Abstract
The rates of restenosis and stent thrombosis after the therapeutic stent deployment for bifurcation lesions are still comparably high after the introduction of the new-generation drug-eluting stents (DESs), because of the various factors including their morphology. We experienced a case of a successful percutaneous coronary intervention using three-dimensional optical coherence tomography (3D OCT) with a single stent deployment to a bifurcation lesion of the left anterior descending artery (LAD) and left circumflex artery (LCx) with a following kissing-balloon inflation (KBI). The 3D OCT, after the inflation of the jailed ostium of the LCx following the stent deployment to the LAD crossing the LCx, could clearly demonstrate a stent deformation and incomplete apposition at an opposite site of the LCx, which may cause high rates of restenosis and stent thrombosis. These stent abnormalities were steadily corrected by a subsequent KBI of the LAD and LCx. Furthermore, the 3D OCT images were the same findings as those of the experiments from both an in vitro phantom coronary bifurcation model and macroscopic images of the stent.
<Learning objective: In view of this case report, these modalities with three-dimensional optical coherence tomography and the techniques for the following kissing-balloon inflation may be one of the useful and effective therapeutic strategies to reduce the rates of restenosis and stent thrombosis of the percutaneous coronary intervention for bifurcation lesions.>
Keywords: Bifurcated lesion, Kissing-balloon inflation, Optical coherence tomography, Stent deformation
Introduction
Although the new-generation drug-eluting stents (DESs) have gained widespread use due to the low rates of restenosis and stent thrombosis, and lower risk of death [1], the rates of restenosis and stent thrombosis after the therapeutic stent deployment for bifurcation lesions are still comparably high, because of various factors including their morphology defined by the Medina bifurcation classification [2], the target vessel's reference diameter, bifurcation angle, design of the stents, and strategies of the stent implantation. Thus, the strategies used for those lesions are still not well established [3], [4], [5] in the new-generation DES era. Here we report a case that progressed satisfactorily after a bifurcation stenting using three-dimensional optical coherence tomography (3D OCT) (St. Jude Medical, ILUMIEN OPTIS™, St. Paul, MN, USA) and following a kissing-balloon inflation (KBI) for the bifurcation lesions.
Case report
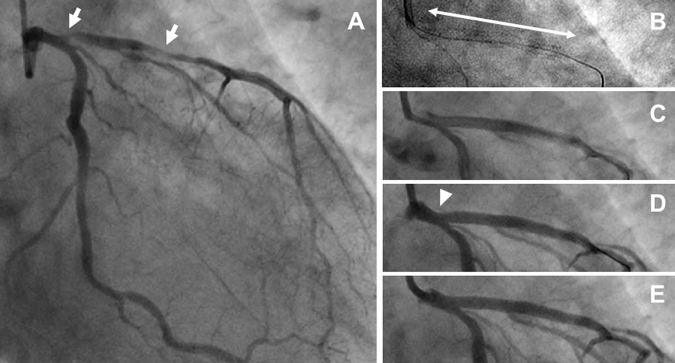
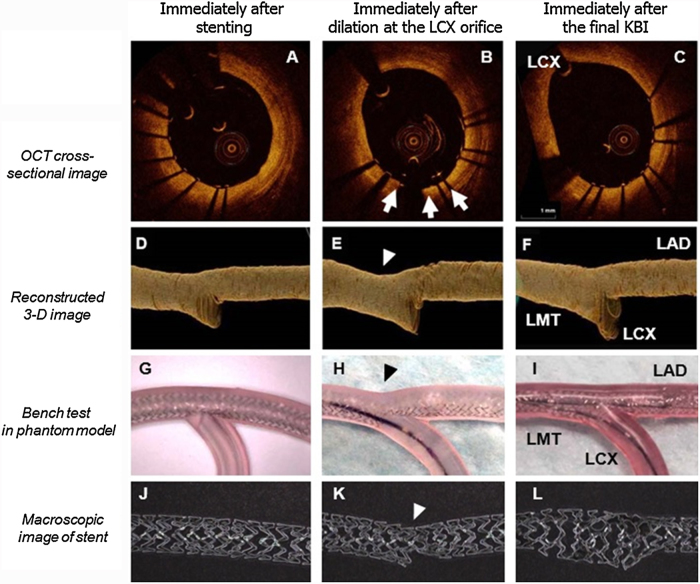
A 62-year-old male was admitted to our hospital with the chief complaint of increasing episodes of chest pain on exercise. His coronary risk factors included hypertension, dyslipidemia, and a family history of coronary artery disease. A 12-lead electrocardiogram revealed a T-wave inversion in the precordial leads. His plasma troponin I levels were significantly elevated, but the other cardiac enzymes were not. Since the emergent coronary angiography (CAG) revealed that there was one-vessel disease with a long diffuse narrow and severe stenosis of the proximal left anterior descending (LAD) coronary artery (Medina's classification 0, 1, 0 [2]) (Fig. 1A), percutaneous coronary intervention (PCI) with a new-generation DES