Abstract
Objectives
Older patients with advanced cancer often have age-related health issues (e.g., memory impairment) that influence their cancer treatment decisions. Communication about these age-related concerns can potentially lead to further assessment and subsequent clinical interventions to improve treatment decision-making and patients’ quality of life. Yet, little is known about the communication of age-related concerns between oncologists, patients, and caregivers.
Materials and Methods
This study is a secondary analysis of data from the Values and Options in Cancer Care (VOICE) study. Audio-recorded and transcribed outpatient clinical oncology encounters with 37 advanced cancer patients >60 years of age were content-analyzed. Two trained coders used a structured coding scheme based on pre-specified geriatric assessment (GA) domains to examine the transcripts for the frequency and quality of communication about age-related concerns. Atlas.ti version 6 was used for all analyses.
Results
The median age of the patients was 66 years (range = 60–90 years); patients were mostly female (26/37), married (22/37), and White (36/37). Out of 37 audio-recorded visits, 31 had at least one mention of an age-related concern with a total of 70 mentions. Oncologists initiated communication about age-related concerns half of the time (53%). When age-related concerns were mentioned, half of the time (50%) the oncologist did not implement further evidence-based interventions to address the age-related concern (e.g., conduct a cognitive screen for a memory concern).
Conclusion
Interventions are needed to improve the frequency and quality of the communication about age-related concerns to improve the care of older adults with cancer.
Keywords: oncology, qualitative, provider-patient communication, geriatric assessment
INTRODUCTION
The intersection of aging and cancer has reached a critical point, with 72% of all patients with cancer being 60 years of age and older.1 Patients aged >65 years are expected to comprise two-thirds of all patients with cancer by 2020,2 bringing to the forefront the critical need for high quality patient-centered communication between older patients with cancer, their oncologists, and their caregivers. Oncologists routinely see older patients who present for discussions regarding the risks and benefits of cancer treatment within a rapidly changing landscape.
Even though the majority of patients with cancer are over 65 years of age, many oncologists are not trained in the care of older patients with cancer.3 They may fail to identify and address age-related concerns (e.g., cognitive impairment and falls) that can affect these patients’ health and quality of life during treatment.4,5 The identification of age-related concerns may encourage discussions about prognosis, which is essential to help older patients with advanced cancer understand that cure is not possible and that treatment side-effects may negatively impact their quality of life.6 Additionally, older patients want information about their illness, prognosis, and treatment choices.7,8
The comprehensive geriatric assessment (GA) is one approach that could help identify age-related concerns. The GA uses validated tools to comprehensively assess geriatric domains including polypharmacy, comorbidity, nutrition, functional status, physical performance, cognition, mental health, and social support known to influence morbidity and mortality in community-dwelling older adults. Additionally, these domains have been associated with survival, treatment tolerance, treatment responsiveness, and/or mortality in older patients with cancer.9–12 Repetto and colleagues found that the GA adds information to traditional performance measures for older patients with cancer.13
Although expert guidelines and the Institute of Medicine recommend a comprehensive assessment, such as the GA, for older patients with cancer to identify age-related concerns and guide treatment decisions 14–18, little is known about the quality of the communication about age-related concerns between oncologists, older patients with advanced cancer, and caregivers. The purpose of this study is to describe the frequency and quality of the communication about age-related concerns consistent with the comprehensive geriatric domains (GA). We expect that communication about age-related concerns will occur infrequently. The findings from this analysis can provide a framework to assess communication and inform interventions for age-related concerns during clinical encounters with older patients with advanced cancer, their caregivers, and their oncologists.
MATERIALS AND METHODS
Setting and Participants
This study analyzed observational data (surveys and transcriptions of the audio-recorded clinical encounters between oncologist, patients, and their caregivers, if present) from the initial phase of the Values and Options in Cancer Care (VOICE) study (NCI, R01CA140419) from upstate New York. The clinical encounter could be an initial or a follow-up consultation. There was no randomization or intervention during the phase one study; neither the patients nor the clinicians received any type of intervention to improve their communication skills. The study design, recruitment, and analysis of VOICE has been previously reported.19 In brief, the purpose of phase one was to obtain the baseline communication patterns of 25 clinicians. All eligible clinicians had to be practicing medical oncologists who treat solid tumors and did not plan on leaving the clinic within the next six months. Investigators recruited clinicians by presenting at grand rounds, faculty meeting; contacting clinical directors; and contacting personal contacts.
