Abstract
Purpose of the Study
Implementing quality improvement (QI) programs in nursing homes continues to encounter significant challenges, despite recognized need. QI approaches provide nursing home staff with opportunities to collaborate on developing and testing strategies for improving care delivery. We present a theory-driven and user-friendly adaptable framework and facilitation package to overcome existing challenges and guide QI efforts in nursing homes.
Design and development
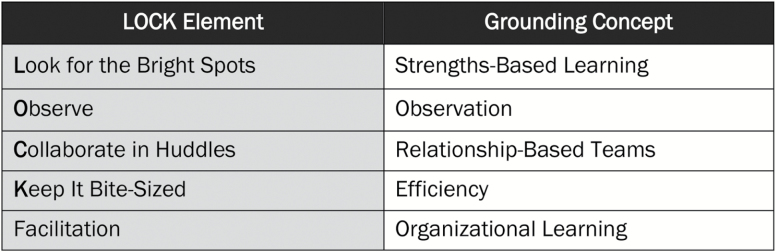
The framework is grounded in the foundational concepts of strengths-based learning, observation, relationship-based teams, efficiency, and organizational learning. We adapted these concepts to QI in the nursing home setting, creating the “LOCK” framework. The LOCK framework is currently being disseminated across the Veterans Health Administration.
Results
The LOCK framework has five tenets: (a) Look for the bright spots, (b) Observe, (c) Collaborate in huddles, (d) Keep it bite-sized, and (e) facilitation. Each tenet is described. We also present a case study documenting how a fictional nursing home can implement the LOCK framework as part of a QI effort to improve engagement between staff and residents. The case study describes sample observations, processes, and outcomes. We also discuss practical applications for nursing home staff, the adaptability of LOCK for different QI projects, the specific role of facilitation, and lessons learned.
Implications
The proposed framework complements national efforts to improve quality of care and quality of life for nursing home residents and may be valuable across long-term care settings and QI project types.
Keywords: Quality of care, Observation, Huddles, Strengths-based learning, Relational coordination
Concerns about quality of care have plagued nursing homes for decades. High-profile instances of abuse or neglect attract public outcry, but improvement has nevertheless not kept pace with documented need (Government Accountability Office, 2015; Grabowski et al., 2016). In this challenging environment, quality improvement (QI) methods may hold promise for improving care in nursing homes (Castle & Ferguson, 2010). QI creates opportunities for nursing home staff to work together across disciplines and hierarchies to identify problem areas and to develop and test strategies for improvement (Allen-Burge, Burgio, Bourgeois, Smith, & Nunnikhoven, 2001; Wilson & Davies, 2009). The Patient Protection and Affordable Care Act (ACA) of 2010 mandated that, over the next several years, all nursing homes implement a program to improve quality of care. Little practical guidance exists, however, for those who are developing such programs for the first time. In this manuscript, we first discuss the importance of QI efforts for improving quality of care, barriers to and facilitators of QI program implementation, and existing nursing home QI programs. We then describe the critical QI-related concepts that create the foundation of a theory-driven, user-friendly integrated QI framework, and share a case study of how the framework may be used in practice. We conclude with a discussion of practical applications of the framework for nursing home staff, its adaptability for different QI projects, the specific role of facilitation, and lessons learned.
Design and Development
Background
Quality Improvement Approaches Can Improve Quality of Care
The Omnibus Budget Reconciliation Act of 1987 (OBRA ‘87) enacted sweeping changes intended to improve quality of care in nursing homes. But since its implementation, there have been, at best, mixed findings regarding improvement across a range of indicators (Castle & Ferguson, 2010; Government Accountability Office, 2015; Office of Inspector General, 2014). A more recent shift away from a regulation-based impetus for change and toward a business-case approach (e.g., pay-for-performance) has also failed to produce meaningful improvements in nursing home quality (Grabowski et al., 2016; Werner, Konetzka, & Kim, 2013). The ACA contains the first significant legislation focused on improving quality of care in Centers for Medicare and Medicaid Services (CMS)-certified nursing homes since OBRA ‘87. As part of the ACA mandate, CMS-certified nursing homes will be required to implement quality assurance and performance improvement (QAPI) programs. While this type of policy change is significant, staff-based efforts can be argued to be at the heart of any meaningful changes (Castle & Ferguson, 2010). QI methods enable providers to develop initiatives tailored to the individual needs and specific capabilities of their nursing home.
