Abstract
Objective. Patients in remote areas lack access to specialist care and pain management services. In order to provide pain management care to patients remote from our center, we created a telemedicine pain clinic (telepain) at Massachusetts General Hospital (MGH) in Boston, MA to extend services to the Island of Martha’s Vineyard.
Design. Over 13 months, 238 telepain video clinic evaluations were conducted. A pain physician visited the island 1–2 days per month and performed 121 interventions. Given the novelty of telemedicine clinics, we surveyed patients to gauge satisfaction and identify perceived weaknesses in our approach that could be addressed. Forty-nine consecutive patients answered a 14-question, 5-point balanced Likert-scale survey with 1 (no, definitely not) being most negative and 5 (yes, definitely) being most positive.
Setting. Patients on Martha’s Vineyard referred for pain management consultation services via telemedicine.
Patients. Forty-nine consecutive patients evaluated via telemedicine.
Interventions. Likert-scale survey administered.
Measures. Questions measured patient impressions of video-based visits with their doctor, convenience of the visit, concerns about privacy, and whether they would recommend such a visit, among other items.
Results. Mean respondent scores for each question were >4.3 indicating a favorable impression of the telepain clinic experience. Lowest mean scores were found when respondents were asked to compare the care they received by telepain versus an in-person visit, or whether they were able to develop a friendly relationship with the doctor.
Conclusions. The results suggest an overall positive reception of telepain by patients, yet highlight the challenge of building a patient-physician relationship remotely.
Keywords: Telemedicine, Telehealth, Pain Medicine, Pain Management
Introduction
Chronic pain affects over 100 million American adults [ 1 ]. As reported by the Institute of Medicine, “pain costs society at least $500–$635 billion annually [ 1 ].” To appreciate its profound impact, one must appreciate that the costs of chronic pain are higher than those of diabetes mellitus, heart disease, and cancer combined. Furthermore, back pain alone is the leading cause of disability in Americans under 45 years old [ 2 ]. The costs of chronic pain care results from work-day and productivity loss, as well as high healthcare resource utilization such as prolonged hospitalizations, and more frequent emergency room visits. Future challenges of chronic pain medicine are multifold including overcoming the geographical barriers that separate pain sufferers from accessible care and the discomfort of some primary care providers in managing complicated chronic pain. Nonetheless, telemedicine offers a unique solution to these obstacles by extending medical care to patients in distant communities and providing readily accessible counseling to primary care physicians caring for this challenging subset of patients.
Telemedicine is defined as the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. It includes a growing variety of applications and services using two-way video, e-mail, smart phones, wireless tools and other forms of telecommunications technology [ 3 ]. Telemedicine dates back to the early twentieth century and has been implemented in many medical fields such as cardiology, psychiatry, and neurology. In the field of neurology, telemedicine has impacted stroke management enabling early intervention by specialist care remotely, improved patient outcomes, and has helped to overcome neurologist shortages [ 4 , 5 ]. Similarly, telemedicine in pain management has been reported to improve care in patients with multiple sclerosis and phantom limb pain [ 6 , 7 ]. In the Canadian province of Ontario, telemedicine has been used to support primary care physicians in caring for chronic pain patients [ 8 ]. Pain management psychologists have also successfully used similar technology to provide services to chronic pain patient populations [ 9 ].
Distance separates many chronic pain patients from obtaining necessary care from pain specialists. This distance is particularly noticeable in rural communities where patients are not only physically separated from pain specialists, but they tend to be financially burdened with higher rates of poverty, lack of insurance, and less formal education [ 10 ]. Additionally, some primary care providers have expressed discomfort with caring for chronic pain patients, especially those with high opioid requirements. The lack of comfort of primary care physicians in caring for chronic pain patients was suggested by a recent survey of 856 primary care physicians and nurse practitioners in Washington State, where providers expressed the need for continuing support and education in treating patients with chronic non-cancer pain [ 10 ]. Project ECHO (Extension for Community Healthcare Outcomes) focused on addressing the needs of rural and underserved communities by providing weekly chronic pain didactics and case presentations to primary care physicians [ 11 , 12 ]. Providers were educated in a multidisciplinary approach with didactics provided by specialists in the fields of neurology, internal medicine, addiction psychiatry, and pain management. From the period of January 2010 to December 2012, there were 3,835 total instances of participation, representing: 763 individuals, 191 sites, 29 states and the District of Columbia (DC). Ninety-three individuals presented 304 cases: 261 new, and 43 follow-up. It is noteworthy that CME evaluations completed by the providers showed statistically significant improvement in participant self-reported knowledge, skills, and practice [ 11 ]. This project aimed at equipping providers in underserved areas with the necessary tools to meet the ever-growing needs of their patients.
