and COPD alone [6, 12–14]. Given that Aboriginal peoples are at a higher risk of chronic respiratory diseases [1, 2, 15], there is a need to study the prevalence and risk factors of this new disease (ACO) in Aboriginal people. Data from the 2012 Aboriginal Peoples Survey (APS), a national survey with detailed information on the demographic, environmental, health, and lifestyle status of Aboriginal peoples provided a unique platform to address these questions.
2. Methods
2.1. Study Design
Data from the 2012 APS collected by Statistics Canada from February to July 2012 were used for this study. This is a national cross-sectional survey of First Nations living off reserve, Metis and Inuit. It collected detailed information on Aboriginal identity, education, culture, income, health status, housing, and family background. Respondents were chosen based on self-identification as being Aboriginal or having Aboriginal ancestry from the 2011 National Health Survey (NHS). This study included only Aboriginal peoples aged ≥12 years from whom the information on the diagnosis of COPD was collected.
2.2. Outcome Variable and Risk Factors
The primary outcome variable ACO was based on the respondent giving positive responses to both of the following questions “Do you/Does (name) have Asthma diagnosed by a health professional?” and “Do you/Does (name) have chronic bronchitis, emphysema, or chronic pulmonary obstructive disease or COPD diagnosed by a health professional?”
The variables of interest were categorized into Demographic, Environmental, Socioeconomic, and Lifestyle variables and other diseases. Demographic variables consist of Age, Sex, and Marital Status. Environmental variables consist of Rural or Urban (This is defined by the NHS Population Centre size); Province; Dwelling—owned or rented; Dwelling—need repairs; and Number of people in a household/Number of rooms in a dwelling. Socioeconomic variables consisted of Total Personal Income and Employment—the number of paid hours per week. Lifestyle variables consisted of Smoking Status and Anybody smoking in the dwelling and other diseases such as Diabetes.
2.3. Statistical Analysis
Mean (standard deviation) and count (frequency) were calculated for continuous and categorical variables, respectively. Sampling weights were included in all statistical analyses. PROC SURVEYLOGISTIC was used to identify the significant risk factors for ACO in the univariate and multivariate analysis. Only clinically important factors and variables with a p-value lower than 0.20 in the univariate analysis were included in the multivariate analysis. To account for complex survey design of the APS, variances were estimated using 1,000 bootstrap weights with a Fay adjustment factor of 0.75. The level of significance α = 0.05 was used for the multivariate logistic regression. Data analysis was conducted using SAS version 9.4.
3. Results
3.1. Descriptive Statistics
The distribution of the population is shown in Table 1. The prevalence of ACO in the aboriginal population was 2.7%.
Table 1.
Descriptive statistics for the variables in our study.
| Variables | Labels | % of the population |
|---|---|---|
| Age | 12 to 34 | 45 |
| 35 to 44 | 17 | |
| 45 to 54 | 18 | |
| 55 to 64 | 12 | |
| 65 and over | 8 | |
|
| ||
| Sex | Men | 46 |
| Women | 54 | |
|
| ||
| Marital status | Married and living common-law | 48 |
| Widowed, separated, and divorced | 14 | |
| Single, never married | 38 | |
|
| ||
| Rural or urban | Rural area | 24 |
| Small population centre | 21 | |
| Medium population centre | 12 | |
| Large urban population centre | 43 | |
|
| ||
| Personal income | $5000 or less income | 18 |
| $5000 to $19,999 | 28 | |
| $20,000 to 49,999 | 32 | |
| $50,000 to $100,000 and over | 23 | |
|
| ||
| Province | Atlantic∗ | 8 |
| Quebec | 10 | |
| Ontario | 25 | |
| Prairies | 36 | |
| British Columbia | 17 | |
| Territories∗∗ | 4 | |
|
| ||
| Smoking status | Daily | 28 |
| Occasionally | 9 | |
| Not at all | 63 | |
|
| ||
| Anybody smoking at home | Yes | 64 |
| No | 36 | |
|
| ||
| Dwelling (owned/rented) | Owned | 58 |
| Rented | 42 | |
|
| ||
| Dwelling in need of major repairs | Yes, major repairs are needed | 12 |
| Yes, minor repairs are needed | 26 | |
| No, only regular maintenance is needed | 62 | |
|
| ||
| Diabetes | Diabetes type 1 and type 2 | 9 |
| Gestational and no diagnosis of diabetes | 91 | |
|
| ||
| How many rooms are there in a dwelling | 0 and 2 rooms | 6 |
| 3 and 5 rooms | 45 | |
| 6 and 8 rooms | 33 | |
| 9 rooms and over | 16 | |
|
| ||
| Number of paid hours per week | 0 to 20 hours | 8 |
| 21 to 40 hours | 37 | |
| 41 to 79 hours | 9 | |
| 80 hours and over | 46 | |
∗Including Nova Scotia, Newfoundland and Labrador, Prince Edward Island, and New Brunswick. ∗∗Including Nunavut, Yukon, and Northwest Territories.