Barriers and Facilitators to QI Efforts in Nursing Homes
The often hectic nursing home environment frequently renders QI a low priority for staff. Chronic understaffing, for example, can leave frontline staff struggling to complete their typical daily duties, leading to the perception of QI work as an additional burden (Collier & Harrington, 2008). There may thus be little incentive on an individual level to engage in and maintain QI activities. For those who are interested in QI, there are few training opportunities (Smith, Castle, & Hyer, 2013). One-size-fits-all approaches to QI, in addition, do not translate easily across facilities, because nursing homes are not homogeneous in terms of size, location, staffing levels, staff skills and knowledge, and regulatory requirements. Collection of resident-level QI data is an additional challenge due to the difficulty of collecting reliable satisfaction data from residents with cognitive impairment, comorbidities, and polypharmacy (Sangl et al., 2007). These barriers contribute individually and collectively to low systematic uptake of QI interventions (Parmelee, 2004; Tolson et al., 2011), although some relatively widely adopted QI programs exist, as described below.
Existing Models for QI
Successful QI efforts typically engage all levels of staff and leadership in the QI process, have clear goals, focus on systems change, consider organizational and clinical barriers to change, encourage the development of problem-solving skills among staff, and create mechanisms for self-monitoring to provide timely feedback on progress and success (Bowers, Nolet, Roberts, & Esmond, n.d.; Centers for Medicare and Medicaid Services, 2014). A limited number of such QI models have been created for nursing homes (Bakerjian & Zisberg, 2013; Reinhard & Stone, 2001; Stone et al., 2002). One noteworthy example is the Wellspring Model of QI that advances an organizational culture dedicated to resident-centered care (Reinhard & Stone, 2001). Early evaluation of the model has shown decreases in staff turnover, improved performance on federal surveys, better quality of life for residents, and improved quality of interactions between residents and staff (Stone et al., 2002). Implementation of the Wellspring model, however, requires large-scale financial investments—including the creation of data systems, training programs, and professional QI staff roles—to set up data-driven QI systems.
ACA-mandated QAPI programs are expected to focus on improving residents’ quality of life and quality of care through systematic and data-driven QI methodologies (Centers for Medicare and Medicaid Services, 2014). According to CMS, the goals of QAPI are to have all members at all levels of the organization involved in the following: identifying opportunities for improvement, addressing challenges in systems or processes, developing and implementing interventions, and conducting ongoing monitoring of the effectiveness of interventions (Centers for Medicare and Medicaid Services, 2014). In anticipation of this mandate, CMS and some long-term care providers have started to create guiding documents for nursing homes (Centers for Medicare and Medicaid Services, n.d.), including extensive “menus” of QI strategies and tools like Plan-Do-Study-Act checklists (e.g., the Nursing Home Quality Care Collaborative Change Package (Centers for Medicare and Medicaid Services, 2013) and Getting Better All the Time: Working Together for Continuous Improvement (Wyatt, 2010)). Yet nursing homes may still struggle with implementing these strategies. For facilities and individual staff members not familiar with QI, the amount of information provided may be overwhelming. It is thus necessary to identify approaches that all nursing home staff members can use to guide staff-driven QI efforts, regardless of their previous experience or perceived barriers. To address this need, we present a theory-driven, user-friendly, and adaptable framework called “LOCK” to guide QI efforts in nursing homes.
Conceptual Framework
To develop the tenets of the LOCK framework, we reviewed existing approaches to QI work in nursing homes and other settings and examined the behavior change and implementation science literatures. Through this effort, we identified five concepts critical to successful QI efforts that may be easily implemented as part of nursing home staff members’ regular routines: strengths-based learning, observation, relationship-based teams, efficiency, and organizational learning. Simply focusing on implementation of an intervention is not sufficient to effect sustained change in nursing homes. Rather, QI efforts need to be surrounded by a framework, such as LOCK, that creates systematic change that will allow for long-term sustainability.
Strengths-Based Learning
The business world has long looked for “positive deviants,” identifying programs that succeed in difficult environments and then studying them to learn how they overcome hurdles and facilitate progress (Kaplan et al., 2010; Lawton, Taylor, Clay-Williams, & Braithwaite, 2014). This strategy has also been used in healthcare (Bradley et al., 2009; Marsh, Schroeder, Dearden, Sternin, & Sternin, 2004). Nursing home frontline staff have reported a preference for tools that focus on areas where staff are doing well (Hartmann et al., Forthcoming). Yet nursing home staff members are subject to frequent inspections and evaluations. These focus on areas of deficit, and resulting reports provide few practicable suggestions for how to improve. In other settings, studies have demonstrated that strengths-based approaches to professional development increase retention of nursing staff and improve the work environment for all clinical staff (Vogt et al., 2015). Strengths-based approaches have also been employed in inpatient mental health care settings to overcome staff and organizational resistance to implementing person-centered care (Beckett et al., 2013). This literature supports the contention that recognizing and sharing positive instances of ideal practice will encourage those doing well to continue those behaviors, give those who are not doing well tangible examples of how they may improve, and provide clearer directives regarding what needs to be done differently to achieve success than would be obtained by focusing on negative instances of poor practice.