Another advantage of telemedicine is that it has shown itself in certain studies to be more efficacious than the current standard of pain care provided by primary care physicians. The SCOPE trial enrolled 250 patients with chronic musculoskeletal pain of greater than 3 months and randomized 124 people to the intervention group and the remaining 126 people to the usual care group. This study involved 12 months of telephone-delivered collaborative care management intervention by nursing staff along with one in-person meeting with a nurse who presented the patient’s care to a pain specialist physician in order to develop a treatment plan. All patients in the intervention group were treated by an algorithm approach to optimize analgesia. Control patients continued to have their usual care provided by their primary care providers. Initially the baseline BPI (Brief Pain Inventory) scores were 5.32 for the intervention group and 5.12 for the control group. The results of the study were significant for the intervention group having 1.02 points lower on BPI score compared to the control group and at least 20% improvement in pain score at the 12-month follow-up. Those in the control group were more likely to experience worsening of pain 36% versus 19% compared with intervention group [ 13 ]. This study suggested that telemedicine can provide a better standard of care compared to the current practices, and prevent worsening of pain in its participants. It highlighted the role of midlevel providers in bridging the gap between the high demand for pain medicine and the low supply of pain specialists.
Our program was aimed at extending pain management services to the residents of Martha’s Vineyard in Massachusetts. Martha’s Vineyard is an island accessible only by sea or air that is home to 15,000 residents year-round, with an increased population of 115,000 during the summer months. Prior to the telehealth pain program, residents of the island would have to endure the inconvenience and cost ($63-$127 per vehicle and an additional $17 per adult traveler) associated with taking a 45-minute ferry ride followed by a 2-hour drive for evaluations, interventions, and follow-up visits with pain specialists [ 14 ].
Methods
The study protocol was approved by the Institutional Review Board of MGH and all patients were asked to review a privacy and confidentiality agreement describing telemedicine services before undergoing care. The MGH Telehealth Program, a hospital-wide program created to support distance medicine in New England, instituted a collaboration with Martha’s Vineyard Hospital (MVH) in 2013 to develop a telepain program. Patients at MVH were seen in telepain clinic 3 days per month by a physician located at MGH for initial consultations and follow-up visits. Communication was mediated by live videoconference (Vidyo, Inc. Hackensack, NJ, USA) controlled by the physician at MGH. The patient and family members, along with a registered nurse were oriented approximately five feet away from a media tower consisting of a large television screen and live audio/visual capabilities in a patient exam room at MVH. Vital signs were recorded in a shared electronic medical record. A registered nurse, trained in physical examination of pain conditions and medical management, performed the exam of the patients at MVH during the clinic visit under direct physician supervision via live videoconference and also verbally announced all findings. Physical examinations were again repeated by the physician during on-site visits prior to any patient intervention. Laboratory data and imaging studies were reviewed in the shared electronic medical record. One or 2 days per month, MGH physicians would travel to MVH to perform on-site pain interventions.
To evaluate patient satisfaction with the telepain experience, a 14-question survey was created using the principles of survey development for telemedicine suggested by Demiris [ 15 ] emphasizing: the importance of designing a survey based on a detailed definition of what it intends to measure; testing it before administering it to the larger sample; and reliability, validity, and generalizability. The patients were asked by the RN to voluntarily complete the survey after either telepain initial or follow-up visit. Forty-nine consecutive patients were asked, and all agreed to participate. Questions were chosen to measure overall satisfaction, specific experience using the technology, convenience to the patient, patient-physician relationship, and ability to communicate. Answers to all questions used a 5-point balanced Likert scale to avoid ceiling effect [ 16 ]. Response range was anchored between 1 (no, definitely not) to 5 (yes, definitely) ( Table 1 ).
Table 1.
