Abstract
Immunotherapy is widely used in the treatment of different cancer types, including metastatic melanoma, non-small cell lung cancer, renal cell carcinoma and urothelial cancer. The results of the phase I JAVELIN study failed to demonstrate a substantial activity of the PDL-1 inhibitor Avelumab in advanced adrenocortical carcinoma (ACC). This editorial focus on the possible mechanisms of ACC immunoevasion and suggests strategies to overcome the intrinsic immunotherapy resistance of this disease.
Adrenocortical carcinoma (ACC) is a rare endocrine neoplasia characterized by an overall dismal prognosis and its clinical manifestations are the consequence of either steroid excess or tumor mass progression (1). Surgery is the mainstay of therapy. For patients with locally advanced or metastatic ACC, not amenable to surgery, mitotane and cytotoxic chemotherapy (with etoposide, doxorubicin and cisplatin – EDP scheme) are the systemic treatments currently in use (2).
No effective second-line therapies are available for patients with disease progression to EDP and mitotane (3).
The concept that immune system modulation can lead to a long-lasting control of tumor growth is well known since decades. However, the interest for cancer immunotherapies used in the past, such as interleukin-2, was modest due to the ability of tumor cells to avoid elimination by the immune system (4).
Over the past two decades, a tremendous progress has been made in the understanding of how cancer evades the immune system, as well as the ways to counteract the cancer immune evasion (5).
Basic science uncovered the pathways restraining antitumor immunity and drugs targeting immune checkpoint molecules, such as cytotoxic T-lymphocyte antigen 4 (CTLA-4), programmed death 1 (PD-1) and programmed death ligand 1 (PD-L1), are important therapeutic breakthroughs in medical oncology (5). These drugs have demonstrated to be efficacious (and obtained the US Food and Drug Administration – FDA – approval) against a broad spectrum of cancer types including metastatic melanoma, non-small-cell lung cancer, renal cell carcinoma and urothelial cancer (6, 7, 8, 9).
There is a rational in the use of immunotherapy also in ACC. This tumor, in fact, has an intermediate mutational load (8.9% of cells with a number of non-synonymous mutations more than 192) (10), that is a surrogate indicator of immune responsiveness (11). In addition, Melan-A/MART1, one of the most immunogenic antigen in melanoma (12), is widely expressed in adrenocortical tumors, being one of the markers used to identify lesions with adrenocortical origin (13).
JAVELIN study is a phase 1, open-label, dose-escalation trial of avelumab, antibody targeting PD-L1, with consecutive parallel group expansion in subjects with selected tumor indications (ClinicalTrials.gov Identifier: Nbib1772004). One of the study cohort included ACC patients previously treated with platinum-based chemotherapy. They received avelumab at 10 mg/kg IV every 2 weeks until progression, unacceptable toxicity or withdrawal. Prior and ongoing treatment with mitotane was permitted. Considering 50 patients, this represents the largest prospective study testing immunotherapy in ACC. The recently published results (14), showed a confirmed overall response rate (ORR) of 6.0% (95% confidence interval (CI): 1.3–16.5), a median progression-free survival (PFS) of 2.6 months (95% CI 1.4–4.0) and a median overall survival (OS) of 10.6 months (95% CI 7.4–not estimable).
These results were similar to the ORR of 4.9%, PFS of 3 months and OS of 10 months obtained by a standard second-line therapy with gemcitabine and metronomic capecitabine (15), employed in a real world practice setting in a retrospective multicenter study (16).
