Abstract
Objectives:
This study investigated potential associations between having a person in need of nursing care at home and psychological distress amongst the Japanese working population, using a nationally representative sample.
Methods:
We extracted data from the 2013 Comprehensive Survey of Living Conditions conducted by the Ministry of Health, Labour and Welfare of Japan. The original survey was conducted amongst 295,367 households in 5,530 randomly selected municipalities. We analyzed participants aged 25-65 years who headed a household. The original questionnaire included questions about the specific qualifications required to receive long-term care insurance benefits, about psychological distress (measured using the K6 scale), and other covariates. If a family contained a member in need of nursing care at home, the person who headed that household was recognized as the participant who had a person in need of nursing care at home. Multiple logistic regression analysis was conducted to investigate the association between having a person in need of nursing care at home and psychological distress.
Results:
A total of 36,193 men and 2,765 women were included in the analysis, 2.9% of whom had a person in need of nursing care at home. Statistical analysis revealed an association between having a care-requiring older relative at home and psychological distress (odds ratio: 1.40, 95% confidence interval: 1.01-1.93).
Conclusions:
Having a person in need of nursing care at home appears to be positively correlated with worsening mental health of working populations in Japan.
Keywords: Caregivers, Cross-sectional studies, Mental health, Working age population
Introduction
In Japan, care for frail, older adults is largely shouldered by that person's family1). Moreover, traditionally the majority of family caregivers have been nonworking spouses, daughters, or daughters-in-law of the older adults in need of care1). The burden on family members who provide that care is considerable, and poses a crucial problem2): caregivers for older people have been found to be more likely than non-caregivers to experience physical and psychological burdens, and to suffer from anxiety and depression3-7).
A recent trend shows an increasing number of primary caregivers who maintain their paid employment because they have no one else to provide care. This reality is part of the ramifications of fewer family members per household in Japan8). Adverse effects seen in such caregivers include lethargy, tiredness and lack of concentration, anxiousness about work-related responsibilities at work, and stress induced by trying to manage the often incompatible roles of worker and caregiver, each with its own conflicting demands and expectations9). To date, only one Japan-based study has investigated the association between caregivers' mental health and caring for older relatives; this was conducted among workers at three sites in a Japanese prefecture10). The authors of that study reported that workers who were caring for older relatives had a significantly increased risk of depression10). The association between caring for older relatives and poor mental health necessitates examining a nationally representative sample using demographic or occupational variables for adjustment.
Like Japan, other Asian countries also face nationally unprecedented situations in their rapidly growing elderly populations. Because of this rapid increase and the shortage of standardized institutional solutions for long-term care in Asian countries11-14), working caregivers will presumably be increasingly called upon to provide home care for disabled older adults. The Japanese experience in arranging work-life balance between employment outside the home and nursing care in the home could beneficially contribute to other Asian countries.
This cross-sectional study aimed to investigate the association between workers' mental health and having a person in need of nursing care at home. The study used a nationally representative sample of the Japanese population derived from the nationwide 2013 Comprehensive Survey of Living Conditions, which was conducted by the Ministry of Health, Labour and Welfare of Japan.
Participants and Methods
Data collection
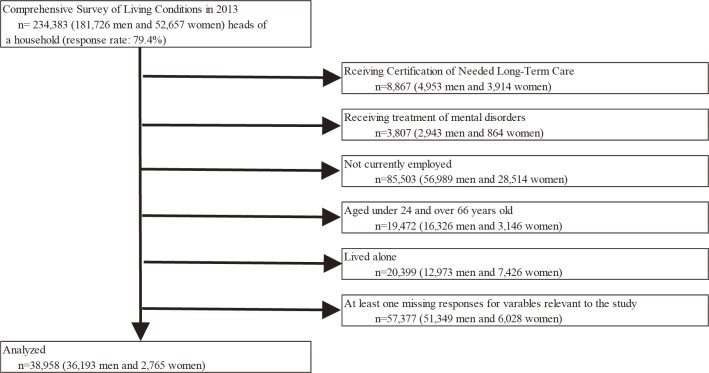
The survey, which covered households and household members nationwide, was conducted in June-July 2013. Participants were chosen from randomly selected areas throughout Japan and given two self-administered questionnaires: one on the household and one on their health. The two questionnaires were distributed to 295,367 households located in 5,530 areas selected randomly from areas of the 2010 Population Census. Members of 234,383 households (response rate: 79.4%) completed the questionnaires, which were collected by survey staff. In the present study, participants were excluded who: had received certification of needing long-term care; were receiving treatment for mental disorders; did not work; were younger than 24 or older than 66 years old; lived alone; or had at least one missing response for variables relevant to the study. The flow of the data collection is presented in Fig. 1. The final analysis was conducted using data on 38,958 participants who were currently employed, were head of a household, whose earnings supported their family, and were aged 25-65 years. This sample comprised 36,193 men and 2,765 women.
