Abstract
Background
Proficiency-based knot-tying curricula have been developed for square knots for medical students, but, to our knowledge, no such curriculum exists for the reverse half hitch alternating-post (RHAP) knot. We aimed to compare medical students’ knot-tying proficiency, knot-tying self-confidence and final knot characteristics for RHAP and square knots in a simulated deep body cavity.
Methods
We performed a within-subject prospective crossover study of novice medical students who received 30 minutes of training in tying both RHAP and square knots. Participant performance was assessed via a knot-tying checklist, and knot configuration, tensile strength, tightness (loop circumference) and mechanism of failure were also assessed. Participants’ self-reported confidence in knot tying was captured.
Results
Twenty-one students participated in the study. Mean scores on the knot-tying checklist were significantly higher for RHAP knots than for square knots (6.9 [standard deviation (SD) 2.1] v. 5.2 [SD 2.3], p < 0.01), and RHAP knots were significantly tighter than square knots (46.8 mm [SD 0.4 mm] v. 49.3 mm [SD 0.7 mm], p < 0.05). There were no differences between RHAP and square knots in correct knot configuration, breaking strength or mechanism of failure. Reverse half hitch alternating-post knots were easier to tie within a deep-body cavity, whereas square knots were easier to learn.
Conclusion
Novice medical students were more proficient in tying RHAP knots than square knots in a simulated deep body cavity. Students were able to construct RHAP knots more securely and reported increased confidence in tying RHAP knots at depth compared to square knots.
Abstract
Contexte
Des programmes d’enseignement fondés sur la compétence dans l’exécution de noeuds chirurgicaux par les étudiants en médecine ont été créés pour les noeuds plats, mais autant que nous sachions, un tel programme n’existe pas pour le noeud de type demi-clé inversée alternée. Nous avons comparé les aptitudes d’exécution de noeuds et la confiance des étudiants en médecine, ainsi que les caractéristiques des noeuds résultants, pour les noeuds de type demi-clé inversée alternée et les noeuds plats, dans une simulation de cavité profonde.
Méthodes
Nous avons réalisé une étude croisée prospective intra-sujet portant sur des étudiants en médecine débutants, qui ont reçu une formation de 30 minutes sur l’exécution de noeuds de type demi-clé inversée alternée et de noeuds plats. Le travail des participants a été évalué à l’aide d’une liste de vérification d’exécution des noeuds; la configuration des noeuds, la résistance à la traction, le serrage (circonférence de la boucle) et le mécanisme de défaillance ont aussi été évalués. La confiance en soi rapportée par les participants quant à leurs aptitudes d’exécution de noeuds a aussi été examinée.
Résultats
Vingt-et-un étudiants ont pris part à cette étude. Les scores moyens de la liste de vérification d’exécution des noeuds étaient significativement plus élevés pour les noeuds de type demi-clé inversée alternée que pour les noeuds plats (6,9 [écart-type (É.T.) : 2,1] contre 5,2 [É.T. : 2,3], p < 0,01), et les noeuds demi-clé inversée alternée étaient significativement plus serrés que les noeuds plats (46,8 mm [É.T. : 0,4 mm] contre 49,3 mm [É.T. : 0,7 mm], p < 0,05). Aucune différence n’a été observée entre les 2 types de noeuds quant à la configuration, à la résistance à la traction et au mécanisme de défaillance. Les noeuds de type demi-clé inversée alternée étaient plus faciles à nouer dans une cavité profonde, mais la technique des noeuds plats était plus simple à apprendre.
Conclusion
Les aptitudes des étudiants en médecine débutants pour l’exécution de noeuds de type demi-clé inversée alternée étaient supérieures à leurs aptitudes pour l’exécution de noeuds plats, lors d’une simulation de cavité profonde. Les étudiants ont pu réaliser des noeuds de type demi-clé inversée alternée plus solides et ont rapporté une confiance plus grande quant à l’exécution de ce type de noeuds que pour l’exécution de noeuds plats en profondeur.
