Abstract
Introduction
Systemic venous circulation anomalies are uncommon; they are often incidental findings during echocardiography.
Case
A 56-year-old man, with dextrocardia, was evaluated for dyspnea. The patient's medical history included diabetes mellitus requiring insulin treatment, hypertension, and tobacco use. Physical examination revealed normal jugular venous pulsations and clear lungs. Cardiac examination revealed normal heart sounds, and grade II/VI systolic ejection murmur over the right precordium. Echocardiography revealed normal chamber size and systolic function, without significant valvular lesions. The coronary sinus was dilated. It was evaluated using intravenous agitated saline contrast to rule out anomalous venous drainage or shunting. When injected into the left antecubital vein, contrast appeared initially in the right atrium followed by the right ventricle. However, when injected into the right antecubital vein, contrast appeared initially in the dilated coronary sinus followed by the right atrium and right ventricle. There was no evidence of intracardiac shunting. These findings were consistent with persistent right superior vena cava in the setting of situs inversus dextrocardia, with normally draining left superior vena cava.
Conclusion
Persistent superior vena cava connection to the coronary sinus is often incidental but an important finding which helps in planning safe invasive procedures.
<Learning objective: Understand the importance of identifying anomalous venous connections with regard to catheter-based procedures. Appreciate the incidence of these vascular anomalies in the normal population and in congenital heart disease. Understand how echocardiography with intravenous agitated saline contrast can be helpful in the diagnosis of such anomalous venous connections.>
Keywords: Dextrocardia, Anomalous venous connections, Echocardiography
Introduction
Anomalies of the systemic venous circulation are not uncommon in patients with congenital heart disease, and can pose a risk if unrecognized prior to diagnostic or therapeutic catheter procedures requiring the use of systemic veins. We present a case of a 56-year-old man with dextrocardia and situs inversus who was found to have a persistent right superior vena cava (PRSVC) by 2D echocardiography using intravenous agitated saline contrast performed to evaluate his dilated coronary sinus.
Case report
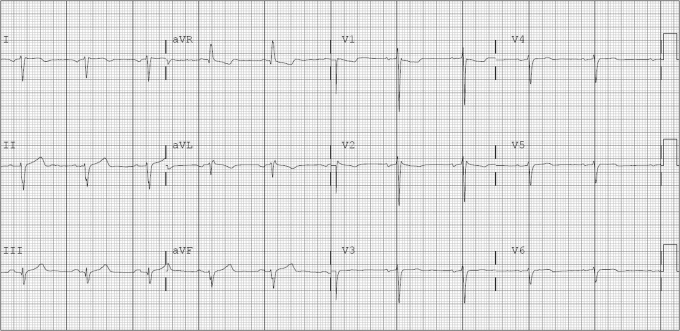
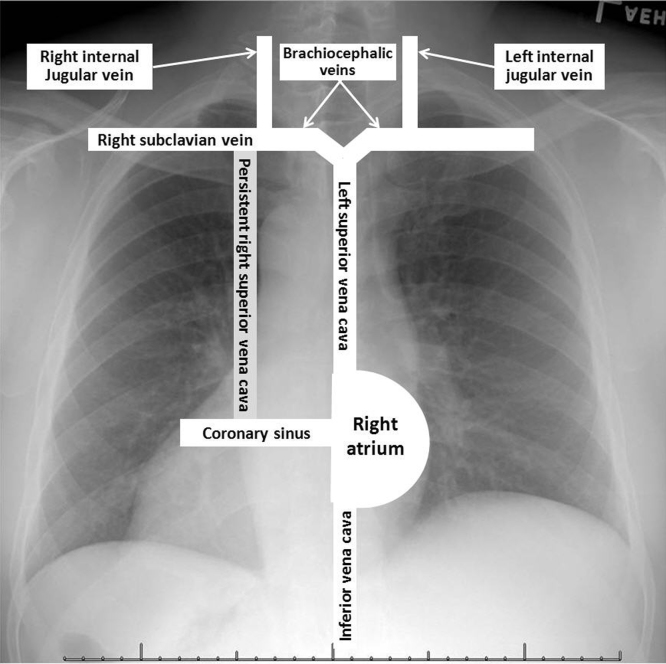
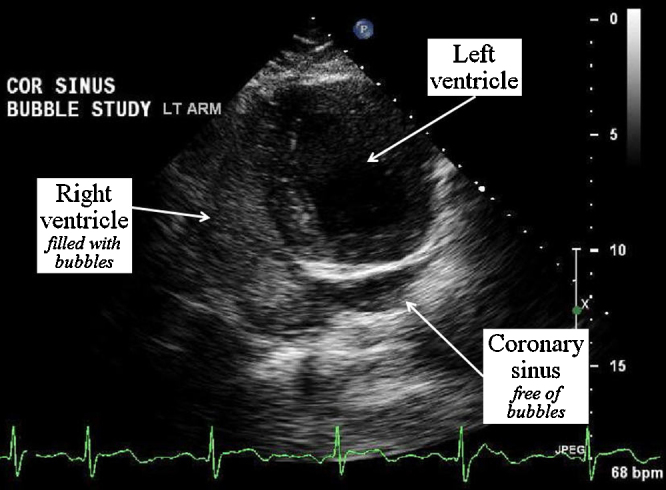