was performed. The OCT before stenting revealed the diameter of the left main trunk (LMT) and the proximal LAD was 3.61 mm × 3.25 mm and 3.13 mm × 2.64 mm, respectively. First, we implanted a 3.0 mm × 38 mm everolimus-eluting stent (EES) (PROMUS Element™, Boston Scientific, Natick, MA, USA) from the LMT to the proximal LAD lesion, crossing over the LCx, at 12 atmospheres to avoid the restenosis of the edge of the stent (Fig. 1B). The images from the cross-sectional OCT (Fig. 2A) and instant reconstruction 3D OCT (Fig. 2D) demonstrated the sufficient expansion from the LMT to LAD, crossing over the ostium of LCx entirely, and good apposition of the stent struts. Good apposition to the vessel wall of the stent struts opposite the LCx was also demonstrated, suggesting that there were no findings of stent malapposition. Then, a guidewire was advanced into the LCx through the jailing struts of the ostium of the LCx, but the recrossing position was unclear in this case. After inflating a 2.75 mm × 12 mm balloon catheter at 12 atmospheres in the jailing struts of the LCx, the well opened jailing struts of the LCx were confirmed with a cross-sectional OCT. However, a new development of stent malapposition was confirmed opposite the LCx ostium by a cross-sectional OCT and instant reconstruction 3D OCT (Fig. 2B, arrows and E, arrow head). Thus, a KBI with a 2.75 mm × 12 mm balloon catheter for the LCx and a 3.0 mm × 12 mm balloon catheter for the LAD was inflated at 8 atmospheres. Finally, the cross-sectional OCT (Fig. 2C) and instant reconstruction 3D OCT (Fig. 2F) imaging after the KBI could clearly demonstrate the adequate expansion of the proximal portion of the stent and the disappearance of the stent malapposition. After this session, we also performed a bench test replicating the clinical situation with a phantom coronary bifurcation model and macroscopic images to evaluate this phenomenon in vivo. The cross-over stenting to the main branch was performed with a 3.0 mm × 32 mm EES in the coronary bifurcation model (Fig. 2G and I). The inflation of the jailing stent struts by a 2.75 mm × 15 mm balloon catheter for a side branch caused a deformation at the vessel wall opposite the side branch (Fig. 2H, arrow head, and K, arrow head). We could confirm that the stent deformation was precisely corrected by the following KBI with a 2.75 mm × 15 mm balloon catheter for the side branch and a 3.0 mm × 15 mm balloon catheter for the main branch for the bifurcation lesions (Fig. 2I and L). These in vitro findings (Fig. 2G–L) were consistent with those in vivo (Fig. 2A–F), respectively. He had no restenosis during the CAG, which was performed 6 months after the PCI, and has remained well without any symptoms thereafter.
Fig. 1.
The coronary angiogram (CAG) before the procedure (A), after the stent implantation from the left main trunk (LMT) to the left anterior descending (LAD) artery across the left circumflex (LCx) artery without contrast (B), the two-way arrow indicates the implanted stent site and with contrast (C), after the balloon inflation for the ostium of the LCx (D), and after a kissing-balloon inflation (KBI) for the LAD and LCx (E). The CAG revealed a 90% luminal diameter stenosis at the proximal lesion of the LAD (A, arrow), and the stent distortion after the balloon inflation for the ostium of the LCx (D, arrow head).
Fig. 2.
