Abstract
Right ventricular (RV) intramyocardial hematoma is a potentially life-threatening condition that can complicate percutaneous coronary intervention (PCI). Natural course of RV hematoma and long-term recovery of the affected myocardium have not been described. We present a case of a 70-year-old male with large RV hematoma caused by distal guidewire perforation during PCI of the right coronary artery. Baseline multimodality imaging, serial echocardiography, and long-term follow-up using cardiac magnetic resonance (CMR) imaging were used to investigate the natural course of this rare condition. Despite its massive initial appearance, the hematoma was successfully managed conservatively. Serial echocardiographic examination showed slow gradual resorption of the hematoma. Follow-up CMR performed at 12 months was strikingly normal, showing no late gadolinium enhancement of the RV myocardium indicating lack of significant fibrotic scarring at the site of hematoma resorption.
<Learning objective: Right ventricular (RV) free wall hematoma is a potentially life-threatening complication of percutaneous coronary intervention. Multimodality imaging combined with serial echocardiography is useful to study the extent of myocardial involvement and the slow resorption process of the hematoma. This case illustrates that even a sizeable RV intramyocardial hematoma can be managed conservatively if no acute hemodynamic compromise occurs and complete recovery of the myocardium can be expected.>
Keywords: Complications, Percutaneous coronary intervention, Cardiac magnetic resonance imaging, Transthoracic echocardiography
Introduction
Development of right ventricular (RV) intramyocardial hematoma is a rare complication of percutaneous coronary intervention (PCI) of the right coronary artery (RCA). It is primarily associated with balloon- or guidewire-induced perforation of the coronary artery. In some cases, the hematoma resolves spontaneously without sequelae [1], but it can result in acute pseudo-pericardial tamponade [2]. The long-term recovery of affected RV myocardium is not known. We describe a large RV hematoma as a complication of PCI in a patient with previous coronary artery bypass grafting (CABG). We show baseline multimodality imaging of the hematoma and the in-hospital course of the patient. Most interestingly, we also describe the natural history of intramyocardial hematoma resorption using serial echocardiography in addition to cardiac magnetic resonance (CMR) imaging at 1-year follow-up.
Case report
Our case is a 70-year-old man with a history of type 2 diabetes, hypertension, and hypercholesterolemia. His cardiovascular history included PCI of RCA with two bare metal stents 9 years previously and CABG 8 years previously. He was evaluated for Canadian Cardiovascular Society class III stable angina pectoris and a positive stress test while on maximal antianginal medication. His left ventricular function was normal with ejection fraction of 60% and no valvular dysfunction. HAS-BLED score was 3.
Elective coronary angiography showed patent grafts to left anterior descending coronary artery and left obtuse marginal. RCA, which had not been bypassed, had a short subtotal occlusion inside previously implanted stents at 2 cm from the ostium (Fig. 1A). There was a reduced thrombolysis in myocardial infarction (TIMI) 2 flow and ad hoc PCI of RCA was decided. The antithrombotic regimen prior to angiography included aspirin 100 mg once daily and the patient was given 600 mg clopidogrel and enoxaparin 0.8 mg/kg intravenously. After passing the tight lesion with a Pilot 50™ guidewire (Abbott Vascular, Abbott Park, IL, USA), balloons could be passed only after numerous attempts using a guide extension catheter (Guideliner™, Vascular Solutions, Maple Grove, MN, USA). Dilatations were then performed with 1.0 mm × 14 mm and 1.5 mm × 10 mm compliant balloons. Immediately following this, extraluminal contrast staining of the aortic root at RCA ostium (Fig. 1B) was observed. To stabilize the local aortic dissection, a 3.0 mm × 12 mm drug-eluting stent (Resolute Integrity™, Medtronic, Dublin, Ireland) was deployed at RCA ostium. While this stabilized the dissection, delivery of a second stent more distally to the original culprit lesion was not successful. Since the flow was normal (TIMI3), and the patient was asymptomatic, the procedure was ended with the intention to finalize in another session after a few weeks. Immediate transthoracic and transesophageal echocardiography showed no visible aortic root dissection or hematoma. Myocardium and pericardium were normal. At this time, the patient was asymptomatic and was transferred to the coronary care unit (CCU) for overnight observation.