A 56-year-old man, with situs inversus dextrocardia, was evaluated for dyspnea. The patient's medical history included diabetes mellitus requiring insulin treatment, hypertension, and tobacco use. Physical examination revealed normal jugular venous pulsations and clear lungs. Cardiac examination revealed normal right-sided point of maximal impulse, normal heart sounds, and grade II/VI systolic ejection murmur over the right precordium. Electrocardiogram revealed sinus rhythm and dextrocardia, without ischemia (Fig. 1). Chest X-ray revealed no acute pathology (Fig. 2). Cardiac catheterization revealed normal coronary arteries and normal ejection fraction. Echocardiography revealed normal chamber size and left ventricular systolic function, without significant valvular lesions. There was an incidental dilated coronary sinus (Fig. 3), which was evaluated using intravenous (IV) agitated saline contrast to rule out anomalous venous drainage or shunting. When injected into the left antecubital vein, the contrast appeared initially in the right atrium followed by the right ventricle (Fig. 4). However, when injected into the right antecubital vein, the contrast appeared initially in the dilated coronary sinus followed by the right atrium and right ventricle (Fig. 5). There was no evidence of intracardiac shunting. These findings were consistent with persistent right superior vena cava in the setting of situs inversus dextrocardia, with normally draining left superior vena cava. Due to the absence of an obvious cardiac cause of his dyspnea and his tobacco use history, pulmonary function tests were performed, which revealed moderate restrictive lung disease and increase in airway resistance. This was thought to explain his symptoms; therefore, pulmonary clinic follow-up was arranged for further diagnosis and therapy.
Fig. 1.
Electrocardiogram showing sinus rhythm with features of dextrocardia.
Fig. 2.

Chest X-ray with situs inversus dextrocardia showing part of the stomach air on the right side.
Fig. 3.
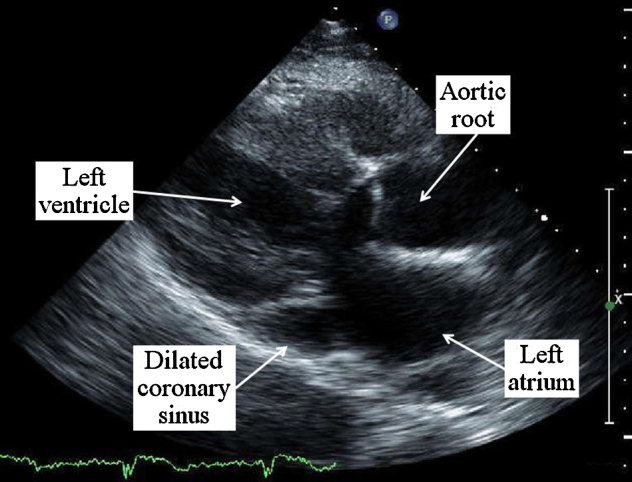
Parasternal long-axis 2D echocardiographic view showing the dilated coronary sinus, which measured 2.5 cm in transverse diameter.
Fig. 4.
Apical four-chamber view angled to reveal the coronary sinus following injection of intravenous agitated saline in the left arm. Note the appearance on the contrast in the right atrium and right ventricle without opacification of the coronary sinus, indicating normal drainage of the left superior vena cava into the right atrium.
Fig. 5.
