Abstract
The knowledge of the skeletal maturation and the stage of the growth of the patients seeking orthodontic treatment are of great value in planning efficient orthodontic therapy. However, different craniofacial structures of patient show variation in growth potential. The routine use of hand-wrist radiograph for growth prediction exposes the patient to extra radiation. Cervical vertebrae in the lateral cephalograph have been recommended as an alternative method. The pubertal growth spurt is a vital period in the orthodontic treatment and should be kept in mind when planning orthodontic treatment in growing children. One of the main objectives of taking hand and wrist radiograph is to determine the amount of growth and get used of it in patients with skeletal discrepancy during adolescence. Further, this will help in the selection of the appliances required, the course of the treatment and the retention after active orthodontic therapy.
KEYWORDS: Bjork system, cervical vertebrae, hand wrist radiograph, skeletal maturation
INTRODUCTION
The orthodontist deals with growing children and nongrowing adults. Most of the information concerning growth are obtained from cephalography and hand and wrist radiograph. Greulich and Pyle[1] have published atlas of hand and wrist radiographs of normal healthy children from birth to adulthood, at every 3-month interval. This atlas serves to compare and indicate the skeletal age of the patient.[1] The developmental stage of a child can be determined from several parameters such as height, weight, chronological age, secondary sexual characteristics, skeletal age, and dental age. However, skeletal age has been considered the most reliable method to assess the developmental status.[2,3]
Skeletal age is an indicator of physiological development and is distinct from the chronological age. The appearance and union of the different skeletal centers of ossification follows a pattern and schedule from birth to maturity. The radiographic assessment of the bone provides a valuable criterion of an individual's osseous maturation and is referred as the skeletal age.[4] The chronological age of a child may be accelerated of decelerated due to the individual variation of the timing of pubertal growth spurt.[2] Hence, chronological age cannot be considered as a reliable indicator for the evaluation of the maturity status of a child.[5] Thus, biological age or physiological age was considered.[6] Dental age estimation is based on the rate of development and calcification of tooth buds and the progressive sequence of their eruption in the oral cavity. Several methods have been developed to assess the dental age according to the degree of calcification observed in permanent teeth.[7,8,9] The relationship among the chronological, dental, and skeletal ages is important in diagnosis and treatment. Further, variations of dental and skeletal ages from known chronological age indicate changes in the standard growth pattern.[10]
The hand and wrist radiograph help in estimating the skeletal age of bone for determining the physical maturation status of the child.[11] The bone age is of great help to the orthodontist in coordinating the orthodontic therapy with the growth process. The idea of using hand and wrist radiograph for determining the skeletal age is that; the skeleton in hand and wrist region is made of several small bones; 27 small bones, distal ends of long bones radius and ulna. The development of these bones from the appearance of calcification centers to epiphyseal plate's closure occurs throughout the entire postnatal growth period and therefore provides a useful means of assessing skeletal maturity.[1,12]
Growth prediction can be estimated utilizing physiological parameters which include the peak of the growth velocity in standing height, pubertal markers, dental development, and radiological finding of skeletal maturation.[13] It was reported that the evaluation of skeletal maturation with the help of radiographs is considered to be the more reliable approach. The most preferred method is the use of hand-wrist radiographs.[14,15,16,17] The use of hand-wrist radiographs to examine skeletal maturity has been criticized as the patient is exposed to additional radiation. Therefore, analysis of the cervical spine[18] or of the frontal sinus[19] on lateral cephalographs was recommended as an alternative method. However, these methods do not give a precise prediction of how much growth left. The hand-wrist radiograph is commonly used for skeletal developmental assessment.[20,21] The Atlas of Greulich and Pyle[1] is the most frequently used method to evaluate skeletal age from hand-wrist radiographs.[22] Furthermore, the changes in the epiphysis of the middle phalanx of the third finger (MP3) follow an orderly sequence. Hägg and Taranger[23] studied pubertal growth from the stages of ossification of the middle phalanx of the third finger of the hand (MP 3 stages).
