Abstract
Aims and Objectives:
The aims of this study were to determine oral health-related quality of life (OHRQoL) among elderly people aged 65 and above years from Hafar Al-Batin area, Saudi Arabia, by utilizing Arabic version of Geriatric Oral Health Assessment Index (GOHAI-Ar).
Materials and Methods:
This was a cross-sectional study undertaken from October 2017 to December 2017. A convenience sampling methodology was employed to select the elderly patients aged ≥65 years attending dental clinics of primary health-care centers in five different regions of the Hafar Al-Batin, Saudi Arabia. OHRQoL of the participants was measured using the Saudi Arabian version of GOHAI-Ar. The oral examinations performed to record a total number of remaining natural teeth, complete and removable partial dentures, and fixed partial dentures. Descriptive and inferential statistics were performed.
Results:
A total of 200 elderly participants (M = 157 and F = 43) having mean age (± standard error [SE]) was 69.26 (±0.34) years, participated in the study. Mean ± SE of GOHAI-Ar was 27.68 ± 0.54, physical function 9.12 ± 0.26, pain and discomfort (6.87 ± 0.18), and psychological discomfort (11.69 ± 0.25). Remaining natural teeth and prosthodontic status significantly correlated with pain and discomfort. The presence of prosthesis was found to influence the psychological function. Gender and prosthodontic statuses were found to have significant correlation with OHRQoL.
Conclusion:
Poor OHRQoL among elderly from Hafar Al-Batin city was found, and presence dental prosthesis showed a positive impact on OHRQoL.
KEYWORDS: Arabic version of geriatric oral health assessment index, elderly, impact, oral health-related quality of life, pain and discomfort, physical function, psychological discomfort
INTRODUCTION
Recently, FDI World dental federation defined oral health as a multifaceted and includes the ability to speak, smile, smell, taste, touch, chew, and swallow, and conveys a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex. It reflects the physiological, social, and psychological attributes that are essential to the quality of life. This new definition encompasses the multifaceted nature and attributes of oral health.[1]
Complete or partial loss dentition has unpleasant consequences on usual functions such as speech, chewing ability, and appearance.[2] In addition, edentulous state can affect psychologically and is closely associated with physical and mental well-being.[3] There are a large number of edentulous patients in all communities, and the trend suggests that the number in this group will continue to increase in the future. This can be demonstrated by the improvement in life expectancy rate due to the improved health care.[4]
The proportion of people in Saudi Arabia aged 60 or more is predicted to be 25% of the whole population of 40 million by the period of 2050. Furthermore, the number of people aged 80 or more is expectant to reach 1.6 million or 4% of the total population in the same period. The population in the age group (60 years and over) was 4.4% (1.1 million) in 2010 and 6.9% (2.1 million) in 2020.[5]
Poor oral health, including edentulism, affects the quality of life in the elderly in a substantial manner.[6] Given the momentum and extent of this growth, care for the elderly is essential to influence the quality of life. It has been agreed that oral health is an important and integral part of systemic health and can influence systemic conditions.[7]
Several socio-dental indicators used to assess the impact of the oral disorder on the quality of patient's life.[8] The oral health-related quality of life measures the degree to which oral health interrupts the normal life and social functioning of an individual.[9] It has been reported that high frequency of fruit and vegetable intake has a strong positive association with the oral health-related quality of life (OHRQoL) in either gender.[10]
High prevalence of oral diseases in older population and absence of valid and reliable instruments to assess the impact of oral diseases among older populations was the precursor for the development of the Geriatric Oral Health Assessment Index (GOHAI). This is a self-reported measure developed to evaluate the oral health problems among older populations.[11]
The original GOHAI consisted of 12 negatively and positively worded items assessing three domains of OHRQoL. It included physical function (PF), pain and discomfort, and psychosocial function.[12] It has been translated in different languages such as French,[13] Arabic,[12] German,[14] Persian,[15] and Hindi[16] and found to have adequate validity and reliability.
