Abstract
The incidence of severe fever with thrombocytopenia syndrome (SFTS) has increased in Korea since a first report in 2013. We investigated whether SFTS existed before 2013 using real-time reverse transcription polymerase chain reaction and stored blood samples from febrile patients with thrombocytopenia. Four cases of SFTS were identified, with the earliest occurring in 2008.
Keywords: SFTS, Phlebovirus, Hemophagocytic Lymphohistiocytosis, Fever, Thrombocytopenia
Graphical Abstract
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging tick-born infectious disease that is caused by a phlebovirus named severe fever with thrombocytopenia syndrome virus (SFTSV).1 It was first discovered in China during 2009, and was subsequently detected in Korea and Japan during 2013–2014.1,2,3 The main SFTSV vector is ticks (Haemaphysalis longicornis) and the reservoir hosts are domestic animals in SFTS-endemic areas.4 Recent data indicate that the number of SFTS cases has been markedly increasing.5,6
The clinical features of SFTS are fever, gastrointestinal symptoms, leukopenia, thrombocytopenia, and elevated hepatic enzymes. In severe SFTS cases, multi-organ dysfunction develops and eventually leads to death, with case fatality rates of 6%–30%.1,5,6 Febrile patients with accompanying cytopenia often undergo a bone marrow examination to determine the cause of their illness,7 and it is possible that SFTS cases went undetected before the emergence of SFTS, although these cases could have undergone bone marrow examinations based on their fever and cytopenia. Interestingly, the first Korean case of SFTS in 2013 was identified based on isolation of SFTSV from a stored blood sample that was collected before the patient's death.3 Furthermore, retrospective studies have identified previously undiagnosed SFTS cases in Japan (2005) and in China (2006).2,8 Therefore, the present study aimed to determine whether unidentified SFTS cases existed in Korea before 2013.This retrospective study evaluated patients who had been admitted to a university-affiliated hospital that is located in southeastern Korea between 2008 and 2013. We selected 2008 at the start year considering the availability of blood samples used for the study.
The inclusion criteria were: 1) fever, 2) thrombocytopenia, 3) available bone marrow examination findings, 4) no clear hematological or microbiological diagnosis, and 5) available leftover blood samples. The blood samples had been preserved at –70ºC and were subjected to RNA extraction before real-time reverse transcription PCR was performed to amplify large, medium, and small SFTSV segments. Samples were considered positive for SFTSV if 2 or more segments were detected.
Records from patients with confirmed SFTSV infection were reviewed to determine their signs and symptoms at presentation, clinical course, laboratory findings, and bone marrow examination results. Based on the 2004 criteria,9 a diagnosis of hemophagocytic lymphohistiocytosis (HLH) was established for patients who fulfilled 5 or more of the following criteria: 1) fever, 2) splenomegaly, 3) cytopenia, 4) hypertriglyceridemia and/or hypofibrinogenemia, 5) hemophagocytosis in the bone marrow, spleen, or lymph nodes, 6) low or absent NK-cell activity, 7) ferritin levels of ≥ 500 µg/L, and 8) soluble CD25 levels of ≥ 2,400 U/mL.
The study was approved by the Institutional Review Board of Pusan National University Hospital (No. E-2013002), and the requirement for obtaining informed consents was waived due to the retrospective design.Among patients who were admitted with fever and thrombocytopenia during the study period, 35 patients fulfilled the inclusion criteria and their stored blood samples were tested for SFTSV infection. Four patients (11.4%) were considered positive for SFTSV infection, with the earliest case having occurred in 2008. All of these patients were male and lived in southeastern Korea, with a median age of 53 years (range, 21–62 years). The onset of their illnesses occurred between July and September, with 3 patients reporting previous outdoor activity and 1 patient having no clear epidemiological link for the SFTSV infection. Data regarding tick bites were not available.
