Abstract
Background
Ulnar-sided wrist pain at the dorsal proximal triquetrum, especially during wrist pronation, flexion and radial deviation, is common in athletes, particularly ice hockey players. The purpose of this study was to evaluate in which position the dorsal ulnotriquetral ligament (DUTL) is placed under the greatest strain, the torque to failure and the injury pattern. We hypothesized that the DUTL is maximally strained with wrist flexion, pronation and radial deviation, and that, at failure, the ligament tears off the triquetrum.
Methods
We performed a biomechanical study on 7 fresh frozen cadaveric upper extremities, with testing done on a wrist-movement stimulator to identify the position (45° of wrist flexion, 45° of wrist extension or neutral) that generated the highest and earliest strain increases in the DUTL. We performed load-to-failure testing, characterized the ligament’s pattern of failure, and repaired and retested the DUTL using the same load-to-failure protocol.
Results
The DUTL reached 3 N·m the earliest in 45° of wrist flexion (p = 0.02). The native DUTL failed at 0.35 N·m (standard deviation [SD] 0.13 N·m) per degree of angular stiffness, 12.93 N·m of yield strength and with angular deformation of 57.73° (SD 20.62°). There was no significant difference in these variables between the native and repaired DUTL. Tearing occurred at a mean of 10 mm (SD 2 mm) proximal from the triquetrum’s insertion in a transverse midsubstance pattern.
Conclusion
This study showed a reproducible pattern of injury to the DUTL in a cadaveric model. Additional work is needed to further characterize the pathoanatomy of “hockey wrist.”
Abstract
Contexte
La douleur cubitale au poignet, au niveau du triquetrum proximal dorsal, surtout à la pronation, à la flexion et à la déviation radiale du poignet, est fréquente chez les athlètes, particulièrement chez les joueurs de hockey. Le but de cette étude était d’évaluer la position dans laquelle le ligament ulnotriquétral dorsal (LUTD) est soumis à la pression la plus grande, le couple de torsion menant à la défaillance et le mode de blessure. Selon notre hypothèse, le LUTD est soumis au maximum de pression lorsque le poignet est en flexion, pronation et déviation radiale, et au moment de la défaillance, le ligament ulnotriquétral se déchire.
Méthodes
Nous avons procédé à une étude biomécanique sur 7 membres supérieurs de cadavres frais congelés, et effectué des tests sur un stimulateur de mouvements du poignet pour établir la position (flexion du poignet à 45°, extension du poignet de 45° ou position neutre) générant les augmentations de pression les plus fortes et les plus rapides sur le LUTD. Nous avons procédé à des tests de mise en charge jusqu’à défaillance, caractérisé le mode de défaillance du ligament et réparé et retesté le LUTD à l’aide du même protocole de mise en charge jusqu’à défaillance.
Résultats
Le LUTD a atteint 3 N·m le plus rapidement avec une flexion du poignet à 45° (p = 0,02). Le LUTD natif a connu une défaillance à 0,35 N·m (écart-type [É.-T.] 0,13 N·m) par degré de raideur angulaire, 12,93 N·m d’élasticité et avec une déformation angulaire de 57,73° (É.-T. 20,62°). On n’a noté aucune différence significative de ces variables entre les LUTD natifs et réparés. La déchirure s’est produite en moyenne à 10 mm (É.-T. 2 mm) en proximal par rapport à l’insertion du triquetrum selon un trajet transverse affectant la moitié de la substance ligamentaire.
Conclusion
L’étude a démontré un mode reproductible de lésion du LUTD à l’aide d’un modèle cadavérique. Il faudra approfondir la recherche pour caractériser avec plus de précision l’anatomopathologie de la lésion au poignet typiquement causée par la pratique du hockey.