The ability to construct secure surgical knots is a skill that every medical student should become proficient in by the end of undergraduate medical training. Suturing and knot tying are used in a variety of specialties including surgery, obstetrics and gynecology, family medicine, dermatology and emergency medicine. Undergraduate surgical education curricula have been reported to be not standardized and highly variable, which may preclude the development of technical skills among medical students.1 This learning gap has been reflected among final-year medical students, who reported lacking the desired proficiency for suturing and surgical knot tying.2
Different knot configurations have different strengths, properties, mechanisms of knot failure and holding strength.3 In general surgery, hand ties are often preferred over instrument ties, as force and tension on the suture can be maintained during tying, resulting in more secure knots.4 A square knot, which is the current reference standard, has alternating throws placed parallel on top of one another.5,6 The locking nature of the suture strands in combination with the maximal contact surface area results in a secure knot. However, square knots are difficult to tie within a deep body cavity owing to limited working space and the requirement for the suture strands to be laid flat on top of each other.5,7 We have previously identified and studied the reverse half hitch alternating-post (RHAP) hand-tied knot as an alternative to the hand-tied square knot.8 The RHAP knot is composed of half hitches that are reversed and thrown on suture posts, which alternate between the left and right hand.7,8 The tensile strength and mechanism of failure are similar for RHAP and square knots when tested with multifilament sutures on a flat surface.8 Proficiency-based knot-tying curricula have been developed for square knots for medical students.9 However, to our knowledge, no such curriculum exists for knot tying at depth or for the RHAP knot.
Within a deep body cavity, slip-knots rather than square knots are often used given the limited working space. Surgical slip-knots are constructed by throwing half hitches around 1 standing post, which inevitably results in a knot that is prone to slippage and failure at a lower tension.5,8 We hypothesized that a RHAP surgical knot would be easier to tie, more secure and a superior alternative to a square surgical knot in a simulated deep body cavity. The objective of our study was to compare knot-tying proficiency, self-perceived knot-tying confidence and final knot characteristics for RHAP knots and square knots tied by novice medical students in a simulated deep body cavity.
Methods
Participants
All first-year novice medical students from Queen’s University, Kingston, Ontario, without previous surgical experience in hand tying knots were contacted via email for voluntary participation in a within-subject prospective crossover study. We used a within-subject crossover study design to avoid order bias during training. Participants were excluded if they had previous surgical hand tying experience or had previously participated in a surgical knot-tying course. Written consent was obtained from all participants before beginning the study. This study was approved by the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board and the Queen’s University Undergraduate Medical Education Curriculum Committee.
Sample size
Sample size calculation was based on the smallest effect size reported for our primary outcome measure, the knot-tying checklist score for constructing knots at depth.10 We calculated a sample size of 10 participants per group, assuming an effect size of 1, a 2-tailed 5% type I error and 80% power.
Training
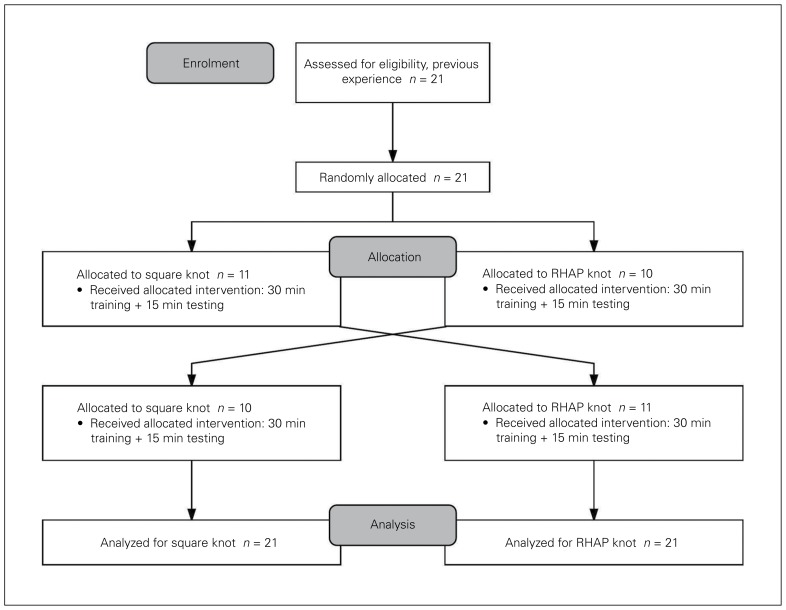
All study participants attended a 1.5-hour training session, with an option to extend the training time to achieve self-perceived knot-tying proficiency. Students were randomly allocated via a simple number generator (http://www.random.org) to 1 of 2 groups (Fig. 1). Group 1 began with 30 minutes of training on the RHAP knot followed by 15-minute assessment of RHAP knot construction in a simulated deep body cavity. Participants in group 1 then crossed over and received 30 minutes of training on square knot construction followed by 15-minute assessment. The same protocol of training and assessment was used for group 2, but starting with square knots rather than RHAP knots. Performance during assessment was video captured.