Oral health-care inequalities do exist between urban and rural areas. These inequalities were obvious in distribution of health services, access, and utilization of dental care, treatment outcomes, OHRQoL, and the prevalence of oral diseases.[17] The prevalence of poor oral health-related quality life was significantly higher in rural areas than in urban zones. Moreover, rural residents reported a significantly higher prevalence of negative daily-life impacts in pain, psychological discomfort, and social disability.[18]
Most of the previous studies in Saudi Arabia that utilized GOHAI were focused on elderly population from capital/or larger cities with little attention on the OHRQoL of elderly living in smaller cities of Saudi Arabia. Therefore, the purpose of this study was to determine OHRQoL among elderly people aged 65 years and above from Hafar Al-Batin area, Saudi Arabia, by utilizing Arabic version of GOHAI (GOHAI-Ar).
MATERIALS AND METHODS
ETHICAL APPROVAL
The study proposal submitted to the research center of Riyadh Elm University and ethical approval was obtained. Concerned primary health center authorities in Hafar Al-Batin area were informed about the research. Elderly patients were invited to participate in the after obtaining informed consent. The study was registered with number (FPGRP/43638003/128).
STUDY PARTICIPANTS
This was a cross-sectional study undertaken from October to December 2017. The elderly patients aged 65 years and above attending dental clinics in primary health-care centers in five different regions of the Hafar Al-Batin, Saudi Arabia, were considered in the study.
The sample size calculation was based on correlation (r) test. Sample size of 200 was decided based on correlation (r) test by assuming H0: P0 = 0.584 and H1: P1 = 0.700 with β = 0.2 (80% power) and α = 0.05 for two-sided test. A G* Power software version 3.1.9.2 for Windows (Faul F et al, 2007 Department of Psychology, Germany) was utilized for the calculation of sample size.
Inclusion criteria
Saudi nationals, ambulatory patients, aged 65 years or more, and able to read and understand Arabic language. Exclusion criteria consisted of uncooperative patients, expatriates, and not willing to participate in the study. Incomplete questionnaires were also excluded from the study.
QUESTIONNAIRE CONTENT
OHRQoL was measured using the Arabic version of GOHAI-Ar. It was translated and validated from original English version into Arabic by Atieh.[12] for the use among elderly in Saudi Arabia. The GOHAI-Ar gave a composite score based on the answers to 12 questions related the following three domains of OHRQoL: PF including eating, speech, and swallowing; psychosocial function that includes worry or concern about oral health, dissatisfaction with appearance, self-consciousness about oral health, and avoidance of social contact because of oral problems; pain or discomfort (PD) including the use of medication to relieve PD in the mouth. All the questionnaire items were scored on 6-point Likert scale (0 = never, 1 = seldom, 2 = sometimes, 3 = often, 4 = very often, and 5 = always). The overall GOHAI-Ar was calculated by adding the score of 12 questions, and it ranged from 0 to 60. The scores were kept similar for three items “able to swallow comfortably,” “able to eat without discomfort,” “pleased with look of teeth,” and reversed for all other nine items to indicate that higher score is associated with more positive oral health. A total of 200 questionnaires were distributed to the patients, and all of them responded to the questions. Each patient took <5 min to complete the questionnaire. For all these patients, oral examination was performed.
Questionnaire consisted of four parts: first part included sociodemographic variables (age, gender, education, occupation, and living status), second part: self-perceived oral health and dental care (self-perception of oral health, self-perception of dental care needs, visit to dentist, payment for dental care, and preferred dental clinics), third part: prosthodontic and dentition status (absence of dental prosthesis, full-mouth complete denture, single complete denture only, single partial denture, full-mouth partial denture, and fixed partial denture), and fourth part measured OHRQoL using GOHAI-Ar.
ORAL EXAMINATION
Oral examinations were performed by single examiner (author), advanced general dentistry specialist having several years of experience. All the oral examinations performed in dental chair while participant is sitting in upright position under chair light using mouth mirror and WHO probe. Intraexaminer reliability was calculated and found to be satisfactory. A total number of remaining natural teeth, complete and removable partial dentures, and fixed partial dentures were recorded.