The wrist joint has a complex anatomy, with multiple structures acting as primary and secondary stabilizers. Intrinsic ligaments originate and insert on carpal bones, whereas extrinsic ligaments connect the carpal bones to the distal radius or ulna and have an important role in carpal stability and alignment.1 Thus, lesions to these ligaments may lead to functional disability and wrist pain.2,3
Ulnar-sided wrist pain is challenging to treat owing to the fact that numerous disorders may present with similar symptoms.4,5 Taneja and colleagues6 reported that the dorsal ulnotriquetral ligament (DUTL) was injured in 71% of cases involving a triquetrum fracture, 36% of those with distal radius fractures, 50% of those with ulna fractures and all those with lunate fractures. Moreover, Chen and Tang7 showed that forearm rotation affects wrist biomechanics and ulnar carpal ligament length. Indeed, the volar ulnotriquetral ligament decreased in length from neutral rotation to pronation and lengthened when brought into supination. At this time, the gold standards for the analysis of wrist ligament problems are magnetic resonance imaging arthrography (MRI-A) and arthroscopic surgery.5
We have treated elite ice hockey players with ulnar-sided wrist pain of various known causes. However, there remains a subset of players with ongoing or recurrent wrist pain that does not fit with any of the known injuries to this area. Indeed, many players present with pain reproduced with direct palpation distal to the triangular fibrocartilage complex near the dorsal/proximal aspect of the triquetrum and/or a manoeuvre combining pronation, flexion and radial deviation of the wrist. We believe that the source of ulnar-sided pain in these athletes is related to injuries to the DUTL. We posit that, since the proximal hand on the hockey stick is often held in flexion–pronation (Fig. 1), when combined with a torque to the wrist in radial deviation (particularly with the long moment arm of the hockey stick), injuries to the DUTL, or “hockey wrist,” can occur. This combination of wrist positions and forces can also take place in other sports such as golf, and, although not specifically described, DUTL injuries are also potentially possible.8–10 Thus, obtaining the correct diagnosis for ulnar-sided wrist pain, specifically DUTL disruption, is of utmost importance for patients, since this easily overlooked injury may affect the treatment and outcome.
Fig. 1.
Top hand on hockey stick held in flexion and pronation.
The purpose of this biomechanical study was to 1) determine in which position of wrist movement the DUTL was placed in greatest strain, 2) evaluate the ligament’s torque to failure and 3) characterize the type of ulnotriquetral ligament injury created by our model. We believe that DUTL injuries are often unreported or overlooked on imaging studies and may cause chronic ulnar-sided wrist pain. We hypothesized that the DUTL is maximally strained with the wrist placed in flexion, the forearm in pronation and moving from ulnar to radial deviation, and that, at failure, the DUTL tears off the triquetrum in this position.
Methods
Based on our recurring clinical, radiographic and surgical observations, we established a cadaveric biomechanical model to determine the strain patterns in the structures present on the ulnar side of the wrist, particularly the DUTL, under various loading conditions. Ethics committee and institutional review board approval were obtained.
The study was performed on 7 fresh frozen adult upper extremities (proximal radio-ulnar joint to the hand distally) from 6 male donors and 1 female donor (mean age 69.5 yr [range 55–86 yr]); there were 3 right and 4 left wrists. We based the sample size determination on previous cadaveric biomechanical studies available in the literature and power analysis for paired statistical tests, assuming a large effect size, α = 0.05 and power of 0.80. Each specimen was thawed at room temperature (mean 21°C [standard deviation (SD) 3°]) overnight before testing.
