In this issue of the Journal, Yoshida et al. presented a report regarding the platelet reactivity assessed with P2Y12 reaction units (PRU) in patients with acute coronary syndrome with essential thrombocythemia (ET) [1]. There are several previous publications regarding cases of acute myocardial infarction concomitant with ET [2], [3], [4]. Some suggest higher risk of thrombus formation in patients with ET [5], [6], [7]. In general, increased platelet cell count correlates with higher thrombogenicity mostly due to increased probability for adhesion and cohesion of platelets [8]. The same is true that the risk of bleeding increases in patients with reduced platelet count unless the sizes of individual platelet cells become bigger than normal [9]. It is important to note that even platelet activation under blood flow conditions is regulated by platelet cell counts [10]. The mechano-biological relationship between platelet membrane glycoprotein (GP) Ibα with von Willebrand factor (VWF) under high shear blood conditions and platelet activation is still to be elucidated. We have to realize the complexity of platelet function and its modification by antiplatelet therapy in ET patients even considering just one parameter of increased platelet count.
Prediction of antiplatelet effects with P2Y12 inhibitor within ET patients with the use of platelet function testing is even more difficult because of increased platelet count and functional abnormality of platelets in ET patients. There are a few differences in platelet function in ET patients and those without ET. The fact that the known stimulus for increased platelet cell count of thrombopoietin is also known as one of the potent platelet stimulating agents [11]. Most probably, platelet cells in ET patients should be sensitive to other stimuli such as VWF, ADP, and so on.
In the report published by Yoshida et al., they suggested that evaluating platelet reaction units (PRU) with the point of care device (Verify Now, Accumetrics, San Diego, CA, USA) is helpful for predicting the effects of dual antiplatelet therapy (DAPT) in patients after percutaneous coronary intervention (PCI) with ET. However, it is impossible to generalize the results with one case for the general patient population with ET. The “Verify Now” they used to measure PRU is one of the new measures for assessing the effect of antiplatelet therapy [12]. In general, “Verify Now” measures ADP-induced platelet aggregation just like the old measure of ADP-induced platelet aggregation measured by light transmittance [13]. One critical difference from traditional ADP-induced platelet aggregation is that another important platelet ADP receptor of P2Y1-induced activation cascade was blocked by addition of prostaglandin E (PGE)-1 in “Verify Now” [14]. There are numerous contradicting publications whether PRU measures are meaningful for “personalized” dose adjustment of P2Y12 inhibitors such as clopidogrel or not [12], [15], [16]. One of the largest hypothesis-testing clinical trials demonstrated that neither efficacy nor safety was improved by dose adjustment of clopidogrel using “Verify Now” [17], [18]. Thus, the clinical relevance of PRU measured by “Verify Now” in patients treated by P2Y12 ADP antagonists is still to be elucidated even in patients without ET [19].
A platelet is a small cell, but the exact functional regulation mechanism in this cell is yet to be clarified [8]. Unlike the concepts used for developing “Verify Now,” some reports suggest a relevant role of both P2Y1 and P2Y12 for increasing intra-cellular calcium ion concentrations [20]. PRU may reflect P2Y12 inhibition more closely than ADP-induced platelet aggregation, but this hypothesis is still to be elucidated. Although “Verify Now” is widely used for assessing the efficacy of P2Y12 inhibitors, we have to be aware that all the results might just be an interesting artifact and not relevant to clinical outcomes.
