Abstract
Kounis syndrome, which is known as allergic angina and allergic myocardial infarction today, was described as the coexistence of acute coronary syndrome with allergic reactions in 1991 by Kounis and Zavras. We report a case of a 79-year-old man with hypertension, hepatocellular carcinoma (HCC), and no allergic history. He had received transcatheter arterial chemoembolization (TACE) for treatment of HCC five times without allergic reactions. At the sixth time of TACE, he presented an anaphylactic reaction such as systemic erythema and severe arterial hypotension. Simultaneously, he complained of anterior chest pain and electrocardiogram showed significant ST segment elevation in inferior leads, indicating inferior myocardial infarction. Emergency coronary angiography, however, did not demonstrate any organic stenoses or occluded lesions of the coronary arteries. We made the diagnosis of Kounis syndrome associated with TACE. Although Kounis syndrome is a rare condition, physicians should be aware of possible co-occurrence of anaphylactic reactions and acute coronary syndrome.
<Learning objective: Kounis syndrome refers to acute coronary syndrome associated with allergic or anaphylactic reactions. Physicians have to be aware and keep Kounis syndrome in mind whenever they encounter patients with an anaphylactic reaction. And immediate diagnosis and prompt treatment are needed.>
Keywords: Kounis syndrome, Acute coronary syndrome, Transcatheter arterial chemoembolization, Anaphylactic reaction
Introduction
Simultaneous occurrence of acute coronary syndrome and allergic reactions is known as Kounis Syndrome, which was described by Kounis and Zavras in 1991 [1]. Although the pathophysiology of Kounis syndrome is not completely understood, allergic reaction-induced coronary inflammation and vasospasm are suggested to play a role. Kounis syndrome is caused by various factors, such as foods, drugs, environmental exposures, and medical conditions, all of which induce allergic reactions. Allergens cause mast cell degranulation and several inflammatory mediators such as histamine, tryptase, chymase, neutral proteases, arachidonic acid products, platelet activating factor, and various cytokines and chemokines are released. These mediators cause coronary arterial spasm, plaque rupture, and thrombosis, resulting in acute coronary syndrome. We report a case of Kounis syndrome that was induced by transcatheter arterial chemoembolization (TACE) for the treatment of hepatocellular carcinoma (HCC). Two similar cases that we experienced are also reviewed.
Case report