Observation
Observation is part of a larger system of human factors engineering principles, which maintain that human systems can be improved by using an integrated approach to study the work system (Caravon et al., 2006). Enabling healthcare professionals to step away from their usual routines and observe the flow of their work environment is a technique increasingly employed in QAPI. A recent review of sixty-nine studies using observation for assessment of clinical performance, for example, underscores the utility of this technique for highlighting factors that can affect quality and safety (Yanes et al., 2016). Observation can yield information about complex and dynamic processes that may be less amenable to other data gathering techniques and is frequently used to assess teamwork and communication (Yanes et al., 2016). Observations by people who are familiar with the realities of a clinical practice environment are essential to the development of an accurate and detailed workflow (Agency for Healthcare Research and Quality, n.d.-b). Studies using human factors observation (Schraagen et al., 2010) have been conducted in many healthcare contexts but only infrequently in nursing homes (Kurowski, Buchholz, Punnett, & ProCare Research, 2014).
Relationship-Based Teams
In almost any healthcare environment, it is difficult to identify gaps and implement facility-wide changes if data are collected and decisions made without involving individuals representing all aspects of the shared work processes (Agency for Healthcare Research and Quality, n.d.-a). A necessary component, therefore, to overcoming barriers to successful QI in nursing homes is effective coordination of team work, as identified by the theory of relational coordination (Gittell, 2012). In this theory, frequent, timely, and accurate communication minimizes delay, facilitates rapid response to patient need, and reduces the potential for error. Such communication is dependent on the underlying quality of relationships among the individuals involved in the shared work processes. This is operationalized as the extent to which those individuals have shared goals, shared knowledge, and mutual respect. Nursing home staff members’ work, for example, often involves task interdependence, uncertainty, and time constraints. Improved effective relational coordination in these situations can lead to higher quality outcomes by allowing individuals to manage their tasks with fewer errors and less wasted effort (Gittell, 2011).
Efficiency
Communication between individuals involved in QI efforts should be focused, direct, and brief (Agency for Healthcare Research and Quality). Quality and teamwork improvement models from other industries or healthcare settings also commonly include a focus on keeping all elements of any change effort manageable (Agency for Healthcare Research and Quality; Phillips, Hebish, Mann, Ching, & Blackmore, 2016). In the nursing home environment, it is particularly important that communication methods are easy to use and are not perceived as time-intensive. Other elements of QI projects (e.g., training or data collection, entry, or analysis) should also be held to these standards. Having short, practical trainings that can happen on the floor without disrupting staff members’ ability to provide care is critical. Continuous incremental improvements that lead toward a greater goal have been shown to be more palatable and allow staff to see outcomes from their efforts on a more regular basis (Phillips et al., 2016).
Organizational Learning
Facilitation plays a unique role in intervention and may be a key component of successful implementation of evidence-based practices in clinical settings (Harvey et al., 2002). It is grounded in organizational learning theory, which describes the phenomena of knowledge translation—knowledge is acquired by individuals, transmitted throughout an organization, stored in organizational memory (e.g., through behavioral norms or formal policies), and influences subsequent learning processes (Argote & Miron-Spektor, 2011). Facilitation, which can stimulate learning in organizations, involves a deliberate process of interactive problem solving and support that occurs in the context of a recognized need for improvement and supportive interpersonal relationships (Stetler et al., 2006) and is often used in conjunction with other implementation activities. Individuals serving as facilitators may be internal or external to the organization. They support the change processes through well-planned, proactive, and mediating roles. Facilitators help end-users gain the knowledge, skills, and confidence to implement a new practice and thus may strengthen the uptake of new QI frameworks (Harvey et al., 2002).
Results
LOCK Framework
We operationalized the grounding concepts of strengths-based learning, observation, relationship-based teams, efficiency, and organizational learning in the “LOCK” framework: (1) Look for the bright spots, (2) Observe, (3) Collaborate in huddles, and (4) Keep it bite-sized, and (5) facilitation (see Figure 1). Each element is described in detail below. LOCK is specifically designed to build on and take advantage of the strong team relationships that exist in nursing homes. Once a nursing home selects a QI project, LOCK helps guide staff in their efforts to achieve positive behavior change through observation, feedback, and relationship-building that fits easily into staff members’ daily workflows. LOCK may be used on its own or in conjunction with other evidence-based interventions. The simultaneous inclusion of all LOCK elements is critical to the success of the framework, but their implementation is also highly customizable to fit the needs and characteristics of any nursing home.
Figure 1.
Relationships between grounding concepts and LOCK elements.
