Abstract
Across the lifespan, attention deficit/hyperactivity disorder (ADHD) is associated with increased health risk behaviors including substance abuse, binge eating and obesity, and unsafe sexual behavior. These risks are directly linked to the neurocognitive deficits associated with ADHD, and are also mediated by the cascade of psychosocial impairments and stressors caused by ADHD across development. However, little is known about optimal approaches to improve health outcomes in this high-risk population. This topical review provides an overview of health risks associated with ADHD and the limited existing research relevant to health promotion for children and adolescents with ADHD. Future research questions and implications for clinicians are also addressed—especially how psychologists and medical practitioners may improve child health through early screenings, increasing medication adherence, and treating psychosocial impairments.
Keywords: attention, hyperactivity, and ADHD; health behavior; health promotion and prevention
Attention deficit/hyperactivity disorder (ADHD) is a neurocognitive disorder affecting 5–10% of children and conferring risk for numerous long-term health problems. Beginning in childhood and adolescence, ADHD is associated with risk behaviors that contribute to chronic health problems, including substance use, binge eating and obesity, and risky sexual behavior. Thus, young people with ADHD have twice the health care costs of those without that disorder ( Leibson, Katusic, Barbaresi, Ransom, & O’Brien, 2001 ), and ADHD is associated with a marked increase in morbidity and mortality rates for children and adults ( Dalsgaard, Ostergaard, Leckman, Mortensen, & Pedersen, 2015 ). Despite these known risks, few studies have investigated methods of improving health behavior for individuals with ADHD, and most ADHD treatment studies have not examined effects on health behaviors.
The purpose of this topical review is to (a) provide a brief overview of the health risks associated with ADHD and underlying mechanisms; (b) identify unanswered questions related to improving this population’s health, and (c) explore the implications of these risks for pediatric psychologists and medical practitioners and propose initial steps toward health promotion. Though an association between certain health risks and ADHD has been noted previously in the literature ( Barkley, 2002 ), we are unaware of prior reviews exploring mechanisms underlying multiple risks or offering implications for health promotion and prevention.
Health Risk Behaviors and ADHD
Individuals with ADHD have at least 1.5 times the average risk of developing dependence on nicotine, alcohol, marijuana, cocaine, and other drugs ( Lee, Humphreys, Flory, Liu, & Glass, 2011 ), and tend to have earlier onset, faster progression, and less remittance of substance use disorders (SUDs) ( Fuemmeler, Kollins, & McClernon, 2007 ; Molina & Pelham, 2003 ). They also have higher rates of obesity ( Spencer, Faraone, Tarko, McDermott, & Biederman, 2014 ) and three times higher rates of binge eating than individuals without ADHD ( Bleck & DeBate, 2013 ). Furthermore, ADHD is associated with unsafe sexual behavior, including earlier sexual activity and more partners ( Brown et al., 2010 ; Flory, Molina, Pelham, Gnagy, & Smith, 2006 ). ADHD youth are also less likely to use contraception, leading to higher rates of sexually transmitted infections (STIs) and unintended pregnancies ( Flory et al., 2006 ).
SUDs, obesity, and STIs are directly associated with chronic health problems as well as morbidity and mortality. SUDs also increase rates of violence, accidents, and unprotected sex. These difficulties, along with unintended pregnancies, additionally reduce socioeconomic attainment and quality of life. In light of the high prevalence of ADHD and associated risks, health promotion efforts for this population are much needed and have the potential for substantial public health impact.