In orthodontic treatment planning, knowledge of facial growth velocity, and percentage of facial growth remains as a very important factor for effective growth modification interventions.[24] On the other hand, skeletal maturation staging from the radiographic analysis is a widely used approach to predict the timing of pubertal growth, to estimate growth velocity, and to estimate the proportion of growth remaining. The beginning of ossification of adductor sesamoid has been advocated by some authors as a reliable indicator of the onset of puberty.[14,25] Other investigators have stated that the appearance of the hook of hamate and the pisiform bone is also a good indicator of the onset of puberty.[26,27] Ghai et al.[28] concluded that hand, wrist and distal epiphysis of the radius and the ulna present a great number of secondary centers of ossification on the whole, and they can reproduce in a single radiograph. For this reason, they are often chosen as study centers when it is thought to determine the state of skeletal maturation, although other centers of ossification of secondary epiphysis can be used, such as the elbow and the tarsal bones. Some authors[29,30] have stressed the use of the hand radiographs to define the specific indicators of the spurt of pubertal growth. Comparison between the cervical vertebra and hand-wrist was used in other studies.[31,32,33,34]
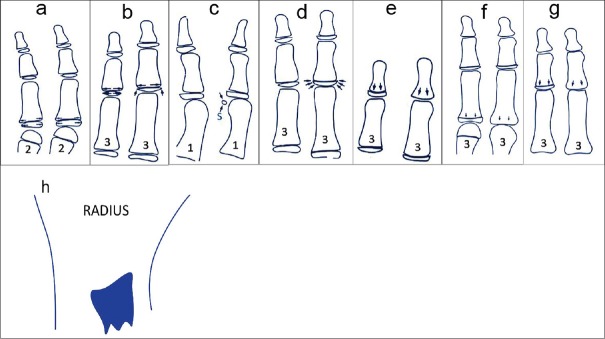
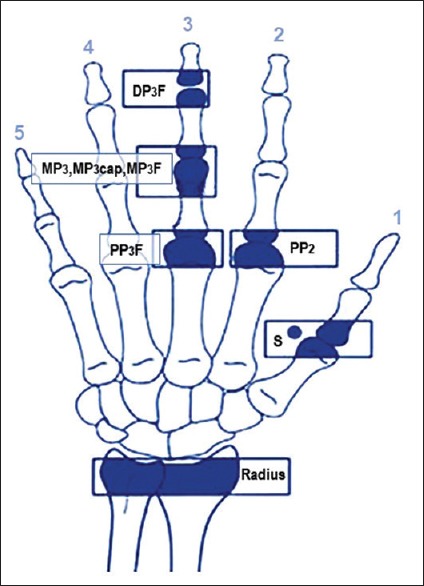
The purpose of hand and wrist radiograph analysis is to determine parameters such as patient's skeletal age, the amount of growth left and to determine whether to use functional appliance or to wait until growth ceased and performed extraction or surgery. Bjork and Helm[2] used four stages of bone maturation, all found at five anatomical sites located on the thumb, second finger, third finger, and radius. However, eight discrete adolescent skeletal maturity indicators covering the entire period of adolescent development are found on these five sites [Figures 1 and 2]. On the other hand, Fishman[20] used eleven indicators covering the entire period of development. The sequence of ossification progresses through four stages; A-Width of the epiphysis equal to the width of the Diaphysis. B-Sesamoid ossification (small calcified bone at the Thumb) C-Capping Stage. D-Fusion stage. The objective of this review is to give an overview of the current methods of skeletal age assessment and to highlight the simple method of hand-wrist radiograph as an indicator using Bjork system.
Figure 1.
Growth sites in hand and wrist
Figure 2.
Anatomy of the skeleton of the hand and wrist
MATERIALS AND METHODS
HAND AND WRIST RADIOGRAPH
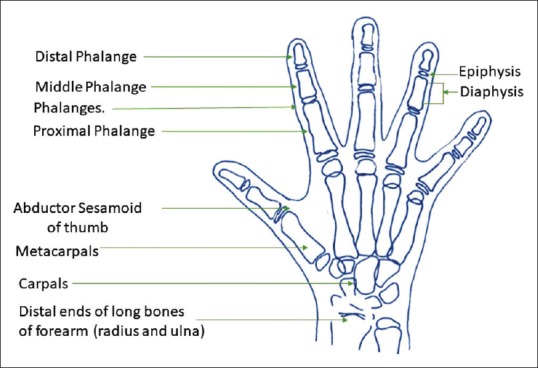
The skeleton of the hand and wrist is made of the following [Figure 2]:
Distal ends of long bones of the forearm (radius and ulna)
Carpals
Metacarpals
Phalanges.