The findings of the cross-sectional optical coherence tomography (OCT) (A–C), three-dimensional (3D) OCT (D–F), bench test in the phantom coronary arterial bifurcation model (G–I), and macroscopic images of the stent (J–L). The images of the cross-sectional OCT and 3D OCT demonstrated a sufficient expansion and well apposition of the stent struts (A) without any stent abnormalities (D). After inflating the balloon catheter in the jailing struts of the left circumflex (LCx) artery, the well opened jailing struts of the LCx were confirmed with a coronary angiogram (CAG). However, a new development of a stent malapposition was confirmed opposite the LCx ostium during the cross-sectional OCT (B, arrows) and 3D OCT (E, arrow head). This shows the adequate expansion of the proximal portion of the stent and disappearance of the stent malapposition after the kissing-balloon inflation (KBI) with balloon catheters for the LCx and left anterior descending artery (LAD) (C and F). This shows the images of the bench test in a phantom model and macroscopic images of the stent exhibiting the same results of A and D as G and J, B and E as H and K, and C and F as I and L, respectively. LMT, left main trunk.
Discussion
The new-generation DESs have significantly reduced the development of restenosis and stent thrombosis, and additionally lowered risk of death [1]. However, the rates of restenosis and stent thrombosis after the therapeutic stent deployment for bifurcation lesions are still comparably high. Previous clinical studies have shown that treatment with two stents for bifurcation lesions causes higher rates of procedure-related myocardial infarction without any significant differences in major adverse cardiac events (MACE), compared with treatment with single stents [6]. On the other hand, the KBI after the stent deployment for bifurcation lesions may yield clinical benefits [4], [5], including (1) the full expansion of the stent struts at the ostium of the side branch for a reduction in side branch restenosis, (2) the precise correction of the stent deformation and/or distortion at the vessel wall opposite the side branch [7], and (3) the adequate expansion of the main vessel and side branch to the appropriate size. However, the strategies for those lesions are not well established [3], [4], [5] even in the new-generation DES era.
Herein, we experienced a case of a successful PCI with a single stent deployment to the bifurcation lesion from the LMT to the LAD crossing the LCx followed by a KBI for the LAD and LCx using cross-sectional OCT and 3D OCT. 3D OCT reconstructed by the automatic detection of lumen-vessel border can help to visualize the deformation of vessel or stent. Although cross-sectional OCT imaging after inflating a balloon catheter in the jailing struts of the LCx could demonstrate that the adequate opening of the jailing struts of the LCx, a new development of stent malapposition was confirmed opposite the LCx ostium by a cross-sectional OCT and instant reconstruction 3D OCT (Fig. 2B, arrows, and E, arrow head). These stent abnormalities, which may cause a high rate of restenosis and stent thrombosis contributing to a higher risk of death [7], were easily corrected by a subsequent KBI of the LAD and LCx using both cross-sectional OCT (Fig. 2C) and instant reconstruction 3D OCT (Fig. 2F) imaging. Recent clinical trials have demonstrated that the optimal rewiring of the side branches during bifurcation stenting is important for favorable stent positioning leading to reduction in stent malapposition after KBI [8]. Furthermore, the asymmetrical dilation during bifurcation stenting after KBI has been also reported [9], [10]. However, the cross-sectional OCT and instant reconstruction 3D OCT imaging can easily confirm these abnormalities independent of rewiring position. The bifurcation stenting has many problems which are affected by a wide range of factors such as lesion morphology defined by Medina bifurcation classification [2], target vessel's reference diameter, the bifurcation angle, the design of the stents, and the strategy of stent implantation. Thus, cross-sectional OCT and instant reconstruction 3D OCT imaging could visually demonstrate more easily the anatomical morphology, and may be one of the helpful and useful intravascular imaging modalities for a PCI to bifurcation lesions.
Next, to confirm these findings, we performed a similar procedure with a phantom bench test and macroscopic images of stent in vitro (Fig. 2G–L). Those in vivo findings, including the CAG and instant reconstruction 3D OCT images, were the same findings as those of the experiments from an in vitro phantom coronary bifurcation model and macroscopic images of stent (Fig. 2G–L). Recent studies using this model in vitro and using intravascular ultrasound (IVUS) described the distortion of the main vessel stent after a side branch inflation was successfully corrected by a following KBI [9], [10], supporting our in vivo results.
To the best of our knowledge, there have been no reports on both 3D OCT in vivo images, and a phantom coronary bifurcation model, and the macroscopic images of a stent in vitro demonstrating a stent malapposition, which was steadily corrected through following final KBI of the bifurcation lesion. These stent malappositions may be one of the important mechanisms of the restenosis of bifurcation lesions even in the new-generation DES era. Thus, the present case report may encourage the use of one of the effective and useful therapeutic strategies of PCI for bifurcation lesions.
