Abstract
Background
Pertussis is highly contagious respiratory disease. Healthcare workers (HCWs) can be an important mediator of the disease. A seroprevalence of pertussis was investigated in HCWs to determine the immune status against pertussis and to detect the unidentified pertussis.
Methods
This study was conducted for HCWs at a hospital located in Korea in 2011. After obtaining written informed consent for HCWs voluntarily participating in the study, 10 mL of blood was collected from each subject. Demographic and medical data were collected using questionnaire. Data on the underlying disease and vaccination history were reviewed again through medical records. The presence of anti-pertussis toxin (anti-PT) immunoglobulin G (IgG), and immunoglobulin A (IgA) was detected by quantitative analysis using a commercially available ELISA kit (EUROIMMUN, Lübeck, Germany).
Results
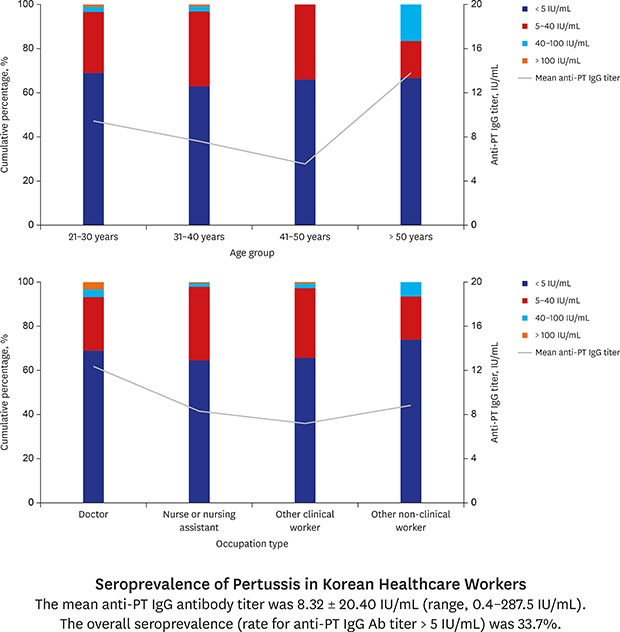
A total of 412 HCW participated in the study. Among them, 14 were excluded due to the inadequate sample amount or medical history not secured. Of the 398 HCWs analyzed, 16.6% (66/398) were men and the mean age was 33.82 ± 9.10 years (range, 21–67). The mean anti-PT IgG titer was 8.32 ± 20.40 IU/mL (range, 0.4–287.5 IU/mL). The overall seroprevalence (rate of anti-PT IgG antibody [Ab] titer > 5 IU/mL) was 33.7%. Three (0.8%) HCWs had the Ab level > 100 IU/mL indicated acute infection. There was no statistically significant difference in the seroprevalence and mean titer of anti-PT IgG Ab according to age group, type of occupation, patient-facing position, or working in the pediatric department.
Conclusion
The seroprevalence of pertussis of the HCWs of a university hospital in Korea was low, and there were some unrecognized acute infections. Therefore, booster immunization of pertussis to HCWs should be actively considered.
Keywords: Pertussis Seroprevalence, Health Personnel, Korea
Graphical Abstract
INTRODUCTION
Bordetella pertussis, a causative organism of pertussis, is a gram-negative coccobacillus that causes disease only in humans.1 It is highly contagious and spreads through the droplets of the carrier. Pertussis occurs anywhere, regardless of climate, region, or race, and can occur at any age. Since the introduction of the vaccine, it has sharply decreased. However, the incidence has recently increased in the United States and Europe. In Korea, local outbreak of pertussis has been reported continuously.
