Abstract
Objectives
To assess the extent of interaction between body mass index (BMI) and triglyceride (TG) level and its effects on blood pressure (BP) in elderly individuals in China.
Design
Cross-sectional study.
Setting
Data were taken from a cross-sectional study called the China Health and Retirement Longitudinal Study.
Participants
The analytic sample included 3629 subjects aged 45 to 96 years.
Main Outcome Measurements
Data were obtained from the China Health and Retirement Longitudinal Study, which is a cross-sectional study. Age-adjusted partial Pearson's correlation test was used to compare various characteristics and BP. Adjusted associations were first used as linear regression models, as appropriate. Then, general linear models adjusted for related potential confounders were used to examine the synergistic effects of BMI and TG level on BP. Finally, a binary logistic regression model adjusted for confounding factors was used to examine the association between BMI or TG level and hypertension.
Results
Age-adjusted partial Pearson's correlation coefficient showed that the TG level was positively correlated with both systolic blood pressure (SBP) and diastolic blood pressure (DBP) in both men and women with BMI < 24.0 kg/m2; however, TG level was positively correlated with DBP in women with BMI ≥ 24.0 kg/m2 but not with DBP in men with BMI ≥ 24.0 kg/m2. Multiple linear regression analysis showed that BMI level was significantly and positively associated with both SBP and DBP in men and women with BMI < 24.0 kg/m2, and TG level was significantly and positively associated with SBP in women with BMI < 24.0 kg/m2, independent of other confounding factors. A general linear model analysis with adjustment for confounding factors (age, educational level, marital status, current residence, smoking, eating habits, taking activities, antidiabetic medication, antihypertensive therapy, fasting plasma glucose [FPG], low-density lipoprotein cholesterol [LDL-C], estimated glomerular filtration rate [eGFR], and serum uric acid [SUA]) showed no interaction between BMI and TG level and SBP (men, β = 0.572, P = 0.845; women, β = 0.122, P = 0.923) and DBP (men, β = -0.373, P = 0.810; women, β = 0.272, P = 0.828). A binary logistic regression model analysis with adjustment for confounding factors (age, educational level, marital status, current residence, smoking, drinking, eating habits, taking activities, major accidental injury, physical activity, history of cardiovascular disease, history of liver disease, antilipidemic medication, antidiabetic medication, antihypertensive therapy, FPG, LDL-C, high-density lipoprotein cholesterol [HDL-C], eGFR, and SUA) showed that overweight and obese men and women were more likely to have hypertension (men: odds ratio [OR] = 1.781, 95% confidence interval [CI] = 1.393–2.277; women: OR = 1.653, 95% CI = 1.330–2.055) and women with high TG were more likely to have hypertension (OR = 1.558, 95% CI = 1.219–1.992).
Conclusion
An interactive effect of BMI and TG level on BP was not observed in either men or women; however, independent effects of BMI on BP were observed in both men and women, and an association between TG level and hypertension was observed in women.
1. Introduction
The prevalence of hypertension has dramatically increased in the past few years in China[1, 2]; furthermore, the rate of hypertension is disproportionately high among elderly individuals in this country[3–5]. Hypertension is defined as a diastolic blood pressure (DBP) of ≥ 90 mmHg and/or systolic blood pressure (SBP) of ≥ 140 mmHg based on the evidence of modestly increasing risk[6–8] and incidence of cardiovascular disease (CVD)[9–11].
Hypertension is a complex disease, and patients with the condition suffer from an economic, psychosocial, and physical burden. Recently, hypertension has become an important global public health challenge [12]. Therefore, an effective strategy to prevent hypertension and determine its associated risks should be carefully implemented. Numerous studies[13–20] have been conducted to determine the risk factors for hypertension, such as aging, overweight, central obesity, lifestyle, family history of hypertension, history of diabetes and dyslipidemia, lack of physical activity, smoking, alcohol consumption, low-density lipoprotein cholesterol (LDL-C) level, triglycerides (TG) level, and high-density lipoprotein cholesterol (HDL-C) level. Lipid abnormalities have been shown to increase the risk factors for hypertension [21]. For example, Teng [22] found an additive effect of TG on DBP. Brennan [23] conducted a study to investigate the effects of body weight on TG and SBP in individuals aged 20 to 49 years and found that, in men, significant correlations with BMI were found for all variables, while in women younger than 40, only the correlation with BP was significant. TG level has been associated with BP since TG level itself can lead to endothelial dysfunction [24, 25], arterial stiffness [26], and loss of vasomotor reactivity [27]. However, it is also important to understand the interrelationships among various risk factors for hypertension. In particular, the association between TG level and risk of hypertension and the effects of obesity on this association are of considerable interest, and an interactive effect between body mass index (BMI) and TG level on BP may also be considered.
No consistent recognition of the association and interaction analysis between BMI and TG level and BP in elderly individuals exists. Thus, the present study particularly aimed to determine the prevalence of normotension and hypertension and their association with BMI, TG level, and other confounding factors based on sex, using cross-sectional data from community-dwelling individuals aged ≥ 60 years in China.
2. Methods
2.1. Study Design and Setting
Data for this cross-sectional study were taken from the China Health and Retirement Longitudinal Study (CHARLS), a biennial and nationally representative longitudinal survey conducted by the China Centre for Economic Research at Peking University [28]. The baseline survey had a four-stage, stratified, cluster probability sampling design.
In the first stage, all counties in China were stratified by region, rural/urban status, and gross domestic product per capita. A random sample of 150 counties was selected to represent the socioeconomic and geographic pattern of all the counties. In the second stage, three primary sampling units (PSUs) were selected in each county with the probability of inclusion of each county in the sample proportional to their population size. In the third stage, all households in each selected PSU were mapped, and a random sample of 24 households was selected among all the households with residents aged ≥ 45 years within each PSU. Finally, for each selected household, one resident aged ≥ 45 years was randomly selected as a participant in the survey. From the 2011 CHARLS Wave1, we included a total of 3629 individuals in our study.
2.2. Information on Demographic Characteristics and Self-Reported Risk Factors
Data including age, education, marital status, current residence, smoking, drinking, eating habits, taking activities, accidental injury, physical exercise, history of cardiovascular disease, history of liver disease, antilipidemic medication, antidiabetic medication, and antihypertensive therapy were obtained using a self-reported questionnaire. (1) Median age was 68 years, and age was categorized as < 68 years and ≥ 68 years. (2) Educational levels were classified into illiterate, less than elementary school, high school, and above vocational school. (3) Marital status was classified into married and single. (4) Current residence was classified into rural and urban. (5) Smoking status was never smoked, ex-smoker, and current smoker. (6) Alcohol consumption was classified into more than non-drinker, less than once a month, and once a month. (7) Eating habits were categorized into 2 meals per day or fewer, 3 meals per day, and 4 meals per day or more. (8) Activity status was dichotomized into at least once a month versus never. (9) Major accidental injury information was obtained by asking the participant whether he/she suffered from any type of major accidental injury and received medical treatment; the answer was “yes” or “no.” (10) Regular physical exercise was defined as exercising at least 3 days per week and more than 30 minutes per day, including moderate to vigorous physical activity and walking. (11) History of CVD, history of liver disease, antilipidemic medication, antidiabetic medication, and antihypertensive therapy were defined as a history of receiving treatment for the respective diseases; the answer was “yes” or “no.”
2.3. Glucose, LDL, HDL, Triglycerides, eGFR, BP, and Uric Acid Measurement
Venous blood samples were obtained at the Centers for Disease Control and Prevention (CDC) station, then immediately stored and frozen at −20°C, and transported within 2 weeks to the Chinese CDC in Beijing, where they were placed in a deep freezer and stored at −80°C until the relevant assay was performed at the China Medical University laboratory. (1) Fasting plasma glucose (FPG), LDL, HDL, and TG levels were analyzed at the Youanmen Center for Clinical Laboratory at Capital Medical University using the enzymatic colorimetric tests, and serum uric acid (SUA) levels were analyzed using the urinalysis (UA) plus method. We classified TG levels into 2 categories: ≥ 150 mg/dL and < 150 mg/dL, a categorization widely used in previous studies [29, 30]. (2) BP was measured 3 times at intervals of 45 seconds with a sphygmomanometer. The value of BP was determined based on the mean of the 3 measurements. Normotension was defined as absence of antihypertensive therapy with an SBP of < 140 mmHg and DBP of < 90 mmHg, while hypertension was defined as an SBP of ≥140 mmHg and/or DBP of ≥ 90 mmHg; this categorization has been widely used in previous studies. (3) Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI creatinine-cystatin equations [31]: (1) in men, serum creatinine (Scr) ≤ 0.9, serum cystatin C(Scys) ≤ 0.8, eGFR = 135∗ (Scr/0.9)−0.207∗ (Scys/0.8)−0.375∗0.995age; Scr≤ 0.9, Scys> 0.8, eGFR = 135∗ (Scr/0.9)−0.207∗ (Scys/0.8)−0.711∗0.995age; Scr> 0.9, Scys≤ 0.8, eGFR=135∗ (Scr/0.9)−0.601∗ (Scys/0.8)−0.375∗0.995age; Scr> 0.9, Scys> 0.8, eGFR = 135∗ (Scr/0.9)−0.601∗ (Scys/0.8)−0.711∗0.995age; (2) in women, Scr ≤ 0.7, Scys ≤ 0.8, eGFR = 130∗(Scr/0.7)−0.248∗(Scys/0.8)−0.375∗0.995age; Scr≤ 0.7, Scys> 0.8, and eGFR = 130∗(Scr/0.7)−0.248∗(Scys/0.8)−0.711∗0.995age; Scr> 0.7, Scys≤ 0.8, eGFR = 130∗ (Scr/0.7)−0.601∗(Scys/0.8)−0.375∗0.995age; Scr> 0.7, Scys> 0.8, and eGFR = 130∗ (Scr/0.7)−0.601∗ (Scys/0.8)−0.711∗0.995age.
2.4. Measurement of Body Mass Index
Weight and height were measured using a weight and height measurement instrument. BMI was calculated based on the measured weight and height of the participants, who were classified into four categories: underweight (BMI, ≤ 18.5 kg/m2), normal weight (18.5–24 kg/m2), overweight (24–28 kg/m2), and obese (> 28 kg/m2)[32].
2.5. Statistical Analysis
Our data are represented as mean ± standard deviation (SD; continuous data) and number and percentage (categorical data). Differences between normotension and hypertension, or between normal weight individuals and those with underweight or adiposity, were evaluated using the t-test or chi-square test, followed by Bonferroni adjustment. Correlations between various characteristics and BP were compared using the age-adjusted partial Pearson's correlation test. The adjusted associations between various characteristics and BP were first compared using linear regression models, as appropriate. Then, general linear models adjusted for related potential confounders (age, educational level, marital status, current residence, smoking, drinking, eating habits, taking activities, major accidental injury, physical activity, history of CVD, history of liver disease, antilipidemic medication, antidiabetic medication, antihypertensive therapy, FPG, LDL-C, HDL-C, eGFR, and SUA) [33] were constructed to examine the synergistic effect of BMI and TG level on BP. A binary logistic regression model adjusted for related potential confounders was used to examine the association between BMI or TG and hypertension. A P-value of 0.05 was considered significant. All data were analyzed using the SPSS version 17.0 (IBM Corp., Armonk, NY, USA).
2.6. Patient and Public Involvement Statement
Consent from the respondents was obtained by the CHARLS. The data information obtained from the study was public, and patients were not involved.
3. Results
The 2011 CHARLS Wave1 sample (N=3629) consists of 49.88% men (Age: Mean = 68.86 years; SD = 6.30; range, 60–93 years) and 50.12% women (Age: Mean = 68.55 years; SD = 6.82; range, 60–96 years). Among men, the mean SBP and DBP were 128.93 mmHg and 72.28 mmHg, respectively, and among women, the mean SBP and DBP were 133.66 mmHg and 73.00 mmHg, respectively. In men, 10.94%, 60.66%, 21.60%, and 6.80% were underweight, normal weight, overweight, and obese, respectively, whereas in women 10.34%, 49.04%, 29.08%, and 11.54% were underweight, normal weight, overweight, and obese, respectively. The mean and SD of TG level were 112.79 ± 83.55 mg/dL in men and 140.14 ± 94.12 mg/dL in women. Tables 1 and 2 present the baseline characteristics of the sample for all variables, and most variables were based on our previous research [32].