STATISTICAL ANALYSIS
All the data were entered into the statistical analysis software SPSS version 21.0 (Armonk, NY: IBM Corp., USA) by considering the significance level of 5%. The categorical variables were calculated in terms of number and percentages and continuous variables were expressed as mean ± standard error (SE). A total GOHAI-Ar and individual domain scores were compared between sociodemographic factors, self-perceived oral health and dental care, prosthodontic, and dentition status. An independent t-test and analysis of variance tests were applied to evaluate the distribution of GOHAI-Ar scores in relation to categorical variables. Pearson's test was also used to assess the correlation between the variables.
RESULTS
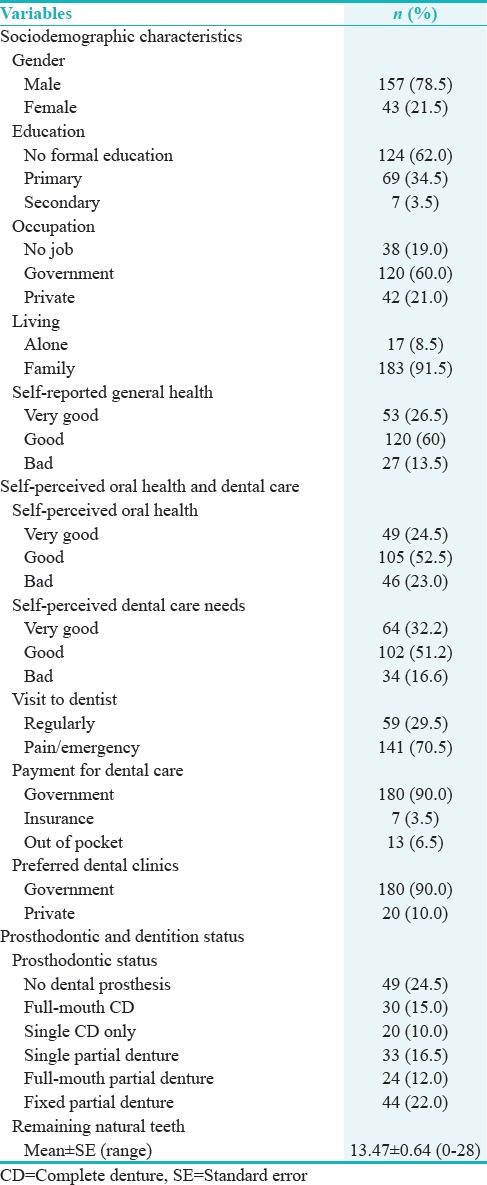
Characteristics of the study participants are displayed in Table 1. Data were collected from the 200 elderly participants in whom more than three-fourth participants were male 157 (78.5%) mean age (±SE) was 69.26 (±0.34) years, most of them 124 (62%) had no formal education and worked in 120 (60%) government sector. Majority of the 183 (91.5%) elderly stayed with their families. Self-reported health status suggested that most (51.2%) of the elderly had good general health.
Table 1.
Characteristics of the participants
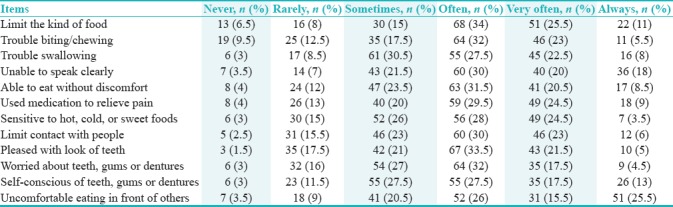
Majority of the elderly study participants often faced with many problems due to conditions of their mouth and teeth such as limited the kinds of food 68 (34%), trouble in biting/chewing 64 (32%), sometimes trouble in swallowing 61 (30.5%), unable to speak clearly 60 (30%), able to eat without discomfort 63 (31.5%), used medication to relieve pain 59 (29.5%), sensitive to hot, cold, or sweet foods 56 (28%), limit contact with people 60 (30%), pleased with look of teeth 67 (33.5%), worried about teeth, gums, or dentures 64 (32%), self-conscious of teeth, gums, or dentures 55 (27.5%), and uncomfortable eating in front of others 52 (26%), as shown in Table 2.
Table 2.