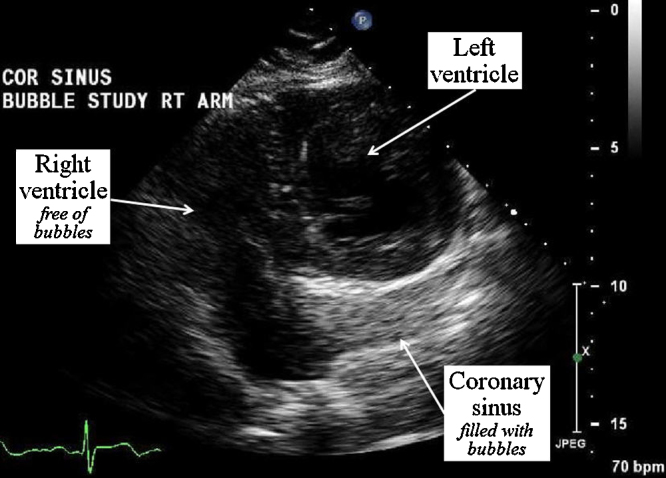
Apical four-chamber view angled to reveal the coronary sinus following injection of intravenous agitated saline in the right arm. Note the appearance on the contrast in the coronary sinus before opacification of the right atrium and right ventricle, indicating anomalous drainage of the right superior vena cava into the coronary sinus.
Discussion
Anomalous connection of systemic venous circulation to the coronary sinus has been previously reported. The most common is a persistent left superior vena cava (PLSVC), which has been reported in approximately 0.5% of the general population, and about 3–10% in patients with congenital heart disease [1]. These anomalies are usually asymptomatic and are discovered incidentally. They have also been reported in patients with dextrocardia, a rarer anomaly in itself. Reports of PLSVC, in addition to pertinent studies of anomalous superior vena cava connections in dextrocardia, will be reviewed to demonstrate the clinical implications of these often incidental findings, especially in relation to catheter-based procedures. The following four case reports will demonstrate the difficulties encountered during pacemaker insertion, and central venous line and Swan–Ganz placement in patients with previously unrecognized PLSVC.
Bhatti and colleagues [2] reported a PLSVC draining into a dilated coronary sinus, associated with anomalous left hepatic vein drainage into the right atrium, in an 86-year-old man undergoing pacemaker implantation for complete heart block. The left subclavian approach had to be abandoned due to difficulty in inserting the pacing catheter, and a right subclavian approach was successful. The diagnosis was confirmed by echocardiography with agitated saline and coronal computed tomography (CT) of the chest with contrast.
Higgs et al. [3] described an anomalous course of a transvenous catheter inserted through the external jugular vein, corresponding to PLSVC course, in a 3-year-old boy requiring venous access for the treatment of scald injury complicated by disseminated intravascular coagulation. The course of the catheter was confirmed with echocardiography; the catheter was retracted to avoid irritation of the coronary sinus and was successfully used for total parenteral nutrition administration.
Goyal et al. [4] reported the case of a 19-year-old man with a motor vehicle accident who was incidentally found to have a dilated coronary sinus on echocardiography. A Swan–Ganz catheter inserted via the left subclavian approach was shown to pass through the coronary sinus by echocardiography. A contrast-enhanced CT study of thorax performed to assess the bone and vascular injuries associated with the motor vehicle accident also revealed PLSVC as an incidental finding.
Walpot et al. [5] reported a case of a 29-year-old man who underwent an emergent laparotomy for multiple intra-abdominal abscesses complicated by sepsis. Postoperatively the tip of a central line catheter inserted through the left subclavian vein was in a left paramediastinal position on chest X-ray, instead of crossing the midline to the superior vena cava. A transthoracic echocardiography study performed after injection of agitated saline in the catheter showed opacification of the coronary sinus, the right atrium, and the right ventricle, confirming the diagnosis of PLSVC.
Next, the seven case reports and case series in which the incidental finding of PLSVC was made by diagnostic echocardiography, as in our patient, will be discussed to demonstrate associated findings and for additional help in testing.
Stoevesandt and colleagues [6] reported a 42-year-old man with primary sclerosing cholangitis and colitis ulcerosa, screened for liver transplantation, who was found to have a dilated coronary sinus by echocardiography. The diagnosis of PLSVC draining into a dilated coronary sinus was made by cardiac magnetic resonance imaging (MRI).
Kong and Ahmad [7] reported the case of a 65-year-old woman with hemoptysis due to chest infection. Transthoracic echocardiography showed dilated atria, right ventricle, and main pulmonary artery; volume overload with diastolic flattening of the interventricular septum was noted. Left-to-right shunting from the left atrium into a dilated unroofed coronary sinus was seen. Agitated normal saline injected into the patient's left antecubital vein appeared in the coronary sinus before appearing in the right heart thus confirming a PLSVC. On transesophageal echocardiography, the right pulmonary veins were noted to drain into the superior vena cava, while the left pulmonary veins drained normally.
