Abstract
Mesalamine has been successfully used as a maintenance treatment in inflammatory bowel diseases such as ulcerative colitis and Crohn's disease for years. Most frequent adverse reactions to this medication are gastrointestinal disorders and headaches while cardiovascular complications are rare and poorly understood. We present a case of a 26-year-old male with ulcerative colitis developing myopericarditis on mesalamine therapy. Although cardiac involvement is reported to be an extraintestinal manifestation of the bowel disease, we describe evidence confirming the diagnosis of mesalamine-induced myopericarditis in our patient and discuss other reports on this topic. Even though myopericarditis is an uncommon adverse reaction to mesalamine, it should be considered in patients with chest pain during mesalamine therapy. In such cases, drug withdrawal may result in rapid clinical improvement.
<Learning objective: Mesalamine therapy of inflammatory bowel disease (IBD) can be connected with common adverse reactions such as headaches and gastrointestinal problems. Cardiovascular complications in patients with IBD may be associated with the disease but may also occur due to mesalamine therapy. Drug cessation is then sufficient to achieve clinical improvement.>
Keywords: Mesalamine, Ulcerative colitis, Myopericarditis, Drug adverse reaction
Introduction
Among anti-inflammatory drugs used to suppress inflammatory bowel diseases (IBD) such as ulcerative colitis (UC) and Crohn's disease, mesalamine (5-aminosalicylic acid, 5-ASA) is a common agent. The efficacy of this nonsteroidal compound is attributed to the way it interferes with the cyclooxygenase pathway and the signaling pathway of γ-form of peroxisomal proliferator-activated receptors, although the exact mechanisms are not established [1]. The basis of mesalamine-induced cardiological adverse reactions is also not fully understood yet. They occur rarely and present mainly as pericarditis 2, 3, which can be also an extraintestinal manifestation of IBD. We present a case of myopericarditis in a 26-year-old patient as an undesirable effect of mesalamine therapy.
Case report
This is a case of a 26-year-old male with 1-month history of UC diagnosed on the basis of endoscopic and histopathologic results. He was initially placed on mesalamine 500 mg three times a day and prednisone 50 mg per day. Two weeks after introduction of the therapy, the patient started to suffer from myalgia, joint pain, and overall fatigue. Therefore, he decided to discontinue the mesalamine treatment.
Drug withdrawal resulted in an exacerbation of the UC that entailed admission to the Gastroenterology Department where mesalamine was readministered.
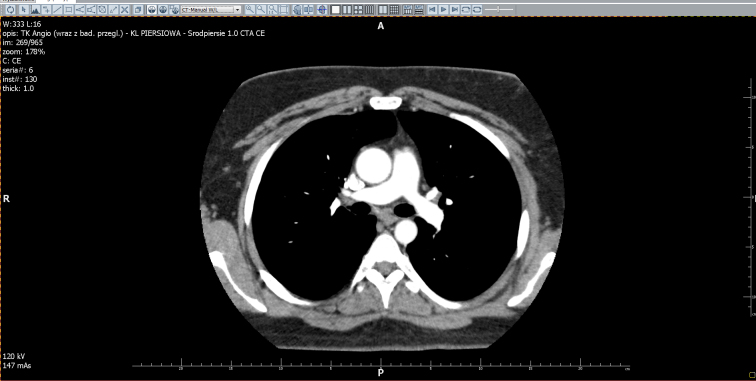
On the third day of mesalamine remedication, the patient developed acute, stabbing chest pain that intensified together with breathing movements. An episode of syncope was also reported. Body temperature was elevated to 37.3 °C. Initial chest radiograph and electrocardiogram (ECG) did not reveal any abnormalities (Fig. 1A). During the following 2 days, the pain did not resolve and it evolved into a constant feeling of chest pressure and tightness. Succeeding ECG revealed sinus tachycardia with T-wave inversion in the limb leads (II, III, aVF) (Fig. 1B). Troponin I concentration was 1.218 ng/mL (reference value: 0.0–0.014 ng/mL) and creatine kinase-MB (CK-MB) concentration was 3.7 ng/mL (reference value: 0.0–4.0 ng/mL) and they subsequently increased up to 2.686 ng/mL and 7.4 ng/mL, respectively. Regarding an elevated D-dimer concentration: 1960.22 ng/mL (reference value: <500 ng/mL), chest computed tomographic angiography was performed to exclude pulmonary embolism (Fig. 2). The results were negative and no pericardial effusion was detected. At that moment the patient was sent to our clinic for further evaluation and treatment.