Fig. 1.
Flow chart of this study sample
We obtained permission to use certain data from the 2013 Comprehensive Survey of Living Conditions for purposes other than those originally intended by the Ministry of Health, Labour and Welfare.
Measures
1) Having a person in need of nursing care at home
Under the Japanese long-term care insurance scheme, individuals certified by the municipal government as needing care or support are eligible to receive insurance benefits. For the household questionnaire, each participant was asked to respond to a question about the specific qualifications for which a household member was receiving long-term care insurance benefits. All respondents were issued a family identification code and, based on this, we were able to delineate the participants into families. If a family contained a member in need of nursing care at home, the person who headed the household was deemed the participant who had a person in need of nursing care at home.
2) Psychological distress
The health questionnaire incorporated the Kessler Psychological Distress Scale (K6) for acquiring data on mental health15). The K6 has been translated into Japanese and has shown acceptable internal consistency, reliability, and validity16). The scale has been shown to have effectively detected major depression and dysthymia in accordance with the established Diagnostic and Statistical Manual of Mental Disorders-IV criteria16). It comprises six items, and measures the extent of psychological distress using a five-point response scale ranging from 0 (none of the time) to 4 (all of the time). Total scores range from 0 to 24, with a higher score indicating proportionally greater distress. In line with the recommended K6 cutoff point, participants with total scores of ≥13 (13-24) were defined as having serious mental illness, while a score of 0-12 suggested no mental illness16,17).
3) Other covariates and demographic characteristics
Questions in the survey covered basic demographic information. The household questionnaire assessed age, sex, educational attainment, number of family members at home, occupation, employment status, company size, and weekly working hours; the health questionnaire measured sleeping time, smoking status, and frequency of drinking alcohol. Age was classified into the following groups: 25-29, 30-39, 40-49, 50-59, and 60-64 years. Weekly working hours were categorized into the following ranges: ≤ 20, 21-30, 31-40, 41-50, 51-60, and ≥61. The number of family members at home was delineated as 2, 3, 4, 5, and ≥6. Participants were each asked to answer questions about their highest level of educational attainment, choosing from: elementary or junior high school; high school; vocational college; junior college; university; or graduate school. For employment status, they chose from: permanent; regular part-time; casual part-time; temporary; full-time fixed-term contract; post-retirement fixed-term contract; and other. For occupation (i.e., type of job), they chose from: management; professional and technical work, including teaching, health care, and research; office administrator; sales; service; security; agriculture and fishery; manufacturing; transportation or machine operator; construction; cleaning, packing, and operator; other; and unknown. For company size (i.e., the total number of employees in the person's company, including headquarters, branch offices, and factories), they chose from: 1-4; 5-29; 30-99; 100-299; 300-499; 500-999; 1,000-4,999; ≥5,000; or unspecified size if employed in a civil service office. For sleeping time, they chose from: <5; 5-6; 6-7; 7-8; 8-9; or >9 hours per night. For smoking status, they chose from: everyday; sometimes; quit smoking for >1 month; or never smoked. For frequency of drinking alcohol, they chose from: everyday; 5-6 days/week; 3-4 days/week; 1-2 days/week; 1-3 days/month; hardly drink; quit drinking; or never drank. Educational attainment was dichotomized into ≤ 12 years or >12 years. Employment status was dichotomized into regular employee or non-regular employee. Occupation was classified into six groups based on previous studies18,19): professional or technician; manager; office administrator; sales or service worker; production worker (i.e., manual laborer), including transportation and communications, and production process and related occupations; and other (if occupation was not classifiable). In line with a previous study19), company size was classified into 1-29, 30-299, 300-999, and ≥1,000 employees, with reference to the definition of small- and medium-sized companies as per Japan's Small and Medium-sized Enterprise Basic Act. Civil service offices were classified as a separate category, irrespective of size, because the original survey did not request that information. Frequency of drinking alcohol was classified into three groups: every day, sometimes, or never.