Healthcare workers (HCWs) are high-risk groups that are expected to have contact with pertussis patients. There are several reports of the outbreak of pertussis in medical institutions.2,3,4,5,6,7 HCWs infected with pertussis can spread it to other susceptible patients or colleagues, and can be a major problem, especially for young children and patients with immune deficiency.8,9
The Korean Society of Infectious Diseases has recommended the booster vaccination against pertussis to all HCWs.10 However, in order to accurately understand the need for the vaccinations, it is important to have enough data on the seroprevalence of HCWs. The seroprevalence data is also useful for determining the unidentified pertussis. The purpose of this study was to investigate the seroprevalence of pertussis in HCWs in a hospital of Korea.
METHODS
Study subjects
This study was conducted for HCWs at a hospital located in Korea. The hospital was the university hospital and had 589 beds. A total of 1,302 HCWs were working in the hospital in 2011 including 243 doctors and 508 nurses or nursing assistants. Blood sampling was carried out in June 2011. The study subjects included not only physicians and nurses, but other workers such as other clinical workers such as nursing assistant, technician, therapist, pharmacist, laboratory personnel, and non-clinical workers. After obtaining the written informed consent, 10 mL of blood was collected from each subject. Following data were collected using structured questionnaire: age, sex, type of occupation, underlying disease, history of cough lasting more than 7 days within 1 year, pertussis vaccination history within 10 years, and other vaccination history within 1 month. Data on the underlying disease and vaccination history were reviewed again through medical records.
Laboratory methods
The presence of anti-pertussis toxin (anti-PT), immunoglobulin G (IgG), and immunoglobulin A (IgA) was detected by quantitative analysis using a commercially available ELISA kit (EUROIMMUN, Lübeck, Germany). The results were interpreted according to the manufacturer's instructions. Increased anti-PT IgG titer (≥ 100 IU/mL) indicated acute pertussis infection or recent vaccination. If anti-PT IgG was 40 to < 100 IU/mL, it was interpreted as probable past exposure to pertussis. For those with anti-PT IgG of 40–100 IU/mL, anti-PT ELISA IgA was performed additionally. If anti-PT ELISA IgA was ≥ 12 IU/mL, it was interpreted as acute infection. If anti-PT IgG titer was 5 to < 40 IU/mL, it was interpreted as no evidence of recent acute infection. Anti-PT IgG titer less than 5 IU/mL indicated seronegative.
Data analysis and statistical analysis
The prevalence of anti-PT IgG antibody (Ab) was stratified by age group, gender, occupation type and department. Subjects were divided into four age groups: 21–30 years, 31–40 years, 41–50 years, and > 50 years. The following occupations were classified as patient-facing position: doctor, nurse, nursing assistant, therapist, radiological technologist, and counselor. The departments in which HCW belonged were categorized into pediatric and non-pediatric departments. The mean anti-PT IgG Ab titers were compared using the t-test or the one-way analysis of variance. Seroprevalence was compared using a χ2 test. Statistical analysis was performed with SPSS Statistics 20.0 software (SPSS Inc., Chicago, IL, USA), and statistical significance was defined as a two-tailed P value < 0.05.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Korea University Ansan Hospital (IRB No. AS11038). Informed consent was obtained from all subjects when they were enrolled.
RESULTS
A total of 412 HCW participated in the study. Among them, 14 were excluded due to the inadequate sample amount or medical history not secured. Of the 398 HCWs analyzed, 29 were physicians, 183 were nurse or nursing assistants, 140 were other clinical workers, and 46 were non-clinical workers. Among them, 16.6% (66/398) were men and the mean age was 33.82 ± 9.10 years (range, 21–67) (Table 1). Twenty-three HCWs (5.8%) had one or more underlying diseases. The most common chronic diseases were hypertension (2.5%) and diabetes (2.5%). Sixteen HCWs (4.0%) reported the history of cough lasting more than 7 days within one year, but none of them was diagnosed as pertussis. None had received pertussis vaccination since childhood.
