Abstract
We experienced a case of acute congestive heart failure in a 73-year-old man who had been followed up due to mild-to-moderate aortic stenosis and moderate-to-severe aortic regurgitation. A huge aortic valve aneurysm was found to extend from his right coronary cusp to a left ventricular outflow tract, resulting in moderate subaortic obstruction and severe aortic regurgitation. Surgical repair was performed and a perforated aneurysm of right aortic cusp was identified. Histological examinations suggested that healed infective endocarditis was responsible for the formation of an aneurysm in the aortic valve.
<Learning objective: Aortic valve aneurysm is an uncommon complication of infective endocarditis. The infective process of a cardiac valve is thought to augment valvular tissue injury, resulting in aneurysmal formation and perforation of the valvular aneurysm. We report an uncommon case of aortic valve aneurysm that was histologically suggested to be caused by subclinical infective endocarditis. The subaortic obstruction and aortic regurgitation were successfully treated using a surgical procedure.>
Keywords: Aortic valve aneurysm, Infective endocarditis, Aortic regurgitation, Aortic stenosis
Introduction
Most valvular aneurysms have been found in the mitral valve, and aortic valve aneurysm is rare. We present a case of aortic valve aneurysm responsible for acute congestive heart failure, which was probably due to exacerbating aortic regurgitation (AR) and subaortic obstruction.
Case report
A 73-year-old man, who had been followed up in an out-patient clinic because of mild-to-moderate aortic stenosis and moderate-to-severe AR, presented with acutely progressing dyspnea and he was admitted for further evaluation of congestive heart failure symptoms. He had no past history of symptoms or signs suggestive of infective endocarditis. On admission, his blood pressure was 158/74 mmHg and he had a regular sinus rhythm with a rate of 100 beats per minute. He had moist crackles in his bilateral lung fields and he had diastolic blowing and harsh systolic ejection murmurs at the left sternal border. A resting electrocardiogram showed a left axial deviation, an ST-segment depression with strain, and a QS pattern in leads V2 and V3, indicating left ventricular (LV) volume overload and LV hypertrophy. Chest radiography showed remarkable pulmonary congestion and enlarged cardiac silhouette with a cardiothoracic ratio of 63%, but no inflammatory reaction was found in a blood test. Transthoracic echocardiography (TTE) revealed mild LV systolic dysfunction (ejection fraction: 55%) and aneurysmal enlargement of the coronary cusp (21 mm × 12 mm) that extended from the right coronary cusp to the LV outflow tract (Fig. 1A). Transesophageal echocardiography (TEE) showed protrusion of the aortic valve aneurysm and obstruction of the LV outflow tract (Fig. 1B). Compared to previous TTE findings [LV end-diastolic dimension of 59 mm, moderate-to-severe AR, and maximal pressure gradient (max PG) of 31 mmHg] obtained 1 month before admission, exacerbation of LV size (LV end-diastolic dimension: 66 mm), severity of AR (severe AR, Fig. 1C), and subaortic obstruction (max PG: 52 mmHg, Fig. 1D) was observed. However, no vegetation was found by TTE and TEE. Cardiac computed tomography clearly depicted anatomical interactions among the right coronary cusp aneurysm, right coronary artery and LV outflow tract (Fig. 2). After treatment using loop diuretics and a vasodilator (i.e. carperitide), surgical treatment of the aortic valve and aneurysm was performed. The markedly enlarged right coronary cusp was removed to repair the LV outflow tract obstruction, and the aortic valve was replaced by a prosthetic valve. Macrographically, the resected right coronary cusp aneurysm was membranous and perforated (Fig. 3A), but there was no rheumatoid reaction, valvular sclerosis, vegetation, or destructive changes of the aortic valve. Histological examinations revealed severe hyalinization but no active inflammatory changes, suggesting healed infective endocarditis (Fig. 3B).
Fig. 1.