Statistical analysis
We tested associations between the studied variables and psychological distress using a Chi-square test. We investigated the demographic characteristics of each variable in relation to psychological distress with the following items as an example: Having a person in need of nursing care at home; male; 30-39 years old; 31-40 weekly working hours; two family members at home; <12 years educational attainment; non-regular employee; manager; smallest company size (1-29 employees); 6-7 hours of sleeping time per night; smoking every day; and drinking alcohol every day. With these, the odds ratio (OR) and 95% confidence interval (CI) of psychological distress were estimated for other categories of each characteristic in a series of logistic regression analyses. We first performed the analysis with adjustment for sex and age, and then fully adjusted for sex, age, weekly working hours, number of family members at home, educational attainment, employment status, occupation, company size, sleeping time, smoking status, and frequency of drinking alcohol. We showed the demographic characteristics of the survey respondents who had a person in need of nursing care at home. All analyses were performed using Stata 14 (StataCorp, College Station, TX), with statistical significance set at p <0.05.
Ethics statement
This study involved a retrospective analysis of data that had already been obtained through a national survey. As we did not use any personally identifiable information, and based on existing regulations in Japan, ethical approval was not required.
Results
Table 1 shows the associations between the studied variables and psychological distress. The portion of survey respondents who reported having a person in need of nursing care at home was 2.9%. The following groups had significantly higher proportions of participants suffering from psychological distress: female, younger, the shortest and longest weekly working hours, smallest family size, "other" occupation, the shortest and longest sleeping times, and no alcohol consumption.
Table 1.
Demographic, occupational, and lifestyle characteristics by psychological distress (n=38,958)
| Psychological distress | ||||||||
|---|---|---|---|---|---|---|---|---|
| Low (K6≤12) n=37,671 | High (K6≥13) n=1,287 | p valuea | ||||||
| n | (%) | n | (%) | |||||
| a Chi-square. | ||||||||
| Sex | ||||||||
| Male | 35,067 | (96.9) | 1,126 | (3.1) | <0.001 | |||
| Female | 2,604 | (94.2) | 161 | (5.8) | ||||
| Age | ||||||||
| 25-29 | 1,443 | (95.7) | 65 | (4.3) | <0.001 | |||
| 30-39 | 8,513 | (95.8) | 378 | (4.2) | ||||
| 40-49 | 11,444 | (96.4) | 428 | (3.6) | ||||
| 50-59 | 10,836 | (97.0) | 339 | (3.0) | ||||
| 60-65 | 5,435 | (98.6) | 77 | (1.4) | ||||
| Having a person in need of nursing care at home | ||||||||
| No | 36,589 | (96.7) | 1,243 | (3.3) | 0.250 | |||
| Yes | 1,082 | (96.1) | 44 | (3.9) | ||||
| Weekly working hours | ||||||||
| Less than 20 | 927 | (95.0) | 49 | (5.0) | <0.001 | |||
| 20-30 | 1,260 | (96.1) | 51 | (3.9) | ||||
| 31-40 | 11,283 | (96.8) | 368 | (3.2) | ||||
| 41-50 | 14,494 | (97.0) | 446 | (3.0) | ||||
| 51-60 | 6,338 | (96.9) | 200 | (3.1) | ||||
| More than 61 | 3,369 | (95.1) | 173 | (4.9) | ||||
| Number of family members at home | ||||||||