The main components of hand and wrist are as follows:
Joint between radius and navicular (Scaphoid) bones (radiocarpal joint)
Joint between the trapezium and first metacarpal bones (carpometacarpal joint)
First metacarpophalangeal joint
Interphalangeal joint of the thumb
Proximal interphalangeal joint
Middle inter-phalangeal joint
Distal interphalangeal joint.
Each phalange consists of epiphysis and diaphysis. The development of the epiphysis and diaphysis of growing child not only differs in the timing of the maturational events (width, ossification, capping, and fusion [Figure 3] but also in the sequence of these events. On the other, the development stage has considerable influence on orthodontic diagnosis and treatment planning.
Figure 3.
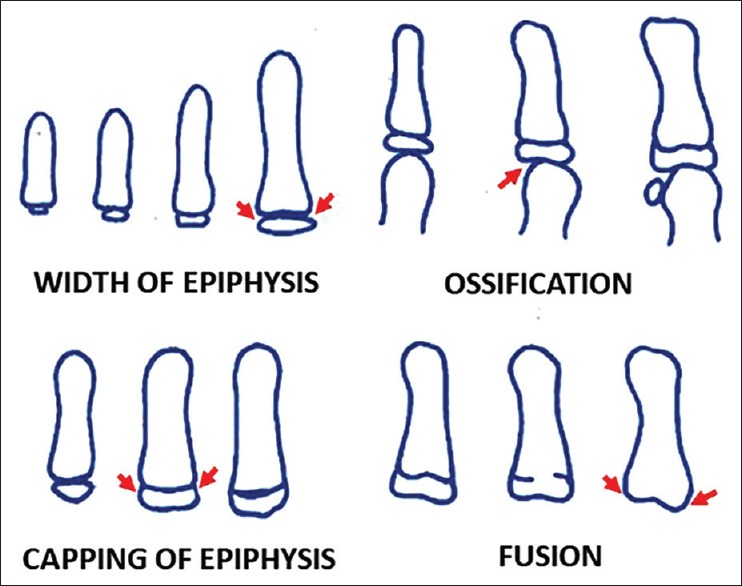
Radiographic identification of skeletal maturity indicators
In Bjork system, the developmental maturity indicators are in the following order [Figure 4]:
Figure 4.
Skeletal maturity indicators according to Bjork. (a) Epiphysis equal in width to diaphysis second finger (b) Epiphysis equal in width to diaphysis third finger (c) Appearance of adductor sesamoid of the thumb (d) Capping in the middle of third finger (e) Fusion of epiphysis and diaphysis in the distal of third finger (f) Fusion of epiphysis and diaphysis in the proximal of third finger (g) Fusion of epiphysis and diaphysis in the middle of third finger (h) Fusion of the radius
-
Width of epiphysis as wide as diaphysis located at:
Ossification of adductor sesamoid located at the thumb(S) [Figure 4c]
Capping of epiphysis located at a-, middle phalanx of the third finger (MP3 Cap) [Figure 4d]
-
Fusion of epiphysis and diaphysis located at
Following the diagram in Figure 5 and 6, the skeletal age can be determined. The following steps should be followed depending on the presence of the Sesamoid Bone (S) in the hand and wrist radiograph to determine the skeletal maturity stage in hand and wrist radiograph.
Figure 5.
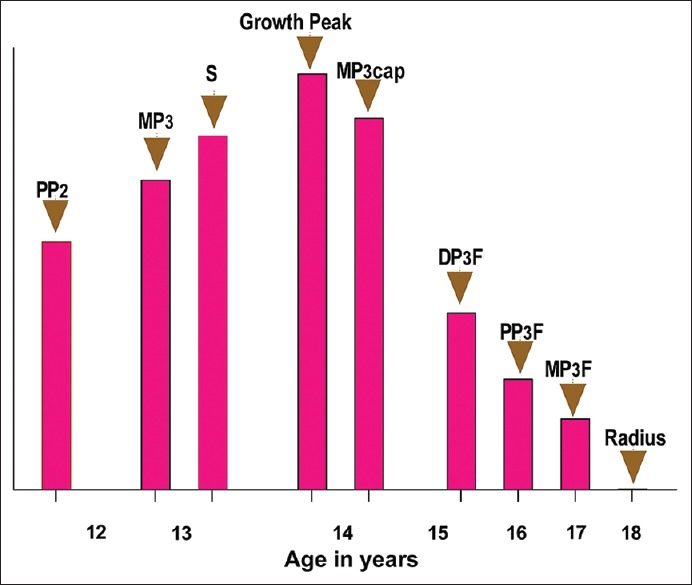
The growth curve
Figure 6.