Guarnieri et al. [8] reported two cases of echocardiographic diagnosis of the absence of the right superior vena cava, with PLSVC and a large coronary sinus in structurally normal heart in a fetus of 20 weeks’ gestation and in a newborn. Upon injection of agitated saline into the right antecubital vein in the newborn, apical four-chamber views showed earlier enhancement of the dilated coronary sinus than the right cardiac chambers. Similar findings after birth confirmed PLSVC in the fetus.
El-Chami et al. [9] reported the case of a 64-year-old woman with progressive shortness of breath who was found to have preserved ejection fraction with marked pulmonary hypertension and severe decrease in right ventricular function by echocardiography. An incidental finding was a dilated coronary sinus. Right heart catheterization and pulmonary angiogram were done for further diagnostic and therapeutic purposes, revealing pruning of the distal vessels consistent with thromboembolic disease. Cannulation and dye injection of the coronary sinus revealed the presence of the incidental PLSVC.
Recupero et al. [10] used contrast echocardiography to demonstrate PLSVC in five patients; the results were confirmed by multislice CT (MCT) or MRI. Four patients revealed contrast appearing first in the coronary sinus after either right or left antecubital injection. These were all shown to have agenesis of the right superior vena cava in addition to PLSVC. The last patient had contrast appearing in the coronary sinus after left antecubetal injection and in the right atrium after right antecubital injection, and was confirmed to have PLSVC associated with right superior vena cava by MCT.
Gonzalez-Juanatey et al. [11] reported 10 cases of PLSVC draining into the coronary sinus diagnosed by transthoracic echocardiogram using echo-contrast enhancement and confirmed by MRI. Three cases were associated with other congenital heart disease including secundum atrial septal defect (ASD), sinus venosus ASD, and severe aortic coarctation. The remaining seven cases were associated with arrhythmia, ischemia, or hypertensive heart disease. In three cases, the right superior vena cava was absent and demonstrated a significant increase in the size of the main coronary sinus.
Hsiao et al. [12] reported four cases of PLSVC diagnosed by contrast echocardiography, transesophageal echocardiography and later confirmed by invasive angiography. They demonstrated 100% diagnostic accuracy with contrast echocardiography using three criteria: (1) dilated coronary sinus in parasternal long-axis view; (2) enhancement of the dilated coronary sinus earlier than the right cardiac chambers after contrast infusion into the left arm; (3) enhancement of the right cardiac chambers earlier than the dilated coronary sinus after contrast infusion into the right arm vein.
Rigatelli [13] reviewed the embryogenesis and diagnostic modalities of PLSVC. The author discussed the related technical problems in the face of invasive cardiovascular procedures, taking into consideration the points of view of anesthesiologists (placement of central vein lines), nephrologists (placement of noncuffed dialysis catheters), electrophysiologists (insertion of right or left ventricular pacemaker leads), invasive/interventional cardiologists (right heart catheterization and placement of ASD closure devices), and cardiothoracic surgeons (use of retrograde cardioplegia and in cardiac transplantation). The author concluded that the recognition of PLSVC before invasive medical–surgical procedures is important in order to avoid medical errors, lost time, and poor results.
Dextrocardia is a rare condition, which often coexists with other congenital anomalies. Bohun et al. [14] reported the prevalence of dextrocardia to be 1 in 12,019 pregnancies. The most prevalent configuration, also corroborated by Garg et al. [15], was situs inversus, which was defined as a left inferior vena cava and a left superior vena cava connecting to the systemic right atrium on the left side of the heart, with a left-sided liver and a right-sided stomach. Situs inversus was also associated with the least cardiac and noncardiac pathology. Few reports of anomalous venous connections in patients with dextrocardia have been published. The following most pertinent five case reports will demonstrate incidentally found anomalous venous connection and associated lesions in patients with dextrocardia during diagnostic or therapeutic procedures.
Murayama et al. [16] reported the case of a 5-year-old girl with progressive cyanosis who had situs inversus dextrocardia with other complex congenital heart anomalies. She was found to have a PRSVC draining into the left-sided right atrium via the coronary sinus, with an absent left superior vena cava.
