Abstract
Background:
The majority of Achilles tendon ruptures are sports related; however, no investigation has examined the impact of surgical repair for complete ruptures on professional soccer players.
Purpose:
To examine the return to play, playing time, and performance of professional soccer players following Achilles tendon repair.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Union of European Football Associations (UEFA) and Major League Soccer (MLS) athletes who sustained a primary complete Achilles tendon rupture and were treated surgically between 1988 and 2014 were identified via public injury reports. Demographic information and performance-related statistics for the identified athletes were recorded for the season before surgery and 2 seasons after surgery and were compared with information for matched controls. Statistical analyses were used to assess differences in recorded metrics.
Results:
A total of 24 athletes with Achilles ruptures met inclusion criteria, 17 (70.8%) of whom were able to return to play. On average, players had 8.3 years of professional-level experience prior to sustaining an Achilles rupture. Among athletes who returned to play, no differences were found in the number of games played or started, minutes played, or goals scored 1 year postoperatively compared with the year prior to injury. However, 2 years postoperatively, these athletes played 28.3% (P = .028) fewer minutes compared with their preoperative season, despite starting and playing in an equivalent number of games. Matched controls had baseline playing time and performance statistics similar to those of players. However, controls played and started in significantly more games and played more minutes at 1 and 2 years compared with players (P < .05). No differences were found in goals scored at any time point.
Conclusion:
This is the first investigation examining the effect of an Achilles repair on the career of professional soccer players. This is a difficult injury that most commonly occurs in veteran players and prevents 29.2% of players from returning to play despite surgical management. Additionally, athletes able to return to play were found to play fewer minutes 2 years postoperatively compared with their baseline as well as playing less at 1 and 2 years postoperatively compared with uninjured matched controls. The reduction in playing time following an Achilles repair has significant implications for professional players and teams.
Keywords: soccer, Achilles tendon, Achilles repair, return to play, Union of European Football Associations, Major League Soccer
Soccer is among the most popular sports in the world, being played by more than 200 million people.9 It is also one of the fastest growing sports in the United States, where 20 million players are registered and 1 million play competitively.8,22 As participation in soccer continues to increase, injury rates can be expected to follow a similar trend. Although injury incidence within the literatures varies widely, some investigators have reported that the match injury incidence is as high as 30 per 1000 hours of exposure while the training injury incidence is lower, at 5 per 1000 hours of exposure.11 Not unexpectedly, the majority of severe soccer injuries, 60% to 80%, occur in the lower extremity.1,5 Although numerous investigations have been conducted regarding anterior cruciate ligament (ACL) ruptures, hamstring and adductor strains, and ankle ligament injuries in professional soccer players, limited information is available regarding Achilles tendon ruptures in this patient population.5–8,17
Rupture of the Achilles tendon requires 2 pathologic processes: tendinosis, or a focus of degeneration within the tendon, and an eccentric contracture of sufficient force to rupture the diseased tendon.4 These injuries are more common in men, typically affect the “weekend warrior,” have an incidence in the general population ranging from 8.3 to 24 per 100,000, and have been found to increase in frequency over time.12–14,19,29 Furthermore, a recent systematic review found that an average 80% of patients are able to return to play (RTP) at a mean of 6.0 months following an Achilles tendon rupture.4,31 The majority of Achilles tendon ruptures are sports related, and while the optimal treatment for Achilles ruptures continues to be debated, some authors have advocated surgical repair in elite athletes.15,18,26
Outcomes, particularly RTP, following numerous orthopaedic injuries and procedures have been documented in a number of professional athletes in the National Basketball Association (NBA), National Football League (NFL), Major League Baseball (MLB), and National Hockey League (NHL).2,3,21,25,27 Trofa et al30 showed that athletes in these leagues experienced a 30.6% rate of failure to RTP following an Achilles rupture treated surgically and that all performance outcomes measured were significantly affected compared with preinjury levels. Thus, despite near-limitless resources to help facilitate appropriate rehabilitation, an Achilles rupture can be a career-threatening injury among elite athletes. However, a similar investigation has not been performed in elite soccer players. The purpose of the current investigation was to determine the RTP rate and functional outcomes of professional soccer players after a primary Achilles tendon repair. The hypothesis was that a significant proportion of athletes would not RTP following repair and that various performance measures would be significantly impaired compared with preinjury baselines and matched controls 1 and 2 years after surgery.