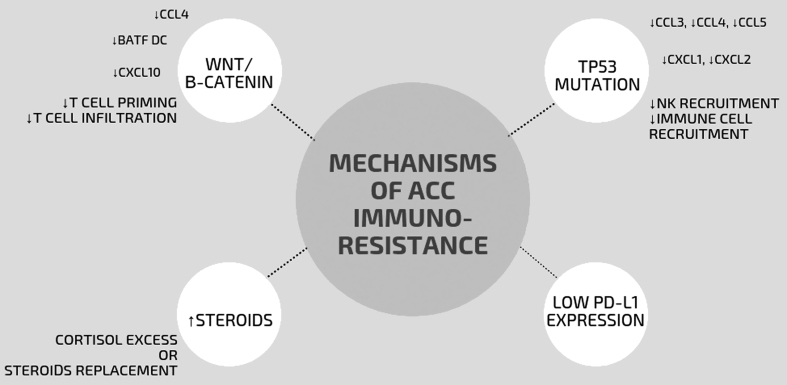
So, why immunotherapy can lead to such modest results in ACC patients? Tumor intrinsic and/or systemic factors could impair immunotherapy activity in this disease (Fig. 1).
Figure 1.
Mechanisms of ACC immunoresistance. The upregulation of β-catenin reduces production of different chemokines (such as CCL4, BATF Dcs, CXCL10) leading to the lack of T cell priming and the consequent recruitment of effector T cells in the tumor. TP53‐mutated tumor cells lack production of key chemokines required for the recruitment of natural killer cells and T cells, which results in exclusion of effector T cell from the tumor infiltration. Low PD-L1 expression and increased production of steroids can impair tumor immunogenicity. BATF DC, basic leucine zipper transcriptional factor ATF-like 3 lineage dendritic cells; CCL, CC-chemokine ligand; CXCL, CXC-chemokine ligand; PD-L1, programmed cell death 1 ligand 1.
First of all, PDL-1 expression, a well-known predictor of activity and better survival for cancer patients treated with immune checkpoint inhibitors (17), was found in a minority of ACC neoplasms (18). Moreover, the majority of ACC patients has a hormone-secreting disease and glucocorticoids are known to exert an immunosuppressive effect (19). Thus, both endogenous glucocorticoid levels, due to tumor secretion, and glucocorticoid supplementation in patients treated with mitotane have the potential to impair immunotherapy efficacy in ACC patients (20).
More importantly, responsiveness to checkpoint blockade immunotherapy requires the presence of CD8+ T cells within the local tumor microenvironment. As recently pointed out (21), molecular analyses revealed that the activation of specific oncogenic pathways in tumor cells leads to an altered production of CD8+ infiltrate thus impairing the local antitumor immune response. At least five pathways have been identified that may impair CD8+ action: (1) activation of WNT-β‐catenin pathway or (2) activation of MYC signaling, (3) loss of liver kinase B1 (LKB1) signaling, (4) loss of PTEN protein function and (5) TP53 mutations. Two of these pathways, namely WNT-B-catenin amplification and TP53 mutation, are involved in the pathogenesis of ACC. Upregulation of β-catenin reduces production by different chemokines, such as CC-chemokine ligand 4 (CCL4), leading to a defective recruitment of BATF3 dendritic cells (basic leucine zipper transcriptional factor ATF-like 3 lineage) and the lack of effector T cell infiltration. Similarly, TP53‐mutated tumor cells lack production of key chemokines required for the recruitment of natural killer cells and T cells, which results in effector T cell exclusion from the tumor infiltration (21, 22, 23).
All these potential mechanisms of immunoresistance are summarized in Fig. 1.
On these grounds, an effective strategy to overcome the immune evasion in ACC could be the administration of immune checkpoint inhibitors in association with drugs targeting the WNT-beta catenin and p53 pathways.
Both active inhibitors of Wnt secretion and Wnt/receptor interactions are being tested in early phase trials (24). Approaches aimed at upregulating p53 are under exploration, including gene therapy that uses viruses to deliver p53 to cancer cells, synthetic peptides that stabilize WT p53 and small molecules that target key signaling interactions involving mutant p53 (25). Moreover, β-catenin-induced immunotherapy resistance could be reversed by injection of mature dendritic cells into β-catenin-positive tumors (26).
None of these new drugs and treatment strategies, however, will be available soon in the management of ACC.