Look for Bright Spots
In our work using the LOCK framework in nursing homes, we instruct staff to look for local “bright spots” of positive change relevant to their chosen QI effort, asking them to focus particularly on the micro- or individual-level. If a nursing home were, for example, implementing LOCK to improve relationships between staff members and residents, they would ask staff members to conduct observations to identify instances of positive interaction. Identifying behavioral events that can serve as positive models give staff local examples that may be emulated in their own practice. This focus on where things are going well instead of where there are problems breaks two common nursing home patterns: (1) it redirects attention from deficits to strengths and (2) it engages everyone in the QI process by replacing abstract quality goals and metrics with concrete instances of sought-after behaviors. Focusing on these bright spots of care and analyzing and discovering how they differ from routine care can provide a blueprint for the spread and adoption of improved practices throughout the nursing home. Methods for identifying and sharing bright spots are included in other elements of the LOCK framework.
Observe
Working through the many details of daily nursing home life, under time-pressed and high-stimulation circumstances, typically necessitates a narrow task focus. The observer role, in contrast, allows an individual to momentarily widen the focus to take in a larger, more inclusive view of the environment. Having everyone in the nursing home participate in observations provides staff members across disciplines, shifts, and positions in the leadership hierarchy with the opportunity to participate in equivalent activities. Observation may be accomplished with validated observational measures or through informal observation approaches developed locally to target a nursing home’s specific QI foci. For LOCK, it is important that these observations focus attention on identifying and documenting areas of strength (i.e., bright spots) that may be analyzed, learned from, and shared with other staff. Observations can be completed in short intervals, guided by the needs and preferences of the nursing home. One nursing home may choose to have staff members conduct a one-minute observation every day, while another may choose a five-minute observation per week.
Collaborate in Huddles
In LOCK, relationship-based teams are created through an emphasis on strengths-based collaboration achieved in short, stand-up meetings called bright spot huddles. These brief huddles facilitate intra- and interdisciplinary communication using open dialogue and collaborative problem solving to promote shared critical thinking. Bright spots huddles can be integrated into existing huddle or stand-up meeting structures so as not to create an additional burden or necessitate another routine, although they can also be spontaneous and independent. During bright spots huddles, staff work across disciplines to discuss and understand why bright spots identified through everyone’s observations are working well, what can be learned from them, and how to move forward in spreading the bright spots to other care processes across the nursing home. Through these conversations and the projects that result from them, they build higher-functioning, relationship-based teams.
Keep it Bite-Sized
New behaviors are more likely to solidify into habits (i.e., automatic routines) when they are practiced regularly. To integrate QI seamlessly into the busy schedule of nursing home life, it is critical that the effort not be seen as a burdensome addition but rather as an easy and useful augmentation. Undertaking smaller incremental changes rather than systemic overhauls is less overwhelming and likely to produce results more quickly, thus maintaining engagement. Keeping all aspects of the QI program short, focused, collaborative, and solution-focused is key to its success, particularly as nursing home staff may feel there is no time to conduct QI work. The LOCK framework thus embraces efficiency, recommending incremental change, with no component exceeding 15 minutes.
Facilitation
Facilitation, as described above, can be critical to the success of QI projects. We provide below a fictional case study to demonstrate how LOCK, including facilitation, can help nursing home staff implement the LOCK framework in their QI efforts.
LOCK was pilot tested in Veterans Health Affairs (VHA) Community Living Centers (CLCs; i.e., nursing homes). Positive findings from preliminary data analyses prompted VHA to disseminate LOCK as part of a larger program to all CLCs across the nation (outcomes papers are forthcoming). We drew on experiences in the pilot and national rollout to develop the case study and present how a nursing home might choose to put the LOCK framework into practice to address a specific QI issue.
Case Study
Ms. Green, the administrator of Victory Nursing Home, frequently rounded through the home and often saw residents with nothing to do. Staff members, on the other hand, expressed stress about engaging with residents. She and her staff therefore began a QI project to improve staff engagement with residents using the LOCK framework and a structured observation tool that focused observations on the bright spots of care (Hartmann et al., in press; Snow et al., in press). The structured observation tool used a 5-minute protocol that involved scanning a location left to right to identify concrete examples of resident engagement and interaction with staff and noting these on a checkbox-based form.
Ms. Green initiated a series of short, iterative huddles, in which she introduced the QI project and LOCK framework to nursing leaders from each of the units and to staff from the other disciplines that worked in the home. The huddles also cultivated relationships and identified specific enthusiastic individuals or early adopters (Rogers, 2003). These early adopters became the local champions for the project. She coached them on how to serve as internal facilitators and to create specific plans using measurable goals. The champions huddled with each other and chose a pilot unit on which to begin the program. They decided that all staff members who entered the unit on a regular basis, regardless of discipline, would be responsible for conducting three 5-minute observations per week using the structured observation tool. Each champion for the pilot unit was responsible for explaining LOCK to a group of staff, teaching them how to do observations, and leading daily huddles.