Methods
Publicly available injury reports, press releases, and player profiles were accessed to yield a list of professional athletes in the Union of European Football Associations (UEFA) and Major League Soccer (MLS) who sustained a primary complete Achilles tendon rupture and subsequently underwent surgical repair between 1988 and 2014. This information was obtained from such sources as www.transfermarket.com, www.espn.com, www.eufa.com, www.mlssoccer.com, and individual team websites. Inclusion criteria for athletes required professional participation in at least 1 game for the season prior to rupture and no confounding injuries. Goalkeepers were excluded because the different roles between these athletes and field players would not allow a fair comparison.
Two matched controls were subsequently selected for all players who returned to play. To match athletes who met the inclusion criteria of the study and controls, a stratified search was performed. First, players within the same league as the injured athlete were collected. Second, those uninjured athletes who did not play the same position as the injured athlete at the time of their injury were eliminated. Third, uninjured athletes who had not played in professional soccer for at least as many years as injured athletes at the time of their injury were eliminated. Finally, if more than 2 potential controls remained after this stratification, then the 2 athletes with the most similar playing statistics to the injured athlete were chosen as controls. Playing statistics assessed included number of games played, playing time, games started, and goals scored. Professional leagues were included in the matching criteria in order to eliminate variations in length of regular season soccer between leagues of different countries and to alleviate variations in player skill across different leagues within the same country. Controls were also verified to have no history of significant lower extremity injury or surgical treatments.
Online databases and publicly available sports statistics websites were mined to find demographic, playing time, and performance-related data for players and controls. Demographic information obtained included age, body mass index, years of professional league experience, and position. The primary outcome of the investigation was RTP following surgical treatment of an Achilles tendon rupture. A strict definition of RTP was implemented, requiring involvement in at least 1 game for 2 consecutive years, ensuring sustained professional level play. Secondary outcomes included comparisons of preoperative versus postoperative playing time, as measured by the number of games played and minutes played; and performance, assessed by the number of games started and goals scored. For injured players, the season prior to which injury and surgical repair occurred was considered to be the index season. Statistics of interest as outlined above were recorded for the index season and 1 and 2 years following surgery. The same measurements were recorded in matched controls, and the index season was defined as the year in which the athlete had participated in an equal number of seasons as the matched player’s index season. As such, the index seasons for players and controls were not required to be from the same calendar year.
Statistical analyses were conducted via PRISM version 7.0b (GraphPad Software). Preinjury versus postinjury performance was compared in players with Achilles tendon rupture through use of a 2-tailed paired t test, and comparisons between athletes with Achilles tendon rupture and matched controls were performed with 2-tailed unpaired t tests.
Results
Overall, 29 athletes were identified as sustaining an Achilles tendon rupture, of whom 24 met inclusion criteria. Reasons for exclusion included partial Achilles tear (n = 2), goalkeeper position (n = 1), and confounding injury (n = 2). Seven (29.2%) of the remaining athletes did not RTP in the 2 seasons following surgery. The 17 athletes who returned consisted of 1 MLS player and 16 UEFA players, and their demographic and baseline characteristics can be seen in Table 1. Although the mean age of players not returning to play was higher than those able to return, it was not significantly different (30.1 vs 28.2 years; P = .31). Returning athletes had an average 8.3 (range, 2-17) seasons of professional soccer experience (Table 1), and the majority of players were midfielders (64.7%).
TABLE 1.
Demographic and Baseline Characteristics of Players and Controls at their Respective Index Seasonsa
| Players | Controls | P Value | |
|---|---|---|---|
| Age, y | 28.2 ± 2.8 | 27.6 ± 3.7 | .53 |
| Body mass index, kg/m2 | 24.1 ± 1.9 | 23.3 ± 1.6 | .14 |
| No. of professional seasons | 8.3 ± 3.8 | 7.8 ± 3.2 | .65 |
| Position, n | |||
| Defense | 4 | 8 | |
| Midfield | 11 | 22 | |
| Forward | 2 | 4 | |
| No. of games played | 27.9 ± 7.8 | 27.1 ± 8.1 | .72 |
| Minutes played | 2112 ± 785 | 2137 ± 840 | .92 |
| No. of games started | 22.2 ± 10.4 | 24.0 ± 9.7 | .56 |
| No. of goals scored | 4.8 ± 6.1 | 4.8 ± 7.0 | >.99 |
aValues are expressed as mean ± SD except for playing position.