In conclusion, the 3D OCT imaging and a following KBI after the stent deployment for bifurcation lesions may be one of the most effective and therapeutic strategies for the PCI of bifurcation stenting. Because the present study is a single case report and the follow-up period was only 6 months, the long-term clinical benefits could not be determined. Supporting data from large clinical trials, however, are needed for such conclusions to be made.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Sarno G., Laqerqvist B., Frobert O., Nisson J., Olivecrona G., Omerovic E., Saleh N., Venetzanos D., James S. Lower risk of stent thrombosis and restenosis with unrestricted use of ‘new-generation’ drug-eluting stents: a report from the nationwide Swedish Coronary Angiography and Angioplasty Registry (SCAAR) Eur Heart J. 2012;33:606–613. doi: 10.1093/eurheartj/ehr479. [DOI] [PubMed] [Google Scholar]
- 2.Medina A., Su’arez de Lezo J., Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006;59:183–184. [PubMed] [Google Scholar]
- 3.Yamawaki M., Muramatsu T., Kozuma K., Ito Y., Kawaguchi R., Kotani J., Yokoi H., Nakamura M., Saito S. Long-term clinical outcome of a single stent approach with and without a final kissing balloon technique for coronary bifurcation – subanalysis of the TAXUS Japan postmarket surveillance study. Circ J. 2014;78:110–121. doi: 10.1253/circj.cj-13-0346. [DOI] [PubMed] [Google Scholar]
- 4.Niemela M., Kervinen K., Erglis A., Holm N.R., Maeng M., Christiansen E.H., Kumsars I., Jegere S., Dombrovskis A., Gunnes P., Stavnes S., Steigen T.K., Trovik T., Eskola M., Vikman S. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic bifurcation study III. Circulation. 2011;123:79–86. doi: 10.1161/CIRCULATIONAHA.110.966879. [DOI] [PubMed] [Google Scholar]
- 5.Hariki H., Shinke T., Otake H., Shite J., Nakagawa M., Inoue T., Osue T., Iwasaki M., Taniguchi Y., Nishio R., Hiranuma N., Kinutani H., Konishi A., Hirata K. Potential benefit of final kissing balloon inflation after single stenting for the treatment of bifurcation lesions – insights from the treatment of bifurcation lesions. Circ J. 2013;77:1193–1201. doi: 10.1253/circj.cj-12-0848. [DOI] [PubMed] [Google Scholar]
- 6.Steigen T.K., Maeng M., Wiseth R., Erglis A., Kumsars I., Narbute I., Gunnes P., Mannsverk J., Meyerdierks O., Rotevatn S., Niemela M., Kervinen K., Jensen J.S., Galloe A., Nikus K. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions. Circulation. 2006;114:1955–1961. doi: 10.1161/CIRCULATIONAHA.106.664920. [DOI] [PubMed] [Google Scholar]
- 7.Attizzani G.F., Capodanno D., Ohno Y., Tamburino C. Mechanisms, pathophysiology, and clinical aspects of incomplete stent apposition. J Am Coll Cardiol. 2014;63:1355–1367. doi: 10.1016/j.jacc.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Okamura T., Onuma Y., Yamada J., Iqbal J., Tateishi H., Nao T., Oda T., Maeda T., Nakamura T., Miura T., Yano M., Serruys P.W. 3D optical coherence tomography: new insights into the process of optical rewiring of side branches during bifurcational stenting. EuroIntervention. 2014;10:907–915. doi: 10.4244/EIJV10I8A157. [DOI] [PubMed] [Google Scholar]
- 9.Foin N., Secco G.G., Ghilencea L., Krams R., Di Mario C. Final proximal post-dilation is necessary after kissing balloon in bifurcation stenting. EuroIntervention. 2011;7:597–604. doi: 10.4244/EIJV7I5A96. [DOI] [PubMed] [Google Scholar]
- 10.Rahman S., Leesar T., Cilingiroglu M., Effat M., Arif I., Helmy T., Leesar M.A. Impact of kissing balloon inflation on the main vessel stent volume, area, and symmetry after side-branch dilation in patients with coronary bifurcation lesions. JACC Cardiovasc Interv. 2013;6:923–931. doi: 10.1016/j.jcin.2013.04.019. [DOI] [PubMed] [Google Scholar]