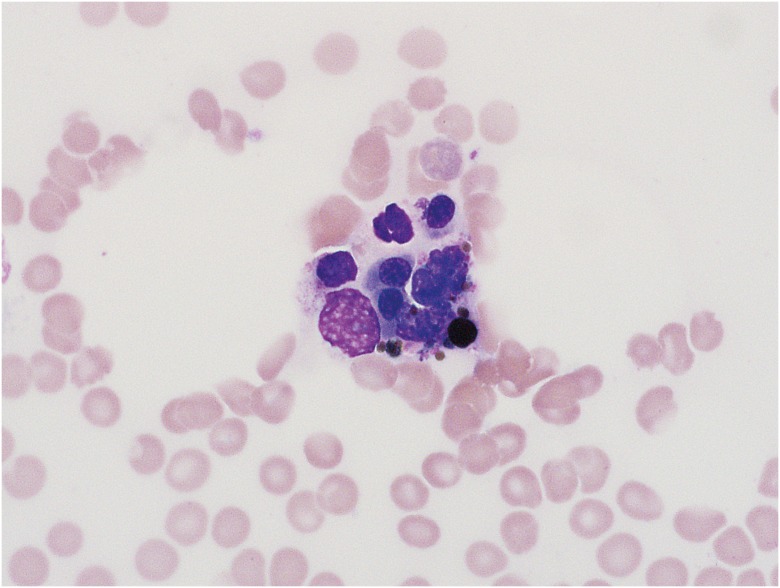
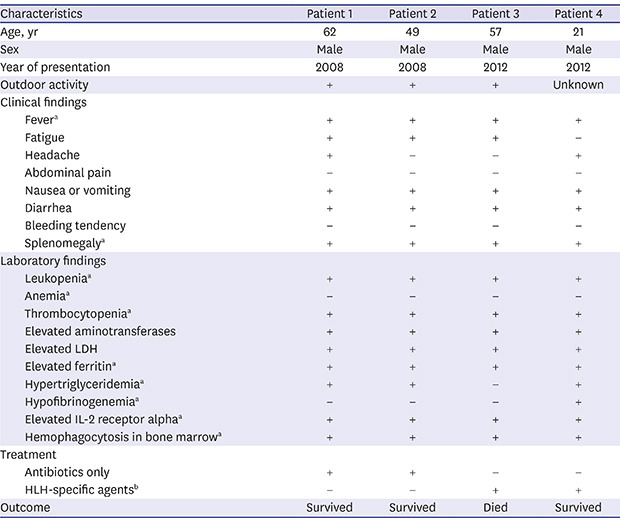
All patients exhibited fever, gastrointestinal symptoms (nausea, vomiting, or diarrhea), and splenomegaly (Table 1), although bleeding tendency was not detected. The common laboratory findings were leukopenia, thrombocytopenia, and elevated levels of aminotransferases, lactate dehydrogenase, ferritin, and soluble interleukin-2 receptor alpha. Hemophagocytosis were observed in the bone marrow of all patients (Fig. 1), which supported diagnosis of HLH according to the 2004 criteria.9 Two patients with mild symptoms were only empirically treated using antibiotics and 2 patients had been treated using HLH-specific chemo-immunotherapy, which included etoposide, dexamethasone, and intravenous immunoglobulin. One patient died after receiving chemo-immunotherapy.This study aimed to determine whether SFTS existed in Korea before the first reported case of SFTS in 2013.3 Among 35 febrile patients with thrombocytopenia during a 6-year period, we retrospectively determined that 4 patients had SFTS that occurred before 2013. Similar retrospective confirmation of SFTS cases dating back to 2005–2006 has been performed in China and Japan,2,8 and our data indicate that SFTS has also been circulating in Korea since at least 2008.
Table 1. Clinical features of 4 SFTS patients retrospectively confirmed using stored blood samples collected during 2008–2013 in Korea.