For each recruited clinician, at least three patients and their caregivers were recruited to participate in phase one. Patients had to be aged 21 years or older, diagnosed with stage III or IV solid tumor, treated by an enrolled physician, and able to be fluent in English. Patients were ineligible if they were scheduled for a bone marrow transplant, diagnosed with lymphoma or leukemia, hospitalized or in hospice. Caregivers were eligible if they were a caregiver to an enrolled patient, aged 21 years or older, and fluent in English. Caregivers were ineligible if they acted as a caregiver in a professional capacity, such as a minister. Clinicians, patients, and caregivers provided written consent and the study received approval from the institutional review board at the University of Rochester.
Audio-Recorded Encounter Data Collection Procedures
At the time of the clinical encounter, a research assistant met the patient and caregiver in the waiting room. The research assistant would follow the patient and caregiver into the clinic room to place two audio-recorders to capture the clinical encounter. If another individual other than the patient or caregiver was in attendance, the research assistant obtained verbal consent. Once the clinical encounter ended, the research assistant picked up the audio-recorders.
Qualitative Analysis
The audio-recorded encounters were transcribed verbatim by a professional transcriptionist. We conducted content analysis, framework method, of the transcriptions from the audio-recorded clinical encounters to assess the frequency and quality of communication about age-related concerns for patients aged 60 years and older.20 Table 1 outlines the general GA domains, definitions, and importance of each domain for older patients with cancer that guided the content analysis.14,21 Although GA has been utilized to in the care of community dwelling older adults in general, guidelines have suggested its use for older patients with cancer since the impairments in GA domains are associated with adverse outcomes in this population.14,18 We also developed codes to identify who initiated the communication about the age-related health concern and the response quality of the communication about age-related concerns by the oncologist, which was an iterative process between LML and SGM.
Table 1. Geriatric Assessment Domains, Definitions, and Importance.
| Domain | Definitions | Importance |
|---|---|---|
| Comorbidities | Mention of chronic illnesses not including cancer. | Comorbidities are associated with poorer overall survival and poor treatment tolerance. |
| Polypharmacy | Mention of other OTC or prescription drugs. | Polypharmacy increases the risk of drug-drug interactions. |
| Nutrition | Mention of weight, appetite, eating, oral health. | Poor nutritional status is associated with increased need for functional assistance and poorer survival. Unintentional weight loss 6 months before chemotherapy is associated with lower chemotherapy response rates and lower overall survival. |
| Physical performance | Mention of exercise, mobility, strength, falls. | Falls are predictive of worse outcomes. |
| Functional status | Mention of ADLs or IADLs. | Poor functional status is predictive of chemotherapy toxicity and lower survival. |
| Social support | Mention of instrumental (e.g., financial, transportation) or emotional support. | Poor social support could impact adherence to treatment and decrease quality of life. |
| Cognition | Mention of ability to make decisions, memory issues, or confusion. | Poor cognition can influence adherence to treatment, understanding of the risks and benefits of treatment, and the ability to make decisions. |
| Mental health | Mention of mood, depression, or anxiety. | Psychological distress can influence patients’ physical performance. |
Note. OTC = over the counter; ADLs = activity of daily living; IADLs = independent activity of daily living.