Mechanisms of Risk
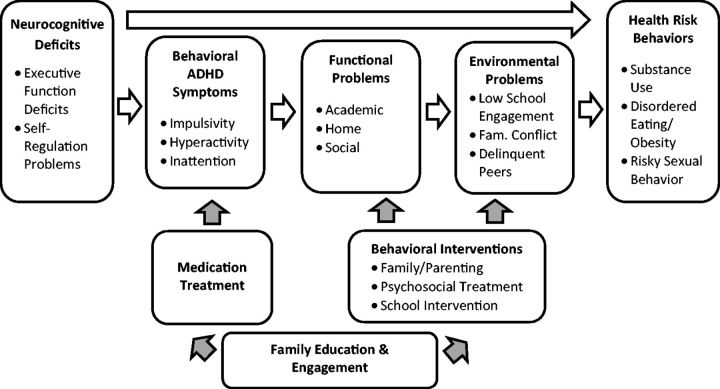
Health promotion approaches should be informed by an understanding of the mechanisms underlying the association between ADHD and health risk behaviors. ADHD may affect health risk behaviors both directly as the result of associated neurocognitive impairments, and indirectly through social-environmental problems that result from ADHD (see Figure 1 ).
Figure 1.
Biopsychosocial model of ADHD and health risk behaviors.
ADHD is characterized by deficits in executive functions (EF), which include the ability to solve problems, self-regulate, and inhibit impulses to address goals ( Pennington & Ozonoff, 1996 ). EF deficits underlie two clusters of behavioral ADHD symptoms—inattentive symptoms (i.e., disorganization, distractibility, etc.) and hyperactive-impulsive symptoms (i.e., high energy, interrupting)—that are both linked to health risk behaviors, independent of ADHD diagnosis ( Fuemmeler et al., 2007 ; Molina & Pelham, 2003 ). Impulsivity is central to many risk-taking behaviors and is directly associated with substance use, binge eating, and overweight status ( Davis, Levitan, Smith, Tweed, & Curtis, 2006 ; Dawe & Loxton, 2004 ). Hyperactive-impulsive symptoms also appear to be key in the development of addiction; for example, they are associated with nearly double the likelihood of progressing from no smoking to regular smoking in adolescence ( Fuemmeler et al., 2007 ). Inattentive symptoms, which result from EF deficits including working memory and sustained attention, also interfere with monitoring internal states and regulating behavior and are linked to multiple substance use outcomes ( Molina & Pelham, 2003 ) and irregular eating ( Davis et al., 2006 ).
Additionally, ADHD-related impairment contributes to environmental stressors that increase the likelihood of risky behavior. ADHD frequently impairs academic functioning, which in turn increases the risk of adolescent substance use ( Molina et al., 2012 ). Parenting a child with ADHD also places high demands on caregivers and increases family stress and conflict. Parent–child relational problems are related to risky sexual behavior ( Guilamo-Ramos et al., 2012 ), eating pathology ( Mikami, Hinshaw, Patterson, & Lee, 2008 ), and substance use for ADHD adolescents specifically ( Molina, Marshal, Pelham, & Wirth, 2005 ; Walther et al., 2012 ). Low engagement in school and positive activities, combined with decreased parental involvement, can increase exposure to negative peer groups and risky situations. Indeed, peers have a greater influence on substance use for youth with ADHD ( Marshal, Molina, & Pelham, 2003 ; Walther et al., 2012 ).
These two pathways by which ADHD influences health risks—through neurocognitive deficits and increased environmental adversity—highlight potential targets for prevention and health promotion. Treating ADHD symptoms and executive dysfunction, for example with stimulant medication, may thereby help to reduce ensuing risk behaviors. Alternatively, strengthening social and environmental factors associated with resilience, such as academic engagement and effective parenting, may also promote healthy behavior.
What We Do Not Know: Directions for Research on ADHD Health Promotion
Almost no existing studies have evaluated specific strategies to address health risk behaviors for ADHD individuals. Several key unanswered questions could help meaningfully guide further research in this area.
Does Treating ADHD Improve Health Behaviors?