So what kind of immunotherapy trials can be currently designed? Immune checkpoint inhibitors can be tested in selected ACC patients, such as those with alterations in the mismatch repair (MMR) pathway that leads to high levels of microsatellite instability (MSI-H). Pertinently, MSI-H constitutes the molecular etiology of Lynch syndrome, an autosomal dominant genetic condition that has a high risk of colon cancer as well as other cancers including ACC (27). The damage to the MMR process leads to additive mutations throughout the genome, leading to a ‘hypermutator’ phenotype that is a predisposing condition of response to immunotherapy. Moreover, there is an increasing interest in combining chemotherapy, radiotherapy or molecular target therapies with immunotherapy (28, 29) and of course also agents inhibiting steroid synthesis may have a role in pretreatment of ACCs with cortisol excess aiming to avoid interference with the efficacy of following immunotherapy. In a recently published prospective clinical trial, the addition of a monoclonal anti-PD-L1 antibody atezolizumab to chemotherapy in the first-line treatment of advanced/metastatic small-cell lung cancer resulted in significantly longer OS than chemotherapy alone (30). On the basis of these results, the efficacy of the standard EDP-M can be improved by the combination with a checkpoint inhibitor.
In conclusion, Paul Carpenter published in 1993 an editorial entitled ‘Mitotane failure in adrenocortical cancer: where next?’ as a comment of some negative results obtained with this drug at that time (31). In the subsequent years, we have learned how to better use this drug with the introduction of serum levels monitoring and the identification of the so-called ‘therapeutic range’ to be attained (32, 33). Mitotane is currently the most important drug in this disease, and it is recommended and widely used also in adjuvant setting (34). We hope that the present editorial with a similar title to that of Paul Carpenter could be auspicious for a future demonstration of efficacy of immunotherapy in ACC.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this editorial.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Acknowledgements
The authors gratefully acknowledge the support and generosity of FIRM Onlus Foundation, Cremona, Italy.
References
- 1.Puglisi S, Perotti P, Cosentini D, Roca E, Basile V, Berruti A, Terzolo M. Decision-making for adrenocortical carcinoma: surgical, systemic, and endocrine management options. Expert Review of Anticancer Therapy 2018. 18 1125–1133. ( 10.1080/14737140.2018.1510325) [DOI] [PubMed] [Google Scholar]
- 2.Fassnacht M, Dekkers O, Else T, Baudin E, Berruti A, de Krijger RR, Haak HR, Mihai R, Assie G, Terzolo M. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. European Journal of Endocrinology 2018. 179 G1–G46. ( 10.1530/EJE-18-0608) [DOI] [PubMed] [Google Scholar]
- 3.Ferrari L, Claps M, Grisanti S, Berruti A. Systemic therapy in locally advanced or metastatic adrenal cancers: a critical appraisal and clinical trial update. European Urology Focus 2016. 1 298–300. ( 10.1016/j.euf.2015.06.005) [DOI] [PubMed] [Google Scholar]
- 4.Amin A, White RL., Jr High-dose interleukin-2: is it still indicated for melanoma and RCC in an era of targeted therapies? Oncology 2013. 27 680–691. [PubMed] [Google Scholar]
