Introduction
Inhalant abuse is the intentional inhalation of volatile substances to achieve intoxication. Inhaled substances include cheap, easily accessible, legal, everyday products, and abuse is most common in adolescence. There is considerable morbidity and mortality associated with this underdetected form of substance abuse, such as cryogenic burns.1 These cryogenic burns may be easily overlooked by clinicians, especially in areas where exposure to freezing temperatures is uncommon. As the prevalence of inhalant abuse steadily increases because of its wide availability, more cryogenic burn cases will likely present to clinicians.
Case report
A 24 year old man with no significant medical history presented to the emergency department and was hospitalized for a painful rash. One week before admission, a progressive, tender, blistering rash developed, involving the left side of his upper chest, left arm and left hand. His lips, oral mucosa, and tongue were also involved with associated erosions and pain in his gums. The patient denied known precipitating factors including associated medication use, preceding infections, new or different topical products, travel history, insect bites, new or multiple sexual partners, and close contacts with similar eruptions. He did, however, report a similar rash on his right leg and groin 1 month before admission that resolved spontaneously with dark spots. The patient had no known allergies, and no personal or family history of skin disease. The patient vehemently denied use of drugs and alcohol. He works in a car factory on an assembly line and denied exposure to chemicals. He reports that since admission, the rash is stable and denies new areas of involvement.
Skin examination found blanching, erythematous to violaceous patches and plaques with sharply defined borders on the left side of the upper chest, shoulder, and arm (Fig 1, A). Tender, tense bullae were found on the left shoulder and left lateral arm (Fig 1, B). Thick yellow-brown plaques with yellow crust were noted on his right thumb. Postinflammatory hyperpigmentation was also noted on the proximal right leg and inguinal fold. Superficial erosions on his tongue and oral commissures with hemorrhagic crust were also noted, and the nasal tip contained a crusted plaque (Fig 1, C).
Fig 1.

Photos taken 7 days after the toxic insult.
In the emergency department, he was given intravenous fluids and broad-spectrum antibiotics for his nausea and vomiting and suspected cellulitis. Chest and abdominal radiographs and electrocardiogram results were normal. Laboratory tests found an elevated a leukocytosis (14.1) with neutrophilia (84%). Troponin levels were elevated to 1.180. Urine drug screen was negative.
Our initial differential diagnosis was broad and included vasculitides and vasculopathies (including levamisole vasculopathy), infectious etiologies (gonococcal, septic thrombosis), irritant or allergic dermatitis, fixed drug eruption, and chemical ingestion. We also considered erythema multiforme with associated viral etiology, given the gastrointestinal symptoms.
A broad, lesional shave biopsy was obtained from the left upper lateral arm for hematoxylin-eosin which showed epidermal necrosis with subepidermal bulla formation (Fig 2). Perilesional direct immunofluorescence was nondiagnostic without evidence of immunobullous disease, lupus, or lichenoid tissue reaction. Hepatitis B serology and hepatitis C polymerase chain reaction, rapid plasma reagin, rheumatoid factor, antineutrophil cytoplasmic antibodies, cryoglobulins, D-dimer, wound, and blood cultures were all normal.
Fig 2.
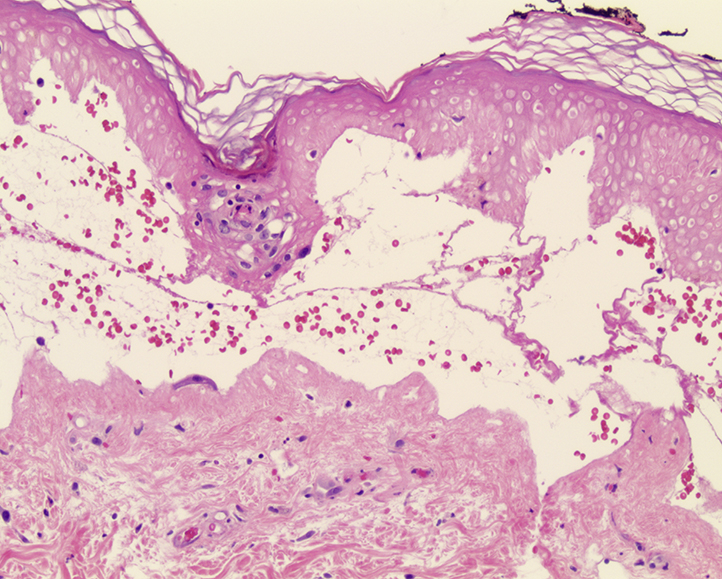
Pathology findings of skin biopsy show epidermal necrosis with subepidermal blister formation.
On hospital day 3, the patient's parents persuaded the patient to reveal that he abuses inhalants. Before admission, the patient had been huffing computer dust cleaning products, containing the hydrofluorocarbon, 1,1 difluoroethane, which is a known cause of cryogenic burns. Supportive dermatologic care was continued. He was medically optimized, provided with mental and drug dependence counseling, then discharged home in stable condition.