Surprisingly few studies have examined the impact of ADHD treatment specifically on health risk behaviors. The only randomized trial to do so is the Multimodal Treatment Study of ADHD, which found no significant effects of either medication or behavioral treatment on later SUD diagnosis or disordered eating ( Mikami et al., 2010 ; Molina et al., 2013 ). A meta-anaysis of naturalistic studies found nonsignificant associations between stimulant treatment and SUDs ( Humphries, Eng, & Lee, 2013 ), although another meta-analysis identified a protective effect of stimulants on later cigarette smoking, especially when medication treatment was administered consistently over time ( Schoenfelder, Faraone, & Kollins, 2014 ). With regard to obesity, stimulant medication has been found to improve eating habits in adults with ADHD ( Levy, Fleming, & Klar, 2009 ), and a stimulant product (Vyvanse) was also recently Food and Drug Administration approved for treatment of binge-eating disorder ( Food and Drug Administration, 2015 ). We are unaware of studies of stimulant treatment effects on disordered eating in youth. Health outcome measures should be systematically included in ADHD treatment studies to determine whether treating ADHD mitigates health risks, or whether additional approaches are needed.
Are Existing Health Promotion Programs Effective for ADHD Youth?
Health promotion programs can use an approach that is universal (targeting entire populations), selected (targeting individuals with environmentally-based risks), or indicated (targeting individuals with person-level risk-factors, such as ADHD). We are unaware of indicated prevention or health promotion programs specifically designed for ADHD youth. Presumably, these youth participate in existing universal and selected interventions, but ADHD has not been examined as a moderator of these program outcomes. Selected programs for youth in poverty yield promising results to reduce delinquency, substance abuse, and pregnancy ( Hawkins, Catalano, Kosterman, Abbott, & Hill, 1999 ). Programs to improve parenting and family functioning also reduce substance use risk ( Stormshak & Dishion, 2009 ) and treat childhood obesity ( Epstein, Valoski, Wing, & McCurley, 1990 ). Moving forward, researchers who evaluate the efficacy of such programs should examine differential outcomes for ADHD youth and assess the need for program adaptations to engage this population.
When Should We Intervene?
Disordered eating may be identified in childhood; substance use and sexual risk behaviors generally emerge in adolescence. High-risk youth may be identified on the basis of ADHD diagnosis, but genetic, neurobiological, or behavioral risk markers may be evident even before full ADHD diagnostic criteria are met. Further research is needed to determine optimal targeting and timing of screening efforts, and given the high prevalence of ADHD, additional markers of high-risk status, such as symptom severity or oppositional defiant disorder ( Molina & Pelham, 2003 ).
What We Do Know: Implications for Clinicians
Psychologists, physicians, and other clinicians in medical settings are well situated to identify children at risk for chronic health problems and implement strategies to promote health. In light of the paucity of knowledge on strategies to reduce health risks for ADHD youth and lack of clinical recommendations on this topic, we offer guidelines to professionals working with this population based on the extant literature (see Table I ).
Table I.
Preventing Health Risks for ADHD Youth: Implications for Clinicians
| Route to health promotion | Strategies for clinicians |
|---|---|
| Early screening |
|
| Treatment adherence |
|
| Strengthen environmental and social contexts |
|
| Early intervention and treatment |
|
| Future research |
|
Early Screening Guides Early Intervention
Three potential screening methods may help identify children at especially high risk of health problems associated with ADHD and connect them to early intervention. First, children with ADHD should be systematically monitored for emerging health risk behaviors through screening incorporated into routine medical appointments. Second, children who have not yet met full criteria for a diagnosis of ADHD (e.g., owing to lack of functional impairment) are still at risk for health problems resulting from poor self-regulation and impulsivity. Parents of children with elevated ADHD symptoms or a family history of ADHD will benefit from psychoeducation to increase awareness and monitoring of potential risks. Third, encouraging a diagnostic evaluation for children exhibiting ADHD symptoms may provide a platform for educating parents to recognize the risks and find resources. A thorough evaluation including comprehensive history, clinical interviewing, and standardized rating scales (in addition to brief screeners such as the Vanderbilt ADHD Diagnostic Parent Rating Scale) can rule out alternative causes of symptoms, facilitate access to appropriate treatment, and start a conversation with families about associated health risk behaviors.