Fig. 1.
The electrocardiogram course. (A) Off mesalamine (28.11); (B) On mesalamine (01.12); (C) On mesalamine (03.12); (D) Off mesalamine (08.12).
Fig. 2.
Computed tomographic angiography excluded pulmonary embolism.
On admission, he presented with substernal chest pain along with pulse rate of 115 beats per minute and systolic/diastolic blood pressure 90/65 mmHg. No other significant findings were noted. Laboratory tests showed elevated levels of cardiac enzymes: Troponin T concentration was 164.8 ng/L and peaked at 232.3 ng/L (reference value: 0.0–14.00 ng/L) and CK-MB concentration was 37 U/L (reference value 0.0–25.0 U/L). White blood cell count was 12.04/μL and C-reactive protein (CRP) level reached 208.6 mg/L.
ECG revealed sinus tachycardia with PQ-segment depression in the limb leads (II, III, aVF) and ST-segment elevation in the precordial leads (V2–V6) (Fig. 1C). In order to exclude the diagnosis of acute coronary syndrome, coronary angiography was performed and showed normal coronary vessels. The echocardiographic evaluation discovered an atrial septal defect with left to right shunt, but did not confirm either left ventricle systolic dysfunction or any pericardial effusion (Fig. 3).
Fig. 3.
Echocardiogram on admission showed no pericardial effusion.
A diagnosis of myopericarditis was settled based on the presence of the typical chest pain associated with PQ-segment depression, ST-segment elevation, and elevated levels of cardiac enzymes in the absence of coronary artery disease. As mesalamine seemed to be the most probable cause of this feature, its administration was ceased. The drug withdrawal resulted in rapid clinical improvement, resolution of the ST-segment elevation (Fig. 1D) and decline in cardiac enzymes, WBC count, and CRP level (Table 1). Within 3-months follow-up since hospital discharge, there has not been any recurrence of the symptoms.
Table 1.
Correlation between clinical data and mesalamine administration.
| Date |
|||||
|---|---|---|---|---|---|
| 28.11 | 1.12 | 3.12 | 5.12 | 8.12 | |
| Mesalamine | + | + | + | − | − |
| Symptoms | None | Chest pain | Chest pain | None | None |
| WBC count/μL | 9540 | 12,040 | 10,800 | 7600 | 6000 |
| CRP (mg/L) | 26 | 208.6 | 154.8 | 58 | 17.6 |
| hsTnT (ng/L) | – | 164.8 232.3 |
183.2 | 125.7 | 83.31 |
WBC, white blood cell; CRP, C-reactive protein; hsTnT, troponin T.
Discussion
The essence of IBD is gastrointestinal tract involvement but the disease may manifest in several other organs simultaneously or independently of the disease activity. Apart from the main intestinal localization, it seldom affects the cardiovascular system, but common clinical manifestations include pericarditis, myocarditis, myopericarditis, cardiac tamponade, pericardial effusion, conductibility disorders, arrhythmias, and systemic thromboembolism 1, 2, 4, 5. However, settling the diagnosis of extraintestinal manifestation of IBD requires rigorous evaluation and succeeding exclusion of other possible causes. Most of the reported cases so far have attributed cardiac symptoms to either an autoimmune disease associated with bowel disease or an adverse effect of the therapy, emphasizing that the exact differentiation is often difficult to achieve 6, 7.
Mesalamine-containing products are reported to cause myo- and pericarditis. It has not been definitely established yet whether 5-ASA itself or its derivatives were accountable for cardiac involvement as it was observed in patients on both types of the therapy 3, 8. Suggested mechanisms include direct cardiotoxicity or hypersensitivity reactions type I, III, or IV [3]. Considering the fact that 5-ASA intake can induce other hypersensitive reactions involving skin, joints, eyes, and lungs, this mechanism rather than direct toxicity seems to be the most likely cause. The improvement obtained after the drug withdrawal and the evident recurrence of symptoms after its readministration also suggest the above explanation.