Table 1. Anti-PT IgG Ab level according to the characteristics in HCWs.
| Characteristics | Total, No. | Seroprevalence | Anti-PT IgG titer, IU/mL | |
|---|---|---|---|---|
| All | 398 | 134 (33.7) | 8.32 ± 20.40 | |
| Age, yr | ||||
| 21–30 | 180 | 56 (31.1) | 9.41 ± 26.62 | |
| 31–40 | 124 | 46 (37.1) | 7.65 ± 14.06 | |
| 41–50 | 76 | 26 (34.2) | 5.53 ± 5.81 | |
| > 50 | 18 | 6 (33.3) | 13.76 ± 24.38 | |
| Gender | ||||
| Men | 66 | 27 (32.2) | 10.67 ± 16.57 | |
| Women | 332 | 107 (32.2) | 7.85 ± 21.06 | |
| Occupation type | ||||
| Doctor | 29 | 9 (31.0) | 12.34 ± 33.34 | |
| Nurse or nursing assistant | 183 | 65 (35.5) | 8.36 ± 22.93 | |
| Other clinical workers | 140 | 48 (34.3) | 7.27 ± 13.46 | |
| Other non-clinical workers | 46 | 12 (26.1) | 8.81 ± 16.72 | |
| Patient-facing position | ||||
| Yes | 269 | 94 (34.9) | 8.58 ± 22.31 | |
| No | 129 | 40 (31.0) | 7.79 ± 15.73 | |
| Department | ||||
| Pediatric department | 40 | 16 (40.0) | 6.57 ± 7.28 | |
| Non-pediatric department | 358 | 118 (33.0) | 8.51 ± 21.37 | |
Values are presented as number (%) or mean ± standard deviation.
Anti-PT = anti-pertussis toxin, IgG = immunoglobulin G, Ab = antibody, HCWs = healthcare workers.
The mean anti-PT IgG titer was 8.32 ± 20.40 IU/mL (range, 0.4–287.5 IU/mL). By age group, mean Ab titer was highest in those over 50 years of age (Table 1). By occupation type, doctor had highest mean Ab titer. HCWs with men gender, patient-facing position, or working in the non-pediatric department had higher Ab titer. However, the differences were not statistically significant.
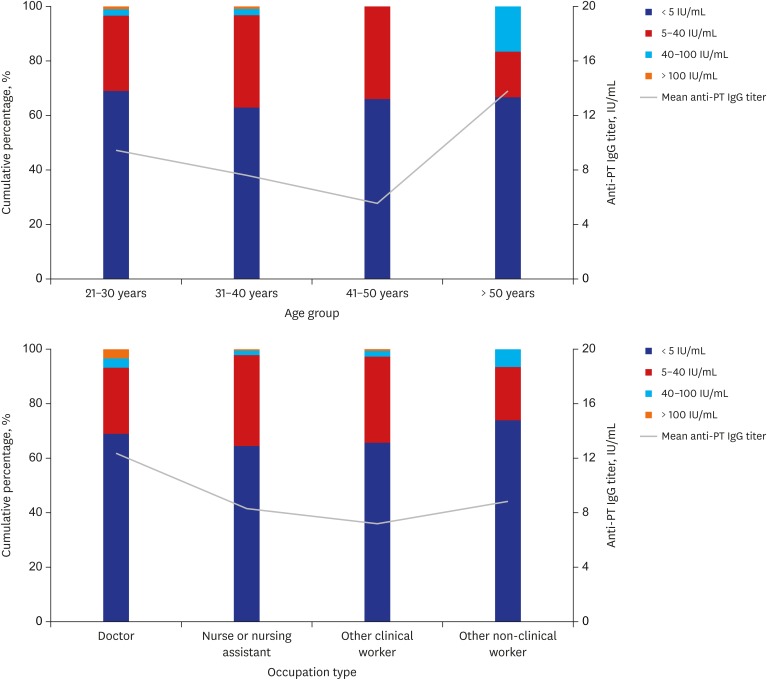
Of the 398 HCWs analyzed, 264 (66.3%) had anti-PT IgG Ab level < 5 IU/mL and 121 (30.4%) had Ab level of 5–40 IU/mL. Three (0.8%) HCWs had the Ab level > 100 IU/mL indicated acute infection. Ten (2.5%) HCWs had anti-PT IgG Ab level of 40–100 IU/mL, but none of them had anti-PT IgA level ≥ 12 IU/mL (range, 0.5–8.2 IU/mL). By age group, anti-PT IgG Ab level of 40–100 IU/mL was more frequently observed in older HCWs > 50 years (P = 0.017) (Fig. 1). By occupation type, there was no statistically significant difference in the distribution of anti-PT IgG Ab level.