Fig. 1.
Study design. RHAP = reverse half hitch alternating-post.
The same instructors taught construction of RHAP and square knots using standard instructions.7,8,11 These instructions included a step-by-step guide for 1-handed knot construction on knot-tying training boards (Knot Tying Kit, Ethicon) followed by 1-handed knot construction in a simulated deep body cavity. Silk ties (Perma-Hand, Ethicon), 3–0 gauge, were used for all knots.
Assessment
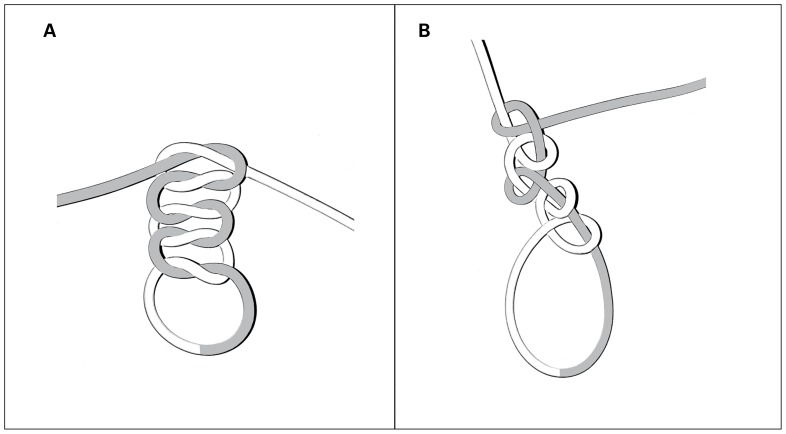
Assessment of knot-tying proficiency was conducted in a simulated deep body cavity (Fig. 2). The simulated cavity was modelled after the knot training board and was constructed from a cardboard cylinder 10 cm in height, with 2 removable pegs embedded 8 cm from the opening. The pegs were 2 cm apart, generating a circumference around the pegs that was 45 mm. Students were asked to tie knots around the 2 pegs — an accepted method in generating a closed loop — to allow for subsequent strength testing of the knot.6,8 Each participant was asked to create 3 knots with 5 throws each during the assessment (Fig. 3). We chose 3 knots based on the evidence for knot-tying proficiency in medical trainees.12,13
Fig. 2.
Schematic of simulated deep cavity set-up.
Fig. 3.
Untightened 5-throw configuration of (A) square knot and (B) reverse half hitch alternating-post knot.
Primary outcome measure
Surgical knot-tying proficiency was the primary outcome measure. It was assessed with a previously validated 5-item surgical knot skills checklist for knot tying at depth (maximum score 10, minimum score 0).10 Assessment focused on the video recording of the third knot — deemed to be most proficient knot in the series — for each study participant.10,13 Each assessment was conducted by 3 blinded independent reviewers (V.W., C.Y. and E.A.S.).
Secondary outcome measures
Secondary outcome measures included the tensile strength of the knot, mechanism of knot failure, knot tightness, knot configuration and participant’s self-confidence in knot tying. We defined the tensile strength of the knot as the tension at which the knot failed, measured in newtons. We measured tensile strength with a static pull machine (ElectroForce 5500, Bose Corporation), using metrics in accordance with accepted methodology.8 A schematic of the static pull machine set-up is illustrated in Fig. 4. We captured the mechanism of knot failure using standard definitions for slippage (> 3 mm of elongation) and breakage.8,14,15 Knot tightness was defined and measured as the circumference of each knot (in millimetres) when it was tied around 2 pegs in the simulated deep body cavity. Knot configuration was assessed by the same 3 independent reviewers as for proficiency using high-powered photographs of knot construction for the third knot tied in each series.16 The images were obtained with an optical zoom lens and then further digitally enhanced, which allowed the reviewers to visualize the actual configuration of the suture strands within the knot. In cases of disagreement, consensus among the reviewers was reached via discussion.