Examinations of demographic variables showed that almost half the population was between the age of 12 to 34 years (45%) followed by those aged 35 to 44 years (17%), 45 to 54 years (18%), 55 to 64 years (12%), and 65 years and over (8%). Fifty-four percent of the sample were Women. Married and Living in common-law represented the highest proportion of 48% followed closely by Single and never married (38%) while the Widowed, separated, and divorced group was 14%.
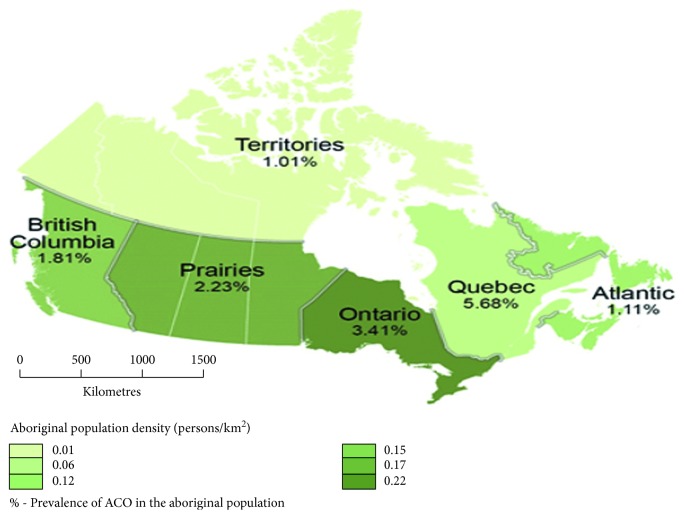
Examination of environmental variables showed that individuals from a Large urban population centre (100,000 or more) represented the highest proportion (43%), followed by Rural area, which was 24%, and Small population centre (1,000 to 29,999) was 21% while the Medium population centre (30,000 to 99,999) had the least at 12%. Aboriginal people residing in the Prairies (Alberta, Manitoba, Saskatchewan) had the highest proportion (36%), followed by Ontario (25%), British Columbia (17%), Quebec (10%), Atlantic Canada (Nova Scotia, Newfoundland and Labrador, Prince Edward Island, and New Brunswick) (8%) while the Territories (Nunavut, Yukon, Northwest Territories) had the lowest (4%) (Figure 1). Dwellings that needed only regular maintenance recorded the highest proportion (62%) while dwellings that required major repairs yielded a proportion of (12%). Most people living in a dwelling of 3 to 5 rooms yielded 45%, 6 to 8 rooms recorded 33%, 9 rooms and over recorded 16% while the least proportion was 0 to 2 rooms with 6%.
Figure 1.
Map showing the Aboriginal population density and prevalence of ACO geographically in Canada.
Examination of socioeconomic status showed that individuals who earn $20,000 to 49,999 per year had the highest proportion (32%), followed by those that earn between $5,000 to 19,999 (28%). Individuals earning $50,000 to $100,000 and over were 23% while the lowest proportion was $5,000 or less with 18%. About employment hours per week, individuals working 80 hours and above recorded the highest proportion (46%), 21 to 40 hours yielded 37%, and 41 to 79 hours per week and working part-time of 0 to 20 hours yielded 9% and 8%, respectively. Individuals that Owned a dwelling had a higher proportion (58%) when compared to those that Rent a dwelling (42%).
Examination of lifestyle variables showed that individuals that smoked Daily had a proportion of 28% while those that smoked Occasionally recorded a lower proportion (9%). Individuals that Smoke at home recorded a proportion of 64% when compared to those that do not smoke at home (36%). Diabetes (type 1 and 2) was reported to be 9% of the respondents.
3.2. Univariate Analysis
The results from the Univariate analysis are shown in Table 2. Age was significantly associated with ACO. In comparison to those aged 12-34 years, individuals who were older than 45 years were about three times more likely to have ACO. Women were two times more likely to be associated with ACO than Men. In comparison to those Married or Living in common-law, individuals who were Widowed, Separated, and Divorced and Single and never married were more likely to be associated with higher risks of ACO.
Table 2.
Univariate analysis of the risk factors associated with the prevalence of ACO.