Distribution of responses to Arabic version of Geriatric Oral Health Assessment Index items
OHRQoL as measured by GOHAI-Ar and its different domains are presented in Figure 1. Mean ± SE, scores for PF (9.12 ± 0.26), pain and discomfort (6.87 ± 0.18), psychological function (11.69 ± 0.25), and overall GOHAI-Ar (27.68 ± 0.54) were observed.
Figure 1.
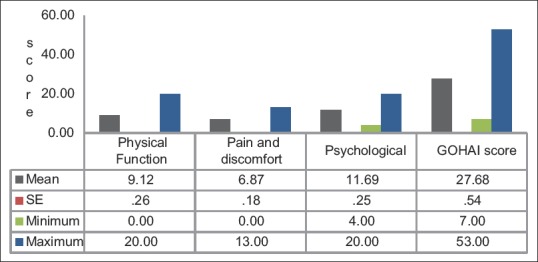
Oral health-related quality of life
Elderly patients complained of bad breath (36%), wide teeth (36%), dryness of mouth (28.50%), pain (28%), and ulcer (25.50%) associated with wearing of prosthetic teeth as shown in Figure 2.
Figure 2.
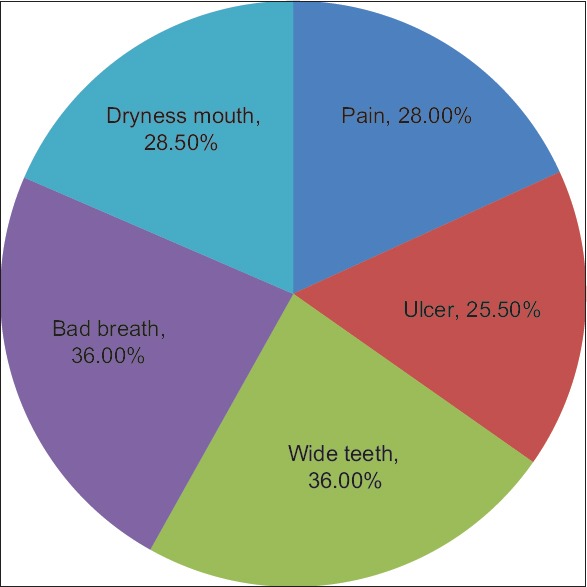
Factors associated with wearing denture
Mean scores of PF, pain and discomfort, psychological function, and overall GOHAI-Ar for various characteristics of the elderly patients are displayed in Table 3. As the age of the elderly participants increased, mean score of PF, pain and discomfort, psychological function, and mean GOHAI-Ar scores increased. However, elderly aged ≥75 years (10.45 ± 0.85) showed significantly higher mean PF score compared to the elderly aged 65–69 years (8.64 ± 0.28) (P = 0.042). Similarly, mean GOHAI-Ar score was also significantly higher among elder aged ≥75 years (30.65 ± 1.71) compared to the elderly 65–69 years (26.67 ± 0.59), (P = 0.035). On the contrary, mean scores of PF, pain and discomfort, psychological function, and GOHAI-Ar varied among different groups of education, occupation, and payment for dental care without any statistical significance (P > 0.05).
Table 3.