| 2 | 10,054 | (96.4) | 379 | (3.6) | 0.040 | |||
| 3 | 10,984 | (96.6) | 391 | (3.4) | ||||
| 4 | 11,349 | (97.1) | 340 | (2.9) | ||||
| 5 | 3,892 | (96.8) | 129 | (3.2) | ||||
| More than 6 | 1,392 | (96.3) | 48 | (3.7) | ||||
| Educational attainment | ||||||||
| Less than 12 | 18,131 | (96.6) | 630 | (3.4) | 0.562 | |||
| More than 12 | 19,540 | (96.8) | 657 | (3.2) | ||||
| Employment status | ||||||||
| Regular employee | 32,150 | (96.7) | 1,084 | (3.3) | 0.266 | |||
| Non-regular employee | 5,521 | (96.5) | 203 | (3.5) | ||||
| Occupation | ||||||||
| Managers | 4,519 | (97.7) | 105 | (2.3) | <0.001 | |||
| Professionals and technicians | 11,005 | (96.6) | 392 | (3.4) | ||||
| Clerks | 4,255 | (96.3) | 165 | (3.7) | ||||
| Sales and service workers | 7,924 | (96.5) | 289 | (3.5) | ||||
| Production workers | 9,134 | (96.8) | 299 | (3.2) | ||||
| Others | 834 | (95.8) | 37 | (4.2) | ||||
| Company size (number of employees) | ||||||||
| 1-29 | 7,150 | (96.6) | 255 | (3.4) | 0.379 | |||
| 30-299 | 11,272 | (96.6) | 403 | (3.4) | ||||
| 300-999 | 5,537 | (96.8) | 181 | (3.2) | ||||
| 1000 or more | 9,760 | (96.7) | 332 | (3.3) | ||||
| Civil service | 3,952 | (97.2) | 116 | (2.8) | ||||
| Sleeping time | ||||||||
| Less than 5 hours | 2,744 | (90.1) | 302 | (9.9) | <0.001 | |||
| 5-6 hour | 11,945 | (96.5) | 433 | (3.5) | ||||
| 6-7 hour | 13,766 | (97.8) | 310 | (2.2) | ||||
| 7-8 hour | 7,276 | (97.8) | 162 | (2.2) | ||||
| 8-9 hour | 1,630 | (97.1) | 49 | (2.9) | ||||
| More than 9 | 310 | (90.9) | 31 | (9.1) | ||||
| Smoking status | ||||||||
| Smokes everyday | 12,954 | (96.5) | 468 | (3.5) | 0.194 | |||
| Smokes sometimes | 817 | (95.9) | 35 | (4.1) | ||||
| Ex-smoker | 3,812 | (97.0) | 119 | (3.0) | ||||
| Non-smoker | 20,088 | (96.8) | 665 | (3.2) | ||||
| Frequency of alcohol consumption | ||||||||
| Everyday | 11,240 | (96.6) | 393 | (3.4) | <0.001 | |||
| Sometimes | 13,657 | (97.4) | 371 | (2.6) | ||||
| Never | 12,774 | (96.1) | 523 | (3.9) | ||||
Table 2 shows the results of multiple logistic regression analysis. This revealed a strong correlation between psychological distress and being an employed worker with a person in need of nursing care at home (OR: 1.40, 95%CI: 1.01-1.93).
Table 2.
Presence of having an older person receiving long-term care at home and psychological distress (n=38,958)
| Odds ratio (95% confidence interval) | |||||||
|---|---|---|---|---|---|---|---|
| Model 1a | Model 2b | ||||||
|
aAdjusted for age and sex bThe fully adjusted logistic regression model is adjusted for sex, age, weekly working hours, number of family at home, educational attainment, employment status, occupation, company size, sleeping time, smoking status, and frequency of drinking alcohol *p<0.05 | |||||||
| Have an older relative requiring care at home | |||||||
| No | 1.00 | 1.00 | |||||
| Yes | 1.56 | (1.14-2.13)* | 1.40 | (1.01-1.93)* | |||
Table 3 shows the demographic characteristics of the survey respondents who reported having a person in need of nursing care at home. As Table 3 indicates, the following groups had higher proportions of participants suffering from psychological distress: female, 25-29, 40-49 and 50-59 years old, fewer than 5 hours and more than 9 hours of sleeping time per night, and no alcohol consumption.
Table 3.