Table 1.
Various characteristics of participants categorized by BMI in male (N=1810).
| Variables | BMI≤18.5 (n=198) |
BMI18.5-24 (n=1098) | BMI 24-28 (n=391) | BMI>28 (n=123) |
t/χ2 | P |
|---|---|---|---|---|---|---|
| Age(years) | 71.49±6.31 | 69.17±6.4 | 67.35±5.71 | 66.7±5.22 | 25.817 | <0.001 |
| Education | ||||||
| Illiterate | 52(26.26) | 256(23.32) | 44(11.25) | 20(16.26) | 42.976 | <0.001 |
| Less than elementary school | 130(65.66) | 773(70.40) | 306(78.26) | 90(73.17) | ||
| High school | 6(3.03) | 17(1.55) | 5(1.28) | 4(3.25) | ||
| Above vocational school | 10(5.05) | 52(4.74) | 36(9.21) | 9(7.32) | ||
| Marital status | ||||||
| Single | 29(14.65) | 179(16.30) | 30(7.67) | 13(10.57) | 19.2333 | <0.001 |
| Married | 169(85.35) | 919(83.70) | 361(92.33) | 110(89.43) | ||
| Current residence | ||||||
| Rural | 152(76.77) | 791(72.04) | 213(54.48) | 65(52.85) | 60.303 | <0.001 |
| Urban | 46(23.23) | 307(27.96) | 178(45.52) | 58(47.15) | ||
| Smoke | ||||||
| NO | 118(59.60) | 632(57.56) | 163(41.69) | 48(39.02) | 43.161 | <0.001 |
| Former smoke | 36(18.18) | 199(18.12) | 105(26.85) | 33(26.83) | ||
| Current smoke | 44(22.22) | 267(24.32) | 123(31.46) | 42(34.15) | ||
| Drinking | ||||||
| NO | 115(58.08) | 543(49.45) | 202(51.66) | 65(52.85) | 197.72 | <0.001 |
| Less than once a month | 13(6.57) | 94(8.56) | 33(8.44) | 14(11.38) | ||
| More than once a month | 70(35.35) | 461(41.99) | 156(39.9) | 44(35.77) | ||
| Eating meals | ||||||
| ≤2 meals per day | 31(15.66) | 174(15.85) | 43(11.00) | 10(8.13) | 15.580 | 0.016 |
| 3 meals per day | 162(81.82) | 905(82.42) | 345(88.24) | 113(91.87) | ||
| ≥4 meals per day | 5(2.53) | 19(1.73) | 3(0.77) | 0(0.00) | ||
| Taking activities | ||||||
| No | 119(60.10) | 593(54.01) | 175(44.76) | 62(50.41) | 15.198 | 0.002 |
| Yes | 79(39.90) | 505(45.99) | 216(55.24) | 61(49.59) | ||
| Ever been in major accidental injury | ||||||
| No | 173(87.37) | 976(88.89) | 349(89.26) | 111(90.24) | 0.743 | 0.863 |
| Yes | 25(12.63) | 122(11.11) | 42(10.74) | 12(9.76) | ||
| Having regular physical exercises | ||||||
| No physical exercise | 122(61.62) | 701(63.84) | 247(63.17) | 69(56.1) | 5.204 | 0.518 |
| Less than regular physical exercises | 39(19.70) | 183(16.67) | 60(15.35) | 23(18.70) | ||
| Regular physical exercises | 37(18.69) | 214(19.49) | 84(21.48) | 31(25.20) | ||
| History of CVD | ||||||
| No | 178(89.90) | 965(87.89) | 323(82.61) | 87(70.73) | 33.007 | <0.001 |
| Yes | 20(10.10) | 133(12.11) | 68(17.39) | 36(29.27) | ||
| History of liver diseases | ||||||
| No | 194(97.98) | 1055(96.08) | 375(95.91) | 114(92.68) | 5.576 | 0.134 |
| Yes | 4(2.02) | 43(3.92) | 16(4.09) | 9(7.32) | ||
| Antilipidemic medication | ||||||
| No | 194(97.98) | 1063(96.81) | 366(93.61) | 104(84.55) | 43.969 | <0.001 |
| Yes | 4(2.02) | 35(3.19) | 25(6.39) | 19(15.45) | ||
| Anti-diabetic medication | ||||||
| No | 195(98.48) | 1069(97.36) | 365(93.35) | 104(84.55) | 54.001 | <0.001 |
| Yes | 3(1.52) | 29(2.64) | 26(6.65) | 19(15.45) | ||
| Anti-hypertensive therapy | ||||||
| No | 186(93.94) | 1036(94.35) | 359(91.82) | 114(92.68) | 3.345 | 0.341 |
| Yes | 12(6.06) | 62(5.65) | 32(8.18) | 9(7.32) | ||
| Fasting plasma glucose(mg/dl) | 105.00±28.94 | 109.16±36.00 | 118.37±41.50 | 119.64±41.26 | 9.994 | <0.001 |
| LDL Cholesterol (mg/dl) | 105.37±32.12 | 110.54±32.35 | 118.02±35.30 | 119.42±34.05 | 9.701 | <0.001 |
| HDL Cholesterol (mg/dl) | 60.04±16.14 | 53.83±15.90 | 44.00±13.320 | 42.9±12.28 | 74.457 | <0.001 |
| eGFR(ml/min/1.73m2) | 71.56±16.22 | 74.92±16.53 | 75.57±16.32 | 75.13±16.23 | 2.868 | 0.035 |
| Serum uric acid(mg/dl) | 4.79±1.29 | 4.98±1.31 | 5.37±1.34 | 5.27±1.29 | 12.990 | <0.001 |
| Systolic blood pressure(mmHg) | 128.93±21.56 | 132.59±24.29 | 139.25±25.58 | 143.94±19.85 | 23.845 | <0.001 |
| Diastolic blood pressure(mmHg) | 72.28±12.34 | 74.59±12.78 | 78.65±12.37 | 81.69±12.29 | 17.079 | <0.001 |
| Body mass index(kg/m2) | 17.24±0.90 | 21.25±1.53 | 25.65±1.12 | 30.71±4.3.00 | 2126.849 | <0.001 |
| Triglycerides (mg/dl) | 84.34±34.71 | 101.52±59.33 | 146.98±129.67 | 150.5±92.37 | 47.962 | <0.001 |
Table 2.
Various characteristics of participants categorized by BMI in female (N=1819).
| Variables | BMI≤18.5 (n=188) |
BMI18.5-24 (n=892) | BMI 24-28 (n=529) | BMI>28 (n=210) |
t/χ2 | P |
|---|---|---|---|---|---|---|
| Age (years) | 71.41±7.07 | 68.77±6.99 | 67.64±6.32 | 67.34±6.25 | 17.169 | <0.001 |
| Education | ||||||
| Illiterate | 133(70.74) | 530(59.42) | 269(50.85) | 111(52.86) | 35.807 | <0.001 |
| Less than elementary school | 55(29.26) | 342(38.34) | 236(44.61) | 97(46.19) | ||
| High school | 0(0.00) | 6(0.67) | 9(1.70) | 0(0.00) | ||
| Above vocational school | 0(0.00) | 14(1.57) | 15(2.84) | 2(0.95) | ||
| Marital status | ||||||
| Single | 72(38.30) | 291(32.62) | 131(24.76) | 49(23.33) | 20.478 | <0.001 |
| Married | 116(61.70) | 601(67.38) | 398(75.24) | 161(76.67) | ||
| Current residence | ||||||
| Rural | 150(79.79) | 588(65.92) | 309(58.41) | 107(50.95) | 43.911 | <0.001 |
| Urban | 38(20.21) | 304(34.08) | 220(41.59) | 103(49.05) | ||
| Smoke | ||||||
| NO | 151(80.32) | 783(87.78) | 479(90.55) | 190(90.48) | 20.377 | <0.001 |
| Former smoke | 6(3.19) | 30(3.36) | 15(2.84) | 8(3.81) | ||
| Current smoke | 31(16.49) | 79(8.86) | 35(6.62) | 12(5.71) | ||
| Drinking | ||||||
| NO | 164(87.23) | 781(87.56) | 462(87.33) | 194(92.38) | 7.632 | 0.266 |
| Less than once a month | 10(5.32) | 32(3.59) | 27(5.10) | 6(2.86) | ||
| More than once a month | 14(7.45) | 79(8.86) | 40(7.56) | 10(4.76) | ||
| Eating meals | ||||||
| ≤2 meals per day | 48(25.53) | 143(16.03) | 58(10.96) | 18(8.57) | 32.785 | <0.001 |
| 3 meals per day | 139(73.94) | 732(82.06) | 463(87.52) | 189(90.00) | ||
| ≥4 meals per day | 1(0.53) | 17(1.91) | 8(1.51) | 3(1.43) | ||
| Taking activities | ||||||
| No | 113(60.11) | 490(54.93) | 241(45.56) | 100(47.62) | 19.191 | <0.001 |
| Yes | 75(39.89) | 402(45.07) | 288(54.44) | 110(52.38) | ||
| Ever been in major accidental injury | ||||||
| No | 173(92.02) | 830(93.05) | 490(92.63) | 197(93.81) | 0.573 | 0.903 |
| Yes | 15(7.98) | 62(6.95) | 39(7.37) | 13(6.19) | ||
| Having regular physical exercises | ||||||
| No physical exercise | 134(71.28) | 569(63.79) | 322(60.87) | 132(62.86) | 9.032 | 0.172 |
| Less than regular physical exercises | 25(13.30) | 172(19.28) | 99(18.71) | 36(17.14) | ||
| Regular physical exercises | 29(15.43) | 151(16.93) | 108(20.42) | 42(20.00) | ||
| History of CVD | ||||||
| No | 160(85.11) | 757(84.87) | 428(80.91) | 158(75.24) | 13.931 | 0.003 |
| Yes | 28(14.89) | 135(15.13) | 101(19.09) | 52(24.76) | ||
| History of liver diseases | ||||||
| No | 183(97.34) | 864(96.86) | 504(95.27) | 203(96.67) | 3.289 | 0.349 |
| Yes | 5(2.66) | 28(3.14) | 25(4.73) | 7(3.33) | ||
| Antilipidemic medication | ||||||
| No | 185(98.40) | 854(95.74) | 474(89.60) | 178(84.76) | 49.744 | <0.001 |
| Yes | 3(1.60) | 38(4.26) | 55(10.40) | 32(15.24) | ||
| Anti-diabetic medication | ||||||
| No | 187(99.47) | 863(96.75) | 490(92.63) | 188(89.52) | 33.154 | <0.001 |
| Yes | 1(0.53) | 29(3.25) | 39(7.37) | 22(10.48) | ||
| Anti-hypertensive therapy | ||||||
| No | 171(90.96) | 838(93.95) | 495(93.57) | 191(90.95) | 33.154 | <0.001 |
| Yes | 17(9.04) | 54(6.05) | 34(6.43) | 19(9.05) | ||
| Fasting plasma glucose (mg/dl) | 105.18±22.29 | 110.63±40.95 | 118.34±48.98 | 116.55±35.01 | 6.659 | <0.001 |
| LDL Cholesterol (mg/dl) | 115.41±33.67 | 122.84±34.65 | 127.66±38.90 | 128.45±41.61 | 6.511 | <0.001 |
| HDL Cholesterol (mg/dl) | 60.31±16.04 | 54.55±15.13 | 47.67±13.02 | 45.26±11.70 | 62.326 | <0.001 |
| eGFR (ml/min/1.73m2) | 72.49±16.54 | 75.97±16.10 | 77.40±15.8 | 75.16±18.06 | 4.396 | 0.004 |
| Serum uric acid (mg/dl) | 3.83±1.14 | 4.06±1.12 | 4.30±1.14 | 4.62±1.22 | 21.304 | <0.001 |
| Systolic blood pressure (mmHg) | 133.66±24.74 | 136.74±23.69 | 141.83±30.53 | 146.33±38.15 | 19.704 | <0.001 |
| Diastolic blood pressure (mmHg) | 73.00±12.26 | 75.01±11.77 | 78.61±12.06 | 79.54±12.23 | 10.742 | <0.001 |
| Body mass index (kg/m2) | 17.13±1.42 | 21.43±1.50 | 25.73±1.15 | 30.90±4.33 | 2202.200 | <0.001 |
| Triglycerides (mg/dl) | 103.17±50.81 | 128.46±82.33 | 158.53±100.30 | 176.54±128.24 | 33.113 | <0.001 |
Tables 1 and 2 show the various characteristics of participants categorized on basis of BMI. The participants comprised 1,810 men aged 68.86 ± 6.30 (range: 60–93) years and 1,819 women aged 68.55 ± 6.82 (range, 60–96) years. According to the modified Chinese criteria for BMI [34], the mean BMI in men was 22.41 kg/m2 (SD, 3.71), with 10.94% underweight (BMI, < 18.5 kg/m2), 60.66% normal weight (BMI, 18.5–24 kg/m2), 21.60% overweight, and 6.80% obese (BMI, ≥ 28 kg/m2), whereas the mean BMI in women was 23.33 kg/m2 (SD, 4.23), with 10.34% underweight (BMI, < 18.5 kg/m2), 49.04% normal weight (BMI, 18.5–24 kg/m2), 29.08% overweight, and 11.54% obese (BMI, ≥ 28 kg/m2). Table 1 shows the background characteristics of male participants categorized based on BMI. Levels of FPG, LDL-C, TG, eGFR, SUA, SBP, and DBP were significantly higher in the high BMI group than in the low BMI group, whereas HDL-C level was higher in the low BMI group than in the high BMI group. However, between-group differences in the prevalence of major accidental injury, regular physical exercise, history of liver disease, and antihypertensive therapy were not observed. In women, levels of FBG, LDL-C, TG, eGFR, SUA, SBP, and DBP were significantly higher in the high BMI group than those in the low BMI group, but HDL-C level was higher in the low BMI group than in the high BMI group. However, between-group differences in categories of alcohol drinking, major accidental injury, physical activity, and history of liver disease were not observed (Table 2).