Fig. 4.
Schematic of static pull machine set-up.
After the assessment session, participants completed a 6-item questionnaire assessing the perceived difficulty in tying each knot configuration (Table 1). Participants rated each item using a 10-point Likert scale where 1 = very easy and 10 = very difficult.
Table 1.
Questionnaire items*
| 1. Ease of tying the RHAP knot in the deep cavity |
| 2. Ease of tying the square knot in the deep cavity |
| 3. Ease of tying the RHAP knot on the surface |
| 4. Ease of tying the square knot on the surface |
| 5. Ease of learning the RHAP knot overall |
| 6. Ease of learning the square knot overall |
RHAP = reverse half hitch alternating-post.
Rated on a 10-point Likert scale where 1 = very easy and 10 = very difficult.
Statistical analysis
We used SPSS v. 21 (IBM Corp.) for all statistical analysis, with significance set to p < 0.05. Results are reported as mean and standard deviation (SD) for normally distributed data, and median and interquartile range (IQR) for skewed data. We performed simple descriptive statistics for the primary and secondary outcomes. We used paired t tests to compare scores for knot-tying proficiency, knot strength and knot tightness, and the Wilcoxon signed-rank test to compare questionnaire results. We used the Fisher exact test to compare the mechanism of knot failure (proportion of slipped knots and broken knots) between RHAP and square knot variations, as well as to compare differences in the structure and configuration of the 2 knots. We calculated the intraclass correlation coefficient using a 2-way mixed-effects model to assess the interrater reliability of reviewer scores from the knot-tying proficiency checklist.
Results
Twenty-one first-year medical students (12 women and 9 men) participated in the study. They created a total of 126 knots. All study participants completed the training and assessment sessions without requiring additional time. The response rate for the 6-item questionnaire was 100%.
Knot-tying proficiency was significantly higher for RHAP knots than for square knots (mean score 6.9 [SD 2.1] v. 5.2 [SD 2.3], p < 0.01). The participants constructed RHAP knots correctly 57.1% of the time, compared to 33.3% of the time for square knots (p = 0.2). The interrater reliability for the knot-tying proficiency checklist was excellent (intraclass correlation coefficient 0.78 (95% confidence interval 0.70–0.86), p < 0.01).
There was no difference in maximal tensile strength between RHAP knots and square knots (18.2 N [SD 0.3 N] v. 17.8 N [SD 0.3 N], p = 0.3). There was no difference in frequency of slippage of RHAP knots and square knots (38.1% v. 47.6%, p = 0.8). Reverse half hitch alternating-post knots were significantly tighter (by 5.1%) than square knots (46.8 mm [SD 0.4 mm] v. 49.3 mm [SD 0.7 mm], p < 0.05).
The questionnaire results are illustrated in Fig. 5. Participants reported that RHAP knots were significantly easier to tie in a deep body cavity than square knots (median rating 5 [IQR 3–7] v. 6 [IQR 5–7], p < 0.05). Participants did not have a preference for either the RHAP knot or the square knot when tied on a surface (median rating 3 [IQR 2–6] v. 3 [IQR 2–5], p = 0.1). Participants reported that, overall, RHAP knots were more difficult to learn than square knots (median rating 6 [IQR 4–7] v. 4 [IQR 3–6], p < 0.05).
Fig. 5.
Mean ratings of difficulty (1 = very easy, 10 = very difficult) for tie at depth, tie on surface and ease of learning of reverse half hitch alternating-post (RHAP) knot and square knot. Error bars = standard deviation.