Comparison of mean scores of Arabic version of Geriatric Oral Health Assessment Index among different groups by Analysis of Variance
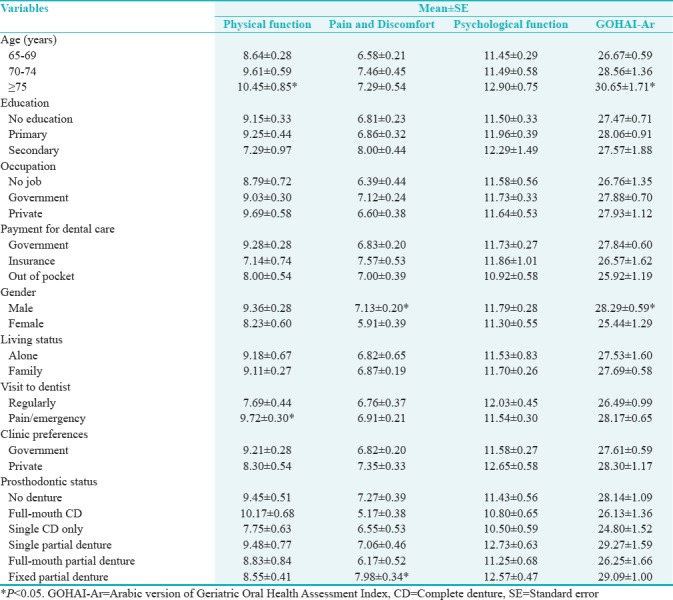
Similarly, males showed significantly higher mean scores of pain and discomfort (7.13 ± 0.20) and overall GOHAI-Ar scores (28.29 ± 0.59) compared to the females (5.91 ± 0.39) and (25.44 ± 1.29) (P < 0.05). Elderly visiting dentist during pain/emergency showed significantly higher mean PF scores (9.72 ± 0.30) compared to those who visited the dentist regularly (7.69 ± 0.44), (P < 0.05). However, elderly clinic preference did not show any significant difference in PF, pain and discomfort, psychological function, and overall GOHAI-Ar scores. Prosthodontic status indicated that elderly having full-mouth complete denture (10.17 ± 9.45) showed significantly higher mean pain and discomfort score compared to the no denture (9.45 ± 0.51) and fixed partial denture (8.55 ± 0.41) group (P < 0.05), as shown in Table 3.
A significant difference in mean scores of PF, pain and discomfort, psychological function, and overall GOHAI-Ar was observed among elderly participants having problems with artificial teeth as shown in Table 4.
Table 4.
Effects of artificial teeth and oral health-related quality of life among elderly
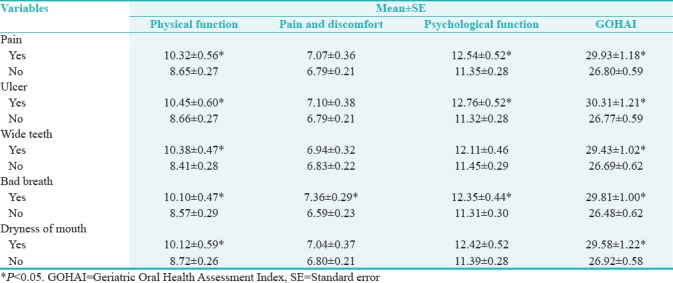
Presence of prosthesis was found to influence the psychological function. Gender and prosthodontic statuses were found to have significant correlation with OHRQoL. Significant negative correlations were observed between the artificial teeth that caused pain (r = −0.216, P = 0.008), ulcer (r = −0.227, P = 0.005), bad breath (r = −0.258, P = 0.001), and OHRQoL as shown in Table 5.
Table 5.
Pearson's correlation test between variables
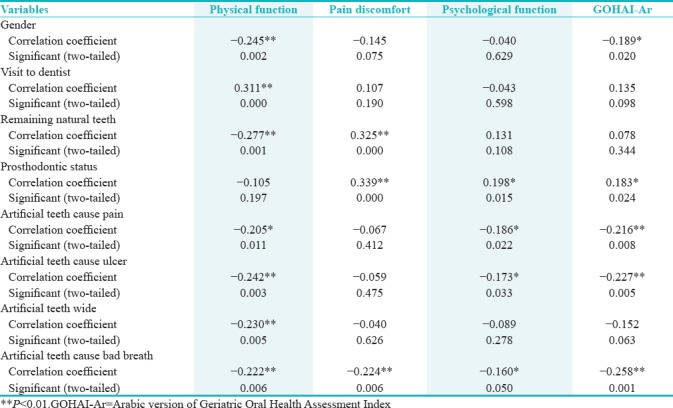
PF was found to be significantly negatively correlated with gender (−0.245, P = 0.002) and remaining teeth (r = 0.277, P = 0.001) and positively correlated with the visit to dentist (r = 0.311, P = 0.000). Pain and discomfort was significantly positively correlated with remaining natural teeth (r = 0.325, P = 0.000) and prosthodontic status (r = 0.339, P = 0.000). Similarly, psychological function shown to be significantly positively correlated with prosthodontic status (r = 0.198, P = 0.015). GOHAI-Ar showed significantly positive correlation with prosthodontic status (r = 0.183, P = 0.024) and negative correlation with gender (r = −0.189, P = 0.020).