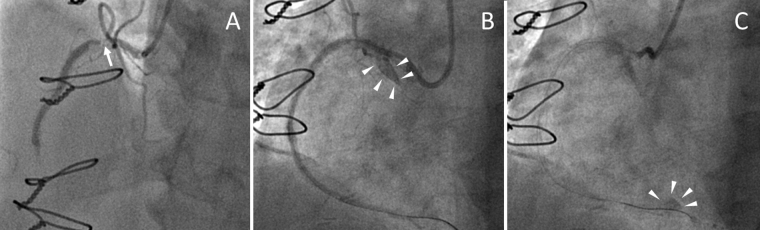
Fig. 1.
Angiographic findings. (A) Proximal right coronary artery (RCA) subtotal occlusion (arrow) prior to percutaneous coronary intervention (PCI). (B) Angiography during PCI. Extravasation of contrast (arrowheads) indicating a local aortic root dissection. (C) Extravasation of small amount of contrast (arrowheads) indicating perforation in distal RCA.
During post-procedural observation at CCU 10 h after the procedure, the patient experienced sudden-onset chest pain, worsened by deep inspiration. Blood pressure was stable at 122/64 mmHg and heart rate was at 85 bpm. Electrocardiogram was normal and following a small dose of analgesic the patient was asymptomatic. Next morning the patient was doing well, but a considerable troponin T elevation of 1700 ng/L was observed. Transthoracic echocardiography unexpectedly showed a sizeable ellipsoid-shaped mass measuring 4 cm × 5 cm located in basolateral RV wall (Fig. 2A and B). By careful examination of the angiographic images afterward, a small distal contrast leak indicating a perforation of a small side branch of distal RCA was spotted (Fig. 1C). The patient's hemodynamic status was stable during the hospitalization and he experienced only a mild feeling of fullness in the chest. C-reactive protein reached a maximum of 103 mg/L at the third post-procedural day, without signs of a bacterial infection. There was also mild leukocytosis of 13.5 × 109/L and a hemoglobin drop of 127–100 g/L. Cardiac computed tomography (CT) performed on the first post-procedural day showed an egg-shaped hematoma in RV basal wall measuring 7.4 cm × 4.2 cm × 4.6 cm (Fig. 2C). No low molecular weight heparin was given post-procedure, but the patient was maintained on dual antiplatelet therapy because of the recent stent implantation. CMR imaging on the fifth day after PCI documented an intramyocardial hematoma measuring 7.3 cm × 3.8 cm × 3.7 cm (Fig. 3A and B) without any other significant findings. The patient was discharged on the seventh post-procedural day. Dual antiplatelet therapy was prescribed for 12 months.
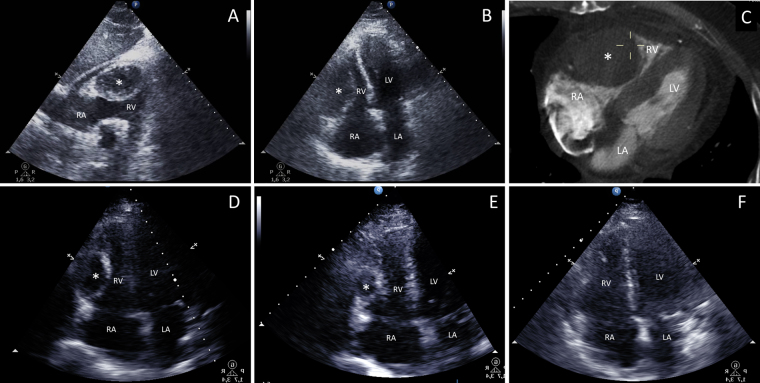
Fig. 2.
The evolution of hematoma resorption. (A) Subcostal and (B) apical echocardiographic views and (C) computed tomography image on the first post-procedural day showing the large intramyocardial hematoma (*) in right ventricular (RV) free wall. (D) At 1 month and (E) at 4 months the hematoma (*) had reduced in size. (F) At 12 months, RV had returned to its normal appearance. RA, right atrium; LA, left atrium; LV, left ventricle.