Nakagawa et al. [17] reported the case of a 56-year-old woman with known situs inversus admitted with dyspnea due to congestive heart failure caused by severe biatrioventricular valve regurgitation. Transesophageal echocardiography and cardiac MRI performed in preparation for surgery revealed the presence of a PRSVC draining into the left atrium via a dilated coronary sinus.
Pott et al. [18] reported the case of a 40-year-old man with dextrocardia and idiopathic dilated cardiomyopathy requiring implantation of a biventricular pacemaker-defibrillator. His left superior vena cava was found to be draining into the coronary sinus, which caused difficulties with multiple lead insertions to the right atrium, right ventricle, and into a left ventricular branch of the dilated coronary sinus, using selective angiography.
Manohar and Tharakan [19] reported a 3-year-old woman with dextrocardia and total anomalous pulmonary venous connection to the coronary sinus, who presented with recurrent respiratory infections and delayed development. Echocardiography revealed normal atrial situs with dextroversion, all four pulmonary veins draining into a large coronary sinus, secundum ASD, and mild pulmonary hypertension. PLSVC draining into the coronary sinus was identified by cardiac catheterization, necessitating the use of the right superior vena cava for central venous access during surgery.
Tripathi et al. [20] reported a 37-year-old man with situs solitus dextrocardia who underwent pulmonary artery catheter insertion in preparation for mitral valve replacement. The patient suffered severe mitral regurgitation following a failed balloon valvotomy for rheumatic mitral valve stenosis associated with pulmonary hypertension. The catheter was introduced through the right internal jugular vein; however, it was shown to take the path of a left-sided superior vena cava which drained into the inferior vena cava. The long course before pulmonary artery pressure waveform was obtained prevented the catheter from wedging, and raised an initial fear of catheter coiling.
The above discussion underscores the importance of identifying anomalous venous drainage especially with regard to catheter-based procedures. In most reports, as in our patient, an incidental finding of a dilated coronary sinus raised the suspicious of an anomalous venous connection, especially PLSVC, to the coronary sinus. Our patient had dextrocardia with clinical features compatible with situs inversus, which is expected to have a left superior vena cava connecting to the systemic right atrium on the left side of the heart [14]. This was demonstrated by the appearance of IV agitated saline contrast through his left arm directly into the right atrium. The appearance of the IV agitated saline injected through his right arm initially into the coronary sinus, however, was indicative of a PRSVC. PRSVC is anticipated to start at the junction of the right subclavian vein and right internal jugular vein and drain into the coronary as illustrated in the diagrammatic overlay in Fig. 6. It is thought to be due to a lack of obliteration of the right anterior cardinal vein during normal fetal development. Our patient the three contrast echocardiography criteria described by Hsiao et al. [12]; but modified to account for the dextrocardia. This incidental, seemingly benign, finding will be important if our patient is to require any diagnostic or therapeutic central venous access procedures in the future, which would have to be limited to his left superior vena cava, avoiding the anomalous connection of the right superior vena cava.
Fig. 6.
Chest X-ray from Fig. 2 with an overlay of a diagrammatic representation of the patient's anticipated major venous connections.
Sources of support
None.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Petronzelli S., Patruno N., Pontillo D. Persistent left superior vena cava: diagnosis with saline contrast echocardiography. Heart. 2008;94:835. doi: 10.1136/hrt.2007.120733. [DOI] [PubMed] [Google Scholar]
- 2.Bhatti S., Hakeem A., Ahmad U., Malik M., Kosolcharoen P., Chang S. Persistent left superior vena cava (PLSVC) with anomalous left hepatic vein drainage into the right atrium: role of imaging and clinical relevance. Vasc Med. 2007;12:319–324. doi: 10.1177/1358863X07084859. [DOI] [PubMed] [Google Scholar]