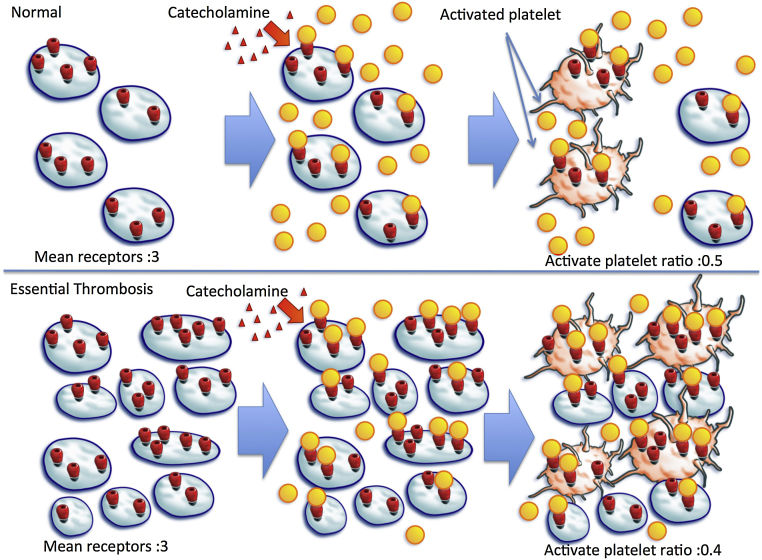
A previous publication suggests that platelet cells in patients with ET are resistant to stimulation by catecholamines [21]. Platelet cells express α2-receptor for stimulation by catecholamines. Platelet cells become more sensitive to other stimulation when α2-receptors are stimulated by small amounts of catecholamine [22]. Increased number of platelets with heterogeneous characteristics of sensitivity or resistance to ADP stimulation in ET might result either in apparently “resistant” or “sensitive” to any stimulations in mass of platelet cells as shown in Fig. 1. “Verify Now” assesses platelet function as a “mass of platelet cells” and not as individual ones. Reaction as a “mass of cells” may not be the same as “individual platelets”. One typical example is that the intracellular calcium ion concentrations of individual platelet cells go up and down over time [20], while it looks like an increased monophasic response in a “mass of platelet cells” [23]. Platelet cells in vivo are hugely heterogeneous in size, number of expressing proteins, and reaction to various stimuli in individual cells [10]. A greater inter-platelet heterogeneity in patients with ET might be the reason to show apparently different behavior against ADP receptor stimulation as shown in Fig. 1.
Fig. 1.
Why the speculation based upon the results of “VerifyNow” for the mechanism of platelet activation and/or its inhibition by drug intervention is problematic? Increased number of platelet cells in ET may influence the apparent response of platelets in “mass”. We have to be careful for assessing the effects of antiplatelet agents with the use of point of care devices just measuring the reaction of “mass of cells”.
Finally, the use of “point of care devices” to individualize antithrombotic therapies remains challenging. Even though some trials suggest correlation of PRU and thrombotic event rates, no study has demonstrated the benefit of personalized adjustment of the dose of P2Y12 ADP receptor inhibitors by PRU. All results using “Verify Now” might just be an interesting artifact. If we really want to establish the logic for “personalized medicine” for the use of P2Y12 ADP receptor inhibitors, quantitative understanding of the relationship between the dose taken as drugs, the actual P2Y12 ADP receptor blockage (e.g. number of receptors blocked/number of available receptors) [8], and the quantification of the heterogeneity between actual P2Y12 ADP receptor blockage and cell response (such as number of GPIIb/IIIa proteins changed to activated form, number of dense granules released, number of fibrinogen molecules released from activated platelet, etc.) is necessary. An evidence-based approach emphasizing the importance of randomized control trials (RCTs) might still have some role for personalized medicine by selecting a small high-risk population who needs new therapies [24]. For the rare case such as ET, a “bottom up” approach with constructive logic from exact understanding of the detailed mechanism of platelet cells is essentially important.