The codes to assess oncologists’ response quality were categorized as being “missed opportunities” or “appropriately addressed.” “Missed opportunities” was used when the oncologist, in response to a GA domain, did not implement a care process (either assessment or intervention) known to improve outcomes of older patients to address the concern.14 “Appropriately addressed” was used when the oncologist implemented a care process to mitigate the concern. For example, if someone had a fall, a referral to physical therapy consult for balance/strength training and assist device evaluation would be implemented. Appropriate interventions were derived from a Delphi study with experts in geriatrics and oncology.14
Using the developed codebook, two coders independently coded all transcripts and met to discuss the coded transcripts. Any coding discrepancies were taken to a third researcher and content expert (SGM). The consensus-coded text were pasted into a matrix for medical content review (SGM), to assess whether an age-related concern was “appropriately addressed.” Analysis was facilitated by the qualitative software Atlas.ti version 6.0.
We then conducted descriptive statistics for the coded data as counts and proportions to determine the number of times who initiated the discussion about the age-related concern, the extent to which the age-related concern was mentioned, and how frequently the clinician addressed the age-related concern.
RESULTS
Characteristics of Participants and Communication about Age-Related Concerns
Thirty-seven patients aged 60–90 years seen by 19 oncologists from 9 oncology practices were included (Table 2). The patients were predominantly female (70%), married (60%), and white (97%). All patients had advanced cancer, (stage III or IV), and were being treated by an oncologist.
Table 2. Patients’ Characteristics.
| Age (years), median (IQR) | 66 (64–73) |
| Gender, n (%) | |
| Male | 11 (29.7) |
| Female | 26 (70.3) |
| Race, n (%) | |
| White | 36 (97.3) |
| Other | 1 (2.7) |
| Marital status, n (%) | |
| Married | 22 (59.5) |
| Divorced | 4 (10.8) |
| Widowed | 8 (21.6) |
| Never married | 3 (8.1) |
| Education, n (%) | |
| ≤ High school | 17 (46.0) |
| Some college or equivalenta | 13 (35.1) |
| ≥ Collegeb | 7 (18.9) |
Note. IQR = inter quartile range.
a Some college or equivalent included participants who completed some college but did not graduate, completed technical school including the Associates degree.
b College or more includes participants who graduated college or completed a masters or doctoral degree.
Extent of Age-Related Concerns Mentioned
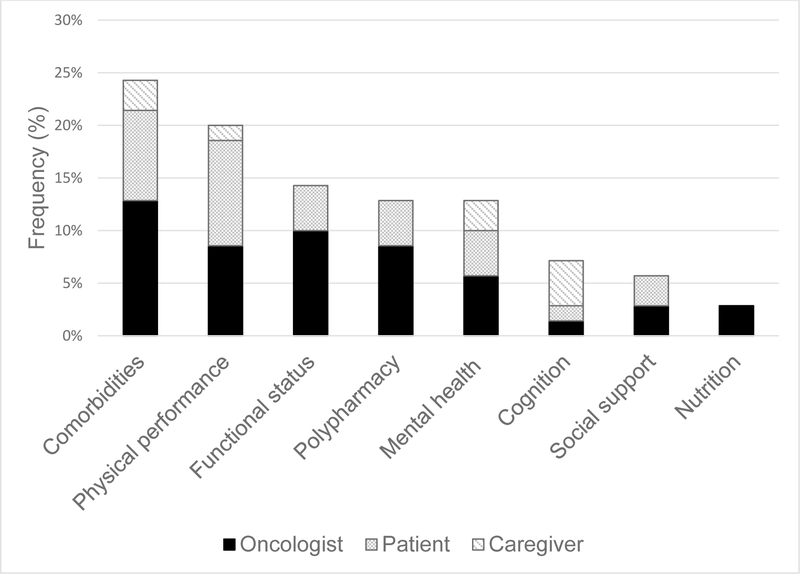
Out of the 37 recorded visits, 31 included at least one mention of an age-related concern. Of these 31 visits, there were 70 mentions of age-related concerns. Figure 1 illustrates the frequency at which the different GA domains were mentioned during the clinical encounters; the person who mentioned the age-related concern first is also indicated. About half (50%) of the communications about age-related concerns were coded as “missed opportunities” where a clinical process or intervention could have been implemented to address the age-related concern (Table 3). Communication about age-related concerns were mainly initiated by oncologists (53%), followed by patients (36%), and then caregivers (11%).
