Abstract
A 46-year-old man who had failed primary angioplasty to the dominant right coronary artery due to high thrombus burden 2 years previously, presented with non-ST-elevation myocardial infarction following discontinuing antiplatelet therapy for 2 months. Angiography showed occluded right coronary artery with extensive thrombus burden. There was no significant left coronary artery disease. Due to failure of thromboaspiration and angiojet from the previous attempt 2 years previously, intracoronary thrombolysis with streptokinase was administered via thromboaspiration catheter. Following intracoronary thrombolysis, aspiration catheter was able to retrieve the majority of thrombi and achieved thrombolysis in myocardial infarction 3 flow at the end of the procedure with resolution of transient ST elevation. This case demonstrated that the use of adjunctive intracoronary thrombolysis and manual aspiration in a patient presenting with myocardial infarction with heavy thrombus burden might be useful in selected cases.
<Learning objective: The use of adjunctive intracoronary thrombolysis and manual aspiration in a patient presenting with myocardial infarction with heavy thrombus burden might be useful in selected cases.>
Keywords: Thrombolysis, Thrombectomy, Acute myocardial infarction
Case report
A 46-year-old man presented with an acute coronary syndrome. He had cardiovascular risk factors of smoking and dyslipidemia and had previously undergone unsuccessful primary angioplasty for an inferior ST-segment elevation myocardial infarction (STEMI) 2 years previously. He presented with non-ST elevation myocardial infarction (NSTEMI) with unstable chest cardiac symptoms. This patient had discontinued routine medications including aspirin for 2 months prior to admission. At his initial presentation with inferior STEMI 2 years previously, emergency coronary angiography had revealed ectatic coronary arteries with a large thrombus burden in the right coronary artery (RCA) (Fig. 1a). Despite aggressive thromboaspiration and the use of 5 Fr Angiojet (Possis Medical, Minneapolis, MN, USA), the procedure was unsuccessful (Fig. 1b). Post-infarct, cardiac echocardiography revealed left ventricular inferior wall hypokinesia and an ejection fraction of 48%. He was maintained on medical therapy thereafter.
Fig. 1.
(a) Previous right coronary artery (RCA) intervention following 5 Fr Angiojet device (Possis Medical, Minneapolis, MN, USA). (b) Final results from previous failed intervention to RCA. (c) Current admission showed acute mid RCA occlusion during emergency diagnostic coronary angiography. (d) RCA was engaged with AL2 guiding catheter and thromboaspiration was performed with the Eliminate (Terumo, Aichi, Japan) aspiration catheter. (e) 250,000 units of streptokinase were administered via the Eliminate aspiration catheter into the distal RCA following contrast injection into the Eliminate catheter to confirm distal location of the guidewire and free of perforation. (f) Final result following multiple manual aspirations via the Eliminate catheter after 10 min of the thrombolysis infusion.
His current admission was associated with raised cardiac Troponin I at presentation [0.528 μg/L (0–0.039 μg/L)] and this peaked at 6.792 μg/L 12 h later. Coronary angiography performed via the right radial approach on the next day showed a thrombus-laden mid RCA as seen on previous admission (Fig. 1c). The procedure was converted to right femoral artery approach due to tortuous right subclavian artery. A 6 Fr AL2 guiding catheter was used to engage the RCA ostium and an 0.014 in. Runthrough NS Hypercoat (Terumo, Aichi, Japan) guidewire was used to cross the occluded mid RCA (Fig. 1d). Thrombus aspiration was attempted using a 6 Fr Eliminate (Terumo) catheter but this could not be advanced across the distal RCA (Fig. 1d). Despite aspirating copious amounts of thrombi, thrombolysis in myocardial infarction (TIMI) flow remained suboptimal and a significant amount of thrombi remained. Due to previous failure of Angiojet thrombectomy attempt 2 years previously, we decided to try intracoronary thrombolysis. The Eliminate aspiration catheter was advanced as far as possible into the distal RCA. Contrast injection into the aspiration port of the Eliminate catheter confirmed its position in the true lumen and presence of significant residual thrombi (Fig. 1e). A dose of 250,000 units of streptokinase diluted into 10 mL of normal saline was injected slowly into the distal RCA via the aspiration port of the Eliminate aspiration catheter over a period of 15 min. Transient bradycardia associated with hypotension was noted and this stabilized with 250 mLs intravenous bolus normal saline. ST-elevation in electrocardiogram leads II and III accompanied with chest pain was also present briefly. Subsequent to intracoronary thrombolysis, we repeated thrombus aspiration with the Eliminate catheter, alternating with use of a 4 mm × 20 mm balloon to mechanically disrupt the partially lysed thrombi (Fig. 2a and b). Final angiography showed restored TIMI 3 flow with a patent right posterior descending artery (Fig. 1f). The chest pain and procedural related ST-elevation resolved and the patient subsequently made an uneventful recovery. He was advised life-long anticoagulation therapy and smoking cessation.