| Variables | Prevalence of ACO | Odds ratio (95% CI) | p value |
|---|---|---|---|
| Age | |||
| 12 to 34 | 1.57 | 1 | |
| 35 to 44 | 1.68 | 1.07 (0.62–1.84) | 0.8045 |
| 45 to 54 | 4.31 | 2.81 (1.71–4.61) | <0.0001 |
| 55 to 64 | 4.28 | 2.80 (1.71–4.59) | <0.0001 |
| 65 and over | 4.88 | 3.20 (1.89–5.43) | <0.0001 |
| Sex | |||
| Men | 1.65 | 1 | |
| Women | 3.53 | 2.18 (1.58–3.00) | <0.0001 |
| Marital status | |||
| Married and living common-law | 1.87 | 1 | |
| Widowed, separated, and divorced | 6.76 | 3.80 (2.48–5.84) | <0.0001 |
| Single, never married | 2.64 | 1.42 (1.01–2.00) | <0.0001 |
| Rural or urban | |||
| Large urban population centre | 3.00 | 1 | |
| Rural area | 2.17 | 0.72 (0.48–1.06) | 0.0953 |
| Small population centre | 2.00 | 0.66 (0.45–0.98) | 0.0370 |
| Medium population centre | 3.63 | 1.22 (0.74–2.00) | 0.4346 |
| Personal income | |||
| $5000 to $19,999 | 5.85 | 1 | |
| $5000 or less income | 2.12 | 0.35 (0.22–0.55) | <0.0001 |
| $20,000 to 49,999 | 2.18 | 0.36 (0.25–0.53) | <0.0001 |
| $50,000 to $100,000 and over | 0.81 | 0.13 (0.07–0.24) | <0.0001 |
| Province | |||
| Ontario | 3.41 | 1 | |
| Atlantic∗ | 1.11 | 0.32 (0.18–0.59) | 0.0002 |
| Quebec | 5.68 | 1.72 (1.05–2.81) | 0.0320 |
| Prairies | 2.23 | 0.65 (0.42–1.00) | 0.0471 |
| British Columbia | 1.81 | 0.52 (0.32–0.86) | 0.0100 |
| Territories∗∗ | 1.01 | 0.29 (0.17–0.51) | <0.0001 |
| Type of smoker | |||
| Not at all | 1.89 | 1 | |
| Daily | 4.47 | 2.42 (1.78–3.32) | <0.0001 |
| Occasionally | 2.38 | 1.26 (0.72–2.20) | 0.4112 |
| Anybody smoking at home | |||
| No | 2.38 | 1 | |
| Yes | 4.21 | 2.04 (1.42–2.94) | 0.0001 |
| Dwelling (owned/rented) | |||
| Owned | 1.58 | 1 | |
| Rented | 4.12 | 2.69 (1.95–3.70) | <0.0001 |
| Dwelling in need of major repairs | |||
| No, only regular maintenance is needed | 2.01 | 1 | |
| Yes, major repairs are needed | 6.44 | 3.35 (2.19–5.13) | <0.0001 |
| Yes, minor repairs are needed | 2.47 | 1.24 (0.86–1.78) | 0.2525 |
| Diabetes | |||
| Gestational and no diagnosis of diabetes | 2.24 | 1 | |
| Diabetes type 1 and type 2 | 7.20 | 3.38 (2.34–4.90) | <0.0001 |
| How many rooms are there in a dwelling | |||
| 0 and 2 rooms | 5.58 | 1 | |
| 3 and 5 rooms | 3.70 | 0.65 (0.38–1.11) | 0.1136 |
| 6 and 8 rooms | 1.87 | 0.32 (0.16–0.63) | 0.0010 |
| 9 rooms and over | 1.23 | 0.21 (0.10–0.44) | <0.0001 |
| Number of paid hours per week | |||
| 0 to 20 hours | 1.19 | 1 | |
| 21 to 40 hours | 1.22 | 1.03 (0.50–2.11) | 0.9402 |
| 41 to 80 hours | 2.09 | 1.77 (0.75–4.17) | 0.1887 |
| 80 hours and over | 4.21 | 3.65 (1.82–7.32) | 0.0003 |
∗Including Nova Scotia, Newfoundland and Labrador, Prince Edward Island, and New Brunswick. ∗∗Including Nunavut, Yukon, and Northwest Territories.
Individuals from the Small population centre were significantly less likely to be associated with ACO in comparison to individuals from a Large urban population centre. In comparison to Ontario, other provinces and regions were significantly less likely to be associated with ACO except for Quebec. Individuals residing in a dwelling in need of major repairs were three times more likely to be associated with ACO compared to those that reside in a dwelling that needs only regular maintenance. In comparison to those living in a dwelling of 0 to 2 rooms, individuals living in a dwelling with 6–8 rooms and 9 rooms and over were significantly less likely to be associated with ACO.
Among the socioeconomic variables, individuals who earn between $5,000 or less to $100,000 and over were significantly less likely to be associated with ACO in comparison to individuals who earn $5,000 to 19,999. Individuals who worked 80 hours and over were approximately four times more likely to be associated with increased risk for ACO when compared to 0 to 20 hours of paid hours per week. Also, individuals living in the rented dwelling were three times more likely to be associated with ACO when compared to those owning the dwelling.
Among lifestyle variables, Daily smoking was more than two times more likely to be associated with ACO in comparison to individuals reporting No smoking at all. Furthermore, individuals with a report of smoking at home were two times more likely to be associated with ACO when compared to those with report Not smoking at home. Individuals who report a diagnosis of Diabetes type 1 and 2 were three times more likely to be associated with ACO compared to those without the diagnosis of diabetes.