Survey questions and response options
Questions:
|
Out of the 14 survey statements, 11 were written with positive tone, that is, greater agreement was associated with greater satisfaction and vice versa. The remaining three questions were written in a negative tone. In order to present the results with consistent tone, the responses to the negative tone questions were reversed (e.g., “No, definitely not” was converted to “Yes, definitely”).
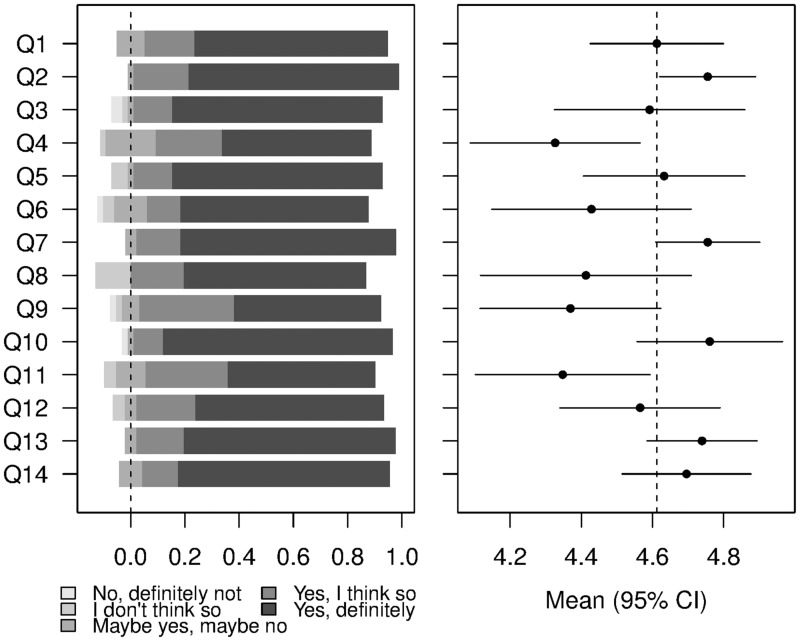
The percentages of the five responses for each question were calculated and presented in a diverging stacked bar chart, in which the fraction of respondents who agreed with the statement are shown to the right of the zero line; respondents who disagreed were shown to the left. Numerical values from one through five were assigned to the Likert scale responses. The mean numerical score and its associated 95% confidence interval were then computed for each question and presented in a forest plot, adjacent to the diverging stacked bar chart ( Figure 1 ).
Figure 1.
Forest plot shows percentage of responses for each survey question (Q1-Q14) on the left, with the mean response score with 95% confidence interval on the right.
Results
In the first 13 months of the telemedicine program, a total of 238 virtual telepain evaluations were performed (185 initial consultations and 53 follow-up visits). One hundred twenty-one on-site evaluations and procedural interventions were conducted during the same period. The most commonly performed procedures included epidural steroid injections (N = 48) and medial branch blocks (N = 29). Forty-nine consecutive patients agreed to be anonymously surveyed after their telepain visit and responded to the majority of questions positively.
Questions measured patient impressions of video-based visits with their doctor, convenience of the visit, concerns about privacy, and whether they would recommend such a visit, among other items ( Table 1 ). Mean respondent scores for each question were >4.3 indicating an overall favorable impression of the telepain clinic experience. Mean respondent score for all questions was 4.57. Lowest mean scores were found when respondents were asked to compare the care they received by telepain versus an in-person visit (Question 4, 4.32), or whether they were able to develop a friendly relationship with the doctor (Question 11, 4.34). Highest mean scores were found when respondents were asked if they were satisfied with the telehealth visit (Question 2, 4.75), if they were comfortable talking by video with a specialist (Question 7, 4.75), and if there was any difficulty hearing or seeing the doctor (Question 10, 4.76).
Discussion
This study demonstrates that it is possible to successfully develop and maintain a telemedicine pain management program in an area as remote as Martha’s Vineyard, which contains one of the top 20 critical access hospitals in the United States and was previously lacking dedicated pain medicine services. With an estimated 8,000-9,000 pain medicine specialists in the United States mainly congregated in large cities, the geographical barriers create a true health care disparity for residents in such areas as Martha’s Vineyard. For example, highly desired areas such as California have upwards of 900 pain medicine specialists, while the state of Wyoming has approximately 13 pain specialists [ 17 ]. Additionally, prior to the establishment of this telemedicine program, patients had to bear the inconvenience and costs of boarding a ferry and traveling several hours to obtain medical care. Our telepain program was able to eliminate these unfavorable conditions and deliver services with overall patient satisfaction.