Demographic, occupational, and lifestyle characteristics among employees who have an older relative requiring care at home by psychological distress (n=1,126)
| Psychological distress | ||||||
|---|---|---|---|---|---|---|
| Low stress (K6≤12) n=1,082 | High stress (K6≥13) n=44 | |||||
| n | (%) | n | (%) | |||
| Sex | ||||||
| Male | 1,018 | (96.4) | 38 | (3.6) | ||
| Female | 64 | (91.4) | 6 | (8.6) | ||
| Age | ||||||
| 25-29 | 5 | (83.3) | 1 | (16.7) | ||
| 30-39 | 41 | (100) | 0 | (0) | ||
| 40-49 | 148 | (93.1) | 11 | (6.9) | ||
| 50-59 | 534 | (95.4) | 26 | (4.6) | ||
| 60-65 | 354 | (98.3) | 6 | (1.7) | ||
| Weekly working hours | ||||||
| Less than 20 | 41 | (97.6) | 1 | (2.4) | ||
| 20-30 | 59 | (100) | 0 | (0) | ||
| 31-40 | 420 | (95.9) | 18 | (4.1) | ||
| 41-50 | 366 | (97.1) | 11 | (2.9) | ||
| 51-60 | 129 | (92.1) | 11 | (7.9) | ||
| More than 61 | 67 | (95.7) | 3 | (4.3) | ||
| Number of family members at home | ||||||
| 2 | 148 | (95.5) | 7 | (4.5) | ||
| 3 | 312 | (96.9) | 10 | (3.1) | ||
| 4 | 251 | (97.7) | 6 | (2.3) | ||
| 5 | 209 | (94.6) | 12 | (5.4) | ||
| More than 6 | 162 | (94.7) | 9 | (5.3) | ||
| Educational attainment | ||||||
| Less than 12 | 646 | (95.4) | 31 | (4.6) | ||
| More than 12 | 436 | (97.1) | 13 | (2.9) | ||
| Employment status | ||||||
| Regular employee | 811 | (95.6) | 37 | (4.4) | ||
| Non-regular employee | 271 | (97.5) | 7 | (2.5) | ||
| Occupation | ||||||
| Managers | 166 | (97.7) | 4 | (2.3) | ||
| Professionals and technicians | 259 | (96.6) | 9 | (3.4) | ||
| Clerks | 95 | (94.1) | 6 | (5.9) | ||
| Sales and service workers | 218 | (96.9) | 7 | (3.1) | ||
| Production workers | 317 | (95.2) | 16 | (4.8) | ||
| Others | 27 | (93.1) | 2 | (6.9) | ||
| Company size (number of employees) | ||||||
| 1-29 | 279 | (96.5) | 10 | (3.5) | ||
| 30-299 | 357 | (95.0) | 19 | (5.0) | ||
| 300-999 | 120 | (96.8) | 4 | (3.2) | ||
| 1000 or more | 206 | (97.2) | 6 | (2.8) | ||
| Civil service | 120 | (96.0) | 5 | (4.0) | ||
| Sleeping time | ||||||
| less than 5 hours | 79 | (92.9) | 6 | (7.1) | ||
| 5-6 hour | 270 | (95.7) | 12 | (4.3) | ||
| 6-7 hour | 309 | (97.5) | 8 | (2.5) | ||
| 7-8 hour | 261 | (97.8) | 6 | (2.2) | ||
| 8-9 hour | 100 | (95.2) | 5 | (4.8) | ||
| more than 9 | 63 | (90.0) | 7 | (10.0) | ||
| Smoking status | ||||||
| Smokes everyday | 302 | (97.1) | 9 | (2.9) | ||
| Smokes sometimes | 10 | (83.3) | 2 | (16.7) | ||
| Ex-smoker | 124 | (96.9) | 4 | (3.1) | ||
| Non-smoker | 646 | (95.7) | 29 | (4.3) | ||
| Frequency of alcohol consumption | ||||||
| Everyday | 364 | (97.9) | 8 | (2.1) | ||
| Sometimes | 298 | (97.4) | 8 | 2.6) | ||
| Never | 420 | (93.8) | 28 | (6.2) | ||
Discussion
The present study investigated potential associations between psychological distress and having a person in need of nursing care at home among the Japanese working population. Around 3% of survey respondents reported having a person in need of nursing care at home. This subgroup experienced significantly higher levels of psychological distress when compared with participants who did not have a person at home in need of nursing care. Among the respondents who reported having a person in need of nursing care at home, psychological distress was most prevalent in those who were young and/or female.
The results suggest that having a person in need of nursing care at home may affect the mental health of working populations in Japan. Providing nursing care at home can be time-consuming and is associated with physical and psychological burdens. Indeed, previous research has reported an association between caregiving and depression3-7),10). In Japan, among people who had left their job and were caring for older relatives, 25.3% of men and 32.8% of women indicated that stress caused by caregiving was a reason for leaving their job1). To reduce workers' care-related stress and prevent them from leaving their jobs, companies in Japan should consider promoting a balance of work and caregiving of older relatives for their employees.