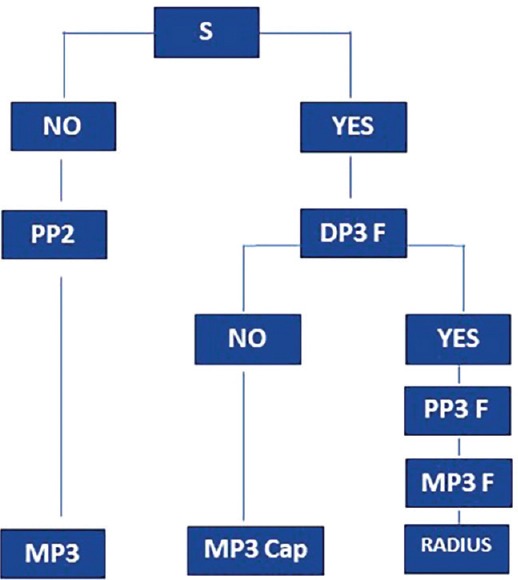
Determination of the skeletal maturity stage from hand and wrist radiograph
The first step is to look for both the Sesamoid bone (S) and fusion of the epiphysis and diaphysis of the third finger at the distal site (DP3F).
The second step: If the Sesamoid bone (S) is not present. Look for the width of the epiphysis and diaphysis of the proximal phalanx of the second finger (PP2). If they are equal, then look for the width of the epiphysis and diaphysis in the middle of the third finger (MP3). If they are not equal, then the patient is in (PP2) stage, but if they are equal, then the patient is in (MP3) stage.
The third step: If the Sesamoid bone (S) is present look at the third finger in the distal site, if there is fusion or not?
If there is no fusion between the epiphysis and diaphysis, then the patient in the capping stage (MP3Cap) stage
If there is fusion in the distal site and no fusion in the proximal and middle site of the third finger, then the patient is in (DP3F)
If there is fusion in the distal site, then look at the proximal site of the third finger and also at the middle site, if there is no fusion in the middle site, then the patient is in the (PP3F) stage
However if there is fusion in the distal and proximal and middle sites of the third finger but no fusion in the radius, then the patient is in the (MP3F) stage
If there is fusion in the radius bone, then the patient is in Radius stage (R) where most of the growth was utilized.
DISCUSSION
Understanding the growth of the oro-facial region is important when planning orthodontic treatment. Skeletal maturation is an integral part of individual patterns of growth and development. Variation in the maturation status is closely associated with deviation in the timing and magnitude of growth. Due to individual variation in timing, duration, and velocity of growth, skeletal age assessment is essential in formulating viable orthodontic treatment plans.[35] Clinical decisions regarding the use of extra-oral traction forces, functional appliances, extraction versus nonextraction treatment or orthognathic surgery are at least based on growth considerations.[36]
Every growing child matures differently and several methods were proposed as maturity indicators. Among these are the chronological age;[37] dental eruption; dental calcification stages;[38,39,40,41] Hand and wrist[2,42] as well as the height;[29] weight;[37] sexual maturation;[23] Frontal sinus;[19] and the Cervical vertebrae;[43] and recently biomarkers.[44] Bacettee et al.[45] and other researchers[46,47] introduced the cervical vertebral maturation method [CVM]). This method has gained popularity in recent years. The method is based on the morphological characteristics of the cervical vertebrae at different developmental stages. These stages are correlated with different growth rates in facial structures. Further, the CVM method cover the entire circumpubertal period for both genders by covering all significant phases in craniofacial growth during adolescence and young adulthood. It is important to identify the maximum growth spurt in growing child.