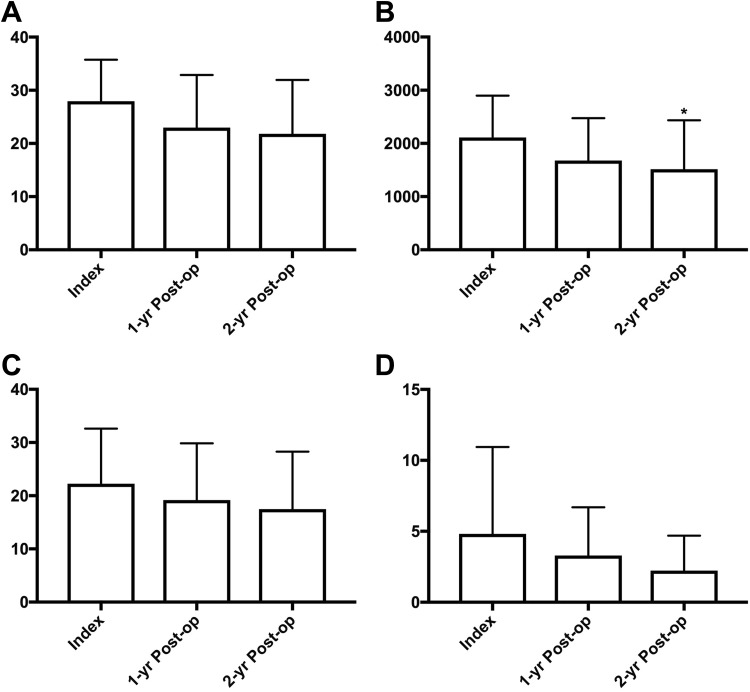
Among athletes returning to play, no significant decreases in playing time or performance in the season following surgery compared with the index season were seen (Table 2 and Figure 1). At 2 years postoperatively, athletes played an average of 78.1% of the games and 71.7% of the minutes played in the season prior to injury, but only the reduction in minutes played was found to be significant (P = .028). The proportion of games started and goal scores also decreased 2 years postoperatively, 78.8% and 45.8%, respectively; however, these differences were not significant.
TABLE 2.
Comparison of Index Versus 1-Year and 2-Year Postoperative Playing Time and Performance in Playersa
| Index | 1 Year Postoperative (P value) | 2 Years Postoperative (P value) | |
|---|---|---|---|
| Games played | 27.9 ± 7.8 | 22.9 ± 9.9 (.114) | 21.8 ± 10.1 (.051) |
| Minutes played | 2112 ± 785 | 1679 ± 797 (.148) | 1514 ± 876 (.028b) |
| Games started | 22.2 ± 10.4 | 19.2 ± 10.7 (.317) | 17.5 ± 10.8 (.156) |
| Goals scored | 4.8 ± 6.1 | 3.3 ± 3.4 (.187) | 2.2 ± 2.5 (.068) |
aValues are expressed as mean ± SD.
bStatistically significant difference compared with index year (P < .05).
Figure 1.
Index versus 1-year and 2-year postoperative comparisons of (A) games played, (B) minutes played, (C) games started, and (D) goals scored among professional soccer players sustaining an Achilles rupture. *P < .05 compared with index year.