Promote ADHD Treatment Adherence
Consistent stimulant medication treatment appears to be a promising component of health promotion for ADHD. Long-term benefits of stimulant treatment are greater when treatment is optimized and consistent, including protective effects against cigarette smoking ( Schoenfelder et al., 2014 ) and potential reduced substance use ( Zaso, Park, & Antshel, 2015 ). However, stimulants are often taken inconsistently, and discontinuation may reach as high as 95% between early adolescence and young adulthood ( McCarthy et al., 2009 ). Psychologists may be the first to hear about nonadherence and can explore barriers and facilitate communication with prescribing physicians. Additionally, adolescents are found to have more resistant attitudes toward medication than their parents ( Bussing, Zima, Mason, Porter, & Garvan, 2011 ). Clinicians may encourage teens’ active involvement in their medication management to promote continued treatment into adulthood.
Strengthen Social–Environmental Protective Factors
Given the strong association between risky behavior and ADHD-related functional problems, psychosocial intervention to improve academic, social, and family functioning may ultimately promote health. For example, clinicians can facilitate access to academic accommodations and improve homework routines. Behavioral parent training is part of comprehensive ADHD treatment, and parents will require additional support and an updated treatment plan as their children enter the highest risk years in adolescence. Additionally, exercise is found to mitigate ADHD symptoms ( Gapin, Labban, & Etnier, 2011 ). Clinician encouragement of physical activity may have far-reaching effects to improve both ADHD symptoms and cardiovascular health.
Conclusion
Individuals with ADHD are at heightened risk for behaviors that interfere with their long-term health. Consistent treatment of ADHD symptoms and promotion of academic, home, and social functioning may mitigate this risk. Unanswered questions remain as to when and how to optimally intervene to improve health outcomes for this population. Clinicians in medical settings are uniquely poised to detect emerging risks and promote resilience in this population through consistent screening, increasing treatment engagement, and strengthening psychosocial functioning.
Funding
This work was supported in part by K24DA023464 (Dr Kollins).
References
- Barkley R. A. ( 2002. ). Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder . The Journal of Clinical Psychiatry , 63 ( Suppl 12 ), 10 – 15 . [PubMed] [Google Scholar]
- Bleck J., DeBate R. D. ( 2013. ). Exploring the co-morbidity of attention-deficit/hyperactivity disorder with eating disorders and disordered eating behaviors in a nationally representative community-based sample . Eating Behaviors , 14 , 390 – 393 . doi:10.1016/j.eatbeh.2013.05.009 [doi] [DOI] [PubMed] [Google Scholar]
- Brown L. K., Hadley W., Stewart A., Lescano C., Whiteley L., Donenberg G., DiClemente R. ( 2010. ). Psychiatric disorders and sexual risk among adolescents in mental health treatment . Journal of Consulting and Clinical Psychology , 78 , 590 – 597 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R., Zima B. T., Mason D. M., Porter P. C., Garvan C. W. ( 2011. ). Receiving treatment for attention-deficit hyperactivity disorder: Do the perspectives of adolescents matter? The Journal of Adolescent Health , 49 , 7 – 14 . doi:10.1016/j.jadohealth.2010.08.014 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalsgaard S., Ostergaard S. D., Leckman J. F., Mortensen P. B., Pedersen M. G. ( 2015. ). Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study . Lancet , 385 , 2190 – 2196 . doi:10.1016/s0140‐6736(14)61684‐6 [DOI] [PubMed] [Google Scholar]
- Davis C., Levitan R. D., Smith M., Tweed S., Curtis C. ( 2006. ). Associations among overeating, overweight, and attention deficit/hyperactivity disorder: A structural equation modelling approach . Eating Behaviors , 7 , 266 – 274 . [DOI] [PubMed] [Google Scholar]
- Dawe S., Loxton N. J. ( 2004. ). The role of impulsivity in the development of substance use and eating disorders . Neuroscience and Biobehavioral Reviews , 28 , 343 – 351 . [DOI] [PubMed] [Google Scholar]
- Epstein L. H., Valoski A., Wing R. R., McCurley J. ( 1990. ). Ten-year follow-up of behavioral, family-based treatment for obese children . JAMA , 264 , 2519 – 2523 . [PubMed] [Google Scholar]
- Flory K., Molina B. S., Pelham W. E., Jr., Gnagy E., Smith B. ( 2006. ). Childhood ADHD predicts risky sexual behavior in young adulthood . Journal of Clinical Child and Adolescent Psychology , 35 , 571 – 577 . doi:10.1207/s15374424jccp3504_8 [doi] [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration, U. S. ( 2015. ). FDA expands uses of Vyvanse to treat binge-eating disorder. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm432543.htm (accessed July 16, 2015), Press Release. Retrieved from www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm432543.htm Retrieved July 16, 2015 .