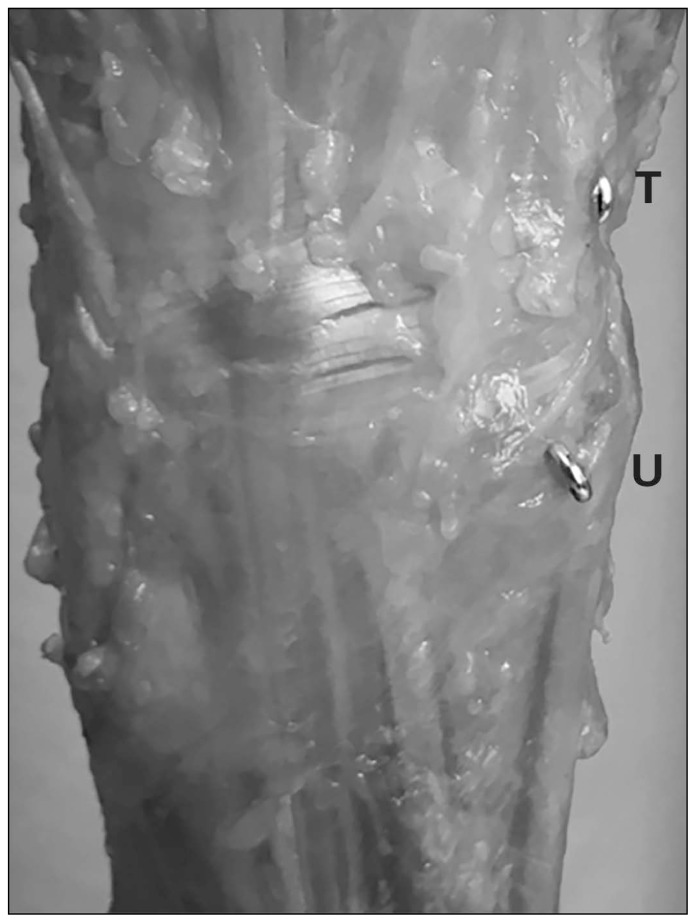
A fellowship-trained musculoskeletal radiologist (M.B.) completed preintervention high-resolution ultrasonography on each specimen to evaluate the DUTL integrity in various wrist positions and to potentially exclude specimens with any underlying disorder. No specimens were excluded. Subsequently, a 1-mm screw eyelet was inserted under ultrasonography guidance at the origin, the ulnar styloid and the insertion (dorsal triquetrum) of the DUTL (Fig. 2).
Fig. 2.
Screw eyelets inserted at origin and insertion of dorsal ulnotriquetral ligament. T = triquetrum; U = ulna.
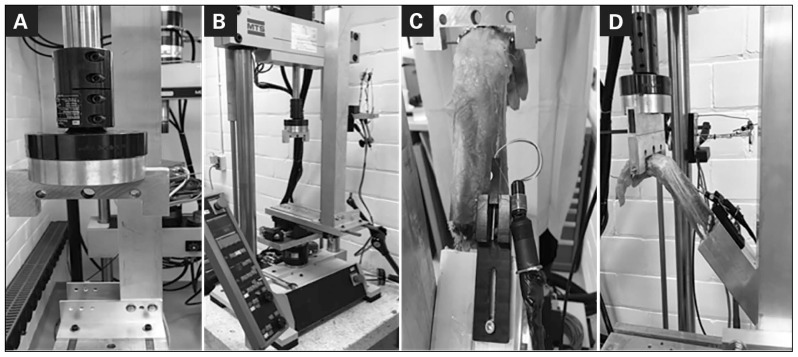
We performed load-to-failure analysis of the specimens using a custom set-up on a Servo Kinetics hydraulic testing machine (MTS 858 Mini Bionix). The specimens were prepared by dissecting the soft tissues from the proximal 10 cm of the forearm. The forearms were then placed in maximal pronation and secured in this position by inserting a pin through the proximal radius and ulna. We chose this position since it has been shown that the DUTL complex is under tension in pronation and relaxed in supination.11 Subsequently, the dissected part of the forearm was placed in an aluminum box and securely cemented in place. While longitudinal traction was maintained through the wrist, a threaded rod was placed into the second to fourth metacarpals, parallel to the wrist’s articulation. A linear motion potentiometer (LCP8ST-10–10K, State Electronics) was installed on the aluminum box, and a monofilament string was attached to it after being passed through the eyelets. Then, the specimens were mounted to the simulator by inserting the metacarpal pins to an inverted U-shaped metallic frame attached to the MTS machine and securing the box containing the forearm with clamps on a metallic post placed on the sliding table (Fig. 3).
Fig. 3.
Custom wrist-movement simulator. (A) Anterior view of U-shaped frame attached to MTS 858 Mini Bionix machine. (B) Posterior view of simulator. (C) Posterior view of forearm mounted on simulator. (D) Lateral view of forearm mounted on simulator.
Initially, all specimens were tested in randomized fashion in 3 positions (45° of wrist flexion, 45° of wrist extension and neutral) to evaluate which position generated the highest and earliest increases in strain in the DUTL. The MTS machine moved the wrist from neutral wrist deviation toward radial deviation. A nondestructive constant torque of 0.05 N·m/s was applied to the wrist until 3 N·m was obtained. The degrees of wrist deviation were measured throughout testing. The position in which the DUTL became taut first was used for subsequent destructive load for failure testing.