Discussion
In the current study, the proficiency score for knot tying in a deep body cavity was significantly higher for RHAP knots than for square surgical knots. Students who score higher on the knot-tying proficiency checklist have been shown to have more experience, improved performance and increased readiness for the operating room based on experts’ opinions.10 The ability to tie knots at depth has also been correlated with a student’s global knot-tying performance, which includes tying on a flat surface and tying atraumatic knots.10 The ability of novice medical students to achieve significantly higher proficiency with the RHAP knot than with the square knot implies the potential utility of the former as a more reproducible knot in deep body cavities. Selecting a knot that can be repeatedly and correctly constructed in a deep body cavity has the potential to improve the clinical outcomes of patients, as failure of knots can directly contribute to severe, life-threatening postoperative complications.16–20
An effective surgical knot must have both knot security and loop security.21 Our study design quantified the mechanism of knot failure and the microscopic knot configuration as proxies for knot security. Loop security was measured as the circumference of the suture loop.22,23 The RHAP knots had a significantly smaller loop circumference than the square knots. The inherent challenge in constructing a square knot may contribute to the difficulty for novice medical students to achieve a small loop circumference. When suture tension is not maintained on the first throw in a square knot, the second throw locks the first throw before all the slack is taken out of the suture loop, resulting in a loose suture loop or an “air knot.”21 Alternatively, when the suture tension is applied unevenly between the 2 strands of an attempted square knot, a slip-knot occurs.7 This slip-knot may initially be a “nonair knot” but may become loose as soon as it starts to slip under tension.16 In comparison, the RHAP knot consists of sequentially stacked throws, which can be pushed down a post strand without allowing the suture loop to become lax. Previous analogies for the RHAP knot have been made to holding one’s finger on the first throw of a shoelace to prevent slippage while tying the second throw.21 Loop security is a clinically important factor for the successful approximation of tissue, as the lack of knot security may result in loss of tissue fixation.21,24,25 The RHAP knot allows for construction of a loop with a smaller circumference, which may correlate with decreased knot failure in the clinical context; this remains to be shown.
We found that the proportion of knots with correct configuration, the mechanism of failure and the tensile breaking strength were not significantly different between RHAP and square knots. Ching and colleagues16 assessed knot tying by medical students without specific training and found that only a minority (8%) were able to repeatedly reconstruct square knots. In our study, a higher proportion of medical students (33%) were able to construct square knots with proper configuration. This discrepancy may be a result of the formal training provided in our study and the requirement for medical students to achieve self-perceived competency before summative assessment. To ensure proficiency in RHAP knot tying for all novice medical students, a competency-based training curriculum should be developed and implemented based on previously published evidence-based frameworks.9,26
Our finding of no difference between the mechanism of knot failure and tensile breaking strength between RHAP and square knots is not surprising. From the standpoint of physical properties, it appears that the mechanism of failure for the 2 types of knot is identical. We have shown previously that both RHAP and square knots constructed correctly with 5 throws on flat surfaces have similar tensile strength and do not slip.8 In the current study, our participants were asked to produce knots with 5 throws, thus minimizing the likelihood of knot slippage with proper knot construction. As such, knot failure was likely due to intraparticipant inconsistencies in knot construction and the inherent difficulty in tying the knots at depth.8,16 Our results suggest that RHAP knots can be used instead of square knots for knot tying in a deep body cavity.
The participants reported that RHAP knots were significantly easier to tie than square knots within a deep body cavity. Knot tying at depth requires more time and greater attention to proper hand positioning than tying on a surface.10,27 The participants’ self-reported confidence scores suggest that the RHAP knot is a rational alternative to the square knot within a deep cavity, as they can be easily applied in cavities and areas of limited working space.7,8 It is important to note, however, that self-reported confidence may not reflect actual performance in the clinical environment.28,29 Future studies will examine the relation between proficiency of knot tying in a simulation laboratory and performance in the clinical setting.
Limitations
There are limitations of our study. First, only 1 type of suture material was used, which limits the generalizability of our findings to other suture materials. Each suture material has a different mechanism of failure and ease of knot construction.8 Using different suture materials for future studies may improve the generalizability of the results. Second, rater bias may have been introduced during assessments of videos of knot tying for RHAP and square knots. Given the study design, it was not possible to blind the reviewers to the knot type they were assessing owing to the inherent difference in the configuration and construction of the knots. Third, baseline assessment of knot-tying proficiency was not performed. However, as we recruited only novice medical students without previous surgical hand tying experience or knot-tying training, we expect that all participants had a similar baseline. Last, surgical residents were not recruited as study participants owing to potential bias stemming from added familiarity of tying square knots.
