Introduction
Since the late 1980s non-invasive ventilatory support (NIV) has become a standard treatment in acute exacerbation of COPD (AECOPD) with hypercapnia.1 Although NIV has been shown to be extremely useful in this situation, but up to 30% of hypercapnic AECOPD patients do not tolerate NIV for several reasons.2
Nasal high-flow (NHF) provides a warmed and humidified airflow up to 60 Liter/min through a specialized nasal cannula. Oxygen admixture is readily available and should be dosed to a desired saturation.3 NHF combines a wash-out effect with a decrease in CO2 rebreathing, support of inspiratory flow, a small increase in airway pressure, a lowering of ambient air admixture during inspiration and possibly a beneficial effect of warmed and saturated air in the airways. Together, these effects lead to a stabilization of oxygen delivery at higher respiratory rates, a decrease in the work of breathing noticeable by a lower respiratory rate and reduced hypercapnia.4–6
Several studies evaluated the effectiveness of NHF therapy in a variety of clinical situations with effects comparable to NIV.3,7 Most of these investigations excluded patients with hypercapnia. It is therefore, impossible to draw meaningful conclusions on the effectiveness of NHF in AECOPD. Several smaller series have observed a significant decrease in partial arterialized carbon dioxide pressure of CO2 (paCO2) in chronic hypercapnic COPD patients.4,6 There are no data available about other endpoints or in a cohort of solely hypercapnic AECOPD patients.
Methods
Thirty-eight patients were treated between 2015 and 2017 at the Department of Respiratory Medicine, University hospital Leipzig, Germany. Patients were included if they a) did not tolerate NIV following a regular trial (intolerance of NIV), b) fulfilled AECOPD criteria (Anthonisen), c) had a decrease in pH (pH ≤7.38) and a capillary paCO2 >45 mmHg at admission, d) had absence of acute metabolic disorders, and e) did not fulfill criteria for intubation. Initiation of NHF (Softflow 50; TNI medical AG, Würzburg) was titrated to achieve a flow rate with greatest tolerability. Oxygen flow (as part of the total flow) was then adjusted to achieve baseline SpO2 values. Changes in partial pressures of oxygen (paO2) and paCO2 as well as pH in capillary blood gas analysis were monitored closely. NHF was terminated when pH increased to more than 7.38 or when the patient no longer tolerated the device or had lesser symptoms. Statistical analysis was performed using an ANOVA test (Sigma Plot; Systat Software GmbH, Ekrath, Germany). This study was approved by the University of Leipzig ethics committee (110/18-ek) and registered (NCT03523481). Patients provided written informed consent. The study was carried out in accordance with the principles of the Declaration of Helsinki.
Results
A significant treatment effect was seen in mean capillary blood pH and in mean paCO2 (Table 1, Figure 1). Greatest improvements in pH and paCO2 were found in 17 patients with baseline pH <7.35 (Table 1).
Table 1.
Parameters during NHF treatment
| Parameters | All patients (pH ≤7.38; n=38) | |||
|---|---|---|---|---|
| Baseline (mean±SD) | End (mean±SD) | Change (mean±SD) | P-value | |
| pH | 7.339±0.041 | 7.392±0.048 | 0.052±0.048 | 0.000 |
| pCO2 mmHg | 67.6±12.9 | 58.5±9.7 | −9.1±8.8 | 0.001 |
| pO2 mmHg | 58.3±15.2 | 58.3±17.6 | – | 0.983 |
| SO2 % | 85.3±9.5 | 86.2±11.3 | – | 0.798 |
| HCO3 mmol/L | 30.8±5.1 | 31.6±5.3 | – | 0.636 |
| Base excess mmol/L | 6.9±4.9 | 7.7±5.4 | – | 0.633 |
| NHF flow L/min | – | 25.8±8.2 | – | – |
| Treatment time min | – | 195±231 | – | – |
| Patients with pH <7.35 (n=17) | ||||
| pH | 7.298±0.046 | 7.379±0.051 | 0.082±0.060 | 0.000 |
| pCO2 mmHg | 73.7±13.7 | 59.6±11.2 | −14.2±10.6 | 0.002 |
| pO2 mmHg | 56.9±14.8 | 55.6±20.7 | – | 0.845 |
| SO2 % | 84.8±10.1 | 84.3±11.9 | – | 0.904 |
| HCO3 mmol/L | 31.6±5.5 | 32.5±5.6 | – | 0.661 |
| Base excess mmol/L | 7.4±5.3 | 8.5±5.7 | – | 0.591 |
| NHF flow L/min | – | 26.3±7.9 | – | – |
| Treatment time min | – | 252±251 | – | – |
Notes: Changes in blood gas analyses data, usage time and flow rates during NHF therapy in all patients and in the subgroup with pH <7.35. All data are organized as mean±SD. “–” indicates no significant differences to report.