- Fuemmeler B. F., Kollins S. H., McClernon F. J. ( 2007. ). Attention deficit hyperactivity disorder symptoms predict nicotine dependence and progression to regular smoking from adolescence to young adulthood . Journal of Pediatric Psychology , 32 , 1203 – 1213 . doi:jsm051 [pii] [DOI] [PubMed] [Google Scholar]
- Gapin J. I., Labban J. D., Etnier J. L. ( 2011. ). The effects of physical activity on attention deficit hyperactivity disorder symptoms: The evidence . Preventive Medicine , 52 ( Suppl 1 ) S70 – S74 . doi:10.1016/j.ypmed.2011.01.022 [doi] [DOI] [PubMed] [Google Scholar]
- Guilamo-Ramos V., Bouris A., Lee J., McCarthy K., Michael S. L., Pitt-Barnes S., Dittus P. ( 2012. ). Paternal influences on adolescent sexual risk behaviors: A structured literature review . Pediatrics , 130 , 2011 – 2066 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins J. D., Catalano R. F., Kosterman R., Abbott R., Hill K. G. ( 1999. ). Preventing adolescent health-risk behaviors by strengthening protection during childhood . Archives of Pediatrics and Adolescent Medicine , 153 , 226 – 234 . [DOI] [PubMed] [Google Scholar]
- Humphreys K. L., Eng T., Lee S. S. ( 2013. ). Stimulant medication and substance use outcomes: A meta-analysis . JaMa Psychiatry , 70 ( 7 ), 740 – 749 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. S., Humphreys K. L., Flory K., Liu R., Glass K. ( 2011. ). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review . Clinical Psychology Review , 31 , 328 – 341 . doi:10.1016/j.cpr.2011.01.006 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibson C. L., Katusic S. K., Barbaresi W. J., Ransom J., O’Brien P. C. ( 2001. ). Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder . JAMA , 285 , 60 – 66 . doi:joc01336 [pii] [DOI] [PubMed] [Google Scholar]
- Levy L. D., Fleming J. P., Klar D. ( 2009. ). Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder . International Journal of Obesity , 33 , 326 – 334 . doi:10.1038/ijo.2009.5 [doi] [DOI] [PubMed] [Google Scholar]
- Marshal M. P., Molina B. S., Pelham W. E., Jr. ( 2003. ). Childhood ADHD and adolescent substance use: An examination of deviant peer group affiliation as a risk factor . Psychology of Addictive Behaviors , 17 , 293 – 302 . doi:10.1037/0893–164X.17.4.293 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy S., Asherson P., Coghill D., Hollis C., Murray M., Potts L., Sayal K., de Soysa R., Taylor E., Williams T., Wong I. C. ( 2009. ). Attention-deficit hyperactivity disorder: Treatment discontinuation in adolescents and young adults . The British journal of Psychiatry , 194 , 273 – 277 . doi:10.1192/bjp.bp.107.045245 [DOI] [PubMed] [Google Scholar]
- Mikami A. Y., Hinshaw S. P., Arnold L. E., Hoza B., Hechtman L., Newcorn J. H., Abikoff H. B. ( 2010. ). Bulimia nervosa symptoms in the multimodal treatment study of children with ADHD . The International Journal of Eating Disorders , 43 , 248 – 259 . doi:10.1002/eat.20692 [DOI] [PubMed] [Google Scholar]