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|---|
| Age, yr | 62 | 49 | 57 | 21 | |
| Sex | Male | Male | Male | Male | |
| Year of presentation | 2008 | 2008 | 2012 | 2012 | |
| Outdoor activity | + | + | + | Unknown | |
| Clinical findings | |||||
| Fevera | + | + | + | + | |
| Fatigue | + | + | + | − | |
| Headache | + | − | − | + | |
| Abdominal pain | − | − | − | − | |
| Nausea or vomiting | + | + | + | + | |
| Diarrhea | + | + | + | + | |
| Bleeding tendency | − | − | − | − | |
| Splenomegalya | + | + | + | + | |
| Laboratory findings | |||||
| Leukopeniaa | + | + | + | + | |
| Anemiaa | − | − | − | − | |
| Thrombocytopeniaa | + | + | + | + | |
| Elevated aminotransferases | + | + | + | + | |
| Elevated LDH | + | + | + | + | |
| Elevated ferritina | + | + | + | + | |
| Hypertriglyceridemiaa | + | + | − | + | |
| Hypofibrinogenemiaa | − | − | − | + | |
| Elevated IL-2 receptor alphaa | + | + | + | + | |
| Hemophagocytosis in bone marrowa | + | + | + | + | |
| Treatment | |||||
| Antibiotics only | + | + | − | − | |
| HLH-specific agentsb | − | − | + | + | |
| Outcome | Survived | Survived | Died | Survived | |
SFTS = severe fever with thrombocytopenia syndrome, LDH = lactate dehydrogenase, IL = interleukin, HLH = hemophagocytic lymphohistiocytosis.
aDiagnostic criteria for HLH; bEtoposide, dexamethasone, and intravenous immunoglobulin.
Fig. 1. A hemophagocytic histiocyte containing erythroid cells and granulocytes in the bone marrow aspiration smear from patient No. 3 with SFTS (Wright-Giemsa stain, original magnification 1,000 ×).
SFTS = severe fever with thrombocytopenia syndrome.
After the emergence of SFTS in Korea, the annual numbers of reported SFTS cases have increased from 36 in 2013 to 165 in 2016, with an overall case fatality rate of 21.8% (73/335).10 The increased incidence of SFTS could be explained by an increasing awareness among physicians that has prompted improved surveillance and screening for suspected cases. For example, SFTS has now been recognized as an important differential diagnosis for Korean patients with fever and thrombocytopenia, along with scrub typhus, human granulocytic anaplasmosis, or hemorrhagic fever with renal syndrome.
All 4 of our retrospectively confirmed SFTS cases were also retrospectively diagnosed with HLH, which is a rapidly progressive life-threatening condition characterized by uncontrolled immune activation that can be triggered by severe infection, malignancy, or autoimmune disorders.9 Several cases of SFTS-associated HLH have already been reported,2,11 and SFTS should be considered a possible infectious cause of HLH in SFTS-endemic areas, in addition to infection with the Epstein-Barr virus or cytomegalovirus.7 Among 4 of our patients with SFTS-associated HLH, 2 were treated with supportive care only. The other 2 received specific chemo-immunotherapy for HLH; 1 of them died despite receiving treatment using HLH-specific agents. Chemo-immunotherapy remains the main treatment for primary HLH, although control of the underlying disease is also important for treating secondary HLH.7 However, there are no clinically effective antiviral therapies or vaccines for SFTS, although some reports have described in vitro activity for ribavirin and interferon.12,13 Several clinical trials have examined plasma exchange with or without ribavirin, intravenous immunoglobulin, and corticosteroids,14,15 although there is no consensus regarding the ideal treatment for SFTS. Considering the increasing incidence and high fatality rate of SFTS, further studies are needed to develop effective therapies.
The present study has two important limitations. First, our center is located in southeastern Korea, which has a lower incidence of SFTS than other regions of Korea.5 Thus, cases earlier than those reported here might be identified if a nationwide retrospective survey was performed. Second, we only included patients who were considered ill enough to warrant a bone marrow examination, and it is possible that undetected mild SFTS cases have occurred among patients with fever and cytopenia who did not undergo a bone marrow examination.
In conclusion, the present study revealed that SFTS has been circulating in Korea since at least 2008, as we retrospectively identified 4 patients with SFTS-associated HLH. Therefore, SFTS should be suspected as a possible cause of HLH in SFTS-endemic areas.
ACKNOWLEDGMENTS
The authors would like to acknowledge Hyerin Kim for the photomicrograph.
Footnotes
Funding: This work was supported by the Basic Science Research Program through the National Research Foundation of Korea, which was funded by the Ministry of Education (NRF-2014R1A1A4A01009748).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim KH, Yi J.