Based on the results of nondestructive testing, each specimen was positioned with the wrist in 45° of flexion on the simulator with the pronated position maintained. A constant torque was applied to the wrist, moving from neutral toward radial deviation at 0.5°/s until failure of the DUTL, which was observed as a sudden decrease in the torque applied and/or an audible sound suggesting a tear in the ligament. The data on strain patterns and ultimate load to failure were collected. After load-to-failure testing was completed, the specimens were again scanned by the same radiologist to confirm the injury to the DUTL. Subsequently, careful dissection was done on the ulnar side of the wrist to evaluate the DUTL integrity. The tear was then repaired by means of a suture anchor (JuggerKnot Soft Anchor 1.0 mm Mini, Zimmer Biomet) placed into the triquetrum insertion site. The specimens were then retested with the wrist in 45° of flexion until failure of the repaired DUTL. The torque and the degrees of displacement were recorded continuously.
Statistical analysis
We used analysis of variance to determine in which wrist position (45° of flexion, 45° of extension or neutral) the DUTL was the tautest in order to select the appropriate wrist position to be tested for load-to-failure analysis. We used paired Student t tests to assess the differences between the native state and the repaired state of the DUTL in all specimens for the yield strength of the maximal torque at failure, the angular deformation at yield strength at failure and the angular stiffness, from the torque/angle results obtained. A p value < 0.05 was considered statistically significant. Statistical analysis was performed with SPSS software (IBM Corp.) and was reviewed by a biomedical statistician.
Results
The mean degree of radial deviation obtained in the specimens for each wrist position tested was 24.9° for 45° of wrist flexion, 36.4° for neutral wrist position and 33.4° for 45° of wrist extension (p = 0.02) (Table 1). Thus, the wrist at 45° of flexion was the position in which the DUTL became taut the fastest and reached 3 N·m the earliest.
Table 1.
Degree of radial deviation obtained at 3 N·m of torque for wrist positions of 45° flexion, neutral and 45° extension
| Specimen no. | Side | Testing order | Wrist position; radial deviation, °* | ||
|---|---|---|---|---|---|
| 45° flexion | Neutral | 45° extension | |||
| 1 | Left | Flexion/extension/neutral | 32.2 | 31.4 | 22.5 |
| 2 | Right | Extension/flexion/neutral | 16.9 | 25.4 | 19.9 |
| 3 | Left | Extension/flexion/neutral | 12.6 | 33.5 | 36.6 |
| 4 | Right | Flexion/neutral/extension | 9.1 | 38.1 | 30.11 |
| 5 | Left | Extension/neutral/flexion | 28.9 | 45.5 | 39.5 |
| 6 | Right | Neutral/extension/flexion | 32.5 | 34.9 | 34.5 |
| 7 | Left | Neutral/flexion/extension | 41.9 | 46.3 | 50.4 |
| Mean | — | — | 24.9 | 36.4 | 33.4 |
p = 0.02, analysis of variance.
The native DUTL failed at 0.35 N·m (SD 0.13 N·m) per degree of angular stiffness, 12.93 N·m of yield strength and with angular deformation of 57.73° (SD 20.62°). The torque–angle data showed no significant difference between the native and the repaired DUTL in angular stiffness, yield strength or angular deformation at yield (Table 1). The mean results obtained for the 2 ulnotriquetral ligament states for each variable are presented in Table 2.
Table 2.
Comparison of load-to-failure results for native and repaired dorsal ulnotriquetral ligaments
| Variable | Mean ± SD n = 7 |
p value |
|---|---|---|
| Angular stiffness, N·m/ ° | ||
| Native | 0.35 ± 0.13 | 0.8 |
| Repaired | 0.34 ± 0.11 | |
| Yield strength, N·m | ||
| Native | 12.93 ± 5.20 | 0.3 |
| Repaired | 12.22 ± 5.14 | |
| Angular deformation at yield, ° | ||
| Native | 57.73 ± 20.62 | 0.4 |
| Repaired | 60.29 ± 22.79 | |
SD = standard deviation.