3.3. Multivariate Analysis
As shown in Table 3, the results from the multivariate analysis showed the following demographic variables were significantly associated with ACO: individuals aged between 45 and 54 years were two times more likely to be associated with ACO in comparison to individuals aged between 12 and 34 years. Women were approximately two times more likely to be associated with ACO compared to Men. Also, individuals who were widowed, separated, or divorced were two times more likely to be associated with ACO compared to individuals who were either married or living in common-law.
Table 3.
Multivariate analysis of the risk factors associated with the prevalence of ACO.
| Variables | Labels | Odds ratio (95% CI) | p value |
|---|---|---|---|
| Age | 12 to 34 | 1 | |
| 35 to 44 | 1.01 (0.54 to 1.87) | 0.9858 | |
| 45 to 54 | 2.43 (1.34 to 4.42) | 0.0035 | |
| 55 to 64 | 2.00 (0.97 to 4.09) | 0.0597 | |
| 65 and over | 1.68 (0.71 to 3.99) | 0.2406 | |
|
| |||
| Sex | Men | 1 | |
| Women | 1.74 (1.25 to 2.45) | 0.0013 | |
|
| |||
| Marital status | Married and living common-law | 1 | |
| Widowed, separated, and divorced | 1.97 (1.19 to 3.25) | 0.0080 | |
| Single, never married | 1.44 (0.94 to 2.20) | 0.0908 | |
|
| |||
| Personal income | $50,000 to $100,000 and over | 1 | |
| $5000 or less income | 1.59 (0.71 to 3.54) | 0.2559 | |
| $5000 to $19,999 | 3.00 (1.44 to 6.23) | 0.0033 | |
| $20,000 to 49,999 | 1.80 (0.89 to 3.66) | 0.1019 | |
|
| |||
| Province | Ontario | 1 | |
| Atlantic∗ | 0.31 (0.16 to 0.61) | 0.0007 | |
| Quebec | 1.58 (0.94 to 2.64) | 0.0834 | |
| Prairies | 0.73 (0.47 to1.14) | 0.1660 | |
| British Columbia | 0.51 (0.30 to 0.88) | 0.0158 | |
| Territories∗∗ | 0.21 (0.12 to 0.39) | <0.0001 | |
|
| |||
| Type of smoker | Not at all | 1 | |
| Daily | 1.66 (1.14 to 2.41) | 0.0084 | |
| Occasionally | 1.10 (0.52 to 2.00) | 0.9896 | |
|
| |||
| Dwelling (owned/rented) | Owned | 1 | |
| Rented | 1.76 (1.24 to 2.51) | 0.0018 | |
|
| |||
| Dwelling in need of major repairs | No, only regular maintenance is needed | 1 | |
| Yes, major repairs are needed | 2.31 (1.46 to 3.65) | 0.0004 | |
| Yes, minor repairs are needed | 1.15 (0.79 to 1.69) | 0.4579 | |
|
| |||
| Diabetes | Gestational and no diagnosis of diabetes | 1 | |
| Diabetes type 1 and type 2 | 1.68 (1.10 to 2.58) | 0.0188 | |
|
| |||
| Number of paid hours per week | 0 to 20 hours | 1 | |
| 21 to 40 hours | 1.16 (0.55 to 2.44) | 0.7004 | |
| 41 to 80 hours | 2.83 (1.12 to 7.14) | 0.0273 | |
| 80 hours and over | 2.85 (1.36 to 5.97) | 0.0057 | |
∗Including Nova Scotia, Newfoundland and Labrador, Prince Edward Island, and New Brunswick. ∗∗Including Nunavut, Yukon, and Northwest Territories.
In comparison to individuals from Ontario, those from Atlantic regions, Territories, and British Columbia were significantly less likely to be associated with ACO. Also, individuals living in a dwelling in need of major repairs were two times more likely to be associated with ACO compared to those living in a dwelling in need of regular maintenance.
Among the socioeconomic variables, the following three variables were significantly associated with ACO: Individuals who earn between $5,000 and $19,999 were three times more likely to be associated with ACO compared to those who earn $50,000 to $100,000 and over. Individuals working for long hours of 41 to 80 hours and 81 hours and over were significantly associated with ACO compared to those working 0 to 20 hours per week. Also, individuals who live in a rented dwelling were approximately two times more likely to be associated with ACO than those owning a dwelling.
Smoking was significantly associated with ACO: individuals who smoke daily were found to be about two times more likely to be associated with ACO compared to those that do not smoke at all. Aboriginal people with diabetes (type 1 and 2) were also approximately two times more likely to develop ACO compared to those without the diagnosis of diabetes.
4. Discussion
Using the APS dataset, our results suggest that Aboriginal peoples older than 45 years, women, widowed, separated, or divorced having a total personal income below $20,000 were associated with a significant risk of ACO. Residing in Ontario, being a daily smoker, living in a rented dwelling, dwelling in need of major repairs, having diabetes, and working more than 40 hrs a week were also significantly associated with increased risk of ACO.