- Data curation: Kim KH, Ko MK, Lee EY, Yi J.
- Formal analysis: Kim KH, Lee MJ, Ko MK, Yi J.
- Funding acquisition: Yi J.
- Methodology: Kim KH, Ko MK, Yi J.
- Writing - original draft: Kim KH, Lee MJ, Yi J.
- Writing - review & editing: Kim KH, Lee MJ, Yi J.
References
- 1.Yu XJ, Liang MF, Zhang SY, Liu Y, Li JD, Sun YL, et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med. 2011;364(16):1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takahashi T, Maeda K, Suzuki T, Ishido A, Shigeoka T, Tominaga T, et al. The first identification and retrospective study of severe fever with thrombocytopenia syndrome in Japan. J Infect Dis. 2014;209(6):816–827. doi: 10.1093/infdis/jit603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim KH, Yi J, Kim G, Choi SJ, Jun KI, Kim NH, et al. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerg Infect Dis. 2013;19(11):1892–1894. doi: 10.3201/eid1911.130792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niu G, Li J, Liang M, Jiang X, Jiang M, Yin H, et al. Severe fever with thrombocytopenia syndrome virus among domesticated animals, China. Emerg Infect Dis. 2013;19(5):756–763. doi: 10.3201/eid1905.120245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi SJ, Park SW, Bae IG, Kim SH, Ryu SY, Kim HA, et al. Severe fever with thrombocytopenia syndrome in South Korea, 2013–2015. PLoS Negl Trop Dis. 2016;10(12):e0005264. doi: 10.1371/journal.pntd.0005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun J, Lu L, Wu H, Yang J, Ren J, Liu Q. The changing epidemiological characteristics of severe fever with thrombocytopenia syndrome in China, 2011–2016. Sci Rep. 2017;7(1):9236. doi: 10.1038/s41598-017-08042-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisman DN. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6(6):601–608. doi: 10.3201/eid0606.000608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Li Q, Hu W, Wu J, Wang Y, Mei L, et al. Person-to-person transmission of severe fever with thrombocytopenia syndrome virus. Vector Borne Zoonotic Dis. 2012;12(2):156–160. doi: 10.1089/vbz.2011.0758. [DOI] [PubMed] [Google Scholar]
- 9.Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 10.Korea Centers for Disease Control and Prevention. Disease web statistics system. [Updated 2018]. [Accessed March 21, 2018]. https://is.cdc.go.kr/dstat/jsp/stat/stat0001.jsp.
- 11.Kim N, Kim KH, Lee SJ, Park SH, Kim IS, Lee EY, et al. Bone marrow findings in severe fever with thrombocytopenia syndrome: prominent haemophagocytosis and its implication in haemophagocytic lymphohistiocytosis. J Clin Pathol. 2016;69(6):537–541. doi: 10.1136/jclinpath-2015-203417. [DOI] [PubMed] [Google Scholar]
- 12.Lee MJ, Kim KH, Yi J, Choi SJ, Choe PG, Park WB, et al. In vitro antiviral activity of ribavirin against severe fever with thrombocytopenia syndrome virus. Korean J Intern Med. 2017;32(4):731–737. doi: 10.3904/kjim.2016.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shimojima M, Fukushi S, Tani H, Taniguchi S, Fukuma A, Saijo M. Combination effects of ribavirin and interferons on severe fever with thrombocytopenia syndrome virus infection. Virol J. 2015;12(1):181. doi: 10.1186/s12985-015-0412-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim UJ, Kim DM, Ahn JH, Kang SJ, Jang HC, Park KH, et al. Successful treatment of rapidly progressing severe fever with thrombocytopenia syndrome with neurological complications using intravenous immunoglobulin and corticosteroid. Antivir Ther. 2016;21(7):637–640. doi: 10.3851/IMP3036. [DOI] [PubMed] [Google Scholar]
- 15.Oh WS, Yoo JR, Kwon KT, Kim HI, Lee SJ, Jun JB, et al. Effect of early plasma exchange on survival in patients with severe fever with thrombocytopenia syndrome: a multicenter study. Yonsei Med J. 2017;58(4):867–871. doi: 10.3349/ymj.2017.58.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]