Tables 3 and 4 show the characteristics of participants categorized by BMI and BP status. First, in the hypertensive group with a BMI < 24.0 kg/m2 in men, levels of glucose, LDL-C, BMI, SUA, SBP, and DBP were significantly higher than those in the hypertensive group, but eGFR level was significantly higher than that in the normotensive group. Second, in the hypertensive group with a BMI ≥ 24.0 kg/m2 in men, levels of SUA, SBP, and DBP were also significantly higher, but eGFR level was significantly lower than that in the normotensive group (shown in Table 3). Third, in the hypertensive group with a BMI < 24.0 kg/m2 in women, levels of TG, SUA, SBP, DBP, and the prevalence of antilipidemic medication were significantly higher than those in the normotensive group, but eGFR level was significantly lower. Lastly, in the hypertensive group with a BMI ≥ 24.0 kg/m2 in women, the prevalence of CVD, antilipidemic medication, and antidiabetic medication were significantly higher, as were levels of glucose, TG, SBP, and DBP (Table 4).
Table 3.
Characteristics of participants categorized by BMI and blood pressure status in male (N=1810).
| Variables | BMI24(n=1296) | t/χ2 | P | BMI≥24 (n=514) | t/χ2 | P | ||
|---|---|---|---|---|---|---|---|---|
| Normotension (n=866) |
Hypertension (n=430) |
Normotension (n=276) |
Hypertension (n=238) |
|||||
| Age(years) | 68.99±6.42 | 70.53±6.33 | -4.080 | <0.001 | 66.84±5.47 | 67.55±5.71 | -1.439 | 0.151 |
| Education | ||||||||
| Illiterate | 200(23.09) | 108(25.12) | 6.278 | 0.099 | 37(13.41) | 27(11.34) | 0.776 | 0.855 |
| Less than elementary school | 600(69.28) | 303(70.47) | 211(76.45) | 185(77.73) | ||||
| High school | 20(2.31) | 3(0.70) | 4(1.45) | 5(2.10) | ||||
| Above vocational school | 46(5.31) | 16(3.72) | 24(8.70) | 21(8.82) | ||||
| Marital status | ||||||||
| Single | 122(14.09) | 86(20.00) | 7.454 | 0.006 | 20(7.25) | 23(9.66) | 0.974 | 0.324 |
| Married | 744(85.91) | 344(80.00) | 256(92.75) | 215(90.34) | ||||
| Current residence | ||||||||
| Rural | 638(73.67) | 305(70.93) | 1.090 | 0.296 | 155(56.16) | 123(51.68) | 1.032 | 0.310 |
| Urban | 228(26.33) | 125(29.07) | 121(43.84) | 115(48.32) | ||||
| Smoke | ||||||||
| NO | 487(56.24) | 263(61.16) | 2.980 | 0.225 | 103(37.32) | 108(45.38) | 3.691 | 0.158 |
| Former smoke | 165(19.05) | 70(16.28) | 81(29.35) | 57(23.95) | ||||
| Current smoke | 214(24.71) | 97(22.56) | 92(33.33) | 73(30.67) | ||||
| Drinking | ||||||||
| NO | 441(50.92) | 217(50.47) | 0.051 | 0.975 | 139(50.36) | 128(53.78) | 0.599 | 0.741 |
| Less than once a month | 72(8.31) | 35(8.14) | 26(9.42) | 21(8.82) | ||||
| More than once a month | 353(40.76) | 178(41.4) | 111(40.22) | 89(37.39) | ||||
| Eating meals | ||||||||
| ≤2 meals per day | 116(13.39) | 89(20.70) | 11.939 | 0.003 | 29(10.51) | 24(10.08) | 0.233 | 0.890 |
| 3 meals per day | 735(84.87) | 332(77.21) | 245(88.77) | 213(89.50) | ||||
| ≥4 meals per day | 15(1.73) | 9(2.09) | 2(0.72) | 1(0.42) | ||||
| Taking activities | ||||||||
| No | 477(55.08) | 235(54.65) | 0.021 | 0.884 | 120(43.48) | 117(49.16) | 1.334 | 0.248 |
| Yes | 389(44.92) | 195(45.35) | 156(56.52) | 121(50.84) | ||||
| Ever been in major accidental injury | ||||||||
| No | 760(87.76) | 389(90.47) | 2.091 | 0.148 | 243(88.04) | 217(91.18) | 1.741 | 0.187 |
| Yes | 106(12.24) | 41(9.53) | 33(11.96) | 21(8.82) | ||||
| Having regular physical exercises | ||||||||
| No physical exercise | 563(65.01) | 260(60.47) | 2.957 | 0.228 | 170(61.59) | 146(61.34) | 1.743 | 0.418 |
| Less than regular physical exercises | 139(16.05) | 83(19.30) | 49(17.75) | 34(14.29) | ||||
| Regular physical exercises | 164(18.94) | 87(20.23) | 57(20.65) | 58(24.37) | ||||
| History of CVD | ||||||||
| No | 772(89.15) | 376(87.44) | 0.947 | 0.330 | 222(80.43) | 183(76.89) | 0.760 | 0.383 |
| Yes | 94(10.85) | 54(12.56) | 54(19.57) | 55(23.11) | ||||
| History of liver diseases | ||||||||
| No | 832(96.07) | 417(96.98) | 0.634 | 0.426 | 260(94.20) | 229(96.22) | 1.122 | 0.290 |
| Yes | 34(3.93) | 13(3.02) | 16(5.80) | 9(3.78) | ||||
| Antilipidemic medication | ||||||||
| No | 839(96.88) | 418(97.21) | 0.105 | 0.746 | 253(91.67) | 217(91.18) | 0.039 | 0.843 |
| Yes | 27(3.12) | 12(2.79) | 23(8.33) | 21(8.82) | ||||
| Anti-diabetic medication | ||||||||
| No | 841(97.11) | 423(98.37) | 1.891 | 0.169 | 252(91.30) | 217(91.18) | 0.003 | 0.959 |
| Yes | 25(2.89) | 7(1.63) | 24(8.70) | 21(8.82) | ||||
| Anti-hypertensive therapy | ||||||||
| No | 866(100.00) | 356(82.79) | 154.880 | <0.001 | 276(100.00) | 197(82.77) | 49.347 | <0.001 |
| Yes | 0(0.00) | 74(17.21) | 0(0.00) | 41(17.23) | ||||
| Fasting plasma glucose(mg/dl) | 106.7±33.3 | 112.26±38.38 | -2.678 | 0.007 | 116.83±37.59 | 120.62±45.51 | -1.029 | 0.304 |
| LDL Cholesterol (mg/dl) | 108.4±32.03 | 112.4±33.07 | -2.089 | 0.037 | 117.46±34.23 | 119.22±35.95 | -0.565 | 0.572 |
| HDL Cholesterol (mg/dl) | 54.94±16.53 | 54.59±15.34 | 0.364 | 0.716 | 44.02±12.93 | 43.18±13.00 | 0.735 | 0.463 |
| eGFR(ml/min/1.73m2) | 75.95±15.97 | 71.69±17.21 | 4.396 | <0.001 | 77.54±16.00 | 73.21±16.46 | 3.011 | 0.003 |
| Serum uric acid(mg/dl) | 4.83±1.25 | 5.15±1.38 | -4.246 | <0.001 | 5.22±1.32 | 5.49±1.31 | -2.278 | 0.023 |
| Systolic blood pressure(mmHg) | 119.36±12.22 | 157.19±21.46 | -25.143 | <0.001 | 124.62±10.54 | 158.37±23.28 | -15.737 | <0.001 |
| Diastolic blood pressure(mmHg) | 69.02±9.26 | 84.54±12.44 | -40.141 | <0.001 | 72.72±8.41 | 86.95±11.89 | -21.480 | <0.001 |
| Body mass index(kg/m2) | 20.53±2.05 | 20.84±2.04 | -2.604 | 0.009 | 26.80±3.76 | 26.88±2.08 | -0.280 | 0.780 |
| Triglycerides (mg/dl) | 95.95±54.77 | 104.34±59.81 | -2.510 | 0.012 | 147.99±135.77 | 147.86±104.59 | 0.012 | 0.990 |
Table 4.