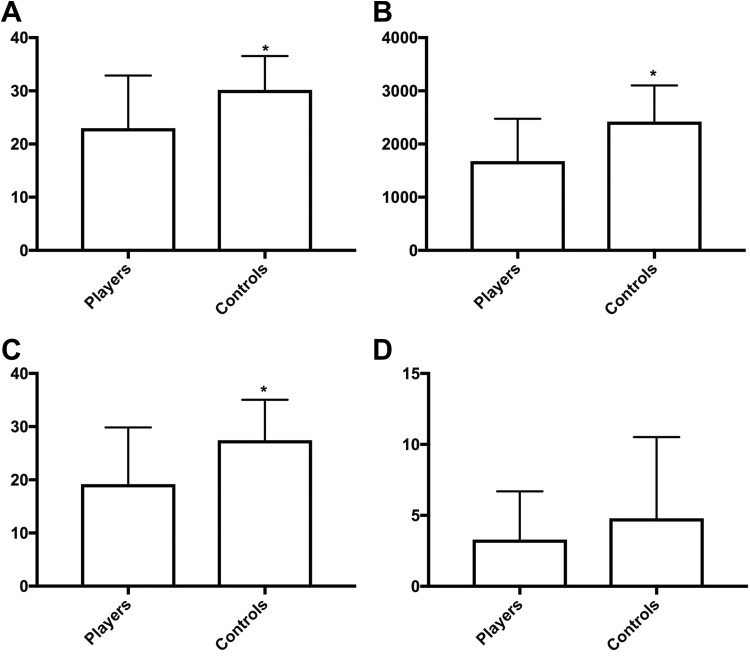
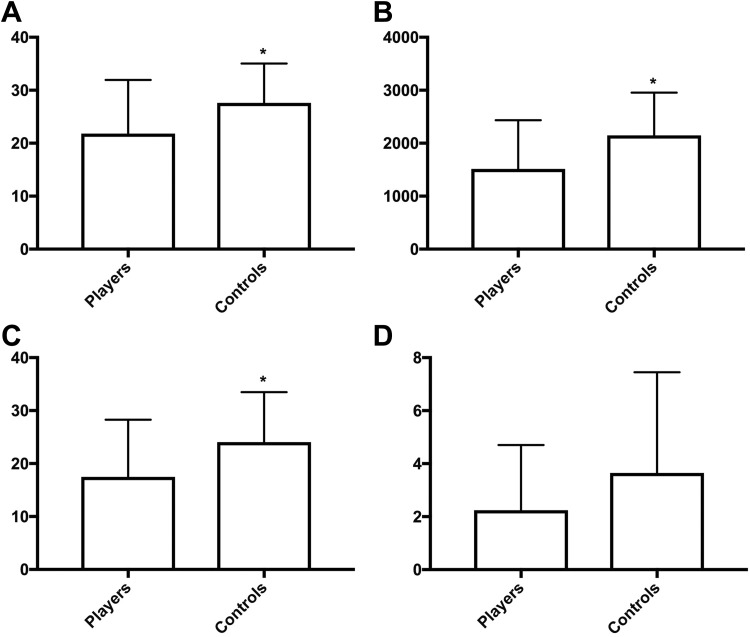
Two matched controls were identified for each injured player. No baseline differences were found at any parameter examined between each group’s respective index season (Table 1). Additionally, no differences were found in any outcome measure compared between the index season and postoperative season 1 or 2 among controls. Despite this, playing time and performance measures were significantly compromised among players compared with controls postoperatively (Table 3, Figures 2 and 3). At 1 year postoperatively, injured players participated in 24.2% fewer games (P = .003), played 30.6% fewer minutes (P = .001), and started in 29.9% fewer games (P = .003) compared with controls. This trend continued 2 years postoperatively, where players participated in 21.0% fewer games (P = .025), played 29.5% fewer minutes (P = .015), and started in 27.4% fewer games (P = .030). No significant differences were identified in the number of goals scored.
TABLE 3.
Postoperative Comparisons of Playing Time and Performance Between Players and Controlsa
| 1 Year Postoperatively | 2 Years Postoperatively | |||||
|---|---|---|---|---|---|---|
| Players | Controls | P Value | Players | Controls | P Value | |
| Games played | 22.9 ± 9.9 | 30.2 ± 6.4 | .003b | 21.8 ± 10.1 | 27.6 ± 7.4 | .025b |
| Minutes played | 1679 ± 797 | 2421 ± 682 | .001b | 1514 ± 876 | 2148 ± 806 | .015b |
| Games started | 19.2 ± 10.7 | 27.4 ± 7.6 | .003b | 17.5 ± 10.8 | 24.1 ± 9.4 | .030b |
| Goals scored | 3.3 ± 3.4 | 4.8 ± 5.7 | .326 | 2.2 ± 2.5 | 3.7 ± 3.8 | .172 |
aValues are expressed as mean ± SD.
bStatistically significant difference between groups (P < .05).
Figure 2.
One-year postoperative comparison of (A) games played, (B) minutes played, (C) games started, and (D) goals scored among professional soccer players sustaining an Achilles rupture and matched controls. *P < .05 between groups.
Figure 3.