Hand and wrist radiographic examination can give accurate bone age (skeletal age) picture. The hand and wrist were used because it is easy to locate the different developmental stages and ossification centers which will give accurate skeletal age compared to chronological age as it is frequently accelerated or decelerated and it is technically simple to make radiograph.[48] Every method mentioned above has its own advantages, disadvantages, and limitation over the other methods. However, more research is needed to find the best method to assess the maturity of subjects seeking orthodontic treatment. This review presents details of the hand and wrist method introduced by Bjork which is simple and easy to use with minimal radiographs.
CONCLUSION
The knowledge of the growth and skeletal maturation stage of the orthodontics patients are of great value for selecting the efficient orthodontic therapy. However, different craniofacial structures of patient show variation in growth potential. The routine use of hand-wrist radiographs for growth prediction exposes the patient to additional radiation. Evaluation using lateral cephalographs has been recommended as alternative method. The pubertal growth spurt is a vital period in the orthodontic treatment and should be kept in mind when planning orthodontic treatment in growing children. One of the main objectives is to make use of growth in patients with skeletal discrepancy during adolescence. This will influence the selection of the appliances, the course of the treatment and the retention after the therapy.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Greulich WW, Pyle SI, Todd TW. Radiographic Atlas of Skeletal Development of the Hand and Wrist. Stanford: Stanford University Press; 1959. [Google Scholar]
- 2.Björk A, Helm S. Prediction of the age of maximum puberal growth in body height. Angle Orthod. 1967;37:134–43. doi: 10.1043/0003-3219(1967)037<0134:POTAOM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Rajagopal R, Kansal S. A comparison of modified MP3 stages and the cervical vertebrae as growth indicators. J Clin Orthod. 2002;36:398–406. [PubMed] [Google Scholar]
- 4.Boeyer ME, Sherwood RJ, Deroche CB, Duren DL. Early maturity as the new normal: A century-long study of bone age? Clin Orthop Relat Res. 2018 doi: 10.1097/CORR.0000000000000446. DOI: 10.1097/CORR.0000000000000446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macha M, Lamba B, Avula JS, Muthineni S, Margana PG, Chitoori P, et al. Estimation of correlation between chronological age, skeletal age and dental age in children – A cross-sectional study. J Clin Diagn Res. 2017;11:ZC01–4. doi: 10.7860/JCDR/2017/25175.10537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baccetti T, Franchi L, De Toffol L, Ghiozzi B, Cozza P. The diagnostic performance of chronologic age in the assessment of skeletal maturity. Prog Orthod. 2006;7:176–88. [PubMed] [Google Scholar]
- 7.Mincer HH, Harris EF, Berryman HE. The A.B.F.O. Study of third molar development and its use as an estimator of chronological age. J Forensic Sci. 1993;38:379–90. [PubMed] [Google Scholar]
- 8.Olze A, Taniguchi M, Schmeling A, Zhu BL, Yamada Y, Maeda H, et al. Studies on the chronology of third molar mineralization in a Japanese population. Leg Med (Tokyo) 2004;6:73–9. doi: 10.1016/j.legalmed.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Maber M, Liversidge HM, Hector MP. Accuracy of age estimation of radiographic methods using developing teeth. Forensic Sci Int. 2006;159(Suppl 1):S68–73. doi: 10.1016/j.forsciint.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 10.Bala M, Pathak A, Jain RL. Assessment of skeletal age using MP3 and hand-wrist radiographs and its correlation with dental and chronological ages in children. J Indian Soc Pedod Prev Dent. 2010;28:95–9. doi: 10.4103/0970-4388.66746. [DOI] [PubMed] [Google Scholar]