- 3.Higgs A., Paris S., Potter F. Discovery of left-sided superior vena cava during central venous catheterization. Br J Anaesth. 1998;81:260–261. doi: 10.1093/bja/81.2.260. [DOI] [PubMed] [Google Scholar]
- 4.Goyal S., Punnam S., Verma G., Ruberg F. Persistent left superior vena cava: a case report and review of literature. Cardiovasc Ultrasound. 2008;6:50. doi: 10.1186/1476-7120-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walpot J., Pasteuning W., Zwienen J. Persistent left superior vena cava diagnosed by bedside echocardiography. J Emerg Med. 2010;38:638–641. doi: 10.1016/j.jemermed.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 6.Stoevesandt D., Buerke M., Behrmann C., Heinroth K., Spielmann R., Werdan K., Schlitt A. Detection of a persistent left superior vena cava by echocardiography, computed tomography, and magnetic resonance imaging. Clin Res Cardiol. 2007;96:191–192. doi: 10.1007/s00392-007-0492-1. [DOI] [PubMed] [Google Scholar]
- 7.Kong P., Ahmad F. Unroofed coronary sinus and persistent left superior vena cava. Eur J Echocardiogr. 2007;8:398–401. doi: 10.1016/j.euje.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Guarnieri G., Romano F., Clerico L., Balducci G. Absent right and persistent left superior vena cava: fetal and neonatal echocardiographic diagnosis. Pediatr Cardiol. 2006;27:646–648. doi: 10.1007/s00246-005-1264-1. [DOI] [PubMed] [Google Scholar]
- 9.El-Chami M., Howell S., Martin R., Lerakis S. Dilated coronary sinus with a persistent left superior vena cava: echo and cath findings. J Echocardiogr. 2005;3:156–157. [Google Scholar]
- 10.Recupero A., Pugliatti P., Rizzo F., Carerj S., Cavalli G., Gregorio C., Bella G., Minutoli F., Arrigo F., Oreto G., Coglitore S. Persistent left-sided superior vena cava: integrated noninvasive diagnosis. Echocardiography. 2007;24:982–986. doi: 10.1111/j.1540-8175.2007.00509.x. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Juanatey C., Testa A., Vidan J., Izquierdo R., Garcia-Castello A., Daniel C., Armesto V. Persistent left superior vena cava draining into the coronary sinus: report of 10 cases and literature review. Clin Cardiol. 2004;27:515–518. doi: 10.1002/clc.4960270909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsiao S., Lee Hsu T., Mar G., Tseng C., Chiao C., Chiou C., Liu C., Chiang H. Diagnosis of an isolated persistent left side superior vena cava by contrast echocardiography compared with invasive angiographic study. Zhonghua Yi Xue Za Zhi (Taipei) 2002;65:320–325. [PubMed] [Google Scholar]
- 13.Rigatelli G. Congenitally persistent left superior vena cava: a possible unpleasant problem during invasive procedures. J Cardiovasc Med. 2007;8:483–487. doi: 10.2459/01.JCM.0000278448.89365.55. [DOI] [PubMed] [Google Scholar]
- 14.Bohun C., Potts J., Casey B., Sandor G. A population-based study of cardiac malformations and outcomes associated with dextrocardia. Am J Cardiol. 2007;100:305–309. doi: 10.1016/j.amjcard.2007.02.095. [DOI] [PubMed] [Google Scholar]
- 15.Garg N., Agarwal B., Modi N., Radhakrishnan S., Sinha N. Dextrocardia: an analysis of cardiac structures in 125 patients. Int J Cardiol. 2003;88:143–155. doi: 10.1016/s0167-5273(02)00539-9. [DOI] [PubMed] [Google Scholar]
- 16.Murayama H., Maeda M., Sakurai H., Watanabe T. Absent left superior vena cava with persistent right superior vena cava in visceroatrial situs inversus. Pediatr Cardiol. 2006;27:293–296. doi: 10.1007/s00246-005-1111-4. [DOI] [PubMed] [Google Scholar]
- 17.Nakagawa T., Tanouchi J., Nishino M., Ito T., Ohnishi S., Tanahashi H., Yamada Y., Abe H. Transesophageal echocardiography combined with magnetic resonance imaging for detecting venous anomalies in dextrocardia. A case report. Angiology. 1995;46:531–535. doi: 10.1177/000331979504600612. [DOI] [PubMed] [Google Scholar]
- 18.Pott C., Brar R., Valderrábano M. Implant of a biventricular pacemaker in a patient with dextrocardia and persistent left superior vena cava. Pacing Clin Electrophysiol. 2006;29:921–922. doi: 10.1111/j.1540-8159.2006.00462.x. [DOI] [PubMed] [Google Scholar]
- 19.Manohar S., Tharakan J. Anomalous systemic and pulmonary venous connections to coronary sinus. Asian Cardiovasc Thorac Ann. 1999;7:71–73. [Google Scholar]
- 20.Tripathi M., Kumar N., Singh P. Pulmonary artery catheter insertion in a patient of dextrocardia with anomalous venous connections. Indian J Med Sci. 2004;58:353–356. [PubMed] [Google Scholar]