Images of transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE). On the TTE (A) and TEE (B), aneurysmal enlargement of coronary cusp (white arrows) that extended from the right coronary cusp to the outflow tract of left ventricle was identified. A severe aortic regurgitation was demonstrated by TTE with color Doppler echocardiography (C). A significant pressure gradient (52 mmHg) due to the aortic valve aneurysm in the left ventricular outflow tract was demonstrated by continuous wave Doppler echocardiography (D). LA, left atrium; LV, left ventricle; RCC, right coronary cusp; RV, right ventricle.
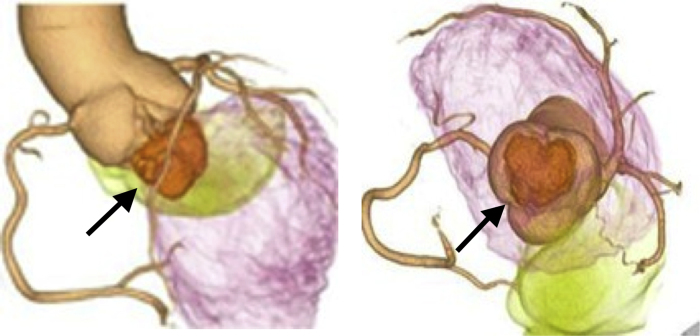
Fig. 2.
Images of cardiac computed tomography (CT). CT demonstrated the anatomical interaction among the right coronary cusp aneurysm (black arrows), right coronary artery and left ventricular outflow tract.
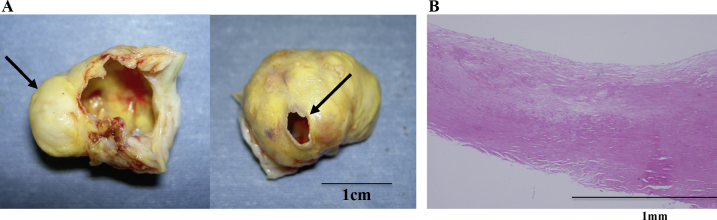
Fig. 3.
Macroscopic (A) and microscopic (B) demonstrations of surgically resected right coronary cusp aneurysm. The resected right coronary cusp aneurysm was membranous and perforated (A, black arrows). Histological examinations revealed severe hyalinization, however, no active inflammatory changes were demonstrated (B).
Discussion
An aortic valve aneurysm is much less frequent than a mitral valve aneurysm and is an uncommon complication of infective endocarditis [1]. Furthermore, the aortic valve aneurysm in this patient had not only perforated into the left ventricle and exacerbated AR, but also caused LV outflow obstruction, both of which resulted in the progression of congestive heart failure. The trigger of the acute congestive heart failure is unknown, but incarceration of the aortic valve aneurysm into the LV outflow tract may explain the hemodynamic deteriorations. Although active infective reactions were not identified in this case, histological examinations suggested healed infective endocarditis. Infective endocarditis is the most frequent cause of valvular aneurysm [2]; however, the mechanisms of aortic valve aneurysm have not been fully elucidated. The infective process of a cardiac valve is thought to augment pre-existing valvular tissue injury, involving aortic root or coronary cusp and then resulting in aneurysmal formation and perforation of the valvular aneurysm [3]. Hemodynamic deteriorations due to AR and subaortic obstruction may have facilitated the aneurysm formation. Table 1 summarizes clinical backgrounds and etiologies of tricuspid aortic valve aneurysm in 22 previously reported cases 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, including the present case. Most of the patients were male (82%) and had suspected or confirmed infective endocarditis (86%) responsible for the aortic valve aneurysm. All the patients had AR (100%), but subaortic stenosis or outflow obstruction of the left ventricle was a rare complication (9%).
Table 1.