Figure 1. Frequency of GA domains.
The figure depicts the frequency in which the GA domains were brought up during clinical encounters and who initiated the communication about the age-related concern. The data are arranged by the most frequently mentioned GA domain to the least mentioned GA domain (left to right).
Table 3. Frequency and Quality of Responses to Age-Related Concerns Addressed during Outpatient Clinical Oncology Visits.
| Initiated by… | Total n (%) |
|||
| Geriatric Assessment Domain | Oncologist n (%) |
Patient n (%) |
Caregiver n (%) |
|
| Comorbidities | ||||
| Missed opportunity | 1 (1.4) | 0 (0.0) | 1 (1.4) | 2 (2.9) |
| AppropriatelyAddressed | 8 (11.4) | 6 (8.6) | 1 (1.4) | 15 (21.4) |
| Polypharmacy | ||||
| Missed opportunity | 2 (2.9) | 2 (2.9) | 0 (0.0) | 4 (5.7) |
| Appropriately Addressed | 4 (5.7) | 1 (1.4) | 0 (0.0) | 5 (7.1) |
| Nutrition | ||||
| Missed opportunity | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Appropriately Addressed | 2 (2.9) | 0 (0.0) | 0 (0.0) | 2 (2.9) |
| Physical performance | ||||
| Missed opportunity | 4 (5.7) | 4 (5.7) | 1 (1.4) | 9 (12.9) |
| Appropriately Addressed | 2 (2.9) | 3 (4.3) | 0 (0.0) | 5 (7.1) |
| Functional status | ||||
| Missed opportunity | 4 (5.7) | 2 (2.9) | 0 (0.0) | 6 (8.6) |
| Appropriately Addressed | 3 (4.3) | 1 (1.4) | 0 (0.0) | 4 (5.7) |
| Social support | ||||
| Missed opportunity | 1 (1.4) | 2 (2.9) | 0 (0.0) | 2 (2.9) |
| Appropriately Addressed | 1 (1.4) | 0 (0.0) | 0 (0.0) | 1 (1.4) |
| Cognition | ||||
| Missed opportunity | 1 (1.4) | 1 (1.4) | 3 (4.3) | 5 (7.1) |
| Appropriately Addressed | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mental health | ||||
| Missed opportunity | 3 (4.3) | 2 (2.9) | 1 (1.4) | 6 (8.6) |
| Appropriately Addressed | 1 (1.4) | 1 (1.4) | 1 (1.4) | 3 (4.3) |
Note. Percentages are based upon the denominator of 70 instances of communication about age-related concerns.
Comorbidities
Slightly less than a quarter of the communications about age-related concerns addressed comorbidities (24%) with oncologists bringing up the topic half of the time (53%). When comorbidities were mentioned, the oncologist would implement some type of care processes (88%) such as medication reconciliation or communication with another clinician, e.g., referral to a cardiologist if the patient had heart disease. For instance, a patient mentioned that his arthritis was flaring up and affecting his mobility. The oncologist implemented an appropriate intervention by encouraging the patient to discuss the arthritis at his next visit with the primary care provider.
Patient: And I’ve been trying to walk a little bit more. Maybe that’s circulation. I noticed this morning I was very stiff when I got up. Not that I couldn’t walk but it was, I was walking pretty slowly for a while.
Oncologist: Okay. That’s not from the shots or from the -
Patient: I wouldn’t think. I don't know what it’s from.
Oncologist: It sounds like arthritis.
Patient: Well, I do have arthritis.
Oncologist: Have you talked to your primary care doctor about this earning morning-
Patient: Well, I go to see [Name] on Friday, anyway. So I’ll bring it up to him.
[Patient 523]
Nutrition
Nutrition age-related concerns were rarely mentioned (3%) and all were initiated by the oncologist. In the two communications about nutrition, the age-related concern was “appropriately addressed.” For example in the following quote, it is clear that the patient has some dental need and a referral has been made. “[Ms. X] dentist would like her seen today because she has an abscess on her tooth. Did we take care of that?” [Patient 538]
Since many older patients with cancer struggle with eating enough food to maintain their weight, an appropriate care process for oncologists or their team members is to provide practical tips to ensure that patients are not malnourished.22
Oncologist: Are you able to eat a regular meal or are you just eating small amounts?