Individuals aged 45 to 54 years old are two times more likely to be associated with ACO when compared to the younger individuals aged 12 to 34 years. In a longitudinal population-based study in the Netherlands, the authors reported that the risk of being diagnosed with COPD increased with age. A man who was free of COPD at age 40 had an increased risk of being diagnosed with COPD from 0.8% to 12% with increasing years from 10 to 40 years; while a woman of the same age had increased risk from 0.8% to 8.3% [16]. In another population-based cohort study from Ontario, Canada, estimating trends in the prevalence and incidence of concurrent physician-diagnosed asthma and COPD, the authors reported that the standardized prevalence increased by 10.5% from 2002 to 2012 mainly in young adults [17]. Additionally, a cross-sectional study among Aboriginal people assessed the risk factors associated with COPD. It was reported that individuals aged 55 and older were significantly associated with the risk of COPD [18]. We could find no other studies that focused on Aboriginal peoples with ACO.
Chronic respiratory diseases, especially COPD have always been attributed to men older than 40 years. However, recent findings suggest that there is a growing increase in women diagnosed with COPD. In a study of 1,633 residents from Saskatchewan, Canada, it was reported that in women, the combined effect of grain farming and smoking history had a significant association with CB but not in men [19]. Another study assessing the prevalence of CB in Aboriginal peoples reported that women had a higher prevalence than men [4]. Additionally, women with more severe COPD have a higher risk of hospitalization and death due to respiratory failure and possible comorbidities when compared to men [20]. Our study that appears to be the first to assess the risk of ACO in Aboriginal peoples suggests that Aboriginal women are approximately two times more likely to report ACO compared to men.
The association between obstructive airway diseases and marital status has been examined in many population studies. In a study, patients diagnosed with COPD were described and compared based on their nutritional status, gender, pulmonary function, and marital status. The authors reported that individuals diagnosed with COPD who lived alone had a worse nutritional status [21]. A longitudinal study in the US focused on the psychological imbalance caused by bereavement and divorce in relation to COPD. It was reported that remarriage after bereavement or divorce was associated with a significantly decreased risk of COPD onset [22]. Our study showed that Widowed, Separated, and Divorced Aboriginal peoples were found to be two times more likely to be associated with ACO compared to those married or living common-law.
We reported significant geographic variation in the prevalence of ACO with people in Ontario being at a significantly higher risk of ACO compared to people from other provinces or regions. A study in Ontario, Canada, assessed individuals with asthma and COPD to see if higher levels of exposure to air pollution will increase the risk for ACO [23]. The authors reported that individuals exposed to higher levels of air pollution had nearly three times the risk of developing ACO [23]. The same group of researchers in a longitudinal cohort of women reported that the risk of COPD increased by more than 20% with each unit increase in exposure to PM2.5 [24].
In our study, we reported that Aboriginal peoples living in dwellings in need of major repairs were two times more likely to develop ACO. A study examining the differences in hospitalization for respiratory tract infections among First Nations using the 2006 census reported that poor housing conditions and income were contributing factors in hospitalization [25]. Another study from Saskatchewan, Canada, which assessed the prevalence of CB in two Aboriginal communities, reported that houses with a musty smell of mould were positively associated with CB [26]. This is also consistent with a study from the United States, which reported that 15% of people who reported a musty smell in their dwelling also reported CB and asthma [27].
Meanwhile, studies have shown that lower socioeconomic status is associated with respiratory diseases [28, 29]. Total personal income and paid employment hours in our study suggested Aboriginal peoples working over 40 hours a week and earning a low annual income of $20,000 were more likely to develop ACO when compared to Aboriginal peoples earning an income of $50,000 or greater and working same or fewer hours. A large population-based study of 8,028 individuals reported that low income and low quality of education were risk factors for asthma and COPD [29]. In a cross-sectional study that focused on the associated factors of COPD among Aboriginal peoples, the authors reported that Aboriginal peoples making less than the median income of $20,600 were at a higher risk to be associated with COPD [18].
There is still conflicting information about the impact of work hours on chronic respiratory diseases. A longitudinal study that continued for a 32-year period made use of the National Longitudinal Survey of Youth 1979. It collected information on job histories and work hours in relation to chronic disease status. The authors reported that there were no significant findings for an association between long hours and asthma [30]. This was not consistent with the result of our study. This could be due to the homogeneity of the Aboriginal population used in our study compared to the general population used in this longitudinal study. In a study that focused on housing conditions, it was reported that homeownership was related to home quality [31]. Poorly maintained houses could also lead to the loss of vapour barrier, which allows areas of dampness that are prone to contamination with mould [32]. Owned dwellings tend to have their repairs fixed quicker than rented dwellings. Our results suggest that individuals renting a dwelling are also approximately three times more likely to develop ACO when compared to owning a house.