Young and female respondents were more likely to suffer psychological distress than other groups, which is consistent with previous studies20-23). Arguably, young female caregivers are more likely than older female caregivers to be working and/or caring for children in the home. Especially in Japanese society, females tend to bear the majority of the child care and housekeeping responsibilities, even when employed outside the home24); this situation is specifically linked to gender and age differences in experiences and perceptions of psychological distress. To reduce the number of people who leave or change their jobs, interventions such as stress management and the provision of information about work-care balance for female and young workers may be effective. Also, it should be noted that the sample size of some sex and age groups is small, which might be a source of bias. Further studies are needed to evaluate psychological conditions among women and younger populations by using a larger sample of participants.
Given Japan's aging society and the continued surge in the population of older adults requiring care, it is possible that the number of workers caring for older relatives at home may also increase. When such workers obtain support from their workplace colleagues and/or supervisors, the workers tend to adjust their working hours to allow them to continue providing care25). Occupational health professionals may consider advising on how to adjust working environments to mitigate the impacts that this form of home caregiving can have on workers' mental health.
As of 2017, the total Japanese population was 126.7 million, which included 35 million aged ≥65 years (27.6%) and 17.3 million aged ≥75 years (13.7%)26). Japan is the global front-runner of super-aged societies27). To maintain the employment rate in Japan, people should be prevented as much as possible from leaving their jobs because of nursing care duties at home. The development of stress management programs for employees who must also fulfill home nursing care for elderly people might be an effective way of helping them retain their paying jobs while also reducing the risk of declining mental health.
There are a few potential limitations of the current study. Firstly, given that this was a cross-sectional investigation, it was not possible to determine causality. Longitudinal studies can be pursued to rectify this. Secondly, the target population of this study was heads of households. Since the head of a household conceivably has the most responsibility within their family, they may feel more stressed than the other household members. Thus, our results may not be generalizable to working populations in other situations. Thirdly, further studies are needed to evaluate whether other confounding factors may provide possible mechanisms for the observed attenuation in the association between having a person in need of nursing care at home and psychological distress amongst the Japanese working population. For example, spousal status (i.e., dual earner or single earner) or being a parent of small children may also play a significant mediating role. Finally, there are additional psychosocial factors in the workplace to consider (e.g., job demands, job control, and support of colleagues and supervisors), which might be important mediators of the association between workers' mental health and their provision of home care for an older relative. These variables should be examined in future research.
Conclusions
This study found that having a person in need of nursing care at home appears to be positively correlated with worsening mental health in working populations in Japan.
Acknowledgments: We thank Arina Harman, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Conflicts of interest: None declared
References
- 1). Cabinet Office, Government of Japan. . Annual Report on the Aging Society: 2016. [Online]. 2016[cited 2016 May 20]; Available from: URL: http://www8.cao.go.jp/kourei/whitepaper/w-2016/html/zenbun/s1_2_3.html
- 2). Tamiya N, Noguchi H, Nishi A, et al. Population ageing and wellbeing: lessons from Japan's long-term care insurance policy. Lancet 2011; 378 (9797): 1183-1192. [DOI] [PubMed] [Google Scholar]
- 3). Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail 2005; 7 (4): 592-603. [DOI] [PubMed] [Google Scholar]
- 4). Waite A, Bebbington P, Skelton-Robinson M, et al. Social factors and depression in carers of people with dementia. Int J Geriatr Psychiatry 2004; 19 (6): 582-587. [DOI] [PubMed] [Google Scholar]
- 5). Hirst M. Carer distress: a prospective, population-based study. Soc Sci Med 2005; 61 (3): 697-708. [DOI] [PubMed] [Google Scholar]