Patient: Soups.
Caregiver: She’ll eat anything, don’t let her fool you.
Patient: I eat chicken noodle soup and I make homemade onion soup and drink water. And everything else tastes absolutely rotten.
Oncologist: I know but you’ve got to get some protein.
Patient: I know I do.
Caregiver: That’s. . . I was wondering. . . she said everything tastes bad. She’ll eat like 2 spoonfuls of something and then she’s done. Is there any tricks to -- like anything you can put on the food to take that taste away to get her eating?
Oncologist: You know I think in part you are going to have to think of food like a medicine.
Patient: I know. That’s what we were talking about on the way up.
Oncologist: Frequent small amounts.
Caregiver: That’s what I told her today.
Patient: I’m gonna have to force myself.
Caregiver: Whether it tastes [bad].
Oncologist: Best source of protein is an egg.
Patient: Yes, I know. I can eat some eggs.
Oncologist: An egg any which way you can get it in.
Patient: All right.
[Patient 559]
Polypharmacy
Polypharmacy accounted for 13% of age-related concerns mentioned during an encounter with oncologist initiating communication about the polypharmacy concern 67% of the time, and 44% of them were “missed opportunities” where the oncologists would mostly review the current medications and move on to the next topic.
Oncologist: There was no refill. If you need one, just ask and I will be happy to write it for you. Now, the medicine that you are taking right now, are you taking Lasix, Spiriva, Metformin and Ipriniol, Gasmin Vitamin D, Singulair, and Zocor?
[Patient 527]
However, the impact of polypharmacy in older patients (e.g., drug interactions), assessment of adherence, or interventions such as medication discontinuation, pillboxes, or bringing in a pharmacist to help streamline medications were not discussed.
Physical performance
Physical performance accounted for 20% of the communication about age-related concerns with patients mentioning it first 50% of the time. Much of the communication about physical performance involved “missed opportunities” (64%). In some visits, the oncologists would make a slight acknowledgement of the concern mentioned and move on to the next topic, which was more related to symptom management. In the below example the caregiver mentions concerns about mobility and the oncologists ends the conversation asking about the pain medication, but does not assess the impact of the pain medication on the mobility concern.
Caregiver: Well, she’s been spending a lot of time in bed lately. […] And for some reason she’s not able to stand for more than a few minutes at a time.
Oncologist: I see.
Caregiver: And she doesn’t walk long distances. That’s why she’s in a wheelchair now.
Patient: But I want to get out of this wheelchair. […] I’ll probably come dancing in here the next time.
Oncologist: And the hope is that we can help you feel better. And how often are you taking the Norco?
[Patient 546]
Functional status
Communication about functional status occurred infrequently (14%) with the oncologist mentioning the concern about functional status first 70% of the time. When functional status was mentioned, about 60% were “missed opportunities.” For example, the oncologists would try to explore the patient’s level of independence but would not provide space for the patient to say she needs help nor mention that there were resources available to help with activities of daily living.
Patient: Well, I really haven’t been pushing myself. I should be out -
Oncologist: Cook, shopping, cleaning, laundry, are you doing those things?
Patient: Yeah.
Oncologist: Is anyone helping you? Are you doing that on your own or[…]?
Patient: She asks me whatever I need, you know, usually the bulk of it I do.
Oncologist: So you are doing all that stuff. Do you go out anywhere -
Patient: I get tired, I get tired.
Oncologist: Do you go out anywhere other than to come to see us?
Patient: Yes, I went to lunch with my friends yesterday.
Oncologist: Okay, well good.
[Patient 539]
Social Support
In general, social support was mentioned infrequently (6%) with the oncologist and patient initiating the topic (50%), equally, and it was mostly a missed opportunity (75%). In one visit, a patient mentioned that she had avoided filling a prescription because she needed to be able to drive her spouse. The oncologist discussed a plan for taking the medications so that it did not interfere with her fulfilling her caregiving responsibilities but did not discuss other transportation strategies.