In our study, individuals who smoke daily were found to be about two times more likely to be associated with ACO compared to those that do not smoke. Even though cigarette smoking has decreased considerably over the past decades, there is still a significant link between positive smoking or the exposure to environmental tobacco and respiratory diseases [10, 33–35]. Aboriginal peoples are observed to have higher smoking rates compared to the general Canadian population [5], but there are not many studies that have focused on the association between smoking and ACO. Kiljander et al. investigated the prevalence of ACO among 190 asthmatic patients with a smoking history. These patients had no previous diagnosis of COPD but were either current or ex-smokers with a history of at least ten pack years. It was reported that 27% of the patients were found to have ACO [10]. Another study from Sweden examining the association between environmental tobacco smoke (ETS) and risk of COPD showed that ETS was independently associated with COPD. However, the association was more significant with increased ETS exposure either at home, previous or current work, or at the three mentioned locations [33]. In two Aboriginal studies that investigated the factors associated with the prevalence of CB and COPD, daily or current smokers were significant compared to never smokers [4, 18].
In our study, Aboriginal peoples with a diagnosis of diabetes (either type 1 or type 2) were approximately two times more likely to develop ACO. Epidemiological studies have consistently reported that many socioeconomic and lifestyle factors such as smoking are significantly associated with both diabetes and chronic respiratory diseases [36, 37]. Pleasants et al. made use of the Behavioural Risk Factor Surveillance System (BRFSS) to assess the relationships between COPD, asthma, and comorbidities such as diabetes. It was reported that adults with overlap syndrome had the highest prevalence of diabetes [37].
In addition to the shared risk factors between chronic respiratory diseases and diabetes, the current medication for patients with asthma and COPD may also play a role. However, the results from different studies are not consistent. A nested case-control study from Quebec, Canada, assessed whether the use and dose of inhaled corticosteroids increase the risk of diabetes onset and progression in patients treated for respiratory diseases. It was reported that current use of inhaled corticosteroids was associated with a 34% increase in diabetes onset and progression while risks were even more significant at higher doses for the treatment of COPD [38]. Another study from Poland reported that concomitant diseases were diagnosed in 85% of patients with ACO, with the prevalence of diabetes being approximately 20% [39]. In contrast, a retrospective study evaluated whether there was an increased risk of new onset of diabetes or hyperglycemia among patients with asthma or COPD treated with inhaled corticosteroids. It was reported that treatment with inhaled corticosteroids in patients with asthma and COPD was not associated with increased risk of diabetes or hyperglycemia [40].
4.1. Limitations
There were several limitations to this study. The APS is a cross-sectional survey in which the information collected was gathered at a one-time period. This could lead to self-reporting bias or misclassification. Individuals self-reported the presence of asthma and COPD, which lacks clinical accuracy. All other answers in this survey were also self-reported, which could underestimate the prevalence of some variables.
5. Conclusion
To our knowledge, this is the first study to evaluate the prevalence and risk factors associated with ACO among Aboriginal peoples. Our study highlights the increasing prevalence of respiratory diseases in Aboriginal women. Even though ACO is a relatively new disease, our study still highlights the significance of smoking and dwelling in a house in need of major repairs, factors already known to be linked with respiratory diseases. Our study also highlights the association between ACO and concomitant diseases such as diabetes in Aboriginal peoples.
There is a need to better understand the burden and risk factors of ACO in Aboriginal peoples. The findings from this study will provide information to health-care workers, patients and their families, Indigenous governments/organizations, and government agencies.
Acknowledgments
This study was funded by the Seed, Bridge and Multidisciplinary Fund Committee and the Research and Graduate Studies, Memorial University of Newfoundland. The analysis presented in this paper was conducted at the Memorial University Research Data Centre, which is part of the Canadian Research Data Centre Network (CRDCN). The services and activities provided by the Memorial University Research Data Centre are made possible by the financial or in-kind support of the SSHRC, the CIHR, the CFI, the Statistics Canada, Seed, Bridge, Multidisciplinary Fund Committee, and the Memorial University of Newfoundland. The views expressed in this paper do not necessarily represent the CRDCN's or that of its partners. This study was approved by the Newfoundland and Labrador Health Research Ethics Board.