DISCUSSION
To improve the oral health of the elderly people through organized efforts of the health-care system, it is utmost important to understand the factors that influence OHRQoL of elderly. Elderly can face several barriers for accessing the care, especially smaller cities with the limited resources and inadequate facilities. Hence, the present study highlighted the factors that affect the OHRQoL among elderly from Hafral Al-Batin region, Saudi Arabia.
Results of the study revealed that an overall (mean ± SE) GOHAI-Ar score was (27.68 ± 0.54) on a scale of (0–60). This result is nearly similar to that of reported among hospitalized (28.95±) and nonhospitalized 28.44 ± 4.4 elderly participants from Riyadh region, Saudi Arabia.[19] On the contrary, Rekhi et al. reported higher a mean GOHAI score of the 41.57 ± 6.07 among the institutionalized elderly in India. Similarly, Yen et al. reported a mean GOHAI score of 47.8 ± 0.5 among elderly Taiwanese patients wearing removable dentures.[20]
This lower GOHAI-Ar score of (27.68 ± 0.54) is suggestive of poor OHRQoL among elderly from Hafar Al-Batin region. This could be directly related to their underlying malnutrition,[21] diabetes,[22] and any other medical condition that has direct influence on the OHRQoL. Moreover, clear socioeconomic inequality in oral health among elderly can be considered as one of the contributing factors for poor OHRQoL among elderly.[23] When compared to the other published literature on OHRQoL among the elderly, we found lower GOHAI-Ar values in the present study. One possible explanation is that the three-fourth of the participants in this study were elderly individuals wearing artificial teeth of some kind. Previous studies indicated that compared to people with natural teeth, those who wear removable dentures experience more significant negative impacts on social and emotional aspects of life.[24] Another possible explanation may be that the participants in this study were patients attending the primary health-care centers around the Hafar Al-Batin region. In addition, 34 (16.6%) of the elderly in this study perceived bad dental care needs.
In the present study, as the mean age increased mean GOHAI-Ar score also increased suggesting less impact and more positive OHRQoL. This finding could be explained on the basis that more than three-fourth of the study participants were wearing artificial teeth and presence of artificial teeth have shown improved OHRQoL among elderly.[25,26,27,28,29]
Fairly strong evidence was found that tooth loss is associated with impairment of OHRQoL and location and distribution of tooth loss affect the severity of the impairment.[28] In addition, reports have also shown correlation between the reductions in number of remaining natural teeth and poor OHRQoL.[29] In our study, male participants had more number of remaining natural than females suggesting more positive OHRQoL among males than females.
Single complete denture wearers and complete denture wearers showed lower GOHAI-Ar score. On the contrary, fixed partial denture wearers and single partial denture wearers showed higher GOHAI-Ar scores. This finding is suggestive of differences in OHRQoL among participants wearing different types of prosthesis.
In our study, GOHAI-Ar score was found to be significantly affected by prosthesis-related factors such as pain, ulcer, wide tooth, bad breath, and dryness mouth. This finding is similar to that of reported study by Yen et al., in which denture satisfaction was found to be the strongest predictor of OHRQoL among elderly.
Among all the factors considered in the study prosthodontic status was found to have significant positive correlation with OHRQoL. This result is consistent with reported study in which dental rehabilitation of geriatric patients resulted in increase in the GOHAI score suggesting improved OHRQoL.[30]
Unlike other studies, our study also had several limitations that need to be taken cautiously during the interpretation of the findings. First, it was not a population-based sample instead of study participants were recruited from the primary health-care centers of Hafar Al-batin region, representing only small group of the whole population. Hence, generalizability of the study results is limited. Future research should take into consideration about the generalizability of the findings among elderly population. Second, the current study is categorized under a cross-sectional design, and therefore, we cannot make interpretations with respect to the observed association.