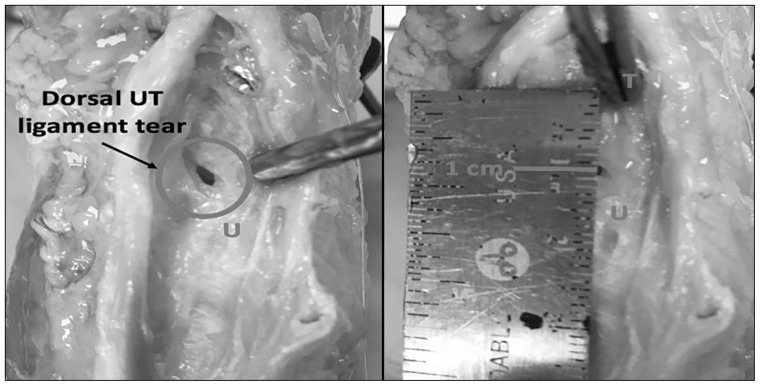
Anatomic assessment showed that, in all specimens, the tear occurred in a consistent pattern at a mean of 10 mm (SD 2 mm) proximal from the insertion on the triquetrum in a transverse midsubstance pattern (Fig. 4).
Fig. 4.
Dorsal ulnotriquetral (UT) ligament tear (arrow) 1 cm proximal from triquetrum. T = triquetrum; U = ulna.
Discussion
The DUTL was first described by Sasao and colleagues11 in 2003 as being a ligament and structure distinct from the ulnar collateral ligament and the extensor carpi ulnaris subsheath. They observed that the DUTL origin and insertion were the styloid process of the ulna and the dorsal aspect of the triquetrum, respectively. Boutry and colleagues12 evaluated the wrist’s ligaments using ultrasonography and reported the thickness of the DUTL to be 1.9 mm (SD 0.6 mm). The DUTL was also described by Lacelli and colleagues13 as originating from the ulna and inserting on the dorsal–ulnar aspect of the triquetrum and having a mean thickness of 2.2 mm (SD 0.5 mm).
Wrist position and forearm rotation influence the kinematics of the wrist joint, as well as the carpal bones. These biomechanical changes are in part due to the different amounts of ligament tension throughout the arc of movement. Becce and colleagues14 evaluated the association of dorsal triquetrum fractures and dorsal carpal ligament injuries using wrist MRI. They found that, in the injured wrist, 81% of dorsal triquetrum fractures were associated with DUTL tears. Moreover, they described the mean thickness of the DUTL at the insertion of the triquetrum in the control (uninjured) group to be 3.5 mm (SD 0.6 mm).
It has been shown that the length of the volar ulnotriquetral ligament varies up to 10%–15% during forearm rotation, with shortening of the ligament in pronation and lengthening in supination.7 Tan and colleagues15 looked at in vivo changes in carpal ligament length during wrist movement from neutral to maximal extension. The palmar ulnotriquetral ligament elongated significantly, by 9%, when the wrist moved from neutral to full extension and by 12% from maximal extension to maximal extension with 10° of radial deviation. Moritomo and colleagues16 observed how the triquetrum rotates dorsally when the wrist moves from flexion to extension, with palmar ulnotriquetral ligament elongation of 1.4 mm (SD 1.5 mm), and shortening of 2.2 mm (SD 1.5 mm) when the movement is reversed. The greatest tension found on the palmar ulnotriquetral ligament was when the wrist was placed in extension/radial deviation, such as in a dart-throwing movement, with an increased ligament length of 3.0 mm (SD 1.7 mm). Currently, there is a lack of literature on the DUTL, with most studies describing the palmar ulnotriquetral ligament. However, these previous descriptions of the volar ulnotriquetral ligament seem to extrapolate well to the opposing findings in our study about the DUTL. We found that the DUTL was placed under greatest tension with wrist flexion, radial deviation and forearm in pronation. The mean yield strength observed on the native DUTL was 12.93 N·m. Daily occupational activities, such as opening a jar or using hand tools, require good power grip strength and endurance for wrist torque tasks.17 To put this into perspective, it has been shown that, for male industrial workers, the mean torque for ulnar deviation wrist tasks and hand-grip tasks necessitating power grip strength is 14.76 N·m (SD 5.66 N·m) and 73.80 N·m (SD 14.97 N·m), respectively.18 Carse and colleagues19 developed a load-measuring device that evaluated the forces applied when opening a jar. They compared the torque needed to open a jar lid in young adults (mean age 26 yr) versus older adults (mean age 77 yr) and found similar results, with maximal torque values of 2.84 N·m and 2.88 N·m, respectively. However, there is a lack of research describing the wrist torque needed for athletes to accomplish their sport-specific tasks and what torque can be withstood before injury occurs. It is also difficult to clinically correlate the values obtained in our experiment, since only the static stabilizers were analyzed, and an important portion of dynamic stabilization of the wrist occurs through muscle function. Moreover, even though the literature seems to show similar results in the general population for the torque applied during functional tasks such as opening a jar lid, further studies are needed to clinically evaluate the torque applied to the wrist, especially for the athletic population.