This report is one of the few known existing programs that allow patients to have direct contact with a pain medicine specialist via live video-teleconferencing. Previous studies feature a system whereby primary care providers are able to use telemedicine to contact specialists regarding management of their chronic pain patients or attend applicable didactic sessions [ 10 , 11 , 13 ]. For example, the Specialty Care Access Network-ECHO pain management program (SCAN-ECHO-PM) provided primary care providers with case-based pain management specialist consultation that led to increased utilization of physical medicine services and initiation of nonopioid analgesics for patients in the Veterans Health Administration [ 18 ]. Another study demonstrated rapid and cost-effective access of telehealth consultation visits between primary care providers in Washington State and a team of pain medicine specialists compared with ‘in-clinic visits,’ as it pertains to transaction cost analysis [ 19 ]. In our study, the quality of care was maintained via direct videoconferences with patients and pain specialists, physical exams performed by appropriately trained nursing staff, and monthly physician visits to the island for procedural interventions. Our project demonstrated that telemedicine can be used as a tool to reach out to a poorly accessible patient population, to greatly expand the number of participants during the initial study period, and to achieve high patient satisfaction with the services provided.
With the heightened interest in using telemedicine in pain medicine care, there have been efforts to identify the limitations of such programs. For patients residing in rural areas with very limited access to physicians, telemedicine offers hope of access to appropriate healthcare. However, much work remains to be done to examine its efficacy compared with in-person physician visits. In a comprehensive review of telehealth programs in pain medicine, the authors identified that at the present time there has been a lack of outcomes research addressing the short- and long-term benefits of telehealth. [ 20 , 21 ]. Much of the outcomes research, including our featured survey, report on patients’ subjective experiences with the program. It would be imperative to collect objective patient data on telemedicine programs, such as recording patients’ longitudinal opioid medication usage once appropriate telemedicine treatment is established and maintained. There are also financial limitations to such programs including the expenses of initiating such programs, and challenges in obtaining financial reimbursement from third parties for services that are not in person with physicians. On the other hand, these programs may prove to be rather cost effective by reducing the number of “no shows to appointment” and decreasing the number of hospitalizations and emergency department visits for patients who previously had no access to care. There are also concerns about the shortcomings of technology including bandwidth strength and its ability to maintain good connectivity during these sessions. Finally, there is thought that telemedicine compromises the quality of care by limiting ability to obtain pertinent clinical information over such telehealth sessions.
Specific to our study, there are limitations that exist. Although a random selection of 49 consecutive patients were surveyed, this sample size may not be entirely representative of the chronic pain patients on Martha’s Vineyard, or other pain populations elsewhere. Additionally, in the future, studies should report demographic data, types of pain syndromes and conditions, and analgesic/opioid requirements for a comprehensive assessment of the patient population being treated. It must also be noted that patient survey responses may be skewed because of social desirability to respond favorably. Further studies must also be performed to determine the reproducibility of these findings and to establish threshold values defining successes and failures of responses given.
The future of this program will include collecting objective data comparing the efficacy of telemedicine with in-person physician visits. This will include comparing pain scores between patients randomized to telemedicine interventions versus control group receiving standard via in person visits, performing cost effectiveness analysis of the program, and examining whether opioid usage decreases once appropriate telemedicine intervention and follow-up is established. While much remains to be investigated in the emerging field of telemedicine, our project demonstrates success in bridging the geographical gaps in healthcare disparities in the field of pain medicine and that patients have an overall positive reception of the service.
Conflicts of interest: There are no conflicts of interest to report.
References
- 1. Johannes CB, Le TK, Zhou X. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research . Washington, DC: : National Academy of Sciences; ; 2011. . [Google Scholar]
- 2. U.S. Department of Health and Human Services, National Center for Health Statistics . Chartbook on trends in the health of Americans. Special feature: Pain. Washington, DC: U.S. Government Printing Office; 2006. . Available at: http://www.cdc.gov/nchs/data/hus/hus06.pdf (accessed: March 2016).
- 3. American Telemedicine Association . What is telemedicine? 2015. . Available at: http://www.americantelemed.org/about-telemedicine (accessed: March 2016).