- 11.De Sanctis V, Di Maio S, Soliman AT, Raiola G, Elalaily R, Millimaggi G, et al. Hand X-ray in pediatric endocrinology: Skeletal age assessment and beyond. Indian J Endocrinol Metab. 2014;18:S63–71. doi: 10.4103/2230-8210.145076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crowder C, Austin D. Age ranges of epiphyseal fusion in the distal tibia and fibula of contemporary males and females. J Forensic Sci. 2005;50:1001–7. [PubMed] [Google Scholar]
- 13.Mohammed RB, Reddy MA, Jain M, Singh JR, Sanghvi P, Thetay AA. Digital radiographic evaluation of hand-wrist bone maturation and prediction of age in South Indian adolescents. Hand (N Y) 2014;9:375–83. doi: 10.1007/s11552-013-9598-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chapman SM. Ossification of the adductor sesamoid and the adolescent growth spurt. Angle Orthod. 1972;42:236–44. doi: 10.1043/0003-3219(1972)042<0236:OOTASA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Grave KC, Brown T. Skeletal ossification and the adolescent growth spurt. Am J Orthod. 1976;69:611–9. doi: 10.1016/0002-9416(76)90143-3. [DOI] [PubMed] [Google Scholar]
- 16.Houston WJ, Miller JC, Tanner JM. Prediction of the timing of the adolescent growth spurt from ossification events in hand-wrist films. Br J Orthod. 1979;6:145–52. doi: 10.1179/bjo.6.3.145. [DOI] [PubMed] [Google Scholar]
- 17.Flores-Mir C, Burgess CA, Champney M, Jensen RJ, Pitcher MR, Major PW, et al. Correlation of skeletal maturation stages determined by cervical vertebrae and hand-wrist evaluations. Angle Orthod. 2006;76:1–5. doi: 10.1043/0003-3219(2006)076[0001:COSMSD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]
- 19.Ruf S, Pancherz H. Development of the frontal sinus in relation to somatic and skeletal maturity. A cephalometric roentgenographic study at puberty. Eur J Orthod. 1996;18:491–7. doi: 10.1093/ejo/18.5.491. [DOI] [PubMed] [Google Scholar]
- 20.Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented method based on hand-wrist films. Angle Orthod. 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Koshy S, Tandon S. Dental age assessment: The applicability of Demirjian's method in South Indian children. Forensic Sci Int. 1998;94:73–85. doi: 10.1016/s0379-0738(98)00034-6. [DOI] [PubMed] [Google Scholar]
- 22.Jiménez-Castellanos J, Carmona A, Catalina-Herrera CJ, Viñuales M. Skeletal maturation of wrist and hand ossification centers in normal Spanish boys and girls: A study using the Greulich-Pyle method. Acta Anat (Basel) 1996;155:206–11. doi: 10.1159/000147806. [DOI] [PubMed] [Google Scholar]
- 23.Hägg U, Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982;82:299–309. doi: 10.1016/0002-9416(82)90464-x. [DOI] [PubMed] [Google Scholar]
- 24.Flores-Mir C, Nebbe B, Major PW. Use of skeletal maturation based on hand-wrist radiographic analysis as a predictor of facial growth: A systematic review. Angle Orthod. 2004;74:118–24. doi: 10.1043/0003-3219(2004)074<0118:UOSMBO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Bakerly SD, Saleh F. Correlation of adductor metacarpophalangeal sesamoid ossification stages with dentofacial profile changes. Eur Sci J. 2013;9:450–69. [Google Scholar]
- 26.Grave KC. Timing of facial growth: A study of relations with stature and ossification in the hand around puberty. Aust Orthod J. 1973;3:117–22. [PubMed] [Google Scholar]
- 27.Fishman LS. Maturational patterns and prediction during adolescence. Angle Orthod. 1987;57:178–93. doi: 10.1043/0003-3219(1987)057<0178:MPAPDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Ghai O, Paul V, Bagga A. Essential pediatrics. 9th Edition. New Delhi India: CBS Publisher and distributors; 2018. p. 11. [Google Scholar]
- 29.Hunter CJ. The correlation of facial growth with body height and skeletal maturation at adolescence. Angle Orthod. 1966;36:44–54. doi: 10.1043/0003-3219(1966)036<0044:TCOFGW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Bowden BD. Epiphysial changes in the hand/wrist area as indicators of adolescent stage. Aust Orthod J. 1976;4:87–104. [PubMed] [Google Scholar]