- Mikami A. Y., Hinshaw S. P., Patterson K. A., Lee J. C. ( 2008. ). Eating pathology among adolescent girls with attention-deficit/hyperactivity disorder . Journal of Abnormal Psychology , 117 , 225 – 235 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S., Hinshaw S. P., Eugene Arnold L., Swanson J. M., Pelham W. E., Hechtman L., Hoza B., Epstein J. N., Wigal T., Abikoff H. B., Greenhill L. L., Jensen P. S., Wells K. C., Vitiello B., Gibbons R. D., Howard A., Houck P. R., Hur K., Lu B., Marcus S., ; Group M. T. A. C. ( 2013. ). Adolescent substance use in the multimodal treatment study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication . Journal of the American Academy of Child and Adolescent Psychiatry , 52 , 250 – 263 . doi:10.1016/j.jaac.2012.12.014 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S., Marshal M. P., Pelham W. E., Jr., Wirth R. J. ( 2005. ). Coping skills and parent support mediate the association between childhood attention-deficit/hyperactivity disorder and adolescent cigarette use . Journal of Pediatric Psychology , 30 , 345 – 357 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S., Pelham W. E., Cheong J., Marshal M. P., Gnagy E. M., Curran P. J. ( 2012. ). Childhood attention-deficit/hyperactivity disorder (ADHD) and growth in adolescent alcohol use: The roles of functional impairments, ADHD symptom persistence, and parental knowledge . Journal of Abnormal Psychology , 121 , 922 – 935 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B. S., Pelham W. E., Jr. ( 2003. ). Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD . Journal of Abnormal Psychology , 112 , 497 – 507 . [DOI] [PubMed] [Google Scholar]
- Pennington B. F., Ozonoff S. ( 1996. ). Executive functions and developmental psychopathology . Journal of Child Psychology and Psychiatry, and Allied Disciplines , 37 , 51 – 87 . [DOI] [PubMed] [Google Scholar]
- Schoenfelder E. N., Faraone S. V., Kollins S. H. ( 2014. ). Stimulant treatment of ADHD and cigarette smoking: A meta-analysis . Pediatrics , 133 , 1070 – 1080 . doi:10.1542/peds.2014‐0179 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer T. J., Faraone S. V., Tarko L., McDermott K., Biederman J. ( 2014. ). Attention-deficit/hyperactivity disorder and adverse health outcomes in adults . The Journal of Nervous and Mental Disease , 202 , 725 – 731 . [DOI] [PubMed] [Google Scholar]
- Stormshak E. A., Dishion T. J. ( 2009. ). A school-based, family-centered intervention to prevent substance use: The family check-up . The American Journal of Drug and Alcohol Abuse , 35 , 227 – 232 . doi:10.1080/00952990903005908 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther C. A., Cheong J., Molina B. S., Pelham W. E., Jr., Wymbs B. T., Belendiuk K. A., Pedersen S. L. ( 2012. ). Substance use and delinquency among adolescents with childhood ADHD: The protective role of parenting . Psychology of Addictive Behaviors , 26 , 585 – 598 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaso M. J., Park A., Antshel K. M. ( 2015. ). Treatments for adolescents with comorbid ADHD and substance use disorder: A systematic review . Journal of Attention Disorders . doi:10.1177/1087054715569280. https://www.researchgate.net/profile/Aesoon_Park/publication/272079159_Treatments_for_Adolescents_With_Comorbid_ADHD_and_Substance_Use_Disorder_A_Systematic_Review/links/54de20ac0cf23bf2043a9cbe.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]