Previous case reports of patients with tricuspid aortic valve aneurysm.
| No. | Age/sex | Location of aortic valve aneurysm | Backgrounds | Mitral valve involvement | Clinical manifestations | References |
|---|---|---|---|---|---|---|
| 1 | 40/F | LCC (+NCC) | IE | No | AR | Fujiwara et al. [4] |
| 2 | 46/M | NCC | IE | No | AR | Morimoto et al. [3] |
| 3 | 49/M | Unknown | IE | No | AR | Aokage et al. [5] |
| 4 | 44/M | RCC | Unknown | No | AR | Nyui et al. [6] |
| 5 | 42/F | RCC | IE | No | AR | Abe et al. [7] |
| 6 | 49/M | RCC | IE | No | AR | Iemura et al. [8] |
| 7 | 33/M | LCC | Unknown | No | AR | Kinoshita et al. [9] |
| 8 | 60/M | LCC | IE | Present | AR + MR | Kinoshita et al. [9] |
| 9 | 22/M | NCC | IE | Present | AR + MR | Kinoshita et al. [9] |
| 10 | 63/M | LCC | IE | No | AR | Plein et al. [10] |
| 11 | 57/M | RCC | IE | Present | AR + MR | Harada et al. [11] |
| 12 | 58/M | LCC | IE | No | AR | Nakayama et al. [1] |
| 13 | 51/M | LCC | RA | No | AR | Alpaslan et al. [12] |
| 14 | 42/M | RCC | IE | Present | AR + MR | de Castro et al. [13] |
| 15 | 35/F | RCC | IE | Present | AR + MR | de Castro et al. [13] |
| 16 | 49/F | LCC | Healed IE | No | AR | Scholte et al. [14] |
| 17 | 54/M | LCC | Unknown | No | AR + AS | Matsukuma et al. [2] |
| 18 | 49/M | NCC | IE | No | AR | Wojciuk et al. [15] |
| 19 | 53/M | NCC | IE | No | AR | Zhang et al. [16] |
| 20 | 71/M | NCC | Healed IE | No | AR | Naraoka et al. [17] |
| 21 | 30/M | NCC | IE | Present | AR + MR | Azevedo et al. [18] |
| 22 | 73/M | RCC | Healed IE s/o | No | AR + AS | Presented case |
AR, aortic regurgitation; AS, aortic stenosis; IE, infective endocarditis; LCC, left coronary cusp; MR, mitral regurgitation, NCC, noncoronary cusp; RCC, right coronary cusp; RA, rheumatoid arthritis.
In conclusion, we report an uncommon case of aortic valve aneurysm that was histologically suggested to be caused by subclinical infective endocarditis. The subaortic stenosis and AR, which were exacerbated by the aneurysm formation and were responsible for acute congestive heart failure, were successfully treated using a surgical procedure.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We are grateful to Hideki Okinaka, MT, Naoko Kohata, MT, Keiko Odawara, MT and Rumi Hayashi, MT for their assistance in echocardiographic examinations.
References
- 1.Nakayama M., Isobe F., Yutani C. Aneurysmal pouch on left coronary cusp accompanied by bacterial endocarditis. Jpn J Thorac Cardiovasc Surg. 1998;46:667–670. doi: 10.1007/BF03217800. [DOI] [PubMed] [Google Scholar]
- 2.Matsukuma S., Eishi K., Yamachika S., Hayashi T., Hazama S., Yamaguchi H., Ariyoshi T., Takai H., Odate T., Onohara D., Yanatori M. Saccular aneurysm of the aortic cusp associated with discrete subaortic stenosis. Ann Thorac Surg. 2005;80:2364–2365. doi: 10.1016/j.athoracsur.2004.07.041. [DOI] [PubMed] [Google Scholar]
- 3.Morimoto K., Matsuzaki M., Anno Y., Tanimoto Y., Kobayashi Y., Takashiba K., Yamagishi T., Kusukawa R. Echocardiographic assessment of aneurysm of the aortic valve caused by infective endocarditis. Jpn Circ J. 1989;53:819–824. doi: 10.1253/jcj.53.819. [DOI] [PubMed] [Google Scholar]
- 4.Fujiwara S., Arita M., Umemoto M., Ueno Y., Kuchii M., Nishio I., Masuyama Y., Kowazoe K. A case of infective endocarditis with aortic ring abscess and aneurysm of the aortic valve. Shinzo. 1987;19:602–609. (in Japanese) [Google Scholar]