Grip strength is influenced by wrist position, and it has been shown that maximal grip strength is obtained with the wrist in 35° of extension combined with 7° of ulnar deviation, with significant decrease in strength in any other wrist position.20 Grip strength plays an important role in the success of athletes participating in stick or racquet sports. Indeed, these sports require repeated axial and rotational loads to the wrist and are often associated with ulnar-sided wrist pain.10 Consequently, we believe that the position of the proximal hand on the stick in ice hockey, which is typically held in flexion and pronation, is thus at a mechanical disadvantage and also not in a position to allow significant dynamic muscular stabilization of the wrist. Therefore, the static restraints provided by the DUTL can easily be overwhelmed in this position, leading to injury (i.e., hockey wrist). In addition, the forces acting on the DUTL in this position of maximal strain are amplified by the moment arm of the hockey stick, which likely places even more supraphysiological stress on the DUTL.
The most common diagnoses reported for ulnar-sided wrist pain are injuries to the extensor carpi ulnaris, triangular fibrocartilage complex injuries and distal radioulnar joint instability.10,21,22 Mölsä and colleagues23 observed that 31% of injuries in ice hockey players are located in the upper extremity, with 45% of these injuries distributed to the hand or wrist, which may be due to repetitive micro-trauma or to external factors such as a stick blow, puck impact, board collision or being checked. In golf, it has been described that wrist injuries most commonly occur in the leading wrist, which is typically the nondominant extremity and is placed proximally near the end of the club, whereas the trailing wrist is placed distally.22 Indeed, Hawkes and colleagues22 described how the leading wrist moves from ulnar deviation to radial deviation and back to ulnar deviation during a swing, while the trailing wrist moves from neutral, extension and flexion during the movement. The leading-wrist movement in combination with the moment arm of the golf club, high swing speeds and ground impact is also a “perfect storm” for sustaining a DUTL injury.
We observed localized DUTL tears about 1 cm from the triquetrum insertion in a transverse pattern, rather than a distal avulsion tear as initially hypothesized, that were consistent in all of our specimens. We believe that the DUTL pattern of tear eventually causes a thickening of this structure and later progresses to focal synovitis of the ulnar side of the wrist, with subsequent triquetral bone erosion. This could explain the dorsal–ulnar pain on palpation of the triquetrum in many ice hockey players who present with ulnar-sided wrist symptoms.
When we analyzed the graphs containing the torque–angle and displacement per degree results, the curves did not present as we would have expected, in the classic stress–strain distribution shape. Rather, at yield strength in the torque–angle distribution and at yield angle in the displacement per degree distribution, there was a small flattening of the curves, and then the slope continued to rise. This may have been owing to recruitment of other, secondary static restraints of the wrist after the DUTL was torn. Indeed, to preserve the normal anatomy of the wrist, the DUTL was not isolated; hence, other structures of the wrist likely influenced the overall wrist mechanics. However, the reproducible and consistent injury generated in all the specimens tested leads us to believe that the DUTL is the main stabilizer of the wrist to radial deviation in a starting position of pronation and flexion. Moreover, we observed no significant changes in the load applied to the wrist between the native ligament state and after repairing the DUTL. Thus, following repair, the DUTL presented with similar angular stiffness, yield strength and angular deformation at yield. Further studies are required to investigate the correlation between a torn ulnotriquetral ligament, the functional limitations associated with this type of injury and whether it is then clinically necessary to repair the DUTL tear.
