Abstract
The present case report describes a 53-year-old man with drug-resistant heart failure. Electrocardiogram showed complete right-bundle branch block and left anterior fascicular block. A cardiac resynchronization therapy (CRT) device was implanted in him because echocardiography showed obvious left ventricular dyssynchrony between septal and lateral walls. After CRT implantation, dyssynchrony was improved and ejection fraction was increased. Evaluation of coexisting left hemiblock and left ventricular dyssynchrony may be needed in patients with atypical indications for CRT.
<Learning objective: Cardiac resynchronization therapy (CRT) for patients with complete right-bundle branch block (CRBBB) is still controversial. Presence of hemiblock and left ventricular dyssynchrony between the pacing sites may be essential to determine CRT indication even in patients with CRBBB.>
Keywords: Cardiac resynchronization therapy, Right-bundle branch block, Left anterior fascicular block
Introduction
Cardiac resynchronization therapy (CRT) has emerged as an effective therapy for drug-refractory congestive heart failure patients. Standard selection criteria for CRT include severe heart failure, systolic dysfunction, and a wide QRS complex on the surface electrocardiogram. However, CRT for patients with complete right-bundle branch block (CRBBB) is still controversial.
Case report
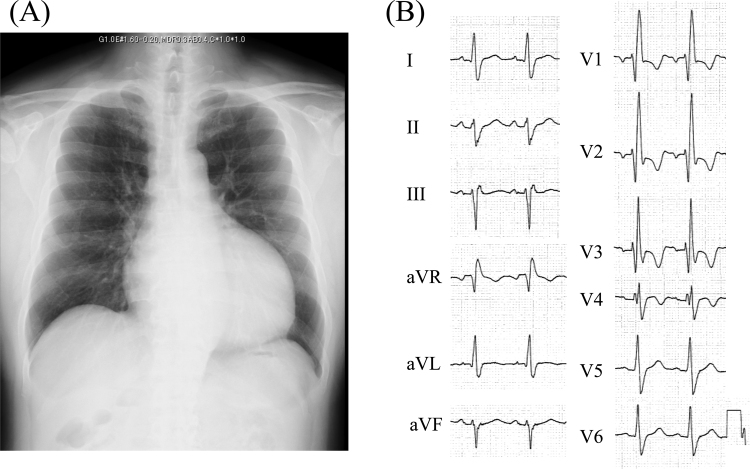
A 53-year-old man who experienced heart failure symptoms from the past 2 years previously had been admitted to hospital for congestive heart failure twice in the past year. Although optimal medical therapy including maximally tolerated doses of β-blockers, angiotensin II receptor antagonists, loop diuretics, spironolactone, and digitalis was taken, his symptoms were not improved. He was transferred to our hospital for further evaluation. On physical examination, his blood pressure was 94/76 mmHg, his pulse rate was 88 beats per minute, and his New York Heart Association functional class was at III. Laboratory evaluations revealed elevation of the plasma N-terminal pro B-type natriuretic peptide level. A chest radiograph showed cardiomegaly (Fig. 1A). The 12-lead electrocardiogram showed CRBBB and left anterior fascicular block morphology (Fig. 1B). A transthoracic echocardiography showed marked left ventricular (LV) dilatation with severe systolic dysfunction, an ejection fraction of 29%, and mild mitral regurgitation.
Fig. 1.
(A) Chest radiograph, and (B) electrocardiogram on admission.
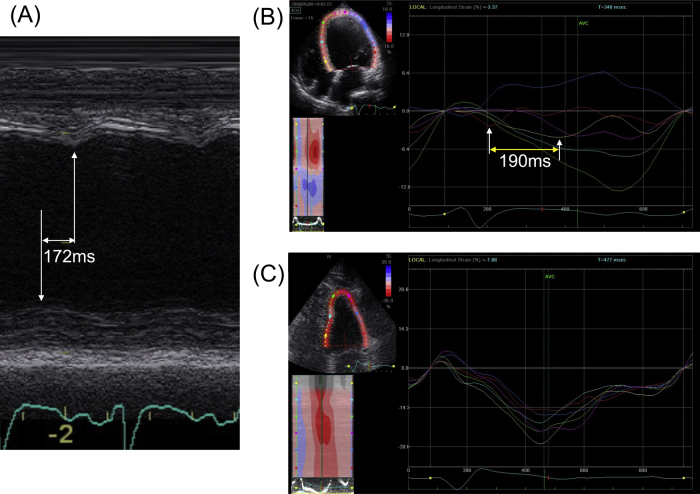
Echocardiographic dyssynchrony analysis was performed a Vivid 7 system (GE Vingmed Ultrasound, Horten, Norway) to evaluate the indication for CRT. In the M-mode image of the septal-to-posterior wall motion, posterior wall motion was paradoxically faster than septal wall motion (Fig. 2A). Similarly, speckle tracking echocardiography revealed obvious dyssynchrony between opposite walls, in which contraction may be modified by CRT (Fig. 2B) [1]. Coronary angiography revealed no significant stenotic lesion, and he was diagnosed as having nonischemic cardiomyopathy. Then, the patient was thought to be a CRT responder, and CRT-defibrillator (CRT-D) was selected due to episodes of non-sustained ventricular tachycardia. A CRT-D device was implanted according to a triangle ventricular pacing technique due to a markedly enlarged LV end-diastolic volume of 349 ml, i.e. conventional bi-ventricular pacing from the right ventricular (RV) apex and LV plus additional pacing from the RV outflow tract, using a Y connector to bifurcate the RV bipolar output of the device into an anode and a cathode [2]. The LV lead was placed in a lateral branch of the coronary sinus.