Characteristics of participants categorized by BMI and blood pressure status in female (N=1819).
| Variables | BMI24(n=1080) | t/χ2 | P | BMI≥24 (n=739) | t/χ2 | P | ||
|---|---|---|---|---|---|---|---|---|
| Normotension (n=660) |
Hypertension (n=420) |
Normotension (n=362) |
Hypertension (n=377) |
|||||
| Age(years) | 67.87±6.60 | 71.12±7.30 | -7.518 | <0.001 | 66.27±5.54 | 68.71±6.70 | -5.352 | <0.001 |
| Education | ||||||||
| Illiterate | 385(58.33) | 278(66.19) | 7.660 | 0.054 | 168(46.41) | 212(56.23) | 11.887 | 0.008 |
| Less than elementary school | 260(39.39) | 137(32.62) | 178(49.17) | 155(41.11) | ||||
| High school | 5(0.76) | 1(0.24) | 8(2.21) | 1(0.27) | ||||
| Above vocational school | 10(1.52) | 4(0.95) | 8(2.21) | 9(2.39) | ||||
| Marital status | ||||||||
| Single | 189(28.64) | 174(41.43) | 18.823 | <0.001 | 82(22.65) | 98(25.99) | 1.120 | 0.290 |
| Married | 471(71.36) | 246(58.57) | 280(77.35) | 279(74.01) | ||||
| Current residence | ||||||||
| Rural | 450(68.18) | 288(68.57) | 0.018 | 0.893 | 207(57.18) | 209(55.44) | 0.228 | 0.633 |
| Urban | 210(31.82) | 132(31.43) | 155(42.82) | 168(44.56) | ||||
| Smoke | ||||||||
| NO | 574(86.97) | 360(85.71) | 0.444 | 0.801 | 330(91.16) | 339(89.92) | 0.925 | 0.630 |
| Former smoke | 22(3.33) | 14(3.33) | 9(2.49) | 14(3.71) | ||||
| Current smoke | 64(9.70) | 46(10.95) | 23(6.35) | 24(6.37) | ||||
| Drinking | ||||||||
| NO | 575(87.12) | 370(88.10) | 1.172 | 0.556 | 318(87.85) | 338(89.66) | 1.871 | 0.392 |
| Less than once a month | 29(4.39) | 13(3.10) | 20(5.52) | 13(3.45) | ||||
| More than once a month | 56(8.48) | 37(8.81) | 24(6.63) | 26(6.90) | ||||
| Eating meals | ||||||||
| ≤2 meals per day | 112(16.97) | 79(18.81) | 0.599 | 0.741 | 40(11.05) | 36(9.55) | 0.611 | 0.737 |
| 3 meals per day | 537(81.36) | 334(79.52) | 316(87.29) | 336(89.12) | ||||
| ≥4 meals per day | 11(1.67) | 7(1.67) | 6(1.66) | 5(1.33) | ||||
| Taking activities | ||||||||
| No | 366(55.45) | 237(56.43) | 0.099 | 0.753 | 171(47.24) | 170(45.09) | 0.342 | 0.559 |
| Yes | 294(44.55) | 183(43.57) | 191(52.76) | 207(54.91) | ||||
| Ever been in major accidental injury | ||||||||
| No | 610(92.42) | 393(93.57) | 0.510 | 0.475 | 333(91.99) | 354(93.90) | 1.030 | 0.310 |
| Yes | 50(7.58) | 27(6.43) | 29(8.01) | 23(6.10) | ||||
| Having regular physical exercises | ||||||||
| No physical exercise | 417(63.18) | 286(68.10) | 4.349 | 0.114 | 223(61.60) | 231(61.27) | 0.840 | 0.657 |
| Less than regular physical exercises | 133(20.15) | 64(15.24) | 62(17.13) | 73(19.36) | ||||
| Regular physical exercises | 110(16.67) | 70(16.67) | 77(21.27) | 73(19.36) | ||||
| History of CVD | ||||||||
| No | 561(85.00) | 356(84.76) | <0.001 | 0.985 | 293(80.94) | 293(77.72) | 0.979 | 0.322 |
| Yes | 99(15.00) | 64(15.24) | 69(19.06) | 84(22.28) | ||||
| History of liver diseases | ||||||||
| No | 640(96.97) | 407(96.90) | 0.004 | 0.952 | 342(94.48) | 365(96.82) | 1.912 | 0.167 |
| Yes | 20(3.03) | 13(3.10) | 20(5.52) | 12(3.18) | ||||
| Antilipidemic medication | ||||||||
| No | 641(97.12) | 398(94.76) | 3.912 | 0.048 | 329(90.88) | 323(85.68) | 4.822 | 0.028 |
| Yes | 19(2.88) | 22(5.24) | 33(9.12) | 54(14.32) | ||||
| Anti-diabetic medication | ||||||||
| No | 644(97.58) | 406(96.67) | 0.785 | 0.375 | 343(94.75) | 335(88.86) | 8.466 | 0.004 |
| Yes | 16(2.42) | 14(3.33) | 19(5.25) | 42(11.14) | ||||
| Anti-hypertensive therapy | ||||||||
| No | 660(100.00) | 349(83.10) | 116.690 | <0.001 | 362(100.00) | 324(85.94) | 52.732 | <0.001 |
| Yes | 0(0.00) | 71(16.90) | 0(0.00) | 53(14.06) | ||||
| Fasting plasma glucose(mg/dl) | 107.94±38.43 | 112.33±38.69 | -1.816 | 0.070 | 111.30±31.47 | 123.61±54.14 | -3.727 | <0.001 |
| LDL Cholesterol (mg/dl) | 121.38±33.16 | 121.89±36.31 | -0.235 | 0.814 | 126.38±37.50 | 129.47±41.91 | -1.046 | 0.296 |
| HDL Cholesterol (mg/dl) | 56.09±15.43 | 54.71±15.29 | 1.429 | 0.153 | 47.60±12.33 | 46.48±13.09 | 1.183 | 0.237 |
| eGFR(ml/min/1.73m2) | 77.62±15.26 | 72.13±17.03 | 5.486 | <0.001 | 78.07±15.97 | 75.73±16.73 | 1.935 | 0.053 |
| Serum uric acid(mg/dl) | 3.92±1.10 | 4.17±1.16 | -3.510 | <0.001 | 4.30±1.12 | 4.46±1.21 | -1.950 | 0.052 |
| Systolic blood pressure(mmHg) | 120.81±12.07 | 159.88±17.31 | -20.347 | <0.001 | 123.15±10.88 | 161.97±35.55 | -17.786 | <0.001 |
| Diastolic blood pressure(mmHg) | 69.57±8.82 | 82.44±11.75 | -43.348 | <0.001 | 71.98±8.39 | 85.32±11.53 | -19.691 | <0.001 |
| Body mass index(kg/m2) | 20.6±2.20 | 20.85±2.19 | -1.796 | 0.073 | 26.97±2.92 | 27.43±3.84 | -1.810 | 0.071 |
| Triglycerides (mg/dl) | 119.69±73.83 | 130.67±83.99 | -2.243 | 0.025 | 150.58±87.77 | 174.89±122.44 | -3.067 | 0.002 |
Table 5 shows the various characteristics of participants categorized by age. SUA and SBP levels were significantly higher in the older age group than in the younger age group in men, whereas levels of HDL-C, eGFR, DBP, BMI, and TG were lower in the older age group than in the younger age group. However, between-group differences in categories of current residence, eating habits, taking activities, major accidental injury, regular physical exercise, history of liver disease, antidiabetic medication, antihypertensive therapy, FPG, and LDL-C were not observed. In women, SUA and SBP levels were significantly higher in the older age group than in the younger age group, but eGFR and BMI levels were lower in the older age group than in the younger age group. However, between-group differences in categories of current residence, drinking, eating habits, activity, major accidental injury, history of CVD, history of liver disease, antidiabetic medication, and antihypertensive therapy, FPG, LDL-C, HDL-C, DBP, and TG were not observed.
Table 5.
Characteristics of participants categorized by age in male and female (N=3629).
| Male(n=1810) | Female(n=1819) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Age <68 years (n=807) | Age≥68 years (n=1003) | t/χ2 | P | Age <68 years (n=887) | Age≥68 years (n=932) | t/χ2 | P |
| Education | ||||||||
| Illiterate | 94(11.65) | 278(27.72) | 73.763 | <0.001 | 409(46.11) | 634(68.03) | 94.734 | <0.001 |
| Less than elementary school | 652(80.79) | 647(64.51) | 457(51.52) | 273(29.29) | ||||
| High school | 16(1.98) | 16(1.60) | 8(0.90) | 7(0.75) | ||||
| Above vocational school | 45(5.58) | 62(6.18) | 13(1.47) | 18(1.93) | ||||
| Marital status | ||||||||
| Single | 69(8.55) | 182(18.15) | 34.471 | <0.001 | 138(15.56) | 405(43.45) | 168.901 | <0.001 |
| Married | 738(91.45) | 821(81.85) | 749(84.44) | 527(56.55) | ||||
| Current residence | ||||||||
| Rural | 538(66.67) | 683(68.10) | 0.416 | 0.519 | 580(65.39) | 574(61.59) | 2.831 | 0.092 |
| Urban | 269(33.33) | 320(31.90) | 307(34.61) | 358(38.41) | ||||
| Smoke | ||||||||
| NO | 201(24.91) | 275(27.42) | 10.454 | 0.005 | 791(89.18) | 812(87.12) | 13.584 | 0.001 |
| Former smoke | 145(17.97) | 228(22.73) | 15(1.69) | 44(4.72) | ||||
| Current smoke | 461(57.13) | 500(49.85) | 81(9.13) | 76(8.15) | ||||
| Drinking | ||||||||
| NO | 366(45.35) | 559(55.73) | 19.444 | <0.001 | 777(87.6) | 824(88.41) | 1.095 | 0.578 |
| Less than once a month | 79(9.79) | 75(7.48) | 41(4.62) | 34(3.65) | ||||
| More than once a month | 362(44.86) | 369(36.79) | 69(7.78) | 74(7.94) | ||||
| Eating meals | ||||||||
| ≤2 meals per day | 107(13.26) | 151(15.05) | 1.687 | 0.430 | 119(13.42) | 148(15.88) | 2.586 | 0.275 |
| 3 meals per day | 686(85.01) | 839(83.65) | 752(84.78) | 771(82.73) | ||||
| ≥4 meals per day | 14(1.73) | 13(1.3) | 16(1.8) | 13(1.39) | ||||
| Taking activities | ||||||||
| No | 412(51.05) | 537(53.54) | 1.108 | 0.292 | 448(50.51) | 496(53.22) | 1.339 | 0.247 |
| Yes | 395(48.95) | 466(46.46) | 439(49.49) | 436(46.78) | ||||
| Ever been in major accidental injury | ||||||||
| No | 723(89.59) | 886(88.33) | 0.715 | 0.398 | 825(93.01) | 865(92.81) | 0.027 | 0.869 |
| Yes | 84(10.41) | 117(11.67) | 62(6.99) | 67(7.19) | ||||
| Having regular physical exercises | ||||||||
| No physical exercise | 509(63.07) | 630(62.81) | 3.842 | 0.146 | 530(59.75) | 627(67.27) | 11.203 | 0.004 |
| Less than regular physical exercises | 148(18.34) | 157(15.65) | 181(20.41) | 151(16.2) | ||||
| Regular physical exercises | 150(18.59) | 216(21.54) | 176(19.84) | 154(16.52) | ||||
| History of CVD | ||||||||
| No | 712(88.23) | 841(83.85) | 6.902 | 0.009 | 741(83.54) | 762(81.76) | 0.977 | 0.323 |
| Yes | 95(11.77) | 162(16.15) | 146(16.46) | 170(18.24) | ||||
| History of liver diseases | ||||||||
| No | 769(95.29) | 969(96.61) | 2.154 | 0.142 | 858(96.73) | 896(96.14) | 0.450 | 0.503 |
| Yes | 38(4.71) | 34(3.39) | 29(3.27) | 36(3.86) | ||||
| Antilipidemic medication | ||||||||
| No | 759(94.05) | 968(96.51) | 6.177 | 0.013 | 811(91.43) | 880(94.42) | 6.206 | 0.013 |
| Yes | 48(5.95) | 35(3.49) | 76(8.57) | 52(5.58) | ||||
| Anti-diabetic medication | ||||||||
| No | 769(95.29) | 964(96.11) | 0.739 | 0.390 | 838(94.48) | 890(95.49) | 0.911 | 0.320 |
| Yes | 38(4.71) | 39(3.89) | 49(5.52) | 42(4.51) | ||||
| Anti-hypertensive therapy | ||||||||
| No | 755(93.56) | 940(93.72) | 0.002 | 0.888 | 823(92.78) | 872(93.56) | 0.433 | 0.511 |
| Yes | 52(6.44) | 63(6.28) | 64(7.22) | 60(6.44) | ||||
| Fasting plasma glucose(mg/dl) | 113.22±40.77 | 109.94±34.06 | 1.864 | 0.062 | 112.89±44.91 | 113.09±38.18 | -0.104 | 0.917 |
| LDL Cholesterol (mg/dl) | 113.49±35.56 | 111.15±31.42 | 1.489 | 0.137 | 123.2±36.32 | 125.00±37.35 | -1.041 | 0.298 |
| HDL Cholesterol (mg/dl) | 50.53±15.8 | 52.53±16.25 | 2.633 | 0.009 | 51.62±14.61 | 52.5±15.33 | -1.252 | 0.211 |
| eGFR(ml/min/1.73m2) | 81.50±14.52 | 69.24±15.88 | 16.964 | <0.001 | 82.21±14.6 | 69.97±15.68 | 17.211 | <0.001 |
| Serum uric acid(mg/dl) | 4.97±1.28 | 5.14±1.35 | -2.682 | 0.007 | 4.08±1.13 | 4.26±1.19 | -3.350 | 0.001 |
| Systolic blood pressure(mmHg) | 132±21.28 | 136.32±26.41 | -3.748 | <0.001 | 134.43±25.74 | 143.46±29.58 | -6.885 | <0.001 |
| Diastolic blood pressure(mmHg) | 77.38±12.52 | 74.33±12.96 | 5.036 | <0.001 | 76.83±12.3 | 75.95±11.98 | 1.534 | 0.252 |
| Body mass index(kg/m2) | 23.06±3.61 | 21.88±3.70 | 6.853 | <0.001 | 23.78±3.86 | 22.90±4.51 | 4.428 | <0.001 |
| Triglycerides (mg/dl) | 121.17±99.74 | 106.04±67.08 | 3.843 | <0.001 | 142.91±90.84 | 137.51±97.13 | 1.223 | 0.222 |
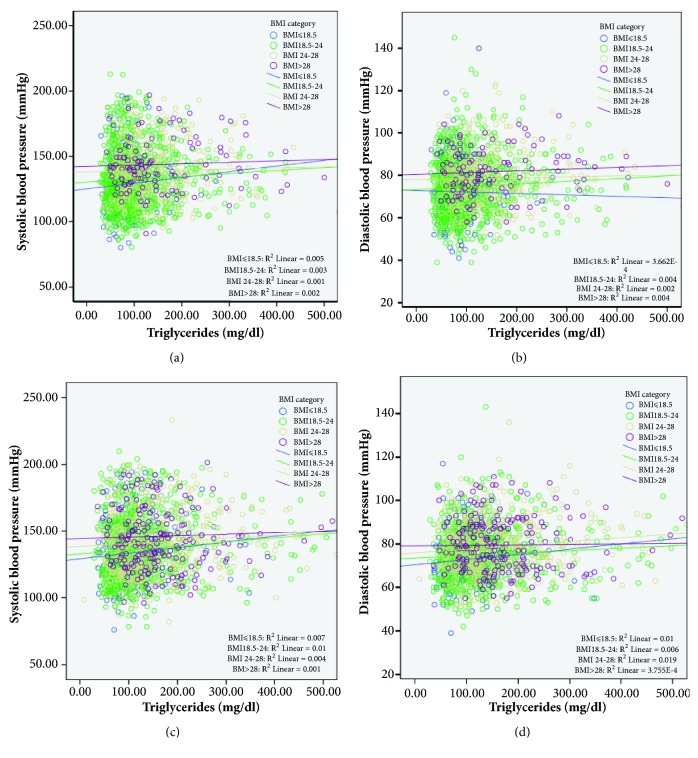
In addition to their direct associations, we observed the effect between BMI category and TG levels on BP in Figure 1. TG correlated positively with both SBP and DBP. Analysis of covariance showed that three regression lines in each graph were not different from those in the other groups (male: SBP, F=0.028, P=0.867 and DBP, F= 0.194, and P =0.660; female: SBP, F=0.783, P=0.376 and DBP, F=0.005, and P =0.941; respectively).