Data Availability
The 2012 Aboriginal Peoples Survey used to support the findings of this study has not been made available because it is not a publicly available dataset. It is available upon request from Statistics Canada.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Fraser-Lee N. J., Hessel P. A. Acute respiratory infections in the Canadian Native Indian population: a review. Canadian Journal of Public Health. 1994;85(3):197–200. [PubMed] [Google Scholar]
- 2.MacMillan H. L., MacMillan A. B., Offord D. R., Dingle J. L. Aboriginal health. Canadian Medical Association Journal. 1996;155(11):1569–1578. [PMC free article] [PubMed] [Google Scholar]
- 3.Sin D. D., Wells H., Svenson L. W., Man S. F. Asthma and COPD among aboriginals in Alberta, Canada. Chest. 2002;121(6):1841–1846. doi: 10.1378/chest.121.6.1841. [DOI] [PubMed] [Google Scholar]
- 4.Konrad S., Hossain A., Senthilselvan A., Dosman J. A., Pahwa P. Chronic bronchitis in Aboriginal people--prevalence and associated factors. Chronic Diseases and Injuries in Canada. 2013;33(4):218–225. [PubMed] [Google Scholar]
- 5.Senthilselvan A., Habbick B. F. Increased asthma hospitalizations among registered Indian children and adults in Saskatchewan, 1970-1989. Journal of Clinical Epidemiology. 1995;48(10):1277–1283. doi: 10.1016/0895-4356(95)00019-z. [DOI] [PubMed] [Google Scholar]
- 6.Bujarski S., Parulekar A. D., Sharafkhaneh A., Hanania N. A. The asthma COPD overlap syndrome (ACOS) Current Allergy and Asthma Reports. 2015;15(3) doi: 10.1007/s11882-014-0509-6. [DOI] [PubMed] [Google Scholar]
- 7.Moorman J. E., Akinbami L. J., Bailey C. M., et al. National surveillance of asthma: United States, 2001–2010. Vital and Health Statistics. 2012;35(35):1–58. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Chronic obstructive pulmonary disease among adults-United States, 2011. Morbidity and Mortality Weekly Report. 2012;61(46):938–943. [PubMed] [Google Scholar]
- 9.Global Initiative for Asthma (GINA) The Global Strategy for Asthma Management and Prevention. 2014. [Google Scholar]
- 10.Kiljander T., Helin T., Venho K., Jaakkola A., Lehtimaki L. Prevalence of asthma-COPD overlap syndrome among primary care asthmatics with a smoking history: a cross-sectional study. NPJ Primary Care Respiratory Medicine. 2015;25(1):p. 15047. doi: 10.1038/npjpcrm.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrecheguren M., Esquinas C., Miravitlles M. The asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): opportunities and challenges. Current Opinion in Pulmonary Medicine. 2015;21(1):74–79. doi: 10.1097/mcp.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 12.Gerhardsson de Verdier M., Andersson M., Kern D. M., Zhou S., Tunceli O. Asthma and chronic obstructive pulmonary disease overlap syndrome: doubled costs compared with patients with asthma alone. Value in Health. 2015;18(6):759–766. doi: 10.1016/j.jval.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Dang-Tan T., Ismaila A., Zhang S., Zarotsky V., Bernauer M. Clinical, humanistic, and economic burden of chronic obstructive pulmonary disease (COPD) in Canada: a systematic review. BMC Research Notes. 2015;8(1) doi: 10.1186/s13104-015-1427-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Postma D. S., Rabe K. F. The asthma-COPD overlap syndrome. New England Journal of Medicine. 2015;373(13):1241–1249. doi: 10.1056/nejmra1411863. [DOI] [PubMed] [Google Scholar]
- 15.Sin D. D., Wells H., Svenson L. W., Man S. F. Asthma and COPD among aboriginals in Alberta, Canada. Chest. 2002;121(6):1841–1846. doi: 10.1378/chest.121.6.1841. [DOI] [PubMed] [Google Scholar]
- 16.Afonso A. S., Verhamme K. M., Sturkenboom M. C., Brusselle G. G. COPD in the general population: prevalence, incidence and survival. Respiratory Medicine. 2011;105(12):1872–1884. doi: 10.1016/j.rmed.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 17.Kendzerska T., Sadatsafavi M., Aaron S. D., et al. Concurrent physician-diagnosed asthma and chronic obstructive pulmonary disease: a population study of prevalence, incidence and mortality. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173830.e0173830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bird Y., Moraros J., Mahmood R., Esmaeelzadeh S., Kyaw Soe N. M. Prevalence and associated factors of COPD among Aboriginal peoples in Canada: a cross-sectional study. International Journal of Chronic Obstructive Pulmonary Disease. 2017;12:1915–1922. doi: 10.2147/copd.s138304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Y., Horne S. L., McDuffie H. H., Dosman J. A. Combined effect of grain farming and smoking on lung function and the prevalence of chronic bronchitis. International Journal of Epidemiology. 1991;20(2):416–423. doi: 10.1093/ije/20.2.416. [DOI] [PubMed] [Google Scholar]
- 20.Prescott E., Bjerg A. M., Andersen P. K., Lange P., Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. European Respiratory Journal. 1997;10(4):822–827. [PubMed] [Google Scholar]
- 21.Odencrants S., Bjustrom T., Wiklund N., Blomberg K. Nutritional status, gender and marital status in patients with chronic obstructive pulmonary disease. Journal of Clinical Nursing. 2013;22(19-20):2822–2829. doi: 10.1111/jocn.12222. [DOI] [PubMed] [Google Scholar]