- 31.Moorrees CF, Fanning EA, Hunt EE., Jr Age variation of formation stages for ten permanent teeth. J Dent Res. 1963;42:1490–502. doi: 10.1177/00220345630420062701. [DOI] [PubMed] [Google Scholar]
- 32.Singer J. Physiologic timing of orthodontic treatment. Angle Orthod. 1980;50:322–33. doi: 10.1043/0003-3219(1980)050<0322:PTOOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 33.Demirjian A, Buschang PH, Tanguay R, Patterson DK. Interrelationships among measures of somatic, skeletal, dental, and sexual maturity. Am J Orthod. 1985;88:433–8. doi: 10.1016/0002-9416(85)90070-3. [DOI] [PubMed] [Google Scholar]
- 34.Kucukkeles N, Acar A, Biren S, Arun T. Comparisons between cervical vertebrae and hand-wrist maturation for the assessment of skeletal maturity. J Clin Pediatr Dent. 1999;24:47–52. [PubMed] [Google Scholar]
- 35.Flieger R, Matys J, Dominiak M. The best time for orthodontic treatment for Polish children based on skeletal age analysis in accordance to refund policy of the Polish National Health Fund (NFZ) Adv Clin Exp Med. 2018;27:1–6. doi: 10.17219/acem/69976. [DOI] [PubMed] [Google Scholar]
- 36.De Stefani A, Bruno G, Siviero L, Crivellin G, Mazzoleni S, Gracco A. Middle phalanx maturation of the third finger (MPM) method in the evaluation of skeletal age in a growing orthodontic patient. Int Orthod. 2018;16:499–513. doi: 10.1016/j.ortho.2018.06.025. [DOI] [PubMed] [Google Scholar]
- 37.Green LJ. The interrelationships among height, weight and chronological, dental and skeletal ages. Angle Orthod. 1961;31:189–93. [Google Scholar]
- 38.Nolla CM. The Development of Permanent Teeth. University of Michigan; 1952. [Google Scholar]
- 39.Demisch A, Wartmann P. Calcification of the mandibular third molar and its relation to skeletal and chronological age in children. Child Dev. 1956;27:459–73. doi: 10.1111/j.1467-8624.1956.tb04824.x. [DOI] [PubMed] [Google Scholar]
- 40.Demirjian A, Goldstein H, Tanner JM. A new system of dental age assessment. Hum Biol. 1973;45:211–27. [PubMed] [Google Scholar]
- 41.Demirjian A, Goldstein H. New systems for dental maturity based on seven and four teeth. Ann Hum Biol. 1976;3:411–21. doi: 10.1080/03014467600001671. [DOI] [PubMed] [Google Scholar]
- 42.Hägg U, Taranger J. Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt. Acta Odontol Scand. 1980;38:187–200. doi: 10.3109/00016358009004719. [DOI] [PubMed] [Google Scholar]
- 43.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–29. [Google Scholar]
- 44.Perinetti G, Baccetti T, Di Leonardo B, Di Lenarda R, Contardo L. Dentition phase and chronological age in relation to gingival crevicular fluid alkaline phosphatase activity in growing subjects. Prog Orthod. 2011;12:100–6. doi: 10.1016/j.pio.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 45.Baccetti T, Franchi L, McNamara JA., Jr An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72:316–23. doi: 10.1043/0003-3219(2002)072<0316:AIVOTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 46.Soegiharto BM, Moles DR, Cunningham SJ. Discriminatory ability of the skeletal maturation index and the cervical vertebrae maturation index in detecting peak pubertal growth in indonesian and white subjects with receiver operating characteristics analysis. Am J Orthod Dentofacial Orthop. 2008;134:227–37. doi: 10.1016/j.ajodo.2006.09.062. [DOI] [PubMed] [Google Scholar]
- 47.Caldas Mde P, Ambrosano GM, Haiter Neto F. Computer-assisted analysis of cervical vertebral bone age using cephalometric radiographs in Brazilian subjects. Braz Oral Res. 2010;24:120–6. doi: 10.1590/s1806-83242010000100020. [DOI] [PubMed] [Google Scholar]
- 48.Szemraj A, Wojtaszek-Słomińska A, Racka-Pilszak B. Is the cervical vertebral maturation (CVM) method effective enough to replace the hand-wrist maturation (HWM) method in determining skeletal maturation? – A systematic review. Eur J Radiol. 2018;102:125–8. doi: 10.1016/j.ejrad.2018.03.012. [DOI] [PubMed] [Google Scholar]