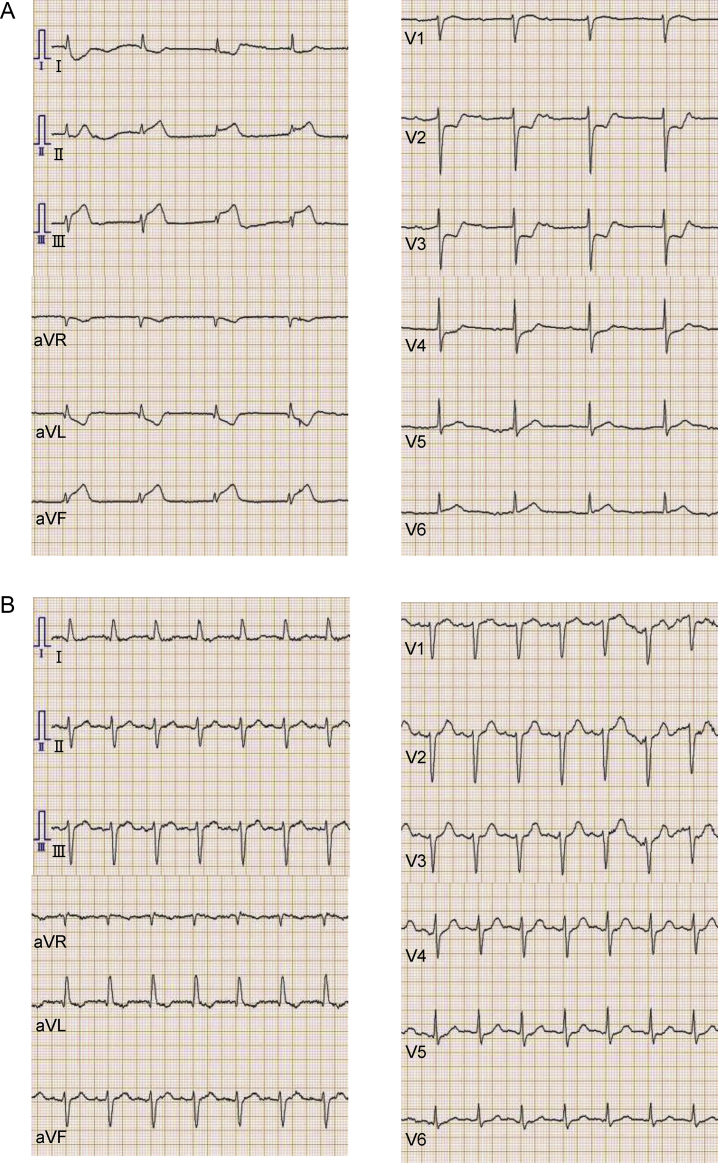
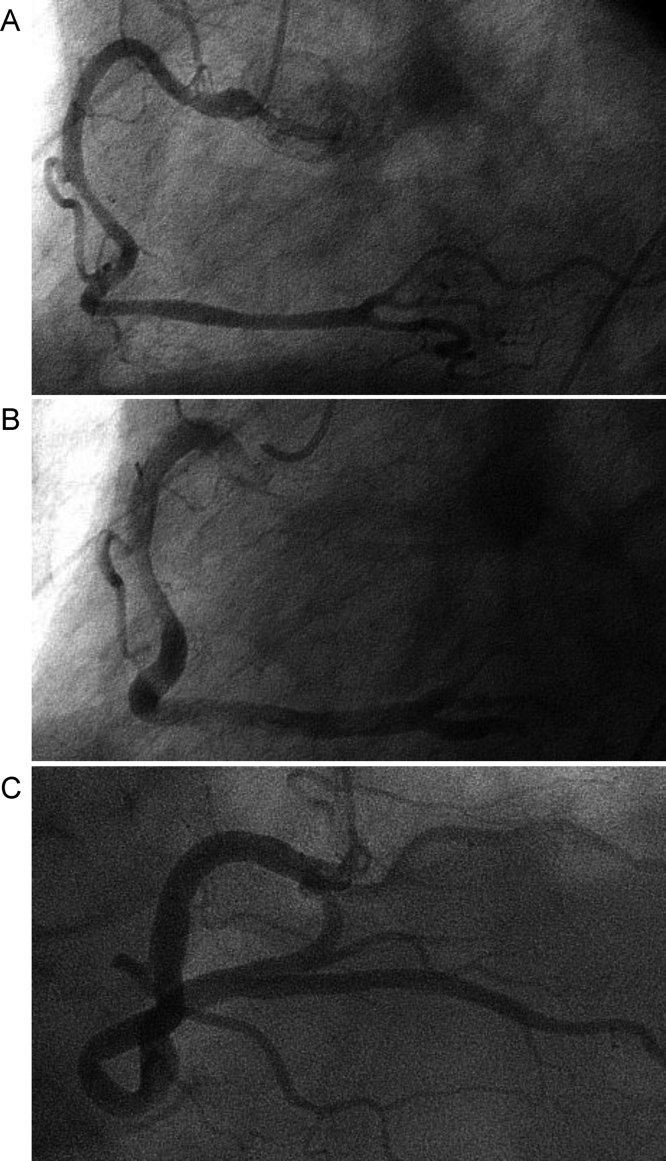
A 79-year-old man with a history of HCC treatment by TACE was admitted to our hospital for another TACE. He had been treated with TACE for five times before without allergic reactions. His medical history was unremarkable except for essential hypertension with medication. There was no history of allergic diseases. And he had never complained of anterior chest pain suggestive of angina pectoris. Approximately 30 min after successful TACE with iopamidol, an iodinated contrast media, and ethylester of iodinated poppy-seed oil fatty acid injection, he complained of anterior chest pain and then lost consciousness. His systolic blood pressure was decreased to 40 mmHg, and his heart rate was 50 beats per minute. His spontaneous breathing stopped. We assisted his breathing with bag valve mask ventilation. Intravenous infusion of normal saline and dopamine (3.0 μg/min/kg) was instituted. Atropine (0.5 mg) was also administered intravenously. Twelve-lead electrocardiogram showed significant ST segment elevation in II, III, and aVF leads and complete atrioventricular block with junctional escape rhythm (Fig. 1A), indicating inferior myocardial infarction. Depression of ST segment in V2 through V4 leads was also observed, which was considered a reciprocal change. Flushing on his extremities and trunk was recognized. Wheeze and stridor were not observed. Emergency coronary angiography was performed after intravenous administration of hydrocortisone (100 mg), d-chlorpheniramine maleate (5 mg), and epinephrine (0.1 mg). When we started coronary angiography, ST segment changes found in the initial electrocardiogram were not observed (Fig. 1B). Angiography of right coronary artery (RCA) revealed no stenosis or occlusion even without intracoronary administration of nitroglycerin (Fig. 2A). After administering nitroglycerin to RCA, marked dilatation of RCA was observed (Fig. 2B and C), suggesting involvement of coronary spasm. Angiography of left coronary artery revealed no organic stenosis or occlusion. The diagnosis of Kounis syndrome associated with TACE was made, because anaphylactic reactions and acute coronary syndrome occurred simultaneously. The next day, physical examination did not reveal any allergic reactions. Laboratory tests of the blood showed mild leukocytosis (11 330/μL, neutrophil 88%, eosinophil 0%) and no change in creatine kinase level (214 U/L, normal range: 62–278 U/L). Electrocardiogram showed the same findings as a previous one before the event. The patient was discharged 2 days after.