Conclusion
Novice medical students were more proficient in tying RHAP knots than square knots in a simulated deep body cavity. Participants were able to construct RHAP knots more securely and reported increased confidence in tying this type of knot at depth compared to square knots. Together, these findings suggest that the RHAP knot may be more reproducible than the square knot within a deep body cavity. Future directions for research include 1) testing the security of knots by examining the burst pressures for vascular ligatures in the laboratory, 2) quantifying the proportion and extent of loose knots constructed by novice trainees by following a previously published format on vessel ligation training via an adaptive simulation curriculum30,31 and 3) performing a validation study of proficiency in tying the RHAP knot among surgical residents.
Acknowledgements
The authors thank Wilma Hopman for her contribution to the statistical analysis. The authors also thank Zuhaib Mir and Guy Sheahan for their time in teaching medical students surgical knot tying.
Footnotes
Competing interests: None declared.
Funding: Department of Surgery, Queen’s University, Kingston, Ont.
Contributors: V. Wu, E. Sykes and B. Zevin designed the study. V. Wu, C. Yeung and E. Sykes acquired the data, which all authors analyzed. V. Wu and C. Yeung wrote the article, which all authors reviewed and approved for publication.
References
- 1.Forbes SS, Fitzgerald PG, Birch DW. Undergraduate surgical training: variations in program objectives and curriculum implementation across Canada. Can J Surg. 2006;49:46–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Dehmer JJ, Amos KD, Farrell TM, et al. Competence and confidence with basic procedural skills: the experience and opinions of fourth-year students at a single institution. Acad Med. 2013;88:682–7. doi: 10.1097/ACM.0b013e31828b0007. [DOI] [PubMed] [Google Scholar]
- 3.Marturello DM, McFadden MS, Bennett RA, et al. Knot security and tensile strength of suture materials. Vet Surg. 2014;43:73–9. doi: 10.1111/j.1532-950X.2013.12076.x. [DOI] [PubMed] [Google Scholar]
- 4.Farquharson M, Hollingshead J, Moran B, editors. Farquharson’s textbook of operative general surgery. 10th ed. Boca Raton (FL): CRC Press; 2015. [Google Scholar]
- 5.Van Rijssel EJ, Trimbos JB, Booster MH. Mechanical performance of square knots and sliding knots in surgery: comparative study. Am J Obstet Gynecol. 1990;162:93–7. doi: 10.1016/0002-9378(90)90828-u. [DOI] [PubMed] [Google Scholar]
- 6.Trimbos JB. Security of various knots commonly used in surgical practice. Obstet Gynecol. 1984;64:274–80. [PubMed] [Google Scholar]
- 7.Gunderson PE. The half-hitch knot: a rational alternative to the square knot. Am J Surg. 1987;154:538–40. doi: 10.1016/0002-9610(87)90273-x. [DOI] [PubMed] [Google Scholar]
- 8.Wu V, Sykes EA, Mercer D, et al. Comparing the tensile strength of square and reversing half-hitch alternating post knots. Can J Surg. 2017;60:179–85. doi: 10.1503/cjs.009716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim EH, Chern H, Huang E, et al. How to teach knot tying: a kinesthetic approach. MedEdPORTAL. 2013 Jan 30; doi: 10.15766/mep_2374-8265.9328. [DOI] [Google Scholar]
- 10.Huang E, Vaughn CJ, Chern H, et al. An objective assessment tool for basic surgical knot-tying skills. J Surg Educ. 2015;72:572–6. doi: 10.1016/j.jsurg.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Dunn DL. Wound closure manual. Somerville (NJ): Ethicon; 2007. [Google Scholar]
- 12.Tytherleigh MG, Bhatti TS, Watkins RM, et al. The assessment of surgical skills and a simple knot-tying exercise. Ann R Coll Surg Engl. 2001;83:69–73. [PMC free article] [PubMed] [Google Scholar]
- 13.Pender C, Kiselov V, Yu Q, et al. All for knots: evaluating the effectiveness of a proficiency-driven, simulation-based knot tying and suturing curriculum for medical students during their third-year surgery clerkship. Am J Surg. 2017;213:362–70. doi: 10.1016/j.amjsurg.2016.06.028. [DOI] [PubMed] [Google Scholar]