CONCLUSION
Within the limitations of the study, it can be concluded that the elderly patients attending primary health-care centers in Hafar Al-Batin region showed poor OHRQoL as measured by GOHAI-Saudi Arabian version. Moreover, the study revealed that the presence of dental prosthesis can have a positive impact on OHRQoL among elderly.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI world dental federation opens the door to a universal definition of oral health. Int Dent J. 2016;66:322–4. doi: 10.1111/idj.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jonkman RE, van Waas MA, van’t Hof MA, Kalk W. An analysis of satisfaction with complete immediate (over) dentures. J Dent. 1997;25:107–11. doi: 10.1016/s0300-5712(96)00012-7. [DOI] [PubMed] [Google Scholar]
- 3.Chen YF, Yang YH, Chen YH, Lee HE, Lin YC, Ebinger J, et al. The impact of complete dentures on the oral health-related quality of life among the elderly. J Dent Sci. 2012;7:289–95. [Google Scholar]
- 4.Assunção WG, Barão VA, Delben JA, Gomes EA, Tabata LF. A comparison of patient satisfaction between treatment with conventional complete dentures and overdentures in the elderly: A literature review. Gerodontology. 2010;27:154–62. doi: 10.1111/j.1741-2358.2009.00299.x. [DOI] [PubMed] [Google Scholar]
- 5.Abusaaq HI. Population Aging in Saudi Arabia: SAMA Working Paper. 2015 [Google Scholar]
- 6.Rodrigues SM, Oliveira AC, Vargas AM, Moreira AN, E Ferreira EF. Implications of edentulism on quality of life among elderly. Int J Environ Res Public Health. 2012;9:100–9. doi: 10.3390/ijerph9010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petersen PE, Kandelman D, Arpin S, Ogawa H. Global oral health of older people – Call for public health action. Community Dent Health. 2010;27:257–67. [PubMed] [Google Scholar]
- 8.Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446–50. [PubMed] [Google Scholar]
- 9.Mesas AE, de Andrade SM, Cabrera MA. Factors associated with negative self-perception of oral health among elderly people in a Brazilian community. Gerodontology. 2008;25:49–56. doi: 10.1111/j.1741-2358.2007.00196.x. [DOI] [PubMed] [Google Scholar]
- 10.Nanri H, Yamada Y, Itoi A, Yamagata E, Watanabe Y, Yoshida T, et al. Frequency of fruit and vegetable consumption and the oral health-related quality of life among Japanese elderly: A cross-sectional study from the Kyoto-Kameoka study. Nutrients. 2017;9 doi: 10.3390/nu9121362. pii: E1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. J Dent Educ. 1990;54:680–7. [PubMed] [Google Scholar]
- 12.Atieh MA. Arabic version of the geriatric oral health assessment index. Gerodontology. 2008;25:34–41. doi: 10.1111/j.1741-2358.2007.00195.x. [DOI] [PubMed] [Google Scholar]
- 13.Tubert-Jeannin S, Riordan PJ, Morel-Papernot A, Porcheray S, Saby-Collet S. Validation of an oral health quality of life index (GOHAI) in France. Community Dent Oral Epidemiol. 2003;31:275–84. doi: 10.1034/j.1600-0528.2003.t01-1-00006.x. [DOI] [PubMed] [Google Scholar]
- 14.Hassel AJ, Rolko C, Koke U, Leisen J, Rammelsberg P. A German version of the GOHAI. Community Dent Oral Epidemiol. 2008;36:34–42. doi: 10.1111/j.1600-0528.2007.00351.x. [DOI] [PubMed] [Google Scholar]
- 15.Rezaei M, Rashedi V, Khedmati Morasae E. A Persian version of geriatric oral health assessment index. Gerodontology. 2016;33:335–41. doi: 10.1111/ger.12161. [DOI] [PubMed] [Google Scholar]
- 16.Mathur VP, Jain V, Pillai RS, Kalra S. Translation and validation of Hindi version of geriatric oral health assessment index. Gerodontology. 2016;33:89–96. doi: 10.1111/ger.12099. [DOI] [PubMed] [Google Scholar]