Patient: Now, I’ve heard a lot of controversy about Lyrica so I haven’t filled the prescription. And only because for two reasons. It said watch if you drive. And because I’m the sole driver.
Oncologist: You’re the sole driver, right.
Patient: He can drive short distances.
Oncologist: Right, right.
Patient: I can’t be out of commission when it comes to driving.
[Patient 515]
Cognition
Cognitive related issues were mentioned in 7% of the communications about age-related health concerns and all were “missed opportunities” (100%). In one visit, the caregiver reiterated a concern about the patient’s confusion after discussing it with the physician assistant. Ideally, the oncologist would have followed up the concern by administering a validated cognitive screen as recommended by the National Comprehensive Cancer Network (NCCN) guidelines.18
Oncologist: And your hallucinations and dreams? […]
Caregiver: He’s more confused. The confusion hasn’t gone away too much but the hallucinations stopped.
Patient: Well, that’s different.
Oncologist: The hallucinations are better.
Caregiver: Better.
Oncologist: You seem pretty with-it today.
[Patient 552]
Mental Health
Mental health was rarely mentioned (13%) with the oncologist bringing up mental health concerns first more frequently (44%). When mental health was mentioned, the oncologist would do an initial ask when there was a history of depression or anxiety by referencing a previous bout of depression or anxiety. There were instances when oncologists would make sure that the patient’s medication was filled.
Patient: It’s just thinking about the whole situation is upsetting.
Oncologist: You don't have to harp on it, you don't have to harp on it. Your session went better than it was a year ago. […] But I did write that prescription, too, for that Ativan. You know. It’s filled out.
[Patient 539]
In the above example, the oncologist was attempting to soothe the patient by stating “you don’t have to harp on it” and pointing out that the chemotherapy treatment was better than the previous treatment.
DISCUSSION
This study found that communication about age-related concerns during outpatient oncology visits occurred infrequently. Furthermore, when age-related concerns regarding physical performance, functional status, social support, cognition, and mental health were addressed, about half were considered “missed opportunities” where beneficial interventions were not initiated.
There appeared to be a higher level of comfort communicating about age-related concerns that were medical, such as comorbidities, polypharmacy, and nutrition with a specific emphasis on weight loss than non-medical concerns. Asking about comorbidities and polypharmacy is consistent with current oncology practice and reflective of normative values among oncologists. In a literature review by Tariman et al., they reported that pre-existing comorbidities and findings from published studies were influential in oncologists treatment decisions.23
The response quality of the medically driven domains (e.g., comorbidities and polypharmacy) could be improved by implementing domain specific care processes or interventions as outlined in a Delphi study with experts in the field of geriatrics and oncology 14. Communication about comorbidities could be improved by coordinating with other clinicians and ensuring that the cancer treatment is not exacerbating the comorbid condition. The medications could be reviewed to determine if some could be switched, decreased, or dropped if there is an increased risk for negative drug-drug interactions. Other areas to assess for nutrition include oral health (e.g., mucositis or dentures not fitting well).
Issues concerning functional status, physical performance, social support, mental health, and cognitive function were not mentioned as much and care processes were rarely implemented. Several reasons may explain these findings. For example, there may be insufficient time to explore these issues during clinical encounters. Also, oncologists are infrequently trained to assess functional status, physical performance, social support, mental health, and cognitive function. As a result, they may feel less comfortable addressing and managing these concerns. Other age-related concerns may not be routinely explored because there may be an underlying belief that age-related concerns are not directly related to clinical outcomes.