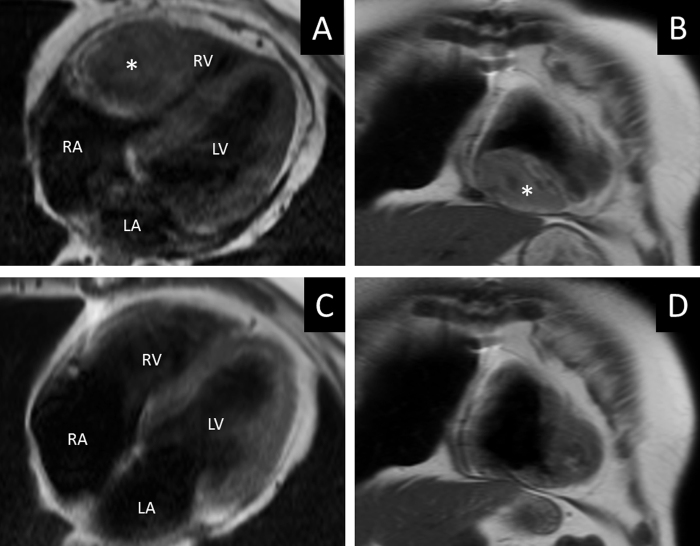
Fig. 3.
Cardiac magnetic resonance imaging of hematoma resorption. (A) Axial 4-chamber view and (B) coronal view at baseline. (C) Axial 4-chamber view and (D) coronal view at 12 months. (*) Hematoma. RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
At 1-month outpatient follow-up visit the patient reported occasional feelings of fullness in the thoracic region unrelated to exercise. The hematoma was still clearly visible, measuring 3.6 cm × 2.8 cm (Fig. 2D). No pericardial effusion was observed and the right and left ventricular contraction was normal. At 4 months, the remnant hematoma was still visible, but reduced in size measuring 1.5 cm × 2.5 cm by echocardiography (Fig. 2E). The patient was asymptomatic; the original anginal symptoms had also been relieved. At the final follow-up visit at 12 months, echocardiographic findings were normal (Fig. 2F) with normal left and right ventricular function. A follow-up CMR at 12 months showed complete disappearance of the hematoma (Fig. 3C and D). CMR imaging showed no late gadolinium enhancement in the RV myocardium.
Discussion
We report here the natural course of RV free wall intramyocardial hematoma, a rare complication, which was caused by wire perforation of a distal side branch during a challenging PCI procedure. The intraprocedural local aortic root dissection had no anatomic connection to the RV hematoma and was an incidental occurrence caused by the forceful use of an extra back-up guide with an extension catheter. Despite its large size, resorption of the hematoma was complete and no evidence of myocardial scarring was found in long-term follow-up CMR imaging. This was unanticipated considering the marked post-procedural troponin elevation due to compression of the RV myocardium.
The therapeutic measures in each case of RV hematoma depend on the acute hemodynamic consequences of the RV inflow or outflow tract obstruction. Immediate echocardiography is the fastest modality to diagnose this life-threatening condition. Both cardiac CT and CMR imaging yield useful information on the extent of hematoma. Once the patient develops hemodynamic instability, emergent surgical intervention may be needed to rescue the pseudo-pericardial tamponade [2]. In our case, the hematoma fortunately caused no hemodynamic disturbance despite its massive appearance in multimodality imaging and was successfully managed conservatively.
To conclude, in the present case a sizeable RV intramyocardial hematoma could be managed conservatively. Gradual resorption of the hematoma is a lengthy process, but complete recovery of the RV myocardium was observed.
Conflict of interest
O.A. Kajander has received lecture fees from St. Jude Medical.
References
- 1.Lee Y.W., Chun K.J., Park Y.H., Kim J.S., Kim J., Kim J.H., Lee S.G., Lee D.I., Kim J.H. Right ventricular wall hematoma secondary to percutaneous coronary intervention. J Cardiovasc Ultrasound. 2009;17:99–101. doi: 10.4250/jcu.2009.17.3.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steinwender C., Hofmann R., Leisch F. Pseudo-pericardial tamponade after perforation of the right coronary artery. Heart. 2004;90:e36. doi: 10.1136/hrt.2004.035378. [DOI] [PMC free article] [PubMed] [Google Scholar]