Limitations
This study design has inherent limitations. First, the motorized wrist-movement stimulator may not have replicated the exact loading forces exerted on the wrist in vivo. Furthermore, the cadaveric wrist model was tested to failure in a single position with the forearm in pronation and with the wrist in 45° of flexion, as we believed that this position exerted the greatest tension on the DUTL. Finally, the current gold standards for diagnosing wrist injuries are MRI-A and arthroscopic surgery.5 However, high-resolution ultrasonography done by a fellowship-trained musculoskeletal radiologist is a cost-effective and valuable diagnostic tool to evaluate not only static but also dynamic wrist structures, which MRI-A cannot perform. Moreover, the disruption of the capsule after dissection and testing precluded the use of MRI-A, as did the mounting of the specimens in aluminum boxes, with metallic screw eyelets in place.
Conclusion
The reproducibility of the pattern of injury to the DUTL when the wrist is stressed in flexion and radial deviation can help us better understand wrist biomechanics and related ulnar-sided wrist injuries, especially in athletes. It is important to obtain an accurate diagnosis to establish proper treatment and to prevent any delay in the return to play for an athlete or the return to work and normal function for any patient. Furthermore, it is essential to provide a unique, sport-specific, individual treatment for each athlete.24 Additional work is needed to further characterize the pathoanatomy of hockey wrist. We plan to review MRI images from elite hockey players and to study the wrist biomechanics in these athletes. Subsequently, we intend to validate diagnostic tests for this injury (physical examination, dynamic ultrasonography, MRI and arthroscopy) in order to better understand, prevent and treat this injury.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study, acquired and analyzed the data, wrote and reviewed the article, and approved the final version for publication.
References
- 1.Shahabpour M, De Maeseneer M, Pouders C, et al. MR imaging of normal extrinsic wrist ligaments using thin slices with clinical and surgical correlation. Eur J Radiol. 2011;77:196–201. doi: 10.1016/j.ejrad.2010.05.043. [DOI] [PubMed] [Google Scholar]
- 2.Linscheid RL, Dobyns JH, Beabout JW, et al. Traumatic instability of the wrist. Diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972;54:1612–32. [PubMed] [Google Scholar]
- 3.Trail IA, Stanley JK, Hayton MJ. Twenty questions on carpal instability. J Hand Surg Eur Vol. 2007;32:240–55. doi: 10.1016/J.JHSB.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Watson HK, Weinzweig J. Triquetral impingement ligament tear (tilt) J Hand Surg Br. 1999;24:321–4. doi: 10.1054/jhsb.1999.0070. [DOI] [PubMed] [Google Scholar]
- 5.Shahabpour M, Van Overstraeten L, Ceuterick P, et al. Pathology of extrinsic ligaments: a pictorial essay. Semin Musculoskelet Radiol. 2012;16:115–28. doi: 10.1055/s-0032-1311763. [DOI] [PubMed] [Google Scholar]
- 6.Taneja AK, Bredella MA, Chang CY, et al. Extrinsic wrist ligaments: prevalence of injury by magnetic resonance imaging and association with intrinsic ligament tears. J Comput Assist Tomogr. 2013;37:783–9. doi: 10.1097/RCT.0b013e318298aa2a. [DOI] [PubMed] [Google Scholar]
- 7.Chen YR, Tang JB. Changes in contact site of the radiocarpal joint and lengths of the carpal ligaments in forearm rotation: an in vivo study. J Hand Surg Am. 2013;38:712–20. doi: 10.1016/j.jhsa.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Cahalan TD, Cooney WP, 3rd, Tamai K, et al. Biomechanics of the golf swing in players with pathologic conditions of the forearm, wrist, and hand. Am J Sports Med. 1991;19:288–93. doi: 10.1177/036354659101900314. [DOI] [PubMed] [Google Scholar]