Two-year postoperative comparison of (A) games played, (B) minutes played, (C) games started, and (D) goals scored among professional soccer players sustaining an Achilles rupture and matched controls. *P < .05 between groups.
Discussion
Successful repair of an Achilles tendon in the general population is measured by return to daily activities, including various levels of athletic participation, as well as the avoidance of complications such as rerupture and wound breakdown. These goals are adjusted in elite athletes given the high physical demands of their profession, where the goal of surgery is to RTP at a level equivalent to their preinjury performance or that of matched controls. As such, the success of an Achilles repair in this population requires increased objective scrutiny of various performance metrics, which can be difficult in a low-scoring sport such as soccer. The current case-control investigation of professional soccer players undergoing an Achilles tendon repair demonstrated a 70.8% RTP rate. These players not only returned to sport postoperatively but successfully competed for 2 years following their injury, ensuring sustained functional capacity to play.
To our knowledge, this is the first assessment of professional soccer players undergoing Achilles tendon repair. Previous literature has demonstrated that an Achilles tendon rupture can be detrimental to a professional athlete’s career. For example, RTP rates in NFL and NBA players have been found to be 68% to 73% and 61% to 71%, respectively.2,20,23,24 More specifically, Trofa et al30 recently performed an investigation of Achilles tendon ruptures among NFL, NBA, and MLB athletes, finding RTP rates of 66%, 68%, and 100%, respectively. The same investigation found that compared with controls, only 1-year postoperative performance metrics were significantly affected. This stands in contrast to soccer players treated for Achilles tendon ruptures, as they were unable to continue playing the same amount of time or to perform at a level commensurate with uninjured controls at both 1 and 2 years following surgery.
Despite performing worse than controls postoperatively, players did not have statistically impaired performance measures compared with their own index season. In fact, the only significant variable identified was a 28.3% reduction in minutes played 2 years postoperatively compared with the index season. This indicates that although players may have started and played in an equivalent number of games, they were either removed from the game earlier or substituted into the game later, possibly as a result of fatigue or poorer performance. However, it is important to note the vital difference between statistically significant results and what is important in the life of a recovering athlete. For instance, on average, players started and played in 13.5% and 17.9% fewer games, respectively, 1 year after surgery, and in 21.2% and 21.9% fewer games, respectively, the following year. Given that the ability to continue playing soccer at a high level determines players’ livelihood, such limitations are detrimental to professional players in ways researchers are simply unable to measure. Finally, it is worth noting that because control players continued to have a consistent amount of playing time over the course of the study, the decrease in minutes played among players with Achilles repairs is more likely a result of their injury as opposed to the natural aging process.
Various investigators have looked at the epidemiological patterns and/or treatment of other musculoskeletal injuries in soccer players.5–8,17,28 Studies that have specifically evaluated postinjury RTP and performance among elite players have focused on ACL reconstruction, ankle syndesmotic injuries, and the arthroscopic treatment of femoroacetabular impingement (FAI).7,8,16 A number of interesting comparisons can be made between these studies and the current investigation. For instance, an Achilles tendon rupture is an injury of veteran players.10 In our player cohort, the average age at the time of injury was 28.2 years, with an average 8.3 years of professional level of play. These data stand in contrast to investigations by Erickson et al,7 who reported that professional soccer players undergoing ACL reconstruction were on average 25.6 years old, and Locks et al,16 who noted that players with FAI underwent surgery at an average age of 25.0 years. The older age of patients sustaining Achilles tendon ruptures may, in part, explain the lower RTP rate compared with players recovering from both ACL reconstruction (77%) and FAI surgery (96%).
Additionally, an Achilles tendon rupture is a comparatively uncommon injury among professional soccer players. For example, between 1996 and 2012, a total of 52 professional players in a single league were identified with ACL ruptures, and in a single-surgeon series between 2005 and 2015, there were 24 professional players treated surgically for FAI.7,16 In the current investigation, after searching multiple leagues, we identified only 24 players who fit the inclusion criteria, which was a surprisingly low number given the overall number of professional soccer athletes. We hypothesize that this is a reflection of the pathologic process necessary to sustain an Achilles rupture, in that there must be underlying tendinosis in addition to an eccentric contracture to fully rupture the tendon. This tendinosis is likely more common in slightly older players. Also, given that tendinosis is a necessary precursor, many team physicians and trainers may aggressively address any tendinosis, thereby minimizing the risk of tendon rupture. Support for this argument comes from an 11-year epidemiological study on Achilles-related injuries in the UEFA, in which the 205 Achilles tendon injuries identified accounted for only 2.5% of all recorded injuries; however, 96% of these were tendinopathies.10 Finally, to our knowledge, only 1 other soccer investigation has compared postsurgical outcomes relative to controls. In that investigation, Erickson et al7 found that players treated for an ACL reconstruction played in significantly fewer games and took fewer total shots and shots on goal. The current investigation identified similarly impaired performances following an Achilles tendon repair compared with controls.