Figure 1.
(a, b) Correlation between serum uric acid and blood pressure status of participants categorized by body mass index in male. (c, d) Correlation between triglycerides and blood pressure status of participants categorized by body mass index in female.
Tables 6 and 7 show the relationship between various characteristics and BP status of participants categorized by BMI (< 24.0 kg/m2 and ≥ 24.0 kg/m2). Age-adjusted partial Pearson's correlation coefficient showed that TG level was positively correlated with both SBP and DBP in men with a BMI < 21.0 kg/m2 (Table 6). In women, the TG level was significantly correlated with SBP and DBP in subjects with a BMI < 21.0 kg/m2 and positively correlated with DBP in those with a BMI ≥ 24.0 kg/m2, but there was no correlation with SBP in women with a BMI ≥ 24.0 kg/m2 (Table 7).
Table 6.
Age-adjusted relationship between various characteristics and blood pressure status of participants categorized by BMI in male (N=1810).
| Variables | BMI<24(n=1296) | BMI≥24 (n=514) | ||
|---|---|---|---|---|
| Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
|
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | -0.024(0.392) | 0.013(0.647) | -0.009(0.848) | -0.042(0.344) |
| Marital status(0= Single,1= Married) | -0.105(<0.001) | -0.092(0.001) | 0.011(0.807) | -0.011(0.798) |
| Current residence(0= Rural,1= Urban) | 0.044(0.117) | 0.032(0.249) | 0.113(0.011) | 0.059(0.187) |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | 0.06(0.033) | 0.009(0.752) | 0.066(0.140) | 0.016(0.727) |
| Drinking(0= NO,1= Less than once a month,2= More than once a month) | 0.015(0.602) | 0.020(0.480) | -0.066(0.139) | -0.003(0.944) |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.061(0.031) | -0.083(0.003) | -0.014(0.759) | -0.056(0.21) |
| Taking activities(0= No,1= Yes) | 0.014(0.623) | 0.031(0.268) | 0.091(0.040) | 0.118(0.008) |
| Ever been in major accidental injury(0= No,1= Yes) | -0.028(0.320) | -0.019(0.505) | -0.035(0.429) | -0.007(0.871) |
| Having regular physical exercises(0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | 0.034(0.23) | 0.006(0.833) | 0.011(0.803) | 0.011(0.814) |
| History of CVD(0= No,1= Yes) | 0.019(0.497) | 0.028(0.327) | -0.009(0.833) | 0.008(0.854) |
| History of liver diseases(0= No,1= Yes) | 0.009(0.760) | 0.013(0.631) | -0.023(0.613) | 0.028(0.526) |
| Antilipidemic medication(0= No,1= Yes) | -0.008(0.787) | 0.019(0.504) | 0.002(0.973) | 0.027(0.546) |
| Anti-diabetic medication(0= No,1= Yes) | 0.002(0.955) | 0.007(0.806) | 0.043(0.339) | -0.012(0.796) |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.140(<0.001) | 0.109(<0.001) | 0.047(0.291) | 0.127(0.004) |
| Fasting plasma glucose(mg/dl) | 0.075(0.007) | 0.046(0.098) | 0.068(0.126) | 0.065(0.147) |
| LDL Cholesterol (mg/dl) | 0.063(0.024) | 0.052(0.067) | 0.063(0.157) | 0.024(0.585) |
| HDL Cholesterol (mg/dl) | -0.005(0.848) | 0.005(0.870) | -0.042(0.344) | -0.003(0.942) |
| eGFR(ml/min/1.73m2) | -0.076(0.007) | -0.043(0.124) | -0.157(<0.001) | -0.107(0.016) |
| Serum uric acid(mg/dl) | 0.108(<0.001) | 0.06(0.032) | 0.056(0.212) | 0.067(0.130) |
| Body mass index(kg/m2) | 0.121(<0.001) | 0.093(0.001) | 0.062(0.163) | 0.048(0.279) |
| Triglycerides (mg/dl) | 0.069(0.014) | 0.058(0.04) | 0.074(0.097) | 0.047(0.288) |
Table 7.
Age-adjusted relationship between various characteristics and blood pressure status of participants categorized by BMI in female (N=1819).
| Variables | BMI<24 (n=1080) | BMI≥24 (n=739) | ||
|---|---|---|---|---|
| Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
|
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | -0.053(0.086) | -0.07(0.024) | -0.002(0.957) | -0.041(0.270) |
| Marital status(0= Single,1= Married) | -0.097(0.002) | -0.077(0.012) | -0.066(0.076) | -0.015(0.687) |
| Current residence(0= Rural,1= Urban) | -0.01(0.745) | -0.039(0.211) | 0.039(0.294) | 0.035(0.344) |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | 0.035(0.255) | 0.021(0.503) | -0.025(0.508) | 0.007(0.844) |
| Drinking(0= NO,1= Less than once a month,2= More than once a month) | -0.016(0.608) | 0.015(0.630) | -0.022(0.549) | -0.02(0.584) |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.021(0.505) | -0.075(0.015) | -0.026(0.483) | -0.069(0.064) |
| Taking activities(0= No,1= Yes) | -0.036(0.251) | -0.034(0.266) | 0.027(0.474) | 0.027(0.472) |
| Ever been in major accidental injury(0= No,1= Yes) | -0.01(0.745) | 0.014(0.640) | -0.041(0.274) | -0.042(0.259) |
| Having regular physical exercises(0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | -0.008(0.799) | -0.008(0.803) | -0.015(0.692) | 0.031(0.401) |
| History of CVD(0= No,1= Yes) | 0.036(0.239) | 0.001(0.986) | -0.014(0.700) | -0.021(0.582) |
| History of liver diseases(0= No,1= Yes) | 0.005(0.868) | 0.003(0.934) | -0.047(0.213) | -0.103(0.006) |
| Antilipidemic medication(0= No,1= Yes) | 0.065(0.034) | 0.054(0.082) | 0.054(0.151) | 0.032(0.399) |
| Anti-diabetic medication(0= No,1= Yes) | 0.013(0.686) | -0.029(0.356) | 0.122(0.001) | 0.046(0.214) |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.110(<0.001) | 0.037(0.029) | 0.128(<0.001) | 0.102(<0.001) |
| Fasting plasma glucose(mg/dl) | 0.049(0.115) | 0.043(0.161) | 0.021(0.577) | 0.158(<0.001) |
| LDL Cholesterol (mg/dl) | 0.028(0.362) | 0.011(0.725) | 0.049(0.189) | -0.005(0.886) |
| HDL Cholesterol (mg/dl) | -0.087(0.005) | -0.06(0.051) | -0.039(0.293) | -0.050(0.184) |
| eGFR(ml/min/1.73m2) | -0.069(0.025) | -0.045(0.147) | 0.067(0.075) | 0.020(0.600) |
| Serum uric acid(mg/dl) | 0.126(<0.001) | 0.074(0.016) | -0.018(0.627) | 0.011(0.764) |
| Body mass index(kg/m2) | 0.105(0.001) | 0.093(0.002) | 0.021(0.583) | 0.075(0.045) |
| Triglycerides (mg/dl) | 0.123(<0.001) | 0.091(0.003) | 0.046(0.218) | 0.097(0.010) |
Tables 8 and 9 show the relationship between various characteristics and BP status of participants categorized by age (< 68 years and ≥ 68 years). TG level was positively correlated with both SBP and DBP in both men and women with age < 68 years and ≥ 68 years.
Table 8.