Fig. 2.
(A) M-mode recording showed that the septal-to-lateral wall motion delay was 172 ms, (B) the time difference of first peak on the radial strain–time curves between left ventricular basal septum portion and left ventricular lateral portion by speckle tracking echocardiography was 190 ms and (C) speckle tracking echocardiography revealed no dyssynchrony in left ventricle.
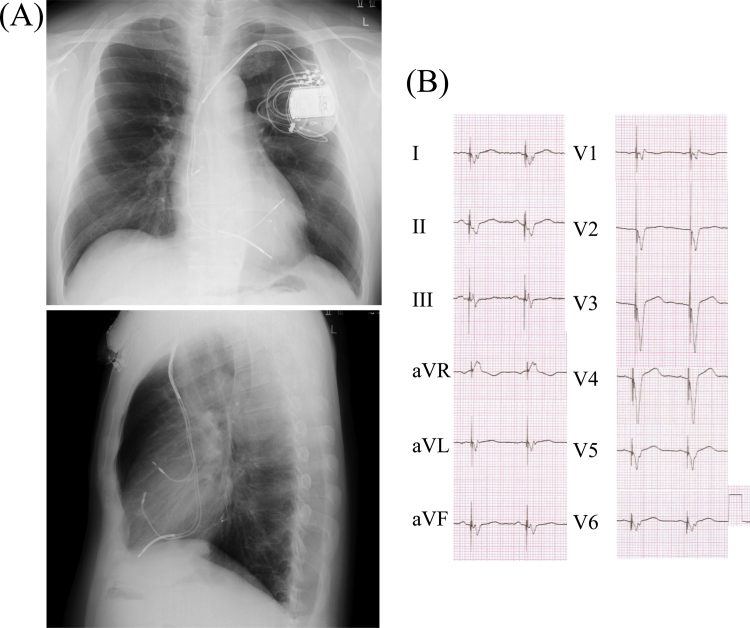
The New York Heart Association functional class immediately improved to class II after the CRT-D implantation. One year after the CRT-D implantation, the plasma N-terminal pro B-type natriuretic peptide level dropped from 2403 to 168 pg/ml, cardio-thoracic ratio decreased from 57% to 46% on the chest radiograph (Fig. 3A), and QRS duration decreased from 180 ms to 160 ms (Fig. 3B). Echocardiographic study also showed decreased LV end-diastolic/systolic volume from 349/248 ml to 139/71 ml, and LV ejection fraction was increased from 29% to 49%. Speckle tracking echocardiography obtained one year after CRT-D implantation showed more resynchronized wall motion (Fig. 2C).
Fig. 3.
(A) Chest radiograph (top: frontal view; and bottom: lateral view) and (B) electrocardiogram at one year after cardiac resynchronization therapy-defibrillator implantation.
Discussion
Although remarkable symptomatic improvement is seen in many patients with CRT, up to 30% of subjects who participated in CRT trials failed to respond to therapy or may have worsened [3]. Benefits of CRT therapy in the setting of CRBBB have been debated with arguments for both sides. Some studies have suggested little or no benefit from CRT in patients with CRBBB. Bilchick et al. reported that the presence of CRBBB was associated with worse overall survival compared with complete left bundle branch block (40.3% versus 29.7% at 3 years) [4]. This study, however, did not analyze the aspect of mechanical dyssynchrony.
In a work by Fantoni et al., right and left ventricular electroanatomic activation maps were evaluated in 100 consecutive patients who were referred for CRT therapy. Significant delay in the LV endocardial activation sequence was seen in most patients with CRBBB morphology and left axis deviation [5]. Some studies showed improvement in quality of life, New York Heart Association functional class, and other measurements of functional capacity, but only when a coexisting left hemiblock was present in patients with CRBBB [6], [7]. Furthermore, Leong et al. [8] showed that LV dyssynchrony was identified as an independent predictor of all-cause mortality or heart failure hospitalization among CRBBB patients with CRT implantation during long-term follow-up.
The left anterior fascicle normally activates the anterosuperior portion of the left ventricle early during the QRS complex. With left anterior fascicular block, this region is activated later than normal, resulting in unbalanced inferior and posterior forces early during ventricular activation (initiated by the left posterior fascicle) and unopposed anterosuperior forces later during the QRS complex. Therefore, left anterior fascicular block could result in paradoxical dyssynchrony.