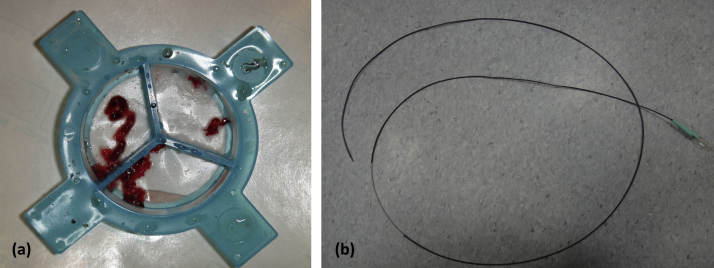
Fig. 2.
(a) Amount of thrombi aspirated at the end of the procedure. (b) The Eliminate aspiration catheter (Terumo, Aichi, Japan).
Discussion
Thrombus burden in primary angioplasty predicts slow and no-reflow phenomenon and manual aspiration of the thrombus via a dedicated aspiration catheter was associated with better myocardial perfusion, less distal embolization, and mortality reduction [1]. Our case involved massive thrombus burden in an ectactic RCA and previously failed procedural attempt with a 5 Fr Angiojet. There was no known history of Kawasaki disease and the diffuse ectactic arteries in both left and right coronary arteries are probably the results of atherosclerosis. In the current presentation, we decided on intracoronary thrombolysis as it has previously been reported that intracoronary injections of tissue plasminogen activator (800,000 units), alteplase 10 mg, tenecteplase 40 mg (8000 units), or streptokinase 250,000 units had achieved variable success [2], [3], [4], [5]. In our case, the thrombi in the right coronary artery were partially lysed over 20 min to allow successful aspiration using the Eliminate catheter. During intra-coronary thrombolysis, transient hypotension and/or temporary rhythm disturbance requiring temporary pacing wire may occur, especially in the dominant RCA. Finally, radial approach might lower the rate of bleeding complications secondary to thrombolysis.
Our case demonstrated a successful thrombectomy with the use of intracoronary thrombolysis and manual aspiration in a patient presenting with unstable inferior STEMI, this may reflect the fact that adjunctive thrombolysis might be useful in selected cases.
Conflict of interest
Authors declare no conflict of interest.
References
- 1.De Luca G., Dudek D., Sardella G., Marino P., Chevalier B., Zijlstra F. Adjunctive manual thrombectomy improves myocardial perfusion and mortality in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: a meta-analysis of randomized trials. Eur Heart J. 2008;29:3002–3010. doi: 10.1093/eurheartj/ehn389. [DOI] [PubMed] [Google Scholar]
- 2.Sezer M., Oflaz H., Goren T., Okcular I., Umman B., Nisanci Y., Bilge A.K., Sanli Y., Meric M., Umman S. Intracoronary streptokinase after primary percutaneous coronary intervention. N Engl J Med. 2007;356:1823–1834. doi: 10.1056/NEJMoa054374. [DOI] [PubMed] [Google Scholar]
- 3.Kim J.S., Kim J.H., Jang H.H., Lee Y.W., Song S.G., Park J.H., Chun K.J. Successful revascularization of coronary artery occluded by massive intracoronary thrombi with alteplase and percutaneous coronary intervention. J Atheroscler Thromb. 2010;17:768–770. doi: 10.5551/jat.4283. [DOI] [PubMed] [Google Scholar]
- 4.Higashi H., Inaba S., Nishimura K., Hamagami T., Fujita Y., Ogimoto A., Okayama H., Higaki J. Usefulness of adjunctive pulse infusion thrombolysis after failed aspiration for massive intracoronary thrombus. Can J Cardiol. 2011;27 doi: 10.1016/j.cjca.2011.07.005. 869–869 e1–2. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher S., Jain A.K., Archbold R.A. Intracoronary thrombolytic therapy: a treatment option for failed mechanical thrombectomy. Catheter Cardiovasc Interv. 2012;80:835–837. doi: 10.1002/ccd.23340. [DOI] [PubMed] [Google Scholar]