- 14.Muffly TM, Boyce J, Kieweg SL, et al. Tensile strength of a surgeon’s or a square knot. J Surg Educ. 2010;67:222–6. doi: 10.1016/j.jsurg.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lo IK, Ochoa E, Jr, Burkhart SS. A comparison of knot security and loop security in arthroscopic knots tied with newer high strength suture materials. Arthroscopy. 2010;26(9 Suppl):S120–6. doi: 10.1016/j.arthro.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Ching SS, Mok CW, Koh YX, et al. Assessment of surgical trainees’ quality of knot-tying. J Surg Educ. 2013;70:48–54. doi: 10.1016/j.jsurg.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Hsu JL, Korndorffer JR, Jr, Brown KM. Force feedback vessel ligation simulator in knot-tying proficiency training. Am J Surg. 2016;211:411–5. doi: 10.1016/j.amjsurg.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Zhao C, Hsu CC, Moriya T, et al. Beyond the square knot: a novel knotting technique for surgical use. J Bone Joint Surg Am. 2013;95:1020–7. doi: 10.2106/JBJS.K.01525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ketchum LD. Suture materials and suture techniques used in tendon repair. Hand Clin. 1985;1:43–53. [PubMed] [Google Scholar]
- 20.Tera H, Aberg C. Tissue strength of structures involved in musculoaponeurotic layer sutures in laparotomy incisions. Acta Chir Scand. 1976;142:349–55. [PubMed] [Google Scholar]
- 21.Burkhart SS, Wirth MA, Simonick M, et al. Loop security as a determinant of tissue fixation security. Arthroscopy. 1998;14:773–6. doi: 10.1016/s0749-8063(98)70110-0. [DOI] [PubMed] [Google Scholar]
- 22.Song Z, Wang GH, Sun LL, et al. Comparative study of surgical knots using a domestically produced Chinese surgical robot, laparoscope, or barehanded approach. Int J Med Robot. 2017;13 doi: 10.1002/rcs.1794. Epub 2016 Dec 20. [DOI] [PubMed] [Google Scholar]
- 23.Lo IK, Burkhart SS, Chan KC, et al. Arthroscopic knots: determining the optimal balance of loop security and knot security. Arthroscopy. 2004;20:489–502. doi: 10.1016/j.arthro.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Burkhart SS, Wirth MA, Simonich M, et al. Knot security in simple sliding knots and its relationship to rotator cuff repair: How secure must the knot be? Arthroscopy. 2000;16:202–7. doi: 10.1016/s0749-8063(00)90037-9. [DOI] [PubMed] [Google Scholar]
- 25.Mishra DK, Cannon WD, Jr, Lucas DJ, et al. Elongation of arthroscopically tied knots. Am J Sports Med. 1997;25:113–7. doi: 10.1177/036354659702500122. [DOI] [PubMed] [Google Scholar]
- 26.Zevin B, Levy JS, Satava RM, et al. A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg. 2012;215:580–6. doi: 10.1016/j.jamcollsurg.2012.05.035. [DOI] [PubMed] [Google Scholar]
- 27.Brydges R, Classen R, Larmer J, et al. Computer-assisted assessment of one-handed knot tying skills performed within various contexts: a construct validity study. Am J Surg. 2006;192:109–13. doi: 10.1016/j.amjsurg.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Zevin B. Self versus external assessment for technical tasks in surgery: a narrative review. J Grad Med Educ. 2012;4:417–24. doi: 10.4300/JGME-D-11-00277.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Panait L, Larios JM, Brenes RA, et al. Surgical skills assessment of applicants to general surgery residency. J Surg Res. 2011;170:189–94. doi: 10.1016/j.jss.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 30.Hu Y, Goodrich RN, Le IA, et al. Vessel ligation training via an adaptive simulation curriculum. J Surg Res. 2015;196:17–22. doi: 10.1016/j.jss.2015.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu Y, Le IA, Goodrich RN, et al. Construct validation of a cost-effective vessel ligation benchtop simulator. J Surg Educ. 2015;72:381–6. doi: 10.1016/j.jsurg.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]