Several studies have shown that age-related concerns affect clinical outcomes.9,24. The assessment of age-related concerns can influence treatment decisions where the treatment intensity is either increased or decreased based on underlying age-related issues.25 Functional status and physical performance concerns could be addressed with referrals to physical therapy and/or recommending strengthening exercises. Age-related concerns about social support are important to address because they can impact patients’ independence, ability to attend treatment visits, and medication management. Mental health or cognitive related issues could be explored and to check that the patient is not on a medication that worsens geriatric symptoms. For example, Ativan may not be the best choice for older patients with a history of falls because it can increase the risk of falls. Clearly, a more patient-centered communication approach could help to optimize treatment outcomes and increase the likelihood that treatment decisions are aligned with the older patients’ and caregivers’ values and goals for treatment.
Some limitations need to be taken into consideration when interpreting these results. Data used in this secondary analysis was collected in community oncology practices in upstate New York. The patients were predominately female and White. Oncologists may encounter different patients and tailor their consultations according to regional practice norms. Although there were limited clinical details about the cancer, all patients had advanced cancer.26 We analyzed a single encounter; therefore, it is possible that age-related concerns were discussed in other encounters. In addition, much of the support for patients in oncology clinics is provided by team members other than the oncologist; future research should explore how other team members (e.g., nurses) foster communication and care-processes to address age-related concerns.
Despite these limitations, this study provides an invaluable look into the clinical encounters in community oncology practices between oncologists, older patients, and caregivers. The data collected here serves as a starting point to further our understanding of 1) oncology clinical encounters with older patients and caregivers; 2) how often communication about age related concerns occur, 3) who initiates the communication about these age-related concerns, and 4) the quality of the communication about age-related concerns. These findings can be used to develop future intervention studies to improve the communication process during oncology visits with older patients. Future work could also explore whether increased communication about age-related concerns improves clinical outcomes and patient reported outcomes.
ACKNOWLEDGMENTS
The authors would like to thank Victoria Yellamaty who helped with coding the transcripts and Sandy Plumb for providing access to the data.
ROLE OF FUNDING AGENCY
This work was supported by the National Cancer Institute [R01CA140419, to R.E.]; the Patient-Centered Outcomes Research Institute [PCORI CD-12–11-4634, to S.G.M]; and The University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. This work was also made possible by the generous donors to the Wilmot Cancer Institute geriatric oncology philanthropy fund. All statements in this report, including its findings and conclusions, are solely those of the authors, do not necessarily represent the official views of the funding agencies, and do not necessarily represent the views of PCORI, its Board of Governors, or Methodology Committee.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
Study concepts: LM Lowenstein, SG Mohile
Study design: LM Lowenstein, SG Mohile
Data acquisition: R Street, R Epstein
Quality control of data and algorithms: LM Lowenstein, SG Mohile
Data analysis and interpretation: All authors
Statistical analysis: LM Lowenstein
Manuscript preparation: LM Lowenstein
Manuscript editing: All authors
Manuscript review: All authors
REFERENCES
- 1.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 2014;64(4):252-71. [DOI] [PubMed] [Google Scholar]
- 2.Parry C, Kent EE, Mariotto AB, Alfano CM, Rowland JH. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev . 2011;20(10):1996-2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hurria A, Balducci L, Naeim A, Gross C, Mohile S, Klepin H, et al. Mentoring junior faculty in geriatric oncology: report from the Cancer and Aging Research Group. J Clin Oncol . 2008;26(19):3125-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurria A, Mohile SG, Dale W. Research priorities in geriatric oncology: addressing the needs of an aging population. J Natl Compr Canc Netw . 2012;10(2):286-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hurria A, Cohen HJ, Extermann M. Geriatric Oncology Research in the Cooperative Groups: A Report of a SIOG Special Meeting. J Geriatr Oncol . 2010;1(1):40-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med . 2012;367(17):1616-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parker SM, Clayton JM, Hancock K, Walder S, Butow PN, Carrick S, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage . 2007;34(1):81-93. [DOI] [PubMed] [Google Scholar]