- 5.Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, Iyer AK. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Frontiers in Pharmacology 2017. 8 561 ( 10.3389/fphar.2017.00561) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuo JC. Immune checkpoint inhibitors in the treatment of advanced mucosal melanoma. Melanoma Management 2017. 4 161–167. ( 10.2217/mmt-2017-0014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suresh K, Naidoo J, Lin CT, Danoff S. Immune checkpoint immunotherapy for non-small cell lung cancer: benefits and pulmonary toxicities. Chest 2018. [epub]. ( 10.1016/j.chest.2018.08.1048) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rassy EE, Khoury Abboud RM, Ibrahim N, Assi T, Aoun F, Kattan J. The current state of immune checkpoint inhibitors in the first-line treatment of renal cancer. Immunotherapy 2018. 10 1047–1052. ( 10.2217/imt-2018-0017) [DOI] [PubMed] [Google Scholar]
- 9.Kim HS, Seo HK. Immune checkpoint inhibitors for urothelial carcinoma. Investigative and Clinical Urology 2018. 59 285–296. ( 10.4111/icu.2018.59.5.285) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colli LM, Machiela MJ, Myers TA, Jessop L, Yu K, Chanock SJ. Burden of nonsynonymous mutations among TCGA cancers and candidate immune checkpoint inhibitor responses. Cancer Research 2016. 76 3767–3772. ( 10.1158/0008-5472.CAN-16-0170) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyu G-Y, Yeh Y-H, Yeh Y-C, Wang Y-C. Mutation load estimation model as a predictor of the response to cancer immunotherapy. NPJ Genomic Medicine 2018. 3 12 ( 10.1038/s41525-018-0051-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ordóñez NG. Value of melanocytic-associated immunohistochemical markers in the diagnosis of malignant melanoma: a review and update. Human Pathology 2014. 45 191–205. ( 10.1016/j.humpath.2013.02.007) [DOI] [PubMed] [Google Scholar]
- 13.Volante M, Buttigliero C, Greco E, Berruti A, Papotti M. Pathological and molecular features of adrenocortical carcinoma: an update. Journal of Clinical Pathology 2008. 61 787–793. ( 10.1136/jcp.2007.050625) [DOI] [PubMed] [Google Scholar]
- 14.Le Tourneau C, Hoimes C, Zarwan C, Wong DJ, Bauer S, Claus R, Wermke M, Hariharan S, von Heydebreck A, Kasturi V, et al Avelumab in patients with previously treated metastatic adrenocortical carcinoma: phase 1b results from the JAVELIN solid tumor trial. Journal for Immunotherapy of Cancer 2018. 6 111 ( 10.1186/s40425-018-0424-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sperone P, Ferrero A, Daffara F, Priola A, Zaggia B, Volante M, Santini D, Vincenzi B, Badalamenti G, Intrivici C, et al Gemcitabine plus metronomic 5-fluorouracil or capecitabine as a second-/third-line chemotherapy in advanced adrenocortical carcinoma: a multicenter phase II study. Endocrine-Related Cancer 2010. 17 445–453. ( 10.1677/ERC-09-0281) [DOI] [PubMed] [Google Scholar]
- 16.Henning JEK, Deutschbein T, Altieri B, Steinhauer S, Kircher S, Sbiera S, Wild V, Schlötelburg W, Kroiss M, Perotti P, et al. Gemcitabine-based chemotherapy in adrenocortical carcinoma: a multicenter study of efficacy and predictive factors. Journal of Clinical Endocrinology and Metabolism 2017. 102 4323–4332. ( 10.1210/jc.2017-01624) [DOI] [PubMed] [Google Scholar]
- 17.Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, Chen L, Pardoll DM, Topalian SL, Anders RA. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clinical Cancer Research 2014. 20 5064–5074. ( 10.1158/1078-0432.CCR-13-3271) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fay AP, Signoretti S, Callea M, Telό GH, McKay RR, Song J, Carvo I, Lampron ME, Kaymakcalan MD, Poli-de-Figueiredo CE, et al Programmed death ligand-1 expression in adrenocortical carcinoma: an exploratory biomarker study. Journal for ImmunoTherapy of Cancer 2015. 3 3 ( 10.1186/s40425-015-0047-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flint TR, Janowitz T, Connell CM, Roberts EW, Denton AE, Coll AP, Jodrell DI, Fearon DT. Tumor-induced IL-6 reprograms host metabolism to suppress anti-tumor immunity. Cell Metabolism 2016. 