References
- 1.Yoshida N., Hiranuma N., Ninomaru T., Nagamatsu Y., Tamada N., Miyoshi T., Sasaki Y., Kanda G., Kobayashi N., Fujii T. Evaluation of platelet reactivity using P2Y12 reaction units in acute coronary syndrome with essential thrombocythemia: a case report. J Cardiol Cases. 2015;11:178–180. doi: 10.1016/j.jccase.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esteves Filho A., Costa Fde A., Lima A.A., Kajita L.J., Martinez Filho E.E. Essential thrombocythemia and acute myocardial infarction treated with rescue coronary angioplasty. Arq Bras Cardiol. 1999;73:97–102. doi: 10.1590/s0066-782x1999000700009. [DOI] [PubMed] [Google Scholar]
- 3.Daya S.K., Gowda R.M., Landis W.A., Khan I.A. Essential thrombocythemia-related acute ST-segment elevation myocardial infarction. A case report and literature review. Angiology. 2004;55:319–323. doi: 10.1177/000331970405500312. [DOI] [PubMed] [Google Scholar]
- 4.Cheng C.W., Hung M.J. Coronary spasm-related acute myocardial infarction in a patient with essential thrombocythemia. World J Cardiol. 2011;3:278–280. doi: 10.4330/wjc.v3.i8.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao W., Shen W., Luo X., Shi H., Jiang X., Pan J. ST-segment elevation myocardial infarction in patient with essential thrombocythemia without associated risk. Int J Cardiol. 2015;180:223–225. doi: 10.1016/j.ijcard.2014.11.147. [DOI] [PubMed] [Google Scholar]
- 6.Isilak Z., Tezcan M., Atalay M., Kardesoglu E. Acute myocardial infarction and sub-acute stent thrombosis associated with occult essential thrombocythemia. Chin Med J (Engl) 2014;127:3512–3513. [PubMed] [Google Scholar]
- 7.Bhat T., Ahmed M., Baydoun H., Ghandour Z., Bhat A., McCord D. Acute ST-segment elevation myocardial infarction in a young patient with essential thrombocythemia: a case with long-term follow-up report. J Blood Med. 2014;5:123–127. doi: 10.2147/JBM.S53539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goto S., Hasebe T., Takagi S. Platelet: small in size but play essential role in regulation of vascular homeostaisis. -translation from basic science to clinical medicine. Circ J. 2015 doi: 10.1253/circj.CJ-14-1434. [in press] [DOI] [PubMed] [Google Scholar]
- 9.Goto S., Kasahara H., Sakai H., Goto M., Ono M., Ikeda Y., Jorquera J.I., Bravo M.I., Handa S. Functional compensation of the low platelet count by increased individual platelet size in a patient with May-Hegglin anomaly presenting with acute myocardial infarction. Int J Cardiol. 1998;64:171–177. doi: 10.1016/s0167-5273(98)00043-6. [DOI] [PubMed] [Google Scholar]
- 10.Goto S., Salomon D.R., Ikeda Y., Ruggeri Z.M. Characterization of the unique mechanism mediating the shear-dependent binding of soluble von Willebrand factor to platelets. J Biol Chem. 1995;270:23352–23361. doi: 10.1074/jbc.270.40.23352. [DOI] [PubMed] [Google Scholar]
- 11.Miyakawa Y., Oda A., Druker B.J., Miyazaki H., Handa M., Ohashi H., Ikeda Y. Thrombopoietin induces tyrosine phosphorylation of stat3 and stat5 in human blood platelets. Blood. 1996;87:439–446. [PubMed] [Google Scholar]
- 12.Levine G.N., Jeong Y.H., Goto S., Anderson J.L., Huo Y., Mega J.L., Taubert K., Smith S.C., Jr. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol. 2014;11:597–606. doi: 10.1038/nrcardio.2014.104. [DOI] [PubMed] [Google Scholar]
- 13.Salzman E.W., Chambers D.A. Inhibition of ADP-induced platelet aggregation by substituted amino-acids. Nature. 1964;204:698–700. doi: 10.1038/204698b0. [DOI] [PubMed] [Google Scholar]