Thus, one plausible reason why the present case with CRBBB responds to CRT therapy may be the coexisting left anterior fascicular block and LV dyssynchrony. The present case indicates that coexisting left hemiblock and LV dyssynchrony are important to predict the CRT outcomes because the effect of CRT could be caused by the improvement of LV dyssynchrony. The presence of RBBB morphology on the electrocardiogram does not exclude the presence of LV dyssynchrony, which may be due to the co-existence of hemi-block. Therefore, evaluation of LV dyssynchrony with echocardiography should be performed and coexisting hemiblock could be an easy and useful predictor to estimate CRT responders in patients with RBBB.
We previously reported the advantages of triple-site ventricular pacing compared to biventricular site pacing [2]. The baseline LV end-diastolic volume was an independent predictor for the triple-site ventricular pacing responder. The receiver operating characteristic curve showed that LV end-diastolic volume of >212 ml had a sensitivity of 80% and specificity of 77% to distinguish triple-site ventricular pacing responders [9]. Therefore, we chose triple-site ventricular pacing for the present case. However, whether bi-ventricular pacing would have led to a response in the present case was unclear.
Conflict of interest
Authors declare no conflict of interest.
References
- 1.Seo Y., Ishizu T., Sakamaki F., Yamamoto M., Machino T., Yamasaki H., Kawamura R., Yoshida K., Sekiguchi Y., Kawano S., Tada H., Watanabe S., Aonuma K. Mechanical dyssynchrony assessed by speckle tracking imaging as a reliable predictor of acute and chronic response to cardiac resynchronization therapy. J Am Soc Echocardiogr. 2009;22:839–846. doi: 10.1016/j.echo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 2.Yoshida K., Seo Y., Yamasaki H., Tanoue K., Murakoshi N., Ishizu T., Sekiguchi Y., Kawano S., Otsuka S., Watanabe S., Yamaguchi I., Aonuma K. Effect of triangle ventricular pacing on haemodynamics and dyssynchrony in patients with advanced heart failure: a comparison study with conventional bi-ventricular pacing therapy. Eur Heart J. 2007;28:2610–2619. doi: 10.1093/eurheartj/ehm441. [DOI] [PubMed] [Google Scholar]
- 3.Abraham W.T., Fisher W.G., Smith A.L., Delurgio D.B., Leon A.R., Loh E., Kocovic D.Z., Packer M., Clavell A.L., Hayes D.L., Ellestad M., Trupp R.J., Underwood J., Pickering F., Truex C. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845–1853. doi: 10.1056/NEJMoa013168. [DOI] [PubMed] [Google Scholar]
- 4.Bilchick K.C., Kamath S., DiMarco J.P., Stukenborg G.J. Bundle-branch block morphology and other predictors of outcome after cardiac resynchronization therapy in Medicare patients. Circulation. 2010;122:2022–2030. doi: 10.1161/CIRCULATIONAHA.110.956011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fantoni C., Kawabata M., Massaro R., Regoli F., Raffa S., Arora V., Salerno-Uriarte J.A., Klein H.U., Auricchio A. Right and left ventricular activation sequence in patients with heart failure and right bundle branch block: a detailed analysis using three-dimensional non-fluoroscopic electroanatomic mapping system. J Cardiovasc Electrophysiol. 2005;16:112–119. doi: 10.1046/j.1540-8167.2005.40777.x. [DOI] [PubMed] [Google Scholar]
- 6.Garrigue S., Reuter S., Labeque J.N., Jais P., Hocini M., Shah D.C., Haissaguerre M., Clementy J. Usefulness of biventricular pacing in patients with congestive heart failure and right bundle branch block. Am J Cardiol. 2001;88:1436–1441. doi: 10.1016/s0002-9149(01)02131-2. [DOI] [PubMed] [Google Scholar]
- 7.Chandra R., Zolty R., Palma E. A left hemiblock improves cardiac resynchronization therapy outcomes in patients with a right bundle branch block. Clin Cardiol. 2010;33:89–93. doi: 10.1002/clc.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leong D.P., Höke U., Delgado V., Auger D., Thijssen J., van Erven L., Bax J.J., Schalij M.J., Marsan N.A. Predictors of long-term benefit of cardiac resynchronization therapy in patients with right bundle branch block. Eur Heart J. 2012;33:1934–1941. doi: 10.1093/eurheartj/ehr470. [DOI] [PubMed] [Google Scholar]
- 9.Yamasaki H., Seo Y., Tada H., Sekiguchi Y., Arimoto T., Igarashi M., Kuroki K., Machino T., Yoshida K., Murakoshi N., Ishizu T., Aonuma K. Clinical and procedural characteristics of acute hemodynamic responders undergoing triple-site ventricular pacing for advanced heart failure. Am J Cardiol. 2011;108:1297–1304. doi: 10.1016/j.amjcard.2011.06.048. [DOI] [PubMed] [Google Scholar]