Unfortunately, the patient was lost to follow-up after discharge. Our prediction is that the spray can was held to the lips using his right hand with the index finger on the plastic trigger and his thumb in contact with the cool, metallic can. The cool inhalant material would come in contact with the lips, tongue, and oral mucosa. With loss of consciousness, he may have dropped the canister, which continued to express its contents and contact skin surfaces.
Discussion
Inhalant abuse, or the purposeful inhalation of toxic, industrial-use inhalants for temporary euphoria, is becoming increasingly common, especially among the adolescent population.2 Abusers typically inhale the substance directly from the container or from a bag or cloth to which the inhalant has been placed. Aerosol sprays contain a chemical propellant, usually a hydrocarbon such as propane, butane, or isobutene, stored in a pressurized liquid form. The intoxication is very brief, usually lasting seconds, making dependence very common. Acute intoxication produces dizziness, loss of coordination, euphoria, and sometimes loss of consciousness. It can result in chemical or thermal burns, as seen in this case.3 Experiments have found that aerosol spraying an object from 1 cm away brings its temperature down from room temperature to 0°C in 5 seconds and to –15°C in as little as 20 seconds.4 Another report showed that aerosol spraying from 5 cm decreased temperature to 0°C in 3 seconds.5 This is not representative of biological tissue like skin, but it does show how quickly an aerosol spray can cause frostbite.
Inhaled substances are very accessible to the young population, as they are sold legally for industrial purposes and at a low price. When the trigger is pulled, gas exits the nozzle at temperatures below freezing and immediately vaporizes. However, if the can is shaken or turned upside down, liquid will be released, freezing any tissue that may be exposed to it.6 There have been reports of patients inhaling directly to the mouth and losing consciousness with the container remaining open and continuing to release its contents until it is completely expired.7 This situation can create severe damage to the oral, pulmonary, and gastric mucosa as well as any skin in direct contact with the expressed gas/liquid.
Clinicians must have a high index of suspicion for inhalation abuse because as of now, there is no widely available way to detect inhalant abuse through blood or urine samples and patients may not be willing to divulge their use as demonstrated in this case. If suspected, a patient can be asked to complete a Volatile Solvent Screening Inventory, which is a freely available screen for inhalant abuse.8 Inhalant abuse should be considered in the differential diagnosis of cryogenic burn cases in the adolescent or young adult population, especially if the burns involve a periorofacial or unilateral hand distribution.
Footnotes
Funding sources: None
Conflicts of interest: None disclosed.
References
- 1.Williams J.F., Storck M. Inhalant abuse. Pediatrics. 2007;119(5):1009–1017. doi: 10.1542/peds.2007-0470. [DOI] [PubMed] [Google Scholar]
- 2.Howard M.O., Bowen S.E., Garland E.L., Perron B.E., Vaughn M.G. Inhalant use and inhalant use disorders in the United States. Addict Sci Clin Pract. 2011;6(1):18–31. [PMC free article] [PubMed] [Google Scholar]
- 3.Moreno C., Beierle E.A. Hydrofluoric acid burn in a child from a compressed air duster. J Burn Care Res. 2007;28(6):909–912. doi: 10.1097/BCR.0b013e318159a3b6. [DOI] [PubMed] [Google Scholar]
- 4.Camp D.F., Ateaque A., Dickson W.A. Cryogenic burns from aerosol sprays: a report of two cases and review of the literature. Br J Plast Surg. 2003;56(8):815–817. doi: 10.1016/j.bjps.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 5.May U., Stirner K.H., Lauener R., Ring J., Möhrenschlager M. Deodorant spray: a newly identified cause of cold burn. Pediatrics. 2010;126(3):e716–e718. doi: 10.1542/peds.2009-2936. [DOI] [PubMed] [Google Scholar]
- 6.Koehler M.M., Henninger C.A. Orofacial and digital frostbite caused by inhalant abuse. Cutis. 2014;93(5):256–260. [PubMed] [Google Scholar]
- 7.Kuspis D.A., Krenzelok E.P. Oral frostbite injury from intentional abuse of a fluorinated hydrocarbon. J Toxicol Clin Toxicol. 1999;37(7):873–875. doi: 10.1081/clt-100102469. [DOI] [PubMed] [Google Scholar]
- 8.Howard M.O., Balster R.L., Cottler L.B., Wu L.T., Vaughn M.G. Inhalant use among incarcerated adolescents in the United States: prevalence, characteristics, and correlates of use. Drug Alcohol Depend. 2008;93(3):197–209. doi: 10.1016/j.drugalcdep.2007.08.023. [DOI] [PubMed] [Google Scholar]