After the project began, staff returned completed paper copies of the tool to the champions. This enabled champions to encourage participation from staff members who were not regularly conducting observations. The front desk clerk entered the scores into a simple Excel spreadsheet that generated reports showing change over time. The spreadsheet included a simple algorithm for converting data from the checked boxes into percentages that represented instances of residents’ engagement and positive interactions with staff.
Many direct care staff members were initially resistant to the QI project. They noted that they were already engaging with residents and did not have extra time in their already busy days. During the first few huddles, the champions quickly realized that conducting observations three times per week was too much and instead asked staff members to conduct one 5-minute observation per week. Staff members appreciated this change. During the initial huddles, champions also noted that only certain staff members talked and listened to each other.
After a few weeks of hearing about bright spots in huddles, more staff completed their observations. More staff also began to speak to each other during the huddles. The focus on positive aspects of care made conversation less threatening and more collaborative. No one was blamed, and traditionally more quiet groups, such as nursing assistants and environmental services staff, felt empowered by other people’s positive reactions to their bright spots observations.
Maintaining focus on the positive became an important aspect of the internal facilitation process. The champions created a series of bulletin boards throughout the home that showcased instances of bright spots. This enabled staff from other disciplines and units, as well as residents and families, to appreciate the positive behaviors happening in the home. In this new strengths-focused environment, staff increasingly worked together during huddles to design strategies to spread the lessons from the bright spots. Staff developed a sense of teamwork. Traditional boundaries began to crumble as staff built collaborative relationships.
Over time, small changes led to larger outcomes. In addition to decreased complaints from residents and families, staff noticed reductions in resistance to direct care activities. Increased meaningful conversation at meal times led to increased food intake for residents who required assistance with eating. More staff took time to stop and recognize all residents through eye contact, touch, and/or conversation, which often had a visible impact on resident morale. Engagement also improved between and among individual staff members and across disciplines. Consistently noticing and commending desired behaviors created a more positive culture, leading to a greater sense of community and improved team work.
Implications
The QAPI mandate will soon be implemented for CMS-certified nursing homes. It is therefore critical for researchers and providers to develop QI methodologies that can be easily adopted into practice. Although some guidance for QAPI programs has been created by CMS, the documents contain a great deal of information and may be overwhelming for nursing home staff (Centers for Medicare and Medicaid Services, n.d.). Some existing QI approaches have been successful, but they are often limited to a single aspect of quality and are not tailored to the individual nursing home. Interventions to Reduce Acute Care Transfers (INTERACT), for example, focuses specifically on reducing hospitalizations from the nursing home and Project Re-Engineered Discharge (RED), initially developed for hospital use, has been implemented in the nursing home setting to reduce post-discharge readmissions, but neither is tailorable (Berkowitz et al., 2013; Jack et al., 2009; Ouslander, Bonner, Herndon, & Shutes, 2014). Gillespie et al. advocate for QI methods that complement the resources available in a nursing home, overcome barriers to change, and foster facility-wide culture change that will ensure a sustainable quality-focused mindset (Gillespie et al., 2016). The LOCK framework may help nursing home staff members do this. The components of the framework are theory-based, simple, and adaptable. LOCK is thus designed to be adopted by any nursing home staff member for any type of nursing home QI work. It is a highly adaptable framework that encourages nursing home staff to find positive behaviors, communicate across traditional silos and disciplines, and build collaborative relationships to achieve desired outcomes. The target behaviors, the approach to observation, and the method for identifying and sharing relevant bright spots are all highly customizable to fit the characteristics and strengths of any nursing home.
To date, LOCK has only been evaluated in the context of a research project that involved external facilitation from VHA researchers. A future direction for this work is to test implementation of LOCK, not by researchers, but by staff of nursing homes and other long-term care settings, as described in the case study above. Anecdotal evidence from our work indicates this is highly achievable. Several lessons learned thus far will guide future research and should be considered when implementing LOCK in other settings.
Frequent inspections and evaluations that carry negative consequences have habituated nursing home staff to focus on identifying and reducing areas of deficiency. This means that adopting and maintaining a strengths-based mindset can be challenging. Daily reminders and vigilance are crucial to creating a lasting shift in thinking patterns and creating a strengths-based culture. In our work with LOCK in VHA, participating CLCs overcame this by creating a bright spots bulletin board in a staff break room for posting positive examples of recent bright spots, giving out happy face stickers to staff who had a bright spots moment or reported on a bright spot they had observed, and including bright spots conversations at the beginning of regular huddles and meetings.