- 6). Yokoyama Y, Shimizu T, Hayakawa K. Depressive states and health problems in caregivers of the disabled elderly at home. Environ Health Prev Med 1997; 1 (4): 165-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Evangelista LS, Strömberg A, Dionne-Odom JN. An integrated review of interventions to improve psychological outcomes in caregivers of patients with heart failure. Curr Opin Support Palliat Care 2016; 10 (1): 24-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Gender Equality Bureau Cabinet Office. . Fiscal 2017 government white paper on gender equality. [Online]. 2017[cited 2017 Oct. 20]; Available from: URL: http://www.gender.go.jp/about_danjo/whitepaper/h29/zentai/index.html
- 9). Arksey H. Combining informal care and work: supporting carers in the workplace. Health Soc Care Community 2002; 10 (3): 151-161. [DOI] [PubMed] [Google Scholar]
- 10). Honda A, Date Y, Abe Y, et al. Work-related Stress, Caregiver Role, and Depressive Symptoms among Japanese Workers. Saf Health Work 2014; 5 (1): 7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Du J, Shao S, Jin GH, Qian CG, Xu W, Lu XQ. Factors associated with health-related quality of life among family caregivers of disabled older adults: a cross-sectional study from Beijing. Medicine (Baltimore) 2017; 96 (44): e8489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Park HK, Na DL, Han SH, et al. Clinical characteristics of a nationwide hospital-based registry of mild-to-moderate Alzheimer's disease patients in Korea: a CREDOS (Clinical Research Center for Dementia of South Korea) study. J Korean Med Sci 2011; 26 (9): 1219-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Teerawichitchainan B, Pothisiri W, Long GT. How do living arrangements and intergenerational support matter for psychological health of elderly parents? Evidence from Myanmar, Vietnam, and Thailand. Soc Sci Med 2015; 136-137: 106-116. [DOI] [PubMed] [Google Scholar]
- 14). Matsushita M, Pai MC, Jhou CY, Koyama A, Ikeda M. Cross-cultural study of caregiver burden for Alzheimer's disease in Japan and Taiwan: result from Dementia Research in Kumamoto and Tainan (DeReKaT). Int Psychogeriatr 2016; 28 (7): 1125-1132. [DOI] [PubMed] [Google Scholar]
- 15). Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32 (6): 959-976. [DOI] [PubMed] [Google Scholar]
- 16). Furukawa TA, Kawakami N, Saitoh M, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res 2008; 17 (3): 152-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Sakurai K, Nishi A, Kondo K, et al. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci 2011; 65 (5): 434-441. [DOI] [PubMed] [Google Scholar]
- 18). Kawakami N, Haratani T, Kobayashi F, et al. Occupational class and exposure to job stressors among employed men and women in Japan. J Epidemiol 2004; 14 (6): 204-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19). Inoue A, Kawakami N, Tsuchiya M, Sakurai K, Hashimoto H. Association of occupation, employment contract, and company size with mental health in a national representative sample of employees in Japan. J Occup Health 2010; 52 (4): 227-240. [DOI] [PubMed] [Google Scholar]
- 20). Anderson LA, Edwards VJ, Pearson WS, Talley RC, McGuire LC, Andresen EM. Adult caregivers in the United States: characteristics and differences in well-being, by caregiver age and caregiving status. Prev Chronic Dis 2013; 10: E135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Torimoto-Sasai Y, Igarashi A, Wada T, Ogata Y, Yamamoto-Mitani N. Female family caregivers face a higher risk of hypertension and lowered estimated glomerular filtration rates: a cross-sectional, comparative study. BMC public health 2015; 15: 177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22). Moon H, Dilworth-Anderson P. Baby boomer caregiver and dementia caregiving: findings from the National Study of Caregiving. Age ageing 2015; 44 (2): 300-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23). Carter JH, Lyons KS, Stewart BJ, Archbold PG, Scobee R. Does age make a difference in caregiver strain? Comparison of young versus older caregivers in early-stage Parkinson's disease. Mov Disord 2010; 25 (6): 724-730. [DOI] [PubMed] [Google Scholar]
- 24). Eguchi H, Shimazu A, Fujiwara T, et al. The effects of workplace psychosocial factors on whether Japanese dual-earner couples with preschool children have additional children: a prospective study. Ind Health 2016; 54 (6): 498-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25). Rands G. Working people who also care for the elderly. Int J Geriatr Psychiatry 1997; 12 (1): 39-44. [DOI] [PubMed] [Google Scholar]
- 26). Suzuki T. Health status of older adults living in the community in Japan: Recent changes and significance in the super-aged society. Geriatr Gerontol Int 2018; 18 (5): 667-677. [DOI] [PubMed] [Google Scholar]
- 27). Arai H, Ouchi Y, Toba K, et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr Gerontol Int 2015; 15 (6): 673-687. [DOI] [PubMed] [Google Scholar]