- 8.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol . 2006;24(33):5265-70. [DOI] [PubMed] [Google Scholar]
- 9.Hurria A, Togawa K, Mohile SG, Owusu C, Klepin HD, Gross CP, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol . 2011;29(25):3457-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maione P, Perrone F, Gallo C, Manzione L, Piantedosi F, Barbera S, et al. Pretreatment quality of life and functional status assessment significantly predict survival of elderly patients with advanced non-small-cell lung cancer receiving chemotherapy: a prognostic analysis of the multicenter Italian lung cancer in the elderly study. J Clin Oncol . 2005;23(28):6865-72. [DOI] [PubMed] [Google Scholar]
- 11.Extermann M, Balducci L, Lyman GH. What threshold for adjuvant therapy in older breast cancer patients? J Clin Oncol . 2000;18(8):1709-17. [DOI] [PubMed] [Google Scholar]
- 12.McCorkle R, Strumpf NE, Nuamah IF, Adler DC, Cooley ME, Jepson C, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. J Am Geriatr Soc . 2000;48(12):1707-13. [DOI] [PubMed] [Google Scholar]
- 13.Repetto L, Fratino L, Audisio RA, Venturino A, Gianni W, Vercelli M, et al. Comprehensive geriatric assessment adds information to Eastern Cooperative Oncology Group performance status in elderly cancer patients: an Italian Group for Geriatric Oncology Study. J Clin Oncol . 2002;20(2):494-502. [DOI] [PubMed] [Google Scholar]
- 14.Mohile SG, Velarde C, Hurria A, Magnuson A, Lowenstein L, Pandya C, et al. Geriatric assessment-guided care processes for older adults: A delphi consensus of geriatric oncology experts. J Natl Compr Canc Netw . 2015;13(9):1120-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balducci L, Cohen HJ, Engstrom PF, Ettinger DS, Halter J, Gordon LI, et al. Senior adult oncology clinical practice guidelines in oncology. J Natl Compr Canc Netw . 2005;3(4):572-90. [DOI] [PubMed] [Google Scholar]
- 16.O'Donovan A, Mohile SG, Leech M. Expert consensus panel guidelines on geriatric assessment in oncology. Eur J Cancer Care (Engl) . 2015;24(4):574-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levit L, Balogh E, Nass S, Ganz PA. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis . Washington (DC): Institute of Medicine;2013. 9780309286602 0309286603. [PubMed] [Google Scholar]
- 18.Hurria A, Wildes T, Blair SL, Browner IS, Cohen HJ, Deshazo M, et al. Senior adult oncology, version 2.2014: Clinical practice guidelines in oncology. J Natl Compr Canc Netw . 2014;12(1):82-126. [DOI] [PubMed] [Google Scholar]
- 19.Hoerger M, Epstein RM, Winters PC, Fiscella K, Duberstein PR, Gramling R, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer . 2013;13:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol . 2013;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Extermann M, Hurria A. Comprehensive Geriatric Assessment for Older Patients With Cancer. J Clin Oncol . 2007;25(14):1824-31. [DOI] [PubMed] [Google Scholar]
- 22.Blanc-Bisson C, Fonck M, Rainfray M, Soubeyran P, Bourdel-Marchasson I. Undernutrition in elderly patients with cancer: target for diagnosis and intervention. Crit Rev Oncol Hematol . 2008;67(3):243-54. [DOI] [PubMed] [Google Scholar]
- 23.Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp KG. Physician, patient, and contextual factors affecting treatment decisions in older adults with cancer and models of decision making: a literature review. Oncol Nurs Forum . 2012;39(1):E70-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Extermann M, Boler I, Reich RR, Lyman GH, Brown RH, DeFelice J, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer . 2012;118(13):3377-86. [DOI] [PubMed] [Google Scholar]
- 25.Hamaker ME, Schiphorst AH, ten Bokkel Huinink D, Schaar C, van Munster BC. The effect of a geriatric evaluation on treatment decisions for older cancer patients--a systematic review. Acta Oncol . 2014;53(3):289-96. [DOI] [PubMed] [Google Scholar]
- 26.Epstein RM, Duberstein PR, Fenton JJ, Fiscella K, Hoerger M, Tancredi DJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA oncology . 2017;3(1):92-100. [DOI] [PMC free article] [PubMed] [Google Scholar]