In the current report, we presented a case of a 26-year-old male developing acute myopericarditis on mesalamine therapy. His first symptoms following mesalamine introduction involved joint pains and mood alteration that could also be specified as drug side effects and suggested undesirable reaction to the treatment at its early stage. All the complaints resolved as soon as the therapy was ceased. Remedication evoked substernal pain. Its characteristics and concomitant laboratory test results induced specific diagnostic procedures to exclude pulmonary embolism. Due to the fact that IBD is mostly connected with plasmatic hypercoagulation and thus predisposing to thrombotic events, it seemed essential for ruling out such differential diagnosis. Further evaluation led to the diagnosis of pericarditis and suggested mesalamine to be the most probable cause of the patient's clinical overall outcome. Elevated levels of troponin and CK-MB without significant echocardiographic findings indicated slight myocardial injury that did not impair left ventricle systolic function. Negative coronarography may suggest myocarditis to be responsible for such results. An evident time relation between occurrence of symptoms and 5-ASA intake was observed in our case like others previously reported 6, 7. Drug withdrawal was sufficient to elicit rapid clinical improvement in the cardiac function.
In conclusion, our case reports myopericarditis observed in a patient with UC on 5-ASA therapy. Although the exact mechanisms remain unknown, the presented connection between medication use and cardiac complications makes the diagnosis of mesalamine-induced myopericarditis reliable. IBD, especially treated with mesalamine, should be followed by thoughtful observation and quick evaluation for possible cardiac injury, regardless of the final most probable etiology – an extraintestinal manifestation or drug adverse reaction.
Funding sources
None declared.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Perez-Colon E., Dadlani G.H., Wilmot I., Miller M. Mesalamine-induced myocarditis and coronary vasculitis in a pediatric ulcerative colitis patient: a case report. Case Rep Pediatr. 2011;2011:524364. doi: 10.1155/2011/524364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cappel M.S., Turkieh A. Chronic pericarditis and pericardial tamponade associated with ulcerative colitis. Dig Dis Sci. 2008;53:149–154. doi: 10.1007/s10620-007-9836-y. [DOI] [PubMed] [Google Scholar]
- 3.Sentongo T.A., Piccoli D.A. Recurrent pericarditis due to mesalamine hypersensivity: a pediatric case report and review of the literature. J Pediatr Gastroenterol Nutr. 1998;27:344–347. doi: 10.1097/00005176-199809000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Triantafillidis J.K., Cheracakis P., Mylonaki M., Georgopoulos F., Panteris V., Malgarinos G., Malli C., Fouskas J. Myocarditis due to mesalamine treatment in a patient with ulcerative colitis: favorable outcome after infliximab treatment. Ann Gastroenterol. 2009;22:62–64. [Google Scholar]
- 5.Kafkas N.V., Deboneras C.C., Babalis D.K. Massive pulmonary embolism and ulcerative colitis. Hell J Cardiol. 2008;49:365–370. [PubMed] [Google Scholar]
- 6.Atay O., Radhakrishnan K., Arruda J., Wyllie R. Severe chest pain in a pediatric ulcerative colitis patient after 5-aminosalicylic acid therapy. World J Gastroenterol. 2008;14:4400–4402. doi: 10.3748/wjg.14.4400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park E.H., Kim B.J., Huh J.K., Jeong E.H., Lee S.H., Bang K.B., Seol J.S., Sung J.W., Kim B.S., Kang J.H. Recurrent mesalazine-induced myopericarditis in a patient with ulcerative colitis. J Cardiovasc Ultrasound. 2012;20:154–156. doi: 10.4250/jcu.2012.20.3.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adhiyaman V., Vaishnavi A., Froese S. Drug points: hypersensitivity reaction to balsalazide. BMJ. 2001;323:489. doi: 10.1136/bmj.323.7311.489. [DOI] [PMC free article] [PubMed] [Google Scholar]