- 5.Aokage K., Senoo Y., Yoshida H., Ooba O., Shiote A., Uchida T. A case of infective endocarditis with the myotic aortic valve aneurysm. Jpn Ann Thorac SurgRinsho Kyobu Geka. 1989;9:305–308. (in Japanese, abstract in English) [PubMed] [Google Scholar]
- 6.Nyui S., Inoue S., Sato T., Nakase A. Unruptured aneurysm of the right coronary cusp. Jpn Circ J. 1991;55:695–698. doi: 10.1253/jcj.55.695. [DOI] [PubMed] [Google Scholar]
- 7.Abe Y., Ebara K., Tanimoto T., Yamashita K. A case of aortic valve aneurysm caused by infective endocarditis. Jpn J Med Ultrasonics. 1991;20(Suppl.):241–242. (in Japanese, abstract in English) [Google Scholar]
- 8.Iemura J., Saga T., Oku H., Shirotani H., Naito T., Katori R. Aortic valve aneurysm due to infective endocarditis: a case report. J Cardiol. 1991;23(Suppl. 34):171–179. (in Japanese, abstract in English) [Google Scholar]
- 9.Kinoshita N., Ishiwata S., Nishiyama S., Kuwayama M., Iwase T., Nakanishi S., Seki A., Naruse Y., Makuuchi H., Hara M. Clinical analysis of infective endocarditis with aneurysmal formation of the mitral or aortic valve. J Cardiol. 1997;30:79–87. (in Japanese, abstract in English) [PubMed] [Google Scholar]
- 10.Plein D., Van Camp G., Derluyn M., Vandenbossche J.L. Aortic valve aneurysm after acute endocarditis. Clin Cardiol. 1997;20:969–970. doi: 10.1002/clc.4960201114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harada M., Hirai H., Inoue T., Sakai H., Lee T., Sugiyama Y., Suzuki M., Kamezaki M., Tamura S., Shiroma K., Ebine K., Takahashi K., Naoe S., Yamagichi T. Aortic and mitral valve aneurysms complicated with infective endocarditis: a case report. J Cardiol. 1998;31(Suppl. I):105–113. (in Japanese, abstract in English) [PubMed] [Google Scholar]
- 12.Alpaslan M., Evcik D., Onrat E. Aortic valve aneurysm: a novel cardiac manifestation of rheumatoid arthritis? J Am Soc Echocardiogr. 2001;14:1137–1138. doi: 10.1067/mje.2001.114446. [DOI] [PubMed] [Google Scholar]
- 13.de Castro S., Adorisio R., Pelliccia A., Papetti F., Fedele F., Pandian N.G. Perforated aneurysms of left side valves during active infective endocarditis complicating hypertrophic obstructive cardiomyopathy. Eur J Echocardiogr. 2002;3:100–102. doi: 10.1053/euje.2001.0123. [DOI] [PubMed] [Google Scholar]
- 14.Scholte A.J., Agema W.R., Poldermans D., Somer S.T., Holman E.R., van der Wall E.E., Bax J.J. Aortic valve regurgitation due to cusp aneurysm: a case report. Eur J Echocardiogr. 2004;5:231–236. doi: 10.1016/j.euje.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Wojciuk J., More R., Chauhan A. Tricuspid aortic valve aneurysms. Heart. 2005;91:1035. doi: 10.1136/hrt.2004.056796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang L., Nguyen J., Epelman S., Prichett A., Dokainish H. Enterococcal endocarditis presenting as an isolated aortic valve aneurysm: case report and review of literature. J Am Soc Echocardiogr. 2008;21(1391):e5–e6. doi: 10.1016/j.echo.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Naraoka S., Inoue S., Nakjima T., Niida Y. Aneurysm of the aortic cusp: report of a case. Jpn J Thorac SurgKyobu Geka. 2010;63:1164–1167. (in Japanese, abstract in English) [PubMed] [Google Scholar]
- 18.Azevedo O., Ferreira F., Guardado J., Duraes C., Quelhas I., Pereira A., Almeida J. Mitral and aortic valve aneurysms secondary to infective endocarditis: impressive images of a rare echocardiographic finding. Eur J Echocardiogr. 2010;11:E28. doi: 10.1093/ejechocard/jeq028. [DOI] [PubMed] [Google Scholar]