Fig. 1. Mean anti-PT IgG Ab titer (line) and seroprevalence (bar) according to the age group and occupation type in HCWs.
Anti-PT = anti-pertussis toxin, IgG = immunoglobulin G, Ab = antibody, HCWs = healthcare workers.
The overall seroprevalence was 33.7%. There was no significant difference in the prevalence of anti-PT IgG Ab (≥ 5 IU/mL) according to age group, type of occupation, patient-facing position, or working in the pediatric department (Table 1).
DISCUSSION
Previous three studies of pertussis Ab prevalence have been conducted in the general population in Korea.11,12 In the last study conducted in 2012, mean anti-PT IgG tier was 35.53 ± 62.91 IU/mL and seroprevalence was 41.40%.11 Although direct comparison is inadequate due to the difference of the ELISA kit used and the study population, seroprevalence of two studies seems to be similar.
One seroprevalence study was performed for HCWs of a university hospital in Korea in 2009, and the result was that 20% of HCWs was susceptible to pertussis.13 However, the result of the study was controversial in that they are quite different from the results of the seroprevalence that was conducted on general population. The present study has advantages above the previous study. Larger number of HCWs was studied examined. The anti-PT IgA Ab test was performed additionally for those with the borderline range of anti-PT IgG Ab titer. And the result is more reliable in that it is similar to the result from the general population study.
A number of seroprevalence studies have been performed in HCW in other countries.14,15 In a study performed in the United States, the geometric mean titer of the anti-PT Ab was 3.6 in enzyme-linked immunosorbent assay units, which was very low level.16 In a study conducted in Spain, the overall seroprevalence of HCW was 51.7%.17 The results of this study also showed that the seroprevalence of pertussis Ab in Korean HCW was also low. This indicates that the need for booster immunization of the pertussis vaccine in adults, especially HCW, is very high.
None of the HCWs participated in this study had received pertussis vaccination since childhood. Considering the Ab acquired by the childhood vaccinations can last only for 4–12 years,18 the HCWs with the anti-PT IgG level higher than 40 IU/mL would have the Ab due to the natural infection. Among the HCWs with high anti-PT IgG Ab level, none had chronic cough lasted longer than 7 days within the past year. In the cases of adult pertussis, it is well known that the severity is mild, and that it is difficult to distinguish it from other respiratory diseases. There was no pertussis patient diagnosed at the hospital within one year of the study. Therefore, it was impossible to identify the route through which the HCWs were infected.
The number of reported pertussis cases nationwide in 2010–2011 was less than 100 cases per year.19 However, there have been reports that the incidence of pertussis in Korea has been underestimated.20 The HCWs consistent with acute pertussis infection could not be confirmed to have pertussis without participating this study. This is another evidence that the incidence of pertussis based on the reports in Korea is considerably underestimated.