Relationship between various characteristics and blood pressure status of participants categorized by age in male (N=1810).
| Variables | Age <68 years (n=807) |
Age≥68 years (n=1003) |
||
|---|---|---|---|---|
| Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
|
| Age | 0.052(0.146) | -0.011(0.763) | 0.05(0.116) | -0.096(0.002) |
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | 0.013(0.720) | -0.016(0.646) | -0.019(0.544) | 0.043(0.173) |
| Marital status(0= Single,1= Married) | -0.064(0.070) | -0.086(0.015) | -0.074(0.020) | -0.033(0.295) |
| Current residence(0= Rural,1= Urban) | 0.072(0.042) | 0.039(0.274) | 0.102(0.001) | 0.096(0.003) |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | 0.018(0.616) | 0.017(0.633) | 0.042(0.184) | -0.023(0.462) |
| Drinking(0= NO,1= Less than once a month,2= More than once a month) | -0.028(0.425) | -0.015(0.679) | -0.006(0.856) | 0.037(0.244) |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.065(0.067) | -0.098(0.006) | -0.026(0.420) | -0.050(0.114) |
| Taking activities(0= No,1= Yes) | -0.036(0.315) | -0.040(0.255) | 0.022(0.495) | 0.042(0.189) |
| Ever been in major accidental injury(0= No,1= Yes) | -0.044(0.212) | -0.053(0.137) | -0.026(0.416) | -0.001(0.975) |
| Having regular physical exercises(0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | -0.001(0.987) | -0.005(0.89) | 0.046(0.147) | 0.022(0.489) |
| History of CVD(0= No,1= Yes) | 0.055(0.123) | 0.06(0.089) | 0.009(0.786) | 0.027(0.396) |
| History of liver diseases(0= No,1= Yes) | -0.033(0.357) | -0.019(0.598) | 0.024(0.448) | 0.056(0.078) |
| Antilipidemic medication(0= No,1= Yes) | 0.060(0.092) | 0.06(0.088) | -0.018(0.561) | 0.021(0.502) |
| Anti-diabetic medication(0= No,1= Yes) | 0.038(0.281) | -0.002(0.945) | 0.041(0.198) | 0.045(0.157) |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.131(<0.001) | 0.122(0.001) | 0.103(0.001) | 0.118(<0.001) |
| Fasting plasma glucose(mg/dl) | 0.122(0.001) | 0.092(0.009) | 0.069(0.031) | 0.048(0.131) |
| LDL Cholesterol (mg/dl) | 0.096(0.007) | 0.067(0.056) | 0.061(0.054) | 0.054(0.087) |
| HDL Cholesterol (mg/dl) | -0.102(0.004) | -0.077(0.028) | -0.049(0.122) | -0.026(0.405) |
| eGFR(ml/min/1.73m2) | -0.119(0.001) | -0.084(0.017) | -0.117(<0.001) | -0.016(0.618) |
| Serum uric acid(mg/dl) | 0.143(<0.001) | 0.122(0.001) | 0.104(0.001) | 0.049(0.123) |
| Body mass index(kg/m2) | 0.252(<0.001) | 0.218(<0.001) | 0.146(<0.001) | 0.140(<0.001) |
| Triglycerides (mg/dl) | 0.091(0.010) | 0.091(0.010) | 0.105(0.001) | 0.083(0.009) |
Table 9.
Relationship between various characteristics and blood pressure status of participants categorized by age in female (N=1819).
| Variables | Age <68 years (n=887) |
Age≥68 years (n=932) |
||
|---|---|---|---|---|
| Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
Systolic blood pressure partial r(P-value) |
Diastolic blood pressure partial r(P-value) |
|
| Age | 0.067(0.048) | -0.032(0.348) | 0.117(<0.001) | -0.039(0.244) |
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | -0.033(0.335) | -0.020(0.546) | -0.034(0.308) | -0.051(0.124) |
| Marital status(0= Single,1= Married) | -0.073(0.031) | -0.028(0.409) | -0.104(0.002) | -0.035(0.292) |
| Current residence(0= Rural,1= Urban) | 0.034(0.320) | 0.028(0.410) | 0.021(0.536) | -0.007(0.822) |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | 0.043(0.203) | 0.024(0.481) | -0.040(0.230) | -0.024(0.471) |
| Drinking(0= NO,1= Less than once a month,2= More than once a month) | -0.017(0.605) | -0.008(0.818) | -0.028(0.391) | 0.001(0.970) |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.053(0.118) | -0.07(0.039) | 0.013(0.700) | -0.041(0.221) |
| Taking activities(0= No,1= Yes) | 0.022(0.509) | 0.053(0.115) | -0.002(0.956) | -0.049(0.142) |
| Ever been in major accidental injury(0= No,1= Yes) | -0.018(0.589) | 0.012(0.719) | -0.034(0.300) | -0.032(0.330) |
| Having regular physical exercises(0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | -0.016(0.638) | 0.025(0.460) | -0.011(0.735) | 0.007(0.834) |
| History of CVD(0= No,1= Yes) | 0.079(0.020) | 0.074(0.028) | -0.032(0.332) | -0.057(0.084) |
| History of liver diseases(0= No,1= Yes) | 0.019(0.574) | 0.011(0.746) | -0.054(0.104) | -0.088(0.008) |
| Antilipidemic medication(0= No,1= Yes) | 0.095(0.005) | 0.075(0.027) | 0.058(0.081) | 0.046(0.161) |
| Anti-diabetic medication(0= No,1= Yes) | 0.125(<0.001) | 0.061(0.069) | 0.057(0.087) | -0.004(0.896) |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.096(0.004) | 0.060(0.073) | 0.135(<0.001) | 0.076(0.022) |
| Fasting plasma glucose(mg/dl) | 0.061(0.072) | 0.159(<0.001) | 0.031(0.344) | 0.055(0.097) |
| LDL Cholesterol (mg/dl) | 0.048(0.157) | 0.028(0.404) | 0.05(0.132) | 0.014(0.668) |
| HDL Cholesterol (mg/dl) | -0.137(<0.001) | -0.118(<0.001) | -0.063(0.058) | -0.085(0.010) |
| eGFR(ml/min/1.73m2) | -0.039(0.248) | -0.007(0.836) | -0.025(0.455) | -0.011(0.743) |
| Serum uric acid(mg/dl) | 0.084(0.012) | 0.083(0.013) | 0.092(0.005) | 0.054(0.100) |
| Body mass index(kg/m2) | 0.161(<0.001) | 0.253(<0.001) | 0.116(<0.001) | 0.116(<0.001) |
| Triglycerides (mg/dl) | 0.155(<0.001) | 0.148(<0.001) | 0.069(0.037) | 0.096(0.004) |
Tables 10 and 11 show the multivariate-adjusted relationship between various characteristics and BP status in participants categorized by BMI (< 24.0 kg/m2 and ≥ 24.0 kg/m2). Multiple linear regression analysis showed that TG level was significantly and positively associated with SBP in women with a BMI < 24.0 kg/m2, independent of other confounding factors; however, TG level was not significantly associated with BP in men.
Table 10.
Multivariate-adjusted relationship between various characteristics and blood pressure status of participants categorized by BMI in male (N=1810).
| Variables | BMI<24(n=1296) | BMI≥24 (n=514) | ||
|---|---|---|---|---|
| Systolic blood pressure β(P-value) |
Diastolic blood pressure β (P-value) |
Systolic blood pressure β (P-value) |
Diastolic blood pressure β (P-value) |
|
| Age (years) | 0.117(<0.001) | -0.108(0.001) | — | -0.199(<0.001) |
| Education (0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | — | — | — |
| Marital status (0= Single,1= Married) | -0.101(<0.001) | -0.092(0.001) | — | — |
| Current residence (0= Rural,1= Urban) | — | — | 0.119(0.009) | — |
| Smoke (0= NO,1= Former smoke,2= Current smoke) | 0.060(0.033) | — | 0.104(0.023) | — |
| Drinking (0= NO,1= Less than once a month,2= More than once a month) | — | — | — | — |
| Eating meals (0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.056(0.041) | -0.085(0.002) | — | — |
| Taking activities (0= No,1= Yes) | — | — | -0.108(0.016) | -0.116(0.01) |
| Ever been in major accidental injury (0= No,1= Yes) | — | — | — | — |
| Having regular physical exercises (0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | — | — | — | — |
| History of CVD (0= No,1= Yes) | — | — | — | — |
| History of liver diseases (0= No,1= Yes) | — | — | — | — |
| Antilipidemic medication (0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication (0= No,1= Yes) | — | — | — | — |
| Anti-hypertensive therapy (0= No,1= Yes) | 0.130(<0.001) | 0.103(<0.001) | — | 0.113(0.011) |
| Fasting plasma glucose (mg/dl) | 0.072(0.016) | — | — | — |
| LDL Cholesterol (mg/dl) | 0.056(0.042) | — | 0.091(0.048) | — |
| HDL Cholesterol (mg/dl) | — | — | — | — |
| eGFR (ml/min/1.73m2) | — | — | -0.172(0.002) | — |
| Serum uric acid (mg/dl) | 0.068(0.029) | — | — | — |
| Body mass index (kg/m2) | 0.106(<0.001) | 0.076(0.009) | — | — |
| Triglycerides (mg/dl) | — | — | — | — |
| R2 | 0.098(<0.001) | 0.054(<0.001) | 0.087(0.003) | 0.089(0.0002) |
Table 11.
Multivariate-adjusted relationship between various characteristics and blood pressure status of participants categorized by BMI in female (N=1819).
| Variables | BMI<24(n=1080) | BMI≥24 (n=739) | ||
|---|---|---|---|---|
| Systolic blood pressure β(P-value) |
Diastolic blood pressure β (P-value) |
Systolic blood pressure β (P-value) |
Diastolic blood pressure β (P-value) |
|
| Age (years) | 0.168(<0.001) | — | 0.191(<0.001) | 0.191(<0.001) |
| Education (0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | -0.072(0.030) | — | — |
| Marital status (0= Single,1= Married) | -0.106(0.001) | -0.084(0.013) | -0.082(0.034) | -0.082(0.034) |
| Current residence (0= Rural,1= Urban) | — | — | — | — |
| Smoke (0= NO,1= Former smoke,2= Current smoke) | — | — | — | — |
| Drinking (0= NO,1= Less than once a month,2= More than once a month) | — | — | — | — |
| Eating meals (0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | — | -0.075(0.016) | — | — |
| Taking activities (0= No,1= Yes) | — | — | — | — |
| Ever been in major accidental injury (0= No,1= Yes) | — | — | — | — |
| Having regular physical exercises (0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | — | — | — | — |
| History of CVD (0= No,1= Yes) | — | — | — | — |
| History of liver diseases (0= No,1= Yes) | — | — | — | — |
| Antilipidemic medication (0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication (0= No,1= Yes) | — | — | 0.138(0.001) | 0.138(0.001) |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.12(<0.001) | — | 0.129(0.001) | 0.129(0.001) |
| Fasting plasma glucose(mg/dl) | — | — | — | — |
| LDL Cholesterol (mg/dl) | — | — | — | — |
| HDL Cholesterol (mg/dl) | — | — | — | — |
| eGFR(ml/min/1.73m2) | — | — | — | — |
| Serum uric acid(mg/dl) | 0.084(0.016) | — | — | — |
| Body mass index(kg/m2) | 0.082(0.009) | 0.086(0.008) | — | — |
| Triglycerides (mg/dl) | 0.078(0.025) | — | — | — |
| R2 | 0.119(<0.001) | 0.046(0.001) | 0.089(<0.001) | 0.072(<0.001) |
Tables 12 and 13 show the multivariate-adjusted relationship between various characteristics and BP status in participants categorized by age (< 68 years and ≥ 68 years). Multiple linear regression analysis showed that TG level was significantly and positively associated with SBP in women with age of < 68 years, independent of other confounding factors. In contrast, TG level was significantly associated with SBP in men with age of ≥ 68 years.
Table 12.
Multivariate-adjusted relationship between various characteristics and blood pressure status of participants categorized by age in male (N=1810).
| Variables | Age <68 years (n=807) |
Age≥68 years (n=1003) |
||
|---|---|---|---|---|
| Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
|
| Age | — | — | — | -0.085(0.015) |
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | — | — | — |
| Marital status(0= Single,1= Married) | 0.078(0.024) | 0.1(0.004) | 0.074(0.020) | — |
| Current residence(0= Rural,1= Urban) | — | — | 0.105(0.002) | 0.084(0.014) |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | — | — | 0.078(0.016) | — |
| Drinking(0= NO,1= Less than once a month,2= More than once a month) | — | — | — | — |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | -0.070(0.039) | -0.103(0.003) | — | -0.071(0.025) |
| Taking activities(0= No,1= Yes) | -0.077(0.027) | — | — | — |
| Ever been in major accidental injury(0= No,1= Yes) | — | — | — | — |
| Having regular physical exercises(0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | — | — | — | — |
| History of CVD(0= No,1= Yes) | — | — | — | — |
| History of liver diseases(0= No,1= Yes) | — | — | — | — |
| Antilipidemic medication(0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication(0= No,1= Yes) | — | -0.078(0.046) | — | — |
| Anti-hypertensive therapy(0= No,1= Yes) | 0.09(0.009) | 0.090(0.010) | 0.111(<0.001) | 0.114(<0.001) |
| Fasting plasma glucose(mg/dl) | 0.09(0.022) | — | — | — |
| LDL Cholesterol (mg/dl) | — | — | — | — |
| HDL Cholesterol (mg/dl) | — | — | — | — |
| eGFR(ml/min/1.73m2) | -0.078(0.040) | — | — | — |
| Serum uric acid(mg/dl) | 0.088(0.024) | 0.08(0.042) | — | — |
| Body mass index(kg/m2) | 0.229(<0.001) | 0.213(<0.001) | 0.137(<0.001) | 0.105(0.003) |
| Triglycerides (mg/dl) | 0.024(0.545) | 0.03(0.452) | 0.096(0.009) | 0.063(0.088) |
| R2 | 0.136(<0.001) | 0.115(<0.001) | 0.087(<0.001) | 0.065(<0.001) |
Table 13.