The strengths of this investigation include the use of simple and reproducible outcome variables. Furthermore, a strict definition of RTP was implemented, ensuring a sustained return to professional involvement for a minimum of 2 years. Finally, this is the first investigation of its kind to compare postoperative playing time and performance in professional soccer players after Achilles repair versus matched controls.
Despite these strengths, the investigation has certain limitations. First, a number of confounding variables could not be controlled by our method and may have affected a player’s calculated RTP and performance. These include differences in team playing style, coaching decisions, concomitant minor or unreported injuries that were not identified, athletes’ personal or professional decisions for retirement unrelated to medical conditions, and selection bias where more popular or well-known players were more easily identified for inclusion. Further, since the majority of data obtained in this investigation were from publicly accessible websites, no method was available to verify the accuracy or completeness of the available data. As such, given the low number of Achilles tendon ruptures identified, it is likely that the true incidence was underreported in this investigation. Additionally, over the period of time during which these data were collected, treatment paradigms changed significantly with regard to both surgical treatment and rehabilitation in a way that this investigation could not take into account, as we had no clinical data on these patients. The study design could also not account for various factors that may have affected recovery as well as the ability of players to RTP, including repair technique, use of augmentation, unreported complications, or individual rehabilitation protocols. In the same regard, the method of the investigation did not permit an analysis of other factors that may have influenced the players’ RTP rate, including contract timing, marketing factors, leadership positions, or personal decisions. Finally, Achilles tendon ruptures are rare injuries in this patient population, and the relatively small number of players identified for analysis may have limited the power of this investigation.
Conclusion
Across multiple professional soccer leagues, we found a 29.2% failure rate for RTP following an Achilles rupture treated surgically. Furthermore, those athletes who returned to play played significantly less compared with healthy controls postinjury. These results can help manage postoperative expectations of professional players and amateurs alike while also assisting orthopaedic professionals caring for athletes of all levels following an Achilles rupture. Future investigations may help elucidate whether treating tendinosis in more veteran soccer players, who appear to be at a higher risk of Achilles rupture, can minimize the risk of tendon rupture.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.K.G. receives research support from Extremity Medical and royalties from Saunders/Mosby Elsevier. C.S.A. is a consultant for Arthrex, Acumed, and DePuy and receives research support from Arthrex, Stryker, and Major League Baseball. J.T.V. is a consultant for DJ Orthopaedics, Arthrex, Gotham Surgical Solutions and Devices, and Stryker and receives royalties from NewClip Technics and Saunders/Mosby Elsevier. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Agel J, Evans TA, Dick R, Putukian M, Marshall SW. Descriptive epidemiology of collegiate men’s soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2002-2003. J Athl Train. 42(2):270–277. [PMC free article] [PubMed] [Google Scholar]
- 2. Amin NH, Old AB, Tabb LP, Garg R, Toossi N, Cerynik DL. Performance outcomes after repair of complete Achilles tendon ruptures in National Basketball Association players. Am J Sports Med. 2013;41(8):1864–1868. [DOI] [PubMed] [Google Scholar]
- 3. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 4. Egger AC, Berkowitz MJ. Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017;10(1):72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–558. [DOI] [PubMed] [Google Scholar]
- 6. Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club Injury Study. Br J Sports Med. 2016;50(12):731–737. [DOI] [PubMed] [Google Scholar]