There are few studies on the vaccination rate of pertussis vaccine in Korean adults. In 2003, the Korea Center for Disease Control and Prevention reported that the rate of tetanus and diphtheria/tetanus, diphtheria, and acellular pertussis (Td/Tdap) vaccination among adults aged 19 years and over was only 7.3%.21 The pertussis vaccination for adult is very important considering that there have been large outbreaks in the United States and Europe,22 pertussis epidemic have occurred frequently in Korea,23,24 and adult role as important mediators.25 HCWs have a high likelihood of contact with pertussis patients and there are many immunocompromised patients and infants who are high-risk group of pertussis. Therefore, the pertussis vaccination of HCW should be more encouraged. The Korean Society of Infectious Diseases also recommend that all HCWs be vaccinated with Tdap. The Ab test is not required when considering the adult type pertussis vaccine for HCWs. The test is not available in most clinical settings, and past vaccination history taking is sufficient to determine the need for vaccination. However, the seroprevalence study should be regularly performed to establish appropriate vaccination policies and recommendations. In this study, the adult type pertussis vaccine (Adacel®; Sanofi-Pasteur, Toronto, Canada) was inoculated to the HCWs who wanted to be vaccinated after the blood collection.
In conclusion, the seroprevalence of pertussis of the HCWs of a university hospital in Korea was low, and there were some unrecognized acute infections. Therefore, booster immunization of pertussis to HCWS should be actively considered.
Footnotes
Funding: This work was supported by a research grant from Korea University College of Medicine in 2011.
Disclosure: The authors have no potential conflicts of interest to disclosure.
- Conceptualization: Choi WS, Park DW.
- Data curation: Choi WS.
- Investigation: Choi WS, Kim SH, Park DW.
- Methodology: Choi WS, Park DW.
- Writing - original draft: Choi WS.
- Writing - review & editing: Park DW.
References
- 1.Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ. Pertussis: microbiology, disease, treatment, and prevention. Clin Microbiol Rev. 2016;29(3):449–486. doi: 10.1128/CMR.00083-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matlow AG, Nelson S, Wray R, Cox P. Nosocomial acquisition of pertussis diagnosed by polymerase chain reaction. Infect Control Hosp Epidemiol. 1997;18(10):715–716. doi: 10.1086/647519. [DOI] [PubMed] [Google Scholar]
- 3.Gehanno JF, Pestel-Caron M, Nouvellon M, Caillard JF. Nosocomial pertussis in healthcare workers from a pediatric emergency unit in France. Infect Control Hosp Epidemiol. 1999;20(8):549–552. doi: 10.1086/501667. [DOI] [PubMed] [Google Scholar]
- 4.Bassinet L, Matrat M, Njamkepo E, Aberrane S, Housset B, Guiso N. Nosocomial pertussis outbreak among adult patients and healthcare workers. Infect Control Hosp Epidemiol. 2004;25(11):995–997. doi: 10.1086/502332. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Outbreaks of pertussis associated with hospitals--Kentucky, Pennsylvania, and Oregon, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(3):67–71. [PubMed] [Google Scholar]
- 6.Pascual FB, McCall CL, McMurtray A, Payton T, Smith F, Bisgard KM. Outbreak of pertussis among healthcare workers in a hospital surgical unit. Infect Control Hosp Epidemiol. 2006;27(6):546–552. doi: 10.1086/506232. [DOI] [PubMed] [Google Scholar]
- 7.Baugh V, McCarthy N. Outbreak of Bordetella pertussis among oncology nurse specialists. Occup Med (Lond) 2010;60(5):401–405. doi: 10.1093/occmed/kqq051. [DOI] [PubMed] [Google Scholar]