Creating brief, structured opportunities for observation by all staff is key to successful LOCK implementation. But these observations may create their own struggles. Staff must be empowered to take the time to conduct the observations while also being open to being observed. Both the process and data from the observation must be valued and discussed.
Another important lesson is that the bite-sized components of LOCK may not look the same across nursing homes. Facilitators should remain flexible in all aspects of the QI effort to tailor it to the needs and capabilities of the staff and environment, including training, data collection, and huddles. For example, conducting frequent spontaneous huddles might work better for one nursing home while another may prefer a huddle at the same time each day. While it is important for facilitators to keep huddles bite-sized, huddles are designed to foster relationship-based team building and build rapport across disciplines and the leadership hierarchy. Brevity should not trump quality.
Finally, ensuring collaborative efforts through rapport-building and trust is critical to success and sustainability of LOCK and QI programs. When using LOCK, we encourage nursing homes to consider four criteria when selecting a QI project: (1) the QI effort must be identified collaboratively by nursing home management and front-line staff; (2) the QI effort should focus on an area causing stress for staff that, if solved, would improve resident quality of life; (3) the QI effort should require staff to work across discipline and/or hierarchy silos; and (4) the QI effort should focus on a goal that is achievable. Staff across all disciplines should be considered as potential collaborators in QI efforts.
In sum, nursing homes are under increasing pressure to identify and adopt QI methods. Nursing home staff need theory-driven, user-friendly, and adaptable QI methods that can be used by anyone. The LOCK framework operationalizes critical, evidence-based QI tenets in a manner that is simple and approachable and that can be adapted for use with any QI topic by any member of the nursing home staff. Its wider applicability, while as yet unstudied, holds promise for advancing effective and lasting QI change.
Funding
This work was supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development (grant numbers I01HX000258-01 and HX000797). This material is the result of work supported with the resources and use of facilities of the VA Medical Centers for each author. In addition, Dr. Mills receives resources and support from the Houston Center for Innovations in Quality, Effectiveness & Safety (CIN 13-413) at the Michael E. DeBakey VA Medical Center.
Acknowledgements
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs. The authors have no conflicts of interest to report.
References
- Agency for Healthcare Research and Quality (2016). TeamSTEPPS 2.0 Retrieved from http://www.ahrq.gov/teamstepps/instructor/index.html [DOI] [PubMed]
- Agency for Healthcare Research and Quality (n.d.-a). Creating quality improvement teams and quality improvement plans Retrieved from http://www.ahrq.gov/professionals/prevention-chronic-care/improve/system/pfhandbook/mod14.html [DOI] [PubMed]
- Agency for Healthcare Research and Quality (n.d.-b). Workflow Assessment for Health IT Toolkit Retrieved from https://healthit.ahrq.gov/health-it-tools-and-resources/workflow-assessment-health-it-toolkit/presentations [DOI] [PubMed]
- Allen-Burge R., Burgio L. D., Bourgeois M. S., Smith R., & Nunnikhoven J (2001). Increasing communication among nursing home residents. Journal of Clinical Geropsychology, 7(3), 213–229. [Google Scholar]
- Argote L., & Miron-Spektor E (2011). Organizational learning: From experience to knowledge. Organization Science, 22(5), 1123–1137. [Google Scholar]
- Bakerjian D., & Zisberg A (2013). Applying the Advancing Excellence in America’s Nursing Homes Circle of Success to improving and sustaining quality. Geriatric Nursing, 34(5), 402–411. doi:10.1016/j.gerinurse.2013.06.011 [DOI] [PubMed] [Google Scholar]
- Beckett P. Field J. Molloy L. Yu N. Holmes D. & Pile E (2013). Practice what you preach: developing person-centred culture in inpatient mental health settings through strengths-based, transformational leadership. Issues in Mental Health Nursing, 34(8), 595–601. doi:10.3109/01612840.2013.790524 [DOI] [PubMed] [Google Scholar]
- Berkowitz R. E. Fang Z. Helfand B. K. Jones R. N. Schreiber R. & Paasche-Orlow M. K (2013). Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility. Journal of the American Medical Directors Association, 14(10), 736–740. doi:10.1016/j.jamda.2013.03.004 [DOI] [PubMed] [Google Scholar]