- 7. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sports Med. 2013;1(2):2325967113497189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farber J, Harris JD, Kolstad K, McCulloch PC. Treatment of anterior cruciate ligament injuries by Major League Soccer team physicians. Orthop J Sports Med. 2014;2(11):2325967114559892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med. 2006;16(2):97–106. [DOI] [PubMed] [Google Scholar]
- 10. Gajhede-Knudsen M, Ekstrand J, Magnusson H, Maffulli N. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):763–768. [DOI] [PubMed] [Google Scholar]
- 11. Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40(3):584–588. [DOI] [PubMed] [Google Scholar]
- 12. Gwynne-Jones DP, Sims M, Handcock D. Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int. 2011;32(4):337–343. [DOI] [PubMed] [Google Scholar]
- 13. Ho G, Tantigate D, Kirschenbaum J, Greisberg JK, Vosseller JT. Increasing age in Achilles rupture patients over time. Injury. 2017;48(7):1701–1709. [DOI] [PubMed] [Google Scholar]
- 14. Houshian S, Tscherning T, Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish county. Injury. 1998;29(9):651–654. [DOI] [PubMed] [Google Scholar]
- 15. Lantto I, Heikkinen J, Flinkkilä T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1): e133–e138. [DOI] [PubMed] [Google Scholar]
- 16. Locks R, Utsunomiya H, Briggs KK, McNamara S, Chahla J, Philippon MJ. Return to play after hip arthroscopic surgery for femoroacetabular impingement in professional soccer players. Am J Sports Med. 2018;46(2):273–279. [DOI] [PubMed] [Google Scholar]
- 17. Lubberts B, D’Hooghe P, Bengtsson H, DiGiovanni CW, Calder J, Ekstrand J. Epidemiology and return to play following isolated syndesmotic injuries of the ankle: a prospective cohort study of 3677 male professional footballers in the UEFA Elite Club Injury Study [published online December 21, 2017]. Br J Sports Med. doi:10.1136/bjsports-2017-097710 [DOI] [PubMed] [Google Scholar]
- 18. Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in elite athletes. Foot Ankle Int. 2011;32(1):9–15. [DOI] [PubMed] [Google Scholar]
- 19. Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9(3):157–160. [DOI] [PubMed] [Google Scholar]
- 20. Mai HT, Alvarez AP, Freshman RD, et al. The NFL Orthopaedic Surgery Outcomes Database (NO-SOD): the effect of common orthopaedic procedures on football careers. Am J Sports Med. 2016;44(9):2255–2262. [DOI] [PubMed] [Google Scholar]
- 21. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43(5):1051–1056. [DOI] [PubMed] [Google Scholar]
- 22. Meyers MC. Incidence, mechanisms, and severity of match-related collegiate men’s soccer injuries on fieldturf and natural grass surfaces: a 6-year prospective study. Am J Sports Med. 2017;45(3):708–718. [DOI] [PubMed] [Google Scholar]
- 23. Minhas SV, Kester BS, Larkin KE, Hsu WK. The effect of an orthopaedic surgical procedure in the National Basketball Association. Am J Sports Med. 2016;44(4):1056–1061. [DOI] [PubMed] [Google Scholar]
- 24. Parekh SG, Wray WH, Brimmo O, Sennett BJ, Wapner KL. Epidemiology and outcomes of Achilles tendon ruptures in the National Football League. Foot Ankle Spec. 2009;2(6):283–286. [DOI] [PubMed] [Google Scholar]
- 25. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. [DOI] [PubMed] [Google Scholar]
- 26. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. [DOI] [PubMed] [Google Scholar]
- 27. Scillia AJ, Aune KT, Andrachuk JS, et al. Return to play after chondroplasty of the knee in National Football League athletes. Am J Sports Med. 2015;43(3):663–668. [DOI] [PubMed] [Google Scholar]
- 28. Stubbe JH, van Beijsterveldt A-MMC, van der Knaap S, et al. Injuries in professional male soccer players in the Netherlands: a prospective cohort study. J Athl Train. 2015;50(2):211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Suchak AA, Bostick G, Reid D, Blitz S, Jomha N. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26(11):932–936. [DOI] [PubMed] [Google Scholar]
- 30. Trofa DP, Miller JC, Jang ES, Woode DR, Greisberg JK, Vosseller JT. Professional athletes’ return to play and performance after operative repair of an Achilles tendon rupture. Am J Sports Med. 2017;45(12):2864–2871. [DOI] [PubMed] [Google Scholar]
- 31. Zellers JA, Carmont MR, Grävare Silbernagel K. Return to play post-Achilles tendon rupture: a systematic review and meta-analysis of rate and measures of return to play. Br J Sports Med. 2016;50(21):1325–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]