- 8.Sydnor E, Perl TM. Healthcare providers as sources of vaccine-preventable diseases. Vaccine. 2014;32(38):4814–4822. doi: 10.1016/j.vaccine.2014.03.097. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh YH, Liu J, Tzeng YH, Wu J. Impact of visitors and hospital staff on nosocomial transmission and spread to community. J Theor Biol. 2014;356:20–29. doi: 10.1016/j.jtbi.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 10.The Korean Society of Infectious Diseases. Vaccination for Adult. 2nd ed. Seoul: MIP; 2012. [Google Scholar]
- 11.Lee SY, Han SB, Bae EY, Kim JH, Kang JH, Park YJ, et al. Pertussis seroprevalence in Korean adolescents and adults using anti-pertussis toxin immunoglobulin G. J Korean Med Sci. 2014;29(5):652–656. doi: 10.3346/jkms.2014.29.5.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SY, Choi UY, Kim JS, Ahn JH, Choi JH, Ma SH, et al. Immunoassay of pertussis according to ages. Korean J Pediatr Infect Dis. 2012;19(2):55–60. [Google Scholar]
- 13.Kim S, Oh H, Ham O, Chung MH, Seo W. Susceptibility and factors of pertussis vaccination adherence in Korean health care workers. Am J Health Behav. 2010;34(1):45–53. doi: 10.5993/ajhb.34.1.6. [DOI] [PubMed] [Google Scholar]
- 14.Rodríguez de la Pinta ML, Castro Lareo MI, Ramon Torrell JM, García de Lomas J, Devadiga R, Reyes J, et al. Seroprevalence of pertussis amongst healthcare professionals in Spain. Vaccine. 2016;34(8):1109–1114. doi: 10.1016/j.vaccine.2015.12.036. [DOI] [PubMed] [Google Scholar]
- 15.Mackey JE, Wojcik S, Long R, Callahan JM, Grant WD. Predicting pertussis in a pediatric emergency department population. Clin Pediatr (Phila) 2007;46(5):437–440. doi: 10.1177/0009922806297736. [DOI] [PubMed] [Google Scholar]
- 16.Wright SW, Edwards KM, Decker MD, Lamberth MM. Pertussis seroprevalence in emergency department staff. Ann Emerg Med. 1994;24(3):413–417. doi: 10.1016/s0196-0644(94)70177-6. [DOI] [PubMed] [Google Scholar]
- 17.Urbiztondo L, Broner S, Costa J, Rocamora L, Bayas JM, Campins M, et al. Seroprevalence study of B. pertussis infection in health care workers in Catalonia, Spain. Hum Vaccin Immunother. 2015;11(1):293–297. doi: 10.4161/hv.36167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24(5) Suppl:S58–S61. doi: 10.1097/01.inf.0000160914.59160.41. [DOI] [PubMed] [Google Scholar]
- 19.Choe YJ, Park YJ, Jung C, Bae GR, Lee DH. National pertussis surveillance in South Korea 1955–2011: epidemiological and clinical trends. Int J Infect Dis. 2012;16(12):e850–e854. doi: 10.1016/j.ijid.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 20.Choe YJ, Kim JW, Park YJ, Jung C, Bae GR. Burden of pertussis is underestimated in South Korea: a result from an active sentinel surveillance system. Jpn J Infect Dis. 2014;67(3):230–232. doi: 10.7883/yoken.67.230. [DOI] [PubMed] [Google Scholar]
- 21.Chungnam National University; Korea Center for Disease Control and Prevention. 2013 National Immunization Rate Survey. Cheongju: Korea Center for Disease Control and Prevention; 2014. [Google Scholar]
- 22.Sabbe M, Vandermeulen C. The resurgence of mumps and pertussis. Hum Vaccin Immunother. 2016;12(4):955–959. doi: 10.1080/21645515.2015.1113357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryu S, Kim JJ, Chen MY, Jin H, Lee HK, Chun BC. Outbreak investigation of pertussis in an elementary school: a case-control study among vaccinated students. Clin Exp Vaccine Res. 2018;7(1):70–75. doi: 10.7774/cevr.2018.7.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park S, Lee MG, Lee KH, Park YB, Yoo KH, Park JW, et al. A multicenter study of pertussis infection in adults with coughing in Korea: PCR-based study. Tuberc Respir Dis (Seoul) 2012;73(5):266–272. doi: 10.4046/trd.2012.73.5.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwon HJ, Yum SK, Choi UY, Lee SY, Kim JH, Kang JH. Infant pertussis and household transmission in Korea. J Korean Med Sci. 2012;27(12):1547–1551. doi: 10.3346/jkms.2012.27.12.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]