- Bowers B., Nolet K., Roberts T., & Esmond S (n.d). Implementing Change in Long-Term Care: A Practical Guide to Transformation Retrieved from http://www.pioneernetwork.net/Data/Documents/Implementation_Manual_ChangeInLongTermCare%5B1%5D.pdf
- Bradley E. H. Curry L. A. Ramanadhan S. Rowe L. Nembhard I. M. & Krumholz H. M (2009). Research in action: using positive deviance to improve quality of health care. Implementation Science, 4, 25. doi:10.1186/1748-5908-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caravon P., Hundt A. S., Karsh B., Gurses A. P., Alvarado C. J., Smith M., & Brennan P. F (2006). Work system design for patient safety: the SEIPS model. Quality & Safety in Health Care, 15(Suppl. 1), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle N. G. & Ferguson J. C (2010). What is nursing home quality and how is it measured?The Gerontologist, 50(4), 426–442. doi:10.1093/geront/gnq052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (2013). Nursing Home Quality Care Collaborative: Change package Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/Downloads/NNHQCC-Package.pdf
- Centers for Medicare and Medicaid Services (2014). QAPI Description and Background Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/qapidefinition.html
- Centers for Medicare and Medicaid Services (n.d). QAPI at a Glance: A Step by Step Guide to Implementing Quality Assurance and Performance Improvement (QAPI) in Your Nursing Home Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/Downloads/QAPIAtaGlance.pdf
- Collier E. & Harrington C (2008). Staffing characteristics, turnover rates, and quality of resident care in nursing facilities. Research in Gerontological Nursing, 1(3), 157–170. doi:10.3928/00220124-20091301-03 [DOI] [PubMed] [Google Scholar]
- Gillespie S. M. Olsan T. Liebel D. Cai X. Stewart R. Katz P. R. & Karuza J (2016). Pioneering a nursing home quality improvement learning collaborative: A case study of method and lessons learned. Journal of the American Medical Directors Association, 17(2), 136–141. doi:10.1016/j.jamda.2015.08.014 [DOI] [PubMed] [Google Scholar]
- Gittell J. H. (2011). Supervisory span, relational coordination and flight departure performance. Organization Science, 12(4), 468–483. [Google Scholar]
- Gittell J. H. (2012). New directions for relational coordination theory. In Spreitzer G. M. & Cameron K. S. (Eds.), The Oxford Handbook of Positive Organizational Scholarship (pp. 400–411). [Google Scholar]
- Government Accountability Office (2015). Nursing home quality: CMS should continue to improve data and oversight (GAO-16–33). Washington, DC. [Google Scholar]
- Grabowski D. C., Stevenson D. G., Caudry D. J., O’Malley A. J., Green L. H., Doherty J. A., & Frank R. G (2016). The impact of nursing home pay-for-performance on quality and medicare spending: Results from the nursing home value-based purchasing demonstration. Health Service Research. doi:10.1111/1475–6773.12538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann C. W., Palmer J. A., Mills W. L., Pimentel C. B., Allen R. S., Wewiroski N. J., … Snow A. L (in press). Adaptation of a nursing home culture change research instrument for frontline staff quality improvement use. Psychological Services. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey G. Loftus-Hills A. Rycroft-Malone J. Titchen A. Kitson A. McCormack B. & Seers K (2002). Getting evidence into practice: the role and function of facilitation. Journal of Advanced Nursing, 37(6), 577–588. [DOI] [PubMed] [Google Scholar]
- Jack B. W., Chetty V. K., Anthony D., Greenwald J. L., Sanchez G. M., Johnson A. E.,…, Culpepper L. (2009). A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Annals of Internal Medicine, 150(3), 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan H. C. Brady P. W. Dritz M. C. Hooper D. K. Linam W. M. Froehle C. M. & Margolis P (2010). The influence of context on quality improvement success in health care: a systematic review of the literature. The Milbank Quarterly, 88(4), 500–559. doi:10.1111/j.1468-0009.2010.00611.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurowski A. Buchholz B. & Punnett L; ProCare Research Team (2014). A physical workload index to evaluate a safe resident handling program for nursing home personnel. Human Factors, 56(4), 669–683. doi:10.1177/0018720813509268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton R. Taylor N. Clay-Williams R. & Braithwaite J (2014). Positive deviance: a different approach to achieving patient safety. BMJ Quality & Safety, 23(11), 880–883. doi:10.1136/bmjqs-2014-003115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh D. R. Schroeder D. G. Dearden K. A. Sternin J. & Sternin M (2004). The power of positive deviance. BMJ (Clinical research ed.), 329(7475), 1177–1179. doi:10.1136/bmj.329.7475.1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Inspector General.(2014). Adverse events in skilled nursing facilities: National incidence among Medicare Beneficiaries. Washington, DC. [Google Scholar]