Abbreviation: NHF, nasal high-flow.
Figure 1.
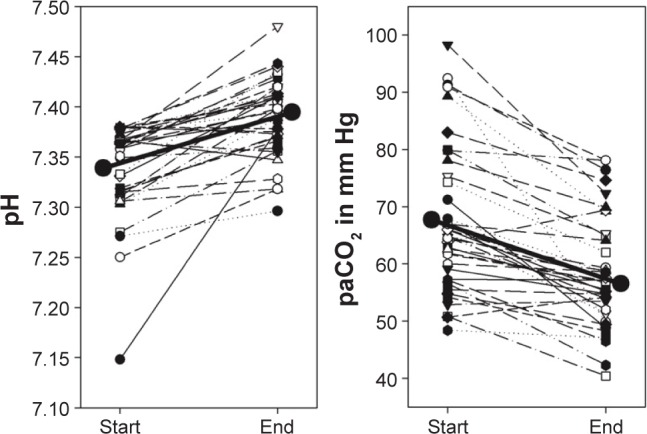
Changes in pH and paCO2 in all patients; the bold line marks mean values; P<0.05.
Conclusion and limitation
To our knowledge, this is the first observation evaluating NHF in a cohort with solely hypercapnic (partly acidotic) AECOPD patients. We found significant improvements of pH and paCO2. Our study demonstrates that using NHF in severe-to-moderate acidotic and non-acidotic hypercapnic AECOPD patients who did not tolerate NIV is useful.
The limitation of this investigation is best described by its retrospective nature with the lack of a control group. The number of patients was low but appears to be sufficient for a first answer as to whether NHF may be useful in hypercapnic AECOPD patients.
Footnotes
Disclosure
The authors report travel grants, non-financial support (equipment), and lecture fees from TNI medical AG and report no other conflicts of interest in this work.
References
- 1.Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 2.Confalonieri M, Garuti G, Cattaruzza MS, et al. A chart of failure risk for noninvasive ventilation in patients with COPD exacerbation. Eur Respir J. 2005;25(2):348–355. doi: 10.1183/09031936.05.00085304. [DOI] [PubMed] [Google Scholar]
- 3.Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 4.Bräunlich J, Köhler M, Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1077–1085. doi: 10.2147/COPD.S104616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bräunlich J, Mauersberger F, Wirtz H. Effectiveness of nasal highflow in hypercapnic COPD patients is flow and leakage dependent. BMC Pulm Med. 2018;18(1):14. doi: 10.1186/s12890-018-0576-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bräunlich J, Seyfarth HJ, Wirtz H. Nasal High-flow versus non-invasive ventilation in stable hypercapnic COPD: a preliminary report. Multidiscip Respir Med. 2015;10(1):27. doi: 10.1186/s40248-015-0019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hernández G, Vaquero C, Colinas L, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316(15):1565–1574. doi: 10.1001/jama.2016.14194. [DOI] [PubMed] [Google Scholar]