- 14.Malinin A., Pokov A., Spergling M., Defranco A., Schwartz K., Schwartz D., Mahmud E., Atar D., Serebruany V. Monitoring platelet inhibition after clopidogrel with the VerifyNow-P2Y12(R) rapid analyzer: the VERIfy Thrombosis risk ASsessment (VERITAS) study. Thromb Res. 2007;119:277–284. doi: 10.1016/j.thromres.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 15.Levine G.N., Jeong Y.H., Goto S., Anderson J.L., Huo Y., Mega J.L., Taubert K., Smith S.C., Jr. World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Glob Heart. 2014;9:457–467. doi: 10.1016/j.gheart.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Price M.J., Angiolillo D.J., Teirstein P.S., Lillie E., Manoukian S.V., Berger P.B., Tanguay J.F., Cannon C.P., Topol E.J. Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention: a time-dependent analysis of the Gauging Responsiveness with a VerifyNow P2Y12 assay: Impact on Thrombosis and Safety (GRAVITAS) trial. Circulation. 2011;124:1132–1137. doi: 10.1161/CIRCULATIONAHA.111.029165. [DOI] [PubMed] [Google Scholar]
- 17.Collet J.P., Cuisset T., Range G., Cayla G., Elhadad S., Pouillot C., Henry P., Motreff P., Carrie D., Boueri Z., Belle L., Van Belle E., Rousseau H., Aubry P., Monsegu J. Bedside monitoring to adjust antiplatelet therapy for coronary stenting. N Engl J Med. 2012;367:2100–2109. doi: 10.1056/NEJMoa1209979. [DOI] [PubMed] [Google Scholar]
- 18.Price M.J., Berger P.B., Teirstein P.S., Tanguay J.F., Angiolillo D.J., Spriggs D., Puri S., Robbins M., Garratt K.N., Bertrand O.F., Stillabower M.E., Aragon J.R., Kandzari D.E., Stinis C.T., Lee M.S. Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: The GRAVITAS randomized trial. JAMA. 2011;305:1097–1105. doi: 10.1001/jama.2011.290. [DOI] [PubMed] [Google Scholar]
- 19.Goto S., Tomiya A. High on-treatment platelet reactivity (HPR): what does it mean, and does it matter? Thromb Haemost. 2013;109:177–178. doi: 10.1160/TH12-12-0910. [DOI] [PubMed] [Google Scholar]
- 20.Goto S., Tamura N., Ishida H., Ruggeri Z.M. Dependence of platelet thrombus stability on sustained glycoprotein IIb/IIIa activation through adenosine 5′-diphosphate receptor stimulation and cyclic calcium signaling. J Am Coll Cardiol. 2006;47:155–162. doi: 10.1016/j.jacc.2005.08.055. [DOI] [PubMed] [Google Scholar]
- 21.Kaywin P., McDonough M., Insel P.A., Shattil S.J. Platelet function in essential thrombocythemia. Decreased epinephrine responsiveness associated with a deficiency of platelet alpha-adrenergic receptors. New Engl J Med. 1978;299:505–509. doi: 10.1056/NEJM197809072991002. [DOI] [PubMed] [Google Scholar]
- 22.Goto S., Ikeda Y., Murata M., Handa M., Takahashi E., Yoshioka A., Fujimura Y., Fukuyama M., Handa S., Ogawa S. Epinephrine augments von Willebrand factor-dependent shear-induced platelet aggregation. Circulation. 1992;86:1859–1863. doi: 10.1161/01.cir.86.6.1859. [DOI] [PubMed] [Google Scholar]
- 23.Ikeda Y., Handa M., Kawano K., Kamata T., Murata M., Araki Y., Anbo H., Kawai Y., Watanabe K., Itagaki I., Sakai K., Ruggeri Z.M. The role of von willebrand factor and fibrinogen in platelet aggregation under varying shear stress. J Clin Investig. 1991;87:1234–1240. doi: 10.1172/JCI115124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goto S., Goto S. Selection of a suitable patient population for new antiplatelet therapy from the large clinical trial database of the thrombin receptor antagonist in secondary prevention of atherothrombotic ischemic events-thrombolysis in myocardial infarction 50 (TRA-2P-TIMI50) trial. Circulation. 2015;131:1041–1043. doi: 10.1161/CIRCULATIONAHA.115.015471. [DOI] [PubMed] [Google Scholar]