- Ouslander J. G. Bonner A. Herndon L. & Shutes J (2014). The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. Journal of the American Medical Directors Association, 15(3), 162–170. doi:10.1016/j.jamda.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmelee P. A. (2004). Quality improvement in nursing homes: the elephants in the room. Journal of the American Geriatrics Society, 52(12), 2138–2140. doi:10.1111/j.1532-5415.2004.52577.x [DOI] [PubMed] [Google Scholar]
- Phillips J. Hebish L. J. Mann S. Ching J. M. & Blackmore C. C (2016). Engaging frontline leaders and staff in real-time improvement. Joint Commission Journal on Quality and Patient Safety, 42(4), 170–183. [DOI] [PubMed] [Google Scholar]
- Reinhard S., & Stone R (2001). Promoting Quality in Nursing Homes: The Wellspring Model Retrieved from http://www.commonwealthfund.org/usr_doc/reinhard_wellspring_432.pdf
- Rogers E. M. (2003). Diffusion of innovations. New York: Free Press. [Google Scholar]
- Sangl J., Buchanan J., Cosenza C., Bernard S., Keller S., Mitchell N.,…, Larwood D. (2007). The development of a CAHPS instrument for Nursing Home Residents (NHCAHPS). Journal of Aging & Social Policy, 19(2), 63–82. doi:10.1300/J031v19n02_04 [DOI] [PubMed] [Google Scholar]
- Schraagen J. M. Schouten T. Smit M. Haas F. van der Beek D. van de Ven J. & Barach P (2010). Assessing and improving teamwork in cardiac surgery. Quality & Safety in Health Care, 19(6), e29. doi:10.1136/qshc.2009.040105 [DOI] [PubMed] [Google Scholar]
- Smith K. M. Castle N. G. & Hyer K (2013). Implementation of quality assurance and performance improvement programs in nursing homes: a brief report. Journal of the American Medical Directors Association, 14(1), 60–61. doi:10.1016/j.jamda.2012.09.010 [DOI] [PubMed] [Google Scholar]
- Snow A. L., Jacobs-Dodson M. L., Palmer J. A., Parmelee P. A., … Hartmann C. W (in press). Development of a new systematic observation tool of nursing home resident and staff engagement and relationship. The Gerontologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetler C. B., Legro M. W., Rycroft-Malone J., Bowman C., Curran G., Guihan M.,…, Wallace C. M. (2006). Role of “external facilitation” in implementation of research findings: a qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implementation Science, 1, 23. doi:10.1186/1748-5908-1-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone R. I., Reinhard S. C., Bowers B., Zimmerman D., Phillips C. D., Hawes C., … Jacobson N (2002). Evaluation of the Wellspring Model for Improving Nursing Home Quality Retrieved from http://www.commonwealthfund.org/~/media/files/publications/fund-report/2002/aug/evaluation-of-the-wellspring-model-for-improving-nursing-home-quality/stone_wellspringevaluation-pdf.pdf
- Tolson D., Rolland Y., Andrieu S., Aquino J. P., Beard J., Benetos A.,…, Morley J. E; The International Association of Gerontology and Geriatrics/World Health Organization/Society Française de Gérontologie et de Gériatrie Task Force (2011). International Association of Gerontology and Geriatrics: a global agenda for clinical research and quality of care in nursing homes. Journal of the American Medical Directors Association, 12(3), 184–189. doi:10.1016/j.jamda.2010.12.013 [DOI] [PubMed] [Google Scholar]
- Vogt K. Johnson F. Fraser V. Koh J. C. McQueen K. Thornhill J. & Verbowski V (2015). An innovative, strengths-based, peer mentoring approach to professional development for registered dietitians. Canadian Journal of Dietetic Practice and Research, 76(4), 185–189. doi:10.3148/cjdpr-2015-027 [DOI] [PubMed] [Google Scholar]
- Werner R. M. Konetzka R. T. & Kim M. M (2013). Quality improvement under nursing home compare: the association between changes in process and outcome measures. Medical Care, 51(7), 582–588. doi:10.1097/MLR.0b013e31828dbae4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson C. B. & Davies S (2009). Developing relationships in long term care environments: the contribution of staff. Journal of Clinical Nursing, 18(12), 1746–1755. doi:10.1111/j.1365-2702.2008.02748.x [DOI] [PubMed] [Google Scholar]
- Wyatt A. (2010). Getting Better All the Time - Working together for continuous improvement: A guide for nursing home staff. Retrieved from http://www.isabella.org/Isabella/News/Article.aspx?id = cff0ab07-d3b1-4645-a81f-953b1d80337f# [Google Scholar]
- Yanes A. F. McElroy L. M. Abecassis Z. A. Holl J. Woods D. & Ladner D. P (2016). Observation for assessment of clinician performance: a narrative review. BMJ Quality & Safety, 25(1), 46–55. doi:10.1136/bmjqs-2015-004171 [DOI] [PubMed] [Google Scholar]