- 22.Noda T., Ojima T., Hayasaka S., Hagihara A., Takayanagi R., Nobutomo K. The health impact of remarriage behavior on chronic obstructive pulmonary disease: findings from the US longitudinal survey. BMC Public Health. 2009;9(1):p. 412. doi: 10.1186/1471-2458-9-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.To T., Zhu J., Larsen K., et al. Progression from asthma to chronic obstructive pulmonary disease. Is air pollution a risk factor? American Journal of Respiratory and Critical Care Medicine. 2016;194(4):429–438. doi: 10.1164/rccm.201510-1932oc. [DOI] [PubMed] [Google Scholar]
- 24.To T., Zhu J., Villeneuve P. J., et al. Chronic disease prevalence in women and air pollution—A 30-year longitudinal cohort study. Environment International. 2015;80:26–32. doi: 10.1016/j.envint.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 25.Carriere G. M., Garner R., Sanmartin C. Housing conditions and respiratory hospitalizations among First Nations people in Canada. Health Report. 2017;28(4):9–15. [PubMed] [Google Scholar]
- 26.Pahwa P., Karunanayake C. P., Rennie D. C., et al. Prevalence and associated risk factors of chronic bronchitis in First Nations people. BMC Pulmonary Medicine. 2017;17(1) doi: 10.1186/s12890-017-0432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shiue I. Indoor mildew odour in old housing was associated with adult allergic symptoms, asthma, chronic bronchitis, vision, sleep and self-rated health: USA NHANES, 2005-2006. Environmental Science and Pollution Research. 2015;22(18):14234–14240. doi: 10.1007/s11356-015-4671-8. [DOI] [PubMed] [Google Scholar]
- 28.Sahni S., Talwar A., Khanijo S., Talwar A. Socioeconomic status and its relationship to chronic respiratory disease. Advances in Respiratory Medicine. 2017;85(2):97–108. doi: 10.5603/arm.2017.0016. [DOI] [PubMed] [Google Scholar]
- 29.Kanervisto M., Vasankari T., Laitinen T., Heliovaara M., Jousilahti P., Saarelainen S. Low socioeconomic status is associated with chronic obstructive airway diseases. Respiratory Medicine. 2011;105(8):1140–1146. doi: 10.1016/j.rmed.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 30.Dembe A. E., Yao X. Chronic disease risks from exposure to long-hour work schedules over a 32-year period. Journal of Occupational and Environmental Medicine. 2016;58(9):861–867. doi: 10.1097/jom.0000000000000810. [DOI] [PubMed] [Google Scholar]
- 31.Kohen D. E., Bougie E., Guevremont A. Housing and health among Inuit children. Health Reports. 2015;26(11):21–27. [PubMed] [Google Scholar]
- 32.Dales R., Liu L., Wheeler A. J., Gilbert N. L. Quality of indoor residential air and health. Canadian Medical Association Journal. 2008;179(2):147–152. doi: 10.1503/cmaj.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hagstad S., Bjerg A., Ekerljung L., et al. Passive smoking exposure is associated with increased risk of COPD in never smokers. Chest. 2014;145(6):1298–1304. doi: 10.1378/chest.13-1349. [DOI] [PubMed] [Google Scholar]
- 34.Kauppi P., Kupiainen H., Lindqvist A., et al. Overlap syndrome of asthma and COPD predicts low quality of life. Journal of Asthma. 2011;48(3):279–285. doi: 10.3109/02770903.2011.555576. [DOI] [PubMed] [Google Scholar]
- 35.McIvor A. Tobacco control and nicotine addiction in Canada: current trends, management and challenges. Canadian Respiratory Journal. 2009;16(1):21–26. doi: 10.1155/2009/485953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin C. S., Liu C. C., Yeh C. C., et al. Diabetes risks and outcomes in chronic obstructive pulmonary disease patients: two nationwide population-based retrospective cohort studies. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0181815.e0181815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pleasants R. A., Ohar J. A., Croft J. B., et al. Chronic obstructive pulmonary disease and asthma-patient characteristics and health impairment. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2014;11(3):256–266. doi: 10.3109/15412555.2013.840571. [DOI] [PubMed] [Google Scholar]
- 38.Suissa S., Kezouh A., Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. American Journal of Medicine. 2010;123(11):1001–1006. doi: 10.1016/j.amjmed.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 39.Brzostek D., Kokot M. Asthma-chronic obstructive pulmonary disease overlap syndrome in Poland. Findings of an epidemiological study. Advances in Dermatology and Allergology. 2014;31(6):372–379. doi: 10.5114/pdia.2014.47120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Byrne P. M., Rennard S., Gerstein H., et al. Risk of new onset diabetes mellitus in patients with asthma or COPD taking inhaled corticosteroids. Respiratory Medicine. 2012;106(11):1487–1493. doi: 10.1016/j.rmed.2012.07.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The 2012 Aboriginal Peoples Survey used to support the findings of this study has not been made available because it is not a publicly available dataset. It is available upon request from Statistics Canada.