Multivariate-adjusted relationship between various characteristics and blood pressure status of participants categorized by age in female (N=1819).
| Variables | Age <68 years (n=887) |
Age≥68 years (n=932) |
||
|---|---|---|---|---|
| Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
|
| Age | — | — | 0.105(0.005) | — |
| Education (0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | — | — | — |
| Marital status (0= Single,1= Married) | 0.071(0.035) | — | 0.103(0.003) | 0.071(0.043) |
| Current residence (0= Rural,1= Urban) | — | — | — | — |
| Smoke (0= NO,1= Former smoke,2= Current smoke) | — | — | — | — |
| Drinking (0= NO,1= Less than once a month,2= More than once a month) | — | — | — | — |
| Eating meals (0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | — | -0.08(0.015) | — | — |
| Taking activities (0= No,1= Yes) | — | — | — | — |
| Ever been in major accidental injury (0= No,1= Yes) | — | — | — | — |
| Having regular physical exercises (0= No physical exercise,1= Less than regular physical exercises,2= Regular physical exercises) | — | — | — | — |
| History of CVD (0= No,1= Yes) | — | — | — | -0.069(0.048) |
| History of liver diseases (0= No,1= Yes) | — | — | — | -0.076(0.023) |
| Antilipidemic medication (0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication (0= No,1= Yes) | 0.105(0.004) | — | — | — |
| Anti-hypertensive therapy (0= No,1= Yes) | 0.085(0.012) | — | 0.153(<0.001) | 0.089(0.008) |
| Fasting plasma glucose (mg/dl) | — | 0.128(<0.001) | — | — |
| LDL Cholesterol (mg/dl) | — | — | — | — |
| HDL Cholesterol (mg/dl) | — | — | — | — |
| eGFR (ml/min/1.73m2) | — | — | — | — |
| Serum uric acid (mg/dl) | — | — | — | — |
| Body mass index (kg/m2) | 0.11(0.003) | 0.23(<0.001) | 0.097(0.007) | 0.105(0.004) |
| Triglycerides (mg/dl) | 0.087(0.031) | 0.056(0.159) | 0.046(0.270) | 0.072(0.090) |
| R2 | 0.087(<0.001) | 0.110(<0.001) | 0.079(<0.001) | 0.057(<0.001) |
Table 14 shows the interaction between BMI and TG level and BP status in men and women. A general linear model with the following confounding factors (age, educational level, marital status, current residence, smoking, eating habits, taking activities, antidiabetic medication, antihypertensive therapy, FPG, LDL-C, eGFR, and SUA) was used to assess the statistical significance of the synergistic relationship between BMI and SUA level. Evidence of interaction between BMI and SUA level on SBP (men, β = 0.572, P = 0.845; women, β = 0.122, and P = 0.923) and DBP (men, β = -0.373, P = 0.810; women, β = 0.272, and P = 0.828) levels was not observed.
Table 14.
Interaction between body mass index and uric acid on blood pressure status in male and female (N=3629).
| Characteristics | Male(n=1810) | Female(n=1819) | ||
|---|---|---|---|---|
| Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
|
| Age(years) | 0.337(0.001) | -0.240(<0.001) | -0.092(0.042) | -0.113(0.013) |
| Education(0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | — | — | -1.119(0.019) |
| Marital status(0= Single,1= Married) | -5.660(0.001) | -2.494(0.004) | -1.503(0.024) | -1.453(0.029) |
| Current residence(0= Rural,1= Urban) | 3.574(0.003) | — | — | — |
| Smoke(0= NO,1= Former smoke,2= Current smoke) | 1.864(0.005) | — | — | — |
| Eating meals(0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | 2.978(0.045) | 2.483(0.002) | — | 2.193(0.003) |
| Taking activities(0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication(0= No,1= Yes) | — | — | — | — |
| Anti-hypertensive therapy(0= No,1= Yes) | 10.228(<0.001) | 5.745(<0.001) | 3.292(0.003) | — |
| Fasting plasma glucose(mg/dl) | 0.039(0.011) | — | — | — |
| LDL Cholesterol (mg/dl) | 0.049(0.004) | — | — | — |
| eGFR(ml/min/1.73m2) | -0.123(0.003) | — | — | — |
| Serum uric acid(mg/dl) | 0.948(0.047) | — | — | — |
| Body mass index | -8.004(0.002) | -4.125(0.002) | -3.668(<0.001) | -4.102(<0.001) |
| Triglycerides | -3.962(0.076) | -1.482(0.203) | -2.140(0.017) | -2.319(0.009) |
| Body mass index∗ Triglycerides | 0.572(0.845) | -0.373(0.810) | 0.122(0.923) | 0.272(0.828) |
Table 15 shows the interaction between BMI and TG on BP status of participants categorized by age in men and women. A general linear model with the following confounding factors (age, educational level, marital status, current residence, smoking, eating habits, activity, physical activity, antilipidemic medication, antidiabetic medication, antihypertensive therapy, FPG, eGFR, and SUA) was used to assess the statistical significance of the synergistic relationship between BMI and SUA level. Evidence of interaction between BMI and SUA level on SBP (men with age of < 68 years, β = -1.075, and P = 0.760; men with age of ≥ 68 years, β = 2.138, and P = 0.654; women with age of < 68 years, β = -1.345, and P = 0.718; women with age of ≥ 68 years, β = -4.192, and P = 0.334) and DBP (men with age of < 68 years, β = -0.095, and P = 0.964; men with age of ≥ 68 years, β = -0.931, and P = 0.691; women with age of < 68 years, β = 2.410, P = 0.170; women with age of ≥ 68 years β = -3.386, and P = 0.439) was not observed.
Table 15.
Interaction between body mass index and uric acid on blood pressure status of participants categorized by age in male and female (N=3629).
| Characteristics | Age <68 years (n=807) |
Age≥68 years (n=1003) |
||
|
| ||||
| Male | Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
|
| ||||
| Marital status (0= Single,1= Married) | -6.913(0.009) | -5.237(0.001) | -5.876(0.007) | |
| Current residence (0= Rural,1= Urban) | 5.232(0.004) | 2.164(0.015) | ||
| Smoke (0= NO,1= Former smoke,2= Current smoke) | 1.917(0.05) | |||
| Eating meals (0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | 3.746(0.058) | 3.227(0.006) | 2.239(0.036) | |
| Taking activities (0= No,1= Yes) | -2.747(0.057) | |||
| Antilipidemic medication (0= No,1= Yes) | -1.651(0.423) | |||
| Anti-hypertensive therapy (0= No,1= Yes) | 9.032(0.002) | 5.343(0.002) | 11.982(<0.001) | 6.384(<0.001) |
| Fasting plasma glucose (mg/dl) | 0.040(0.030) | |||
| eGFR (ml/min/1.73m2) | -0.122(0.024) | |||
| Serum uric acid(mg/dl) | 1.454(0.022) | 0.957(0.006) | ||
| Body mass index | -8.409(0.006) | -4.837(0.008) | -8.347(0.048) | -3.042(0.142) |
| Triglycerides | -0.135(0.958) | -0.587(0.695) | -7.960(0.035) | -1.478(0.427) |
| Body mass index∗ Triglycerides | -1.075(0.760) | -0.095(0.964) | 2.138(0.654) | -0.931(0.691) |
|
| ||||
| Female | Age <68 years (n=887) |
Age≥68 years (n=932) |
||
| Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
Systolic blood pressure β(P-value) |
Diastolic blood pressure β(P-value) |
|
|
| ||||
| Age | — | — | 0.626(0.001) | — |
| Education (0= Illiterate, 1= Less than elementary school, 2= High school, 3= Above vocational school) | — | — | — | — |
| Marital status (0= Single,1= Married) | 5.866(0.012) | — | 5.481(0.007) | 7.504(<0.001) |
| Eating meals (0= ≤2 meals per day,1=3 meals per day,2= ≥4 meals per day) | — | 2.821(0.009) | — | — |
| History of CVD (0= No,1= Yes) | — | — | — | -3.837(0.123) |
| Antilipidemic medication (0= No,1= Yes) | — | — | — | — |
| Anti-diabetic medication (0= No,1= Yes) | 11.822(0.002) | — | — | — |
| Anti-hypertensive therapy (0= No,1= Yes) | 8.946(0.006) | — | 17.459(<0.001) | 17.254(<0.001) |
| Fasting plasma glucose (mg/dl) | — | 0.035(<0.001) | — | |
| Body mass index | -5.696(0.062) | -6.621(<0.001) | -4.726(0.187) | -5.152(0.155) |
| Triglycerides | -4.716(0.063) | -2.716(0.024) | -1.573(0.622) | -2.147(0.507) |
| Body mass index∗ Triglycerides | -1.345(0.718) | 2.410(0.170) | -4.192(0.334) | -3.386(0.439) |
Table 16 shows relationships between BMI or TG level and hypertension in men and women. After adjusting for age, educational level, marital status, current residence, smoking, drinking, eating habits, activity, major accidental injury, physical activity, history of CVD, history of liver disease, antilipidemic medication, antidiabetic medication, antihypertensive therapy, FPG, LDL-C, HDL-C, eGFR, and SUA, compared with their counterparts with BMI < 24.0 kg/m2, both elderly men and women with a BMI ≥ 24.0 kg/m2 were more likely to have high BP (men: odds ratio [OR] = 1.781, 95% confidence interval [CI] = 1.393–2.277; women: OR = 1.653, 95% CI = 1.330–2.055). Among women, compared to those with TG < 150 mg/dL, individuals with a high TG level were more likely to have high BP (OR = 1.558, 95% CI = 1.219–1.992).
Table 16.
Adjusting ORs and 95%CI for BMI or TG and hypertension in male and female.