- 9.Kox LS, Kuijer PP, Kerkhoffs GM, et al. Prevalence, incidence and risk factors for overuse injuries of the wrist in young athletes: a systematic review. Br J Sports Med. 2015;49:1189–96. doi: 10.1136/bjsports-2014-094492. [DOI] [PubMed] [Google Scholar]
- 10.Pang EQ, Yao J. Ulnar-sided wrist pain in the athlete (TFCC/DRUJ/ECU) Curr Rev Musculoskelet Med. 2017;1:53–61. doi: 10.1007/s12178-017-9384-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sasao S, Beppu M, Kihara H, et al. An anatomical study of the ligaments of the ulnar compartment of the wrist. Hand Surg. 2003;8:219–26. doi: 10.1142/s0218810403001844. [DOI] [PubMed] [Google Scholar]
- 12.Boutry N, Lapegue F, Masi L, et al. Ultrasonographic evaluation of normal extrinsic and intrinsic carpal ligaments: preliminary experience. Skeletal Radiol. 2005;34:513–21. doi: 10.1007/s00256-005-0929-4. [DOI] [PubMed] [Google Scholar]
- 13.Lacelli F, Muda A, Sconfienza LM, et al. High-resolution ultrasound anatomy of extrinsic carpal ligaments. Radiol Med. 2008;113:504–16. doi: 10.1007/s11547-008-0269-2. [DOI] [PubMed] [Google Scholar]
- 14.Becce F, Theumann N, Bollmann C, et al. Dorsal fractures of the triquetrum: MRI findings with an emphasis on dorsal carpal ligament injuries. AJR Am J Roentgenol. 2013;200:608–17. doi: 10.2214/AJR.12.8736. [DOI] [PubMed] [Google Scholar]
- 15.Tan J, Chen J, Tang JB. In vivo length changes of wrist ligaments at full wrist extension. J Hand Surg Eur Vol. 2014;39:384–90. doi: 10.1177/1753193413484626. [DOI] [PubMed] [Google Scholar]
- 16.Moritomo H, Murase T, Arimitsu S, et al. Change in the length of the ulnocarpal ligaments during radiocarpal motion: possible impact on triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2008;33:1278–86. doi: 10.1016/j.jhsa.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 17.Dianat I, Rahimi S, Nedaei M, et al. Effects of tool handle dimension and workpiece orientation and size on wrist ulnar/radial torque strength, usability and discomfort in a wrench task. Appl Ergon. 2017;59:422–30. doi: 10.1016/j.apergo.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Ciriello VM, Maikala RV, O’Brien NV. Maximal acceptable torques of six highly repetitive hand–wrist motions for male industrial workers. Hum Factors. 2013;55:309–22. doi: 10.1177/0018720812454539. [DOI] [PubMed] [Google Scholar]
- 19.Carse B, Thomson A, Stansfield B. A novel device for evaluating forces during the dynamic jar opening action — Do older and younger adults do things differently? Med Eng Phys. 2011;33:521–5. doi: 10.1016/j.medengphy.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 20.O’Driscoll SW, Horii E, Ness R, et al. The relationship between wrist position, grasp size, and grip strength. J Hand Surg Am. 1992;17:169–77. doi: 10.1016/0363-5023(92)90136-d. [DOI] [PubMed] [Google Scholar]
- 21.Campbell D, Campbell R, O’Connor P, et al. Sports-related extensor carpi ulnaris pathology: a review of functional anatomy, sports injury and management. Br J Sports Med. 2013;47:1105–11. doi: 10.1136/bjsports-2013-092835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawkes R, O’Connor P, Campbell D. The prevalence, variety and impact of wrist problems in elite professional golfers on the European Tour. Br J Sports Med. 2013;47:1075–9. doi: 10.1136/bjsports-2012-091917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mölsä J, Kujala U, Myllynen P, et al. Injuries to the upper extremity in ice hockey: analysis of a series of 760 injuries. Am J Sports Med. 2003;31:751–7. doi: 10.1177/03635465030310051901. [DOI] [PubMed] [Google Scholar]
- 24.Dy CJ, Khmelnitskaya E, Hearns KA, et al. Opinions regarding the management of hand and wrist injuries in elite athletes. Orthopedics. 2013;36:815–9. doi: 10.3928/01477447-20130523-30. [DOI] [PubMed] [Google Scholar]