- 4. Silva GS, Schwamm LH. Use of telemedicine and other strategies to increase the number of patients that may be treated with intravenous thrombolysis . Curr Neurol Neurosci Rep 2012. ; 12 ( 1 ): 10.. [DOI] [PubMed] [Google Scholar]
- 5. Müller-Barna P, Hubert GJ, Boy S , et al. . Telestroke units serving as a model of care in rural areas: 10-year experience of the telemedical project for integrative stroke care . Stroke 2014. ; 45 ( 9 ): 2739 – 44 . [DOI] [PubMed] [Google Scholar]
- 6. Gover-Chamlou A, Tsao JW. Telepain management of phantom limb pain using mirror therapy . Telemed J E Health 2016. ; 22 ( 2 ): 176 – 9 . [DOI] [PubMed] [Google Scholar]
- 7. Khan F, Amatya B, Kesselring J, Galea M. Telerehabilitation for persons with multiple sclerosis . Cochrane Database Syst Rev 2015. ; Apr 9; 4 : CD010508 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dubin RE, Flannery J, Taenzer P , et al. . ECHO Ontario chronic pain & opioid stewardship: Providing access and building capacity for primary care providers in underserviced, rural, and remote communities . Stud Health Technol Inform 2015. ; 209 : 15 – 22 . [PubMed] [Google Scholar]
- 9. Fisher E, Law E, Palermo TM, Eccleston C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents . Cochrane Database Syst Rev 2015. ; Mar 23; 3 : CD011118 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eaton LH, Gordon DB, Wyant S , et al. . Development and implementation of a telehealth-enhanced intervention for pain and symptom management . Contemp Clin Trials 2014. ; 38 ( 2 ): 213 – 20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Katzman JG, Comerci G, Jr, Boyle JF , et al. . Innovative telementoring for pain management: Project ECHO pain . J Contin Educ Health Prof 2014. ; 34 ( 1 ): 68 – 75 . [DOI] [PubMed] [Google Scholar]
- 12. Scott JD, Unruh KT, Catlin MC , et al. . Project ECHO: A model for complex, chronic care in the Pacific Northwest region of the United States . J Telemed Telecare 2012. ; 18 ( 8 ): 481 – 4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kroenke K, Krebs EE, Wu J , et al. . Telecare collaborative management of chronic pain in primary care: A randomized clinical trial . JAMA 2014. ; 312 ( 3 ): 240 – 8 . [DOI] [PubMed] [Google Scholar]
- 14. The Steamship Authority . Ferry service between Martha’s Vineyard and Cape Cod: Fare information for residents. 2015. . Available at: https://www.steamshipauthority.com/residents/fares (accessed: March 2016).
- 15. Demiris G. Principles of survey development for telemedicine applications . J Telemed Telecare 2006. ; 12 ( 3 ): 111 – 5 . [DOI] [PubMed] [Google Scholar]
- 16. Masino C, Lam TCM. Choice of rating scale labels: Implication for minimizing patient satisfaction response ceiling effect in telemedicine surveys . Telemed J E Health 2014. ; 20 ( 12 ): 1150 – 5 . [DOI] [PubMed] [Google Scholar]
- 17. U.S. News and World Report . Find pain management specialists. July 11, 2015. . Available at: http://health.usnews.com/doctors/location-index/pain-management-specialists (accessed: March 2016).
- 18. Frank JW, Carey EP, Fagan KM , et al. . Evaluation of a telementoring intervention for pain management in the Veterans Health Administration . Pain Med 2015. ; 16 ( 6 ): 1090 – 100 . [DOI] [PubMed] [Google Scholar]
- 19. Theodore BR, Whittington J, Towle C , et al. . Transaction cost analysis of in-clinic versus telehealth consultations for chronic pain: Preliminary evidence for rapid and affordable access to interdisciplinary collaborative consultation . Pain Med 2015. ; 16 ( 6 ): 1045 – 56 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McGeary DD, McGeary CA, Gatchel RJ. A comprehensive review of telehealth for pain management: Where we are and the way ahead . Pain Pract 2012. ; 12 ( 7 ): 570 – 7 . [DOI] [PubMed] [Google Scholar]
- 21. Wechsler LR. Advantages and limitations of teleneurology . JAMA Neurol 2015. ; 72 ( 3 ): 349 – 54 . [DOI] [PubMed] [Google Scholar]