Fig. 1.
Electrocardiogram of the patient on heart attack. Electrocardiogram was taken when the patient complained of anterior chest pain. Electrocardiogram showed ST segment elevation in II, III, aVF leads and complete atrioventricular block with junctional escape rhythm (A). Electrocardiogram showed normalization of ST segment when the patient was referred to cardiac catheterization laboratory (B).
Fig. 2.
Coronary angiography of the patient. Angiography of right coronary artery (RCA) at left anterior oblique (LAO) view revealed no stenosis or occlusion without intracoronary administration of nitroglycerin (A). Angiography of RCA after intracoronary administration of nitroglycerin revealed no stenosis and marked dilatation compared with control angiography at LAO (B) and at LAO cranial view (C).
Discussion
Because there is no specific diagnostic test for Kounis syndrome, the diagnosis of Kounis syndrome is based on clinical signs and symptoms that indicate allergic reactions and acute coronary events [2]. Allergic symptoms typical of anaphylactic reactions include hypotension, skin rash, dyspnea, and wheezing. Acute coronary events are recognized by chest pain and electrocardiogram changes. This case showed skin rash, hypotension, and ischemic electrocardiogram changes. Therefore, our case fulfilled the clinical criteria of Kounis syndrome.
Coronary angiography plays a central role in the diagnosis of acute coronary events. Three variants of Kounis syndrome have been reported based on the pathophysiology of coronary events [3]. Type I variant includes patients with normal coronary arteries and no coronary risk factor, and acute allergic insults induce coronary artery spasm. Type II variant includes patients with quiescent coronary artery disease, and acute allergic insults induce plaque erosion or rapture. Type III variant includes patients with drug-eluting coronary artery stent implantation, and acute allergic insults induce stent thrombosis. Although we did not perform spasm provocation test, an elevation of ST segment in inferior leads and almost normal coronary angiogram with marked vasoconstriction at the baseline angiography strongly suggest vasospasm of the RCA. Therefore, we diagnosed that our case was type I variant of Kounis syndrome.
Some examinations are helpful to prove simultaneous occurrence of cardiac damage and allergic reaction and support the diagnosis. Laboratory tests such as measurement of serum cardiac enzymes, tryptase [4], and histamine, eosinophil number and total IgE level may be helpful [2]. It was reported that histological analysis of the aspirated thrombi by hematoxylin–eosin and Giemsa staining showed the presence of eosinophils and mast cells [5].
Treatment of Kounis syndrome is not established by any guidelines. Both acute coronary syndrome management and anaphylaxis management are needed. Epinephrine (recommended dose 0.01 mg/kg IM, every 5–15 min), H1 and H2 blockers, and corticosteroid (hydrocortisone 1–2 mg/kg IV) are recommended for the treatment of anaphylaxis [6]. Giving aspirin and nitroglycerin and percutaneous coronary intervention are indicated for the management of acute coronary syndrome [7]. However, we have to take care when administering these drugs. Epinephrine may induce or exacerbate coronary vasospasm and aggravate cardiac ischemia. Nitroglycerin that dilates coronary arteries can exacerbate hypotension and tachycardia. Fortunately, epinephrine, hydrocortisone, and d-chlorpheniramine maleate were safely given and relieved the patient's symptoms. Electrocardiogram changes were improved within 20 min after medication without adverse effects.
The prognosis of Kounis syndrome is generally reported to be good and no recurrences have been reported. It is advised to avoid repeat exposure to the allergen. It was difficult to determine the allergen in this case, because carbocaine which is a local anesthetic, iopamidol, and lipiodol were administered through a series of procedures in TACE. Therefore, these agents should be avoided in the future treatment. Because of the risk of another anaphylactic shock, we did not attempt another coronary angiography with a spasm provocation test even after the condition of the patient was stabilized.
We experienced three patients admitted to our hospital between January 2008 and July 2014 including the present case (Case 3), who showed anaphylactic reactions and heart attack simultaneously (Table 1). All of them showed no organic coronary artery stenosis on angiography. Although various electrocardiogram changes such as ST segment elevation or depression, negative T wave, QT interval prolongation, and conduction disturbance were reported in Kounis syndrome [2], it is intriguing that all of our three cases showed an elevation of ST segment in II, III, and aVF leads on electrocardiogram. This finding suggests that RCA may be prone to be affected by acute allergic insults more than left coronary artery. A previous review also suggested that RCA seems to be affected by coronary vasospasm in Kounis syndrome [2]. However, the mechanism is not specified.