24 672–684. ( 10.1016/j.cmet.2016.10.010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connell CM, Raby S, Beh I, Flint TR, Williams EH, Fearon DT, Jodrell DI, Janowitz T. Cancer immunotherapy trial registrations increase exponentially but chronic immunosuppressive glucocorticoid therapy may compromise outcomes. Annals of Oncology 2017. 28 1678–1679. ( 10.1093/annonc/mdx181) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spranger S, Gajewski TF. Impact of oncogenic pathways on evasion of antitumour immune responses. Nature Reviews Cancer 2018. 18 139–147. ( 10.1038/nrc.2017.117) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu S, Ding G, Zhou Z, Feng C. β-Catenin-driven adrenocortical carcinoma is characterized with immune exclusion. OncoTargets and Therapy 2018. 11 2029–2036. ( 10.2147/OTT.S159979) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wasserman JD, Zambetti GP, Malkin D. Towards an understanding of the role of p53 in adrenocortical carcinogenesis. Molecular and Cellular Endocrinology 2012. 351 101–110. ( 10.1016/j.mce.2011.09.010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Hao J. Development of anticancer agents targeting the Wnt/β-catenin signaling. American Journal of Cancer Research 2015. 5 2344–2360. [PMC free article] [PubMed] [Google Scholar]
- 25.Mantovani F, Walerych D, Sal GD. Targeting mutant p53 in cancer: a long road to precision therapy. FEBS Journal 2017. 284 837–850. ( 10.1111/febs.13948) [DOI] [PubMed] [Google Scholar]
- 26.Spranger S, Bao R, Gajewski TF. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature 2015. 523 231–235. ( 10.1038/nature14404) [DOI] [PubMed] [Google Scholar]
- 27.Raymond VM, Everett JN, Furtado LV, Gustafson SL, Jungbluth CR, Gruber SB, Hammer GD, Stoffel EM, Greenson JK, Giordano TJ, et al Adrenocortical carcinoma is a lynch syndrome-associated cancer. Journal of Clinical Oncology 2013. 31 3012–3018. ( 10.1200/JCO.2012.48.0988) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhalla N, Brooker R, Brada M. Combining immunotherapy and radiotherapy in lung cancer. Journal of Thoracic Disease 2018. 10 (Supplement 13) S1447–S1460. ( 10.21037/jtd.2018.05.107) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ko EC, Formenti SC. Radiotherapy and checkpoint inhibitors: a winning new combination? Therapeutic Advances in Medical Oncology 2018. 10 1758835918768240 ( 10.1177/1758835918768240) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horn L, Mansfield AS, Szczęsna A, Havel L, Krzakowski M, Hochmair MJ, Huemer F, Losonczy G, Johnson ML, Nishio M, et al First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. New England Journal of Medicine 2018. [epub]. ( 10.1056/NEJMoa1809064) [DOI] [PubMed] [Google Scholar]
- 31.Carpenter PC. Mitotane failure in adrenocortical cancer: where next? Cancer 1993. 71 2900–2901. () [DOI] [PubMed] [Google Scholar]
- 32.Hermsen IG, Fassnacht M, Terzolo M, Houterman S, den Hartigh J, Leboulleux S, Daffara F, Berruti A, Chadarevian R, Schlumberger M, et al Plasma concentrations of o,p′DDD, o,p′DDA, and o,p′DDE as predictors of tumor response to mitotane in adrenocortical carcinoma: results of a retrospective ENS@T multicenter study. Journal of Clinical Endocrinology and Metabolism 2011. 96 1844–1851. ( 10.1210/jc.2010-2676). [DOI] [PubMed] [Google Scholar]
- 33.Terzolo M, Zaggia B, Allasino B, De Francia S. Practical treatment using mitotane for adrenocortical carcinoma. Current Opinion in Endocrinology and Diabetes and Obesity 2014. 21 159–165. ( 10.1097/MED.0000000000000056) [DOI] [PubMed] [Google Scholar]
- 34.Berruti A, Grisanti S, Pulzer A, Claps M, Daffara F, Loli P, Mannelli M, Boscaro M, Arvat E, Tiberio G, et al Long-term outcomes of adjuvant mitotane therapy in patients with radically resected adrenocortical carcinoma Journal of Clinical Endocrinology and Metabolism 2017. 102 1358–1365. ( 10.1210/jc.2016-2894) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a