- 17.Ogunbodede EO, Kida IA, Madjapa HS, Amedari M, Ehizele A, Mutave R, et al. Oral health inequalities between rural and urban populations of the African and middle east region. Adv Dent Res. 2015;27:18–25. doi: 10.1177/0022034515575538. [DOI] [PubMed] [Google Scholar]
- 18.Gaber A, Galarneau C, Feine JS, Emami E. Rural-urban disparity in oral health-related quality of life. Community Dent Oral Epidemiol. 2018;46:132–42. doi: 10.1111/cdoe.12344. [DOI] [PubMed] [Google Scholar]
- 19.AlBaker AM, AlBaqami FF, AlHarbi TM, AlAmri MD, Baskaradoss JK. Oral health status and oral health-related quality of life among hospitalized and nonhospitalized geriatric patients. J Contemp Dent Pract. 2017;18:228–34. [PubMed] [Google Scholar]
- 20.Yen YY, Lee HE, Wu YM, Lan SJ, Wang WC, Du JK, et al. Impact of removable dentures on oral health-related quality of life among elderly adults in Taiwan. BMC Oral Health. 2015;15:1. doi: 10.1186/1472-6831-15-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu LL, Cheung KY, Lam PY, Gao XL. Oral health indicators for risk of malnutrition in elders. J Nutr Health Aging. 2018;22:254–61. doi: 10.1007/s12603-017-0887-2. [DOI] [PubMed] [Google Scholar]
- 22.Azogui-Lévy S, Dray-Spira R, Attal S, Hartemann A, Anagnostou F, Azerad J. Factors associated with oral health-related quality of life in patients with diabetes. Aust Dent J. 2018;63:163–9. doi: 10.1111/adj.12577. [DOI] [PubMed] [Google Scholar]
- 23.El Osta N, El Osta L, Khabbaz LR, Saad R, Abi-Ghosn C, Hennequin M, et al. Social inequalities in oral health in a group of older people in a Middle Eastern country: A cross-sectional survey? Aging Clin Exp Res. 2018 doi: 10.1007/s40520-018-0927-8. doi: 10.1007/s40520-018-0927-8. [DOI] [PubMed] [Google Scholar]
- 24.Hogenius S, Berggren U, Blomberg S, Jemt T, Ohman SC. Demographical, odontological, and psychological variables in individuals referred for osseointegrated dental implants. Community Dent Oral Epidemiol. 1992;20:224–8. doi: 10.1111/j.1600-0528.1992.tb01721.x. [DOI] [PubMed] [Google Scholar]
- 25.Tôrres AC, Maciel AQ, de Farias DB, de Medeiros AK, Vieira FP, Carreiro AD, et al. Technical quality of complete dentures: Influence on masticatory efficiency and quality of life? J Prosthodont. 2017 doi: 10.1111/jopr.12703. doi: 10.1111/jopr.12703. [DOI] [PubMed] [Google Scholar]
- 26.Policastro VB, Paleari AG, Leite AR, Mendoza-Marin DO, Cassiano AF, Shaddox LM, et al. A randomized clinical trial of oral health-related quality of life, peri-implant and kinesiograph parameters in wearers of one-or two-implant mandibular overdentures? J Prosthodont. 2018 doi: 10.1111/jopr.12796. doi: 10.1111/jopr.12796. [DOI] [PubMed] [Google Scholar]
- 27.Wahbi RH, Elamin EI. Impact of removable partial denture on quality-of-life of Sudanese adults in Khartoum state. J Contemp Dent Pract. 2018;19:102–8. doi: 10.5005/jp-journals-10024-2220. [DOI] [PubMed] [Google Scholar]
- 28.Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126. doi: 10.1186/1477-7525-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jain M, Kaira LS, Sikka G, Singh S, Gupta A, Sharma R, et al. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two state samples of Gujarat and Rajasthan. J Dent (Tehran) 2012;9:135–44. [PMC free article] [PubMed] [Google Scholar]
- 30.İlhan B, Çal E, Dündar N, Güneri P, Dağhan Ş. Oral health-related quality of life among institutionalized patients after dental rehabilitation. Geriatr Gerontol Int. 2015;15:1151–7. doi: 10.1111/ggi.12413. [DOI] [PubMed] [Google Scholar]