Table 1.
Our three cases of possible Kounis syndrome and another five cases of Kounis syndrome in past reports.
| Age | Sex | Allergic history | Cardiovascular risk factor | Allergen | Electrocardiogram | Coronary angiography | |
|---|---|---|---|---|---|---|---|
| Case 1 | 60 | Male | No | Hypertension | Wheat | ST segment elevation in II, III and aVF | Normal |
| Case 2 | 69 | Male | Bronchial asthma | Hypertension | Not determined | ST segment elevation in II, III and aVF | Normal |
| Case 3 | 79 | Male | No | Hypertension | Associated with transcatheter arterial chemoembolization | ST segment elevation in II, III and aVF | Normal |
| Case I | 66 | Male | Food allergy | None | Kiwi | ST segment depression in V3–6 and inferior leads | Not performed |
| Case II | 50 | Female | Bronchial asthma | None | Ibuprofen | ST segment elevation in III and aVF | Normal |
| Case III | 57 | Male | No | None | Ibuprofen | ST segment elevation in inferior leads | Revealed spontaneous spasm |
| Case IV | 68 | Male | No | None | Omeprazole | ST segment elevation in anterior leads | Revealed coronary artery disease of left ascending artery |
| Case V | 67 | Female | Atopy | Hypertension | Metamizole | ST segment elevation in V2–6 | Revealed coronary artery disease of left ascending artery |
Cases 1–3 are our cases. Cases I–V are reported in Ref. [8].
Although Kounis syndrome is a rare condition, there are occasional case reports. One of these reports summarized five cases of Kounis syndrome [8]. Two out of five patients showed an ST segment elevation in anterior leads whereas the other two patients showed an ST segment elevation in inferior leads. Various allergens that induced an anaphylactic reaction were also reported. These findings including our experiences suggest that the (possible) causes that elicit Kounis syndrome and clinical manifestations are diverse. These five cases were included in Table 1 for comparison.
In conclusion, we experienced a case of Kounis syndrome that showed anaphylactic shock and anterior chest pain with ischemic electrocardiogram changes mimicking ST-segment elevation myocardial infarction. Although Kounis syndrome is a rare condition, cardiac symptoms and electrocardiogram changes should be carefully observed in patients with anaphylactic reactions.
Conflict of interest
There is no conflict of interest to declare.
Grant support
No grant supported this study.
References
- 1.Kounis N.G., Zavras G.M. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 2.Rico Cepeda P., Palencia Herrejón E., Rodríguez Aguirregabiria M.M. Kounis syndrome. Med Intensiva. 2012;36:358–364. doi: 10.1016/j.medin.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Kounis N.G., Mazarakis A., Tsigkas G., Giannopoulos S., Goudevenos J. Kounis syndrome: a new twist on old disease. Future Cardiol. 2011;7:805–824. doi: 10.2217/fca.11.63. [DOI] [PubMed] [Google Scholar]
- 4.Baldomà N., Cosmen C.R., Galinski S.F., García L.M., Gracia L.R., Villén F.E. Serum tryptase levels in acute coronary syndromes with ST elevation. Int J Cardiol. 2009;131:403–404. doi: 10.1016/j.ijcard.2007.07.101. [DOI] [PubMed] [Google Scholar]
- 5.Kounis N.G. Coronary hypersensitivity disorder: Kounis syndrome. Clin Ther. 2013;35:563–571. doi: 10.1016/j.clinthera.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Simons F.E., Ardusso L.R., Bilò M.B., El-Gamal Y.M., Ledford D.K., Ring J., Sanchez-Borges M., Senna G.E., Sheikh A., Thong B.Y., World Allergy Organization World Allergy Organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011;4:13–37. doi: 10.1097/WOX.0b013e318211496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Gara P.T., Kushner F.G., Ascheim D.D., Casey D.E., Jr., Chung M.K., de Lemos J.A., Ettinger S.M., Fang J.C., Fesmire F.M., Franklin B.A., Granger C.B., Krumholz H.M., Linderbaum J.A., Morrow D.A., Newby L.K. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation. 2013;127:e374–e391. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 8.Gázquez V., Dalmau G., Gaig P., Gómez, Navarro S., Merce J. Kounis syndrome: report of 5 cases. J Investig Allergol Clin Immunol. 2010;20:162–165. [PubMed] [Google Scholar]