| Male | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI and hypertension | TG and hypertension | BMI and hypertension | TG and hypertension | |||||||||
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Age(years) | 1.027 | (1.007,1.047) | 0.007 | 1.021 | (1.002,1.041) | 0.029 | 1.056 | (1.037,1.076) | <0.001 | 1.054 | (1.035,1.073) | <0.001 |
| education | ||||||||||||
| Illiterate | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than elementary school | 1.066 | (0.817,1.391) | 0.636 | 1.086 | (0.834,1.415) | 0.538 | 0.875 | (0.703,1.088) | 0.229 | 0.876 | (0.705,1.089) | 0.233 |
| High school | 0.649 | (0.271,1.553) | 0.331 | 0.662 | (0.279,1.567) | 0.348 | 0.169 | (0.037,0.777) | 0.022 | 0.178 | (0.038,0.823) | 0.027 |
| Above vocational school | 0.817 | (0.493,1.352) | 0.431 | 0.837 | (0.508,1.379) | 0.485 | 0.671 | (0.304,1.484) | 0.325 | 0.704 | (0.319,1.557) | 0.387 |
| Marital status | ||||||||||||
| Single | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Married | 0.693 | (0.515,0.933) | 0.016 | 0.726 | (0.540,0.975) | 0.033 | 0.833 | (0.660,1.052) | 0.126 | 0.854 | (0.676,1.077) | 0.183 |
| Current residence | ||||||||||||
| Urban | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Rural | 1.281 | (1.021,1.608) | 0.033 | 1.327 | (1.058,1.663) | 0.014 | 1.028 | (0.826,1.278) | 0.807 | 1.057 | (0.851,1.314) | 0.616 |
| Smoke | ||||||||||||
| NO smoke | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Former smoke | 0.892 | (0.660,1.204) | 0.454 | 0.906 | (0.672,1.221) | 0.518 | 0.914 | (0.523,1.599) | 0.753 | 0.844 | (0.482,1.476) | 0.551 |
| Current smoke | 1.309 | (1.019,1.682) | 0.035 | 1.235 | (0.964,1.582) | 0.095 | 1.155 | (0.810,1.648) | 0.427 | 1.106 | (0.777,1.573) | 0.577 |
| Drinking | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than once a month | 1.030 | (0.823,1.289) | 0.796 | 1.051 | (0.841,1.313) | 0.663 | 1.060 | (0.733,1.533) | 0.758 | 1.045 | (0.722,1.513) | 0.814 |
| More than once a month | 1.134 | (0.772,1.665) | 0.523 | 1.141 | (0.780,1.671) | 0.496 | 0.696 | (0.416,1.164) | 0.167 | 0.716 | (0.429,1.196) | 0.202 |
| Eating meals | ||||||||||||
| ≤2 meals per day | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| 3 meals per day | 0.898 | (0.381,2.117) | 0.806 | 0.832 | (0.355,1.953) | 0.673 | 0.777 | (0.328,1.837) | 0.565 | 0.782 | (0.330,1.851) | 0.575 |
| ≥4 meals per day | 0.658 | (0.494,0.875) | 0.004 | 0.682 | (0.513,0.906) | 0.008 | 0.983 | (0.739,1.308) | 0.909 | 1.050 | (0.790,1.396) | 0.737 |
| Taking no activities | ||||||||||||
| No | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.916 | (0.744,1.127) | 0.407 | 0.930 | (0.756,1.142) | 0.487 | 1.021 | (0.834,1.250) | 0.840 | 1.035 | (0.846,1.266) | 0.738 |
| Ever been in major accidental injury | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.746 | (0.535,1.041) | 0.085 | 0.754 | (0.542,1.049) | 0.094 | 0.864 | (0.584,1.279) | 0.4660 | 0.871 | (0.588,1.290) | 0.491 |
| Having regular physical exercises | ||||||||||||
| No physical exercise | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than regular physical exercises | 1.199 | (0.927,1.550) | 0.168 | 1.220 | (0.945,1.576) | 0.127 | 0.975 | (0.748,1.270) | 0.849 | 0.959 | (0.736,1.250) | 0.756 |
| Regular physical exercises | 1.282 | (0.972,1.690) | 0.079 | 1.292 | (0.981,1.701) | 0.068 | 0.919 | (0.705,1.197) | 0.530 | 0.922 | (0.708,1.201) | 0.546 |
| History of CVD | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.170 | (0.869,1.575) | 0.300 | 1.247 | (0.930,1.673) | 0.141 | 0.982 | (0.750,1.286) | 0.896 | 0.986 | (0.753,1.290) | 0.916 |
| History of liver diseases | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.640 | (0.369,1.110) | 0.112 | 0.654 | (0.379,1.129) | 0.128 | 0.795 | (0.466,1.355) | 0.399 | 0.837 | (0.491,1.429) | 0.515 |
| Antilipidemic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.984 | (0.601,1.612) | 0.949 | 1.027 | (0.629,1.679) | 0.914 | 1.711 | (1.127,2.596) | 0.012 | 1.783 | (1.177,2.701) | 0.006 |
| Anti-diabetic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.549 | (0.312,0.965) | 0.037 | 0.586 | (0.334,1.030) | 0.063 | 1.421 | (0.846,2.387) | 0.184 | 1.540 | (0.919,2.581) | 0.101 |
| Anti-hypertensive therapy | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 2.448 | (1.635,3.665) | <0.001 | 2.522 | (1.690,3.766) | <0.001 | 2.097 | (1.416,3.105) | <0.001 | 2.154 | (1.457,3.186) | <0.001 |
| Fasting plasma glucose(mg/dl) | 1.005 | (1.002,1.008) | <0.001 | 1.005 | (1.002,1.008) | 0.001 | 1.004 | (1.001,1.007) | 0.005 | 1.004 | (1.001,1.006) | 0.017 |
| LDL Cholesterol (mg/dl) | 1.004 | (1.001,1.007) | 0.014 | 1.004 | (1.001,1.008) | 0.004 | 1.001 | (0.998,1.004) | 0.585 | 1.001 | (0.999,1.004) | 0.316 |
| HDL Cholesterol (mg/dl) | 0.998 | (0.991,1.005) | 0.614 | 0.995 | (0.988,1.002) | 0.158 | 0.997 | (0.990,1.004) | 0.383 | 0.999 | (0.991,1.006) | 0.708 |
| Egfr (ml/min/1.73m2) | 0.993 | (0.986,1.001) | 0.089 | 0.993 | (0.986,1.001) | 0.091 | 0.998 | (0.990,1.005) | 0.566 | 0.997 | (0.990,1.005) | 0.455 |
| Serum uric acid(mg/dl) | 1.160 | (1.064,1.265) | 0.001 | 1.175 | (1.077,1.282) | <0.001 | 1.122 | (1.017,1.238) | 0.022 | 1.118 | (1.013,1.234) | 0.027 |
| Body mass index (kg/m2) | ||||||||||||
| BMI <24 | 1.000 | 1.000 | ||||||||||
| BM I≥24 | 1.781 | (1.393,2.277) | <0.001 | 1.653 | (1.330,2.055) | <0.001 | ||||||
| Triglycerides (mg/dl) | ||||||||||||
| <150 | 1.000 | 1.000 | ||||||||||
| ≥150 | 1.169 | (0.882,1.548) | 0.277 | 1.558 | (1.219,1.992) | <0.001 | ||||||
Tables 17 and 18 show relationships between BMI or TG and hypertension categorized by age in men and women. After adjusting for age, educational level, marital status, current residence, smoking, drinking, eating habits, taking activities, major accidental injury, physical activity, history of CVD, history of liver disease, antilipidemic medication, antidiabetic medication, antihypertensive therapy, FPG, LDL-C, HDL-C, eGFR, and SUA, compared to individuals with a BMI < 24.0 kg/m2, both elderly men and women with a BMI ≥ 24.0 kg/m2 were more likely to have high BP (men with age of < 68 years, OR=1.805, and 95% CI=1.249-2.610; men with age of ≥ 68 years, OR = 1.796, and 95% CI = 1.275–2.529; women with age of < 68 years, OR = 1.936, and 95% CI = 1.404–2.668; women with age of ≥ 68 years, OR = 1.506, and 95% CI = 1.108–2.047). Among women, compared to those with TG < 150 mg/dL, individuals with a high TG level were more likely to have high BP (women with age of < 68 years, OR = 1.629, and 95% CI = 1.149–2.309; women with age of ≥ 68 years, OR = 1.596, and 95% CI = 1.113–2.288).
Table 17.
Adjusting ORs and 95%CI for BMI or TG and hypertension categorized by age in male.
| Age <68 years (n=807) | Age≥68 years (n=1003) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI and hypertension | TG and hypertension | BMI and hypertension | TG and hypertension | |||||||||
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Age(years) | 1.009 | (0.937,1.088) | 0.806 | 1.006 | (0.934,1.083) | 0.877 | 1.021 | (0.988,1.055) | 0.212 | 1.015 | (0.982,1.048) | 0.383 |
| education | ||||||||||||
| Illiterate | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than elementary school | 0.805 | (0.487,1.330) | 0.397 | 0.850 | (0.516,1.401) | 0.523 | 1.171 | (0.852,1.609) | 0.330 | 1.182 | (0.862,1.621) | 0.299 |
| High school | 1.212 | (0.353,4.157) | 0.760 | 1.201 | (0.352,4.092) | 0.770 | 0.303 | (0.080,1.158) | 0.081 | 0.321 | (0.086,1.207) | 0.093 |
| Above vocational school | 0.687 | (0.288,1.641) | 0.399 | 0.749 | (0.316,1.774) | 0.511 | 0.809 | (0.424,1.543) | 0.519 | 0.802 | (0.423,1.521) | 0.499 |
| Marital status | ||||||||||||
| Single | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Married | 0.501 | (0.283,0.885) | 0.017 | 0.548 | (0.311,0.967) | 0.038 | 0.762 | (0.535,1.085) | 0.132 | 0.785 | (0.552,1.116) | 0.177 |
| Current residence | ||||||||||||
| Urban | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Rural | 1.183 | (0.834,1.680) | 0.346 | 1.244 | (0.880,1.759) | 0.216 | 1.413 | (1.037,1.925) | 0.028 | 1.459 | (1.072,1.986) | 0.016 |
| Smoke | ||||||||||||
| NO smoke | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Former smoke | 0.894 | (0.538,1.486) | 0.666 | 0.897 | (0.541,1.486) | 0.672 | 0.905 | (0.617,1.327) | 0.609 | 0.927 | (0.634,1.356) | 0.696 |
| Current smoke | 1.337 | (0.893,2.000) | 0.158 | 1.219 | (0.820,1.810) | 0.327 | 1.322 | (0.953,1.836) | 0.095 | 1.274 | (0.921,1.763) | 0.144 |
| Drinking | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than once a month | 0.971 | (0.681,1.386) | 0.873 | 0.996 | (0.699,1.418) | 0.980 | 1.049 | (0.778,1.413) | 0.755 | 1.064 | (0.791,1.431) | 0.681 |
| More than once a month | .908 | (0.504,1.636) | 0.747 | 0.918 | (0.512,1.645) | 0.774 | 1.459 | (0.863,2.469) | 0.159 | 1.469 | (0.872,2.475) | 0.148 |
| Eating meals | ||||||||||||
| ≤2 meals per day | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| 3 meals per day | 0.093 | (0.011,0.803) | 0.031 | 0.090 | (0.011,0.756) | 0.027 | 3.274 | (0.921,11.630) | 0.067 | 3.131 | (0.884,11.09) | 0.077 |
| ≥4 meals per day | 0.624 | (0.396,0.983) | 0.042 | 0.644 | (0.408,1.016) | 0.058 | 0.657 | (0.452,0.955) | 0.028 | 0.684 | (0.472,0.992) | 0.045 |
| Taking no activities | ||||||||||||
| No | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.748 | (0.541,1.035) | 0.080 | 0.764 | (0.554,1.054) | 0.101 | 1.053 | (0.798,1.389) | 0.717 | 1.065 | (0.808,1.403) | 0.657 |
| Ever been in major accidental injury | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.640 | (0.363,1.128) | 0.122 | 0.606 | (0.344,1.065) | 0.082 | 0.781 | (0.510,1.197) | 0.256 | 0.809 | (0.530,1.234) | 0.325 |
| Having regular physical exercises | ||||||||||||
| No physical exercise | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than regular physical exercises | 0.959 | (0.626,1.468) | 0.846 | 0.978 | (0.641,1.494) | 0.919 | 1.397 | (1.000,1.952) | 0.050 | 1.418 | (1.017,1.978) | 0.039 |
| Regular physical exercises | 1.185 | (0.776,1.809) | 0.432 | 1.225 | (0.805,1.864) | 0.344 | 1.432 | (0.983,2.084) | 0.061 | 1.422 | (0.978,2.066) | 0.065 |
| History of CVD | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.355 | (0.821,2.238) | 0.235 | 1.478 | (0.902,2.424) | 0.121 | 1.063 | (0.725,1.557) | 0.755 | 1.132 | (0.777,1.650) | 0.518 |
| History of liver diseases | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.630 | (0.283,1.399) | 0.256 | .624 | (0.283,1.378) | 0.244 | 0.595 | (0.270,1.309) | 0.197 | 0.640 | (0.293,1.395) | 0.261 |
| Antilipidemic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.135 | (0.568,2.269) | 0.720 | 1.142 | (0.574,2.273) | 0.706 | 0.861 | (0.407,1.821) | 0.695 | 0.911 | (0.433,1.902) | 0.807 |
| Anti-diabetic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.476 | (0.194,1.173) | 0.107 | 0.520 | (0.210,1.285) | 0.156 | 0.655 | (0.308,1.393) | 0.272 | 0.683 | (0.323,1.447) | 0.320 |
| Anti-hypertensive therapy | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 2.277 | (1.242,4.174) | 0.008 | 2.299 | (1.258,4.202) | 0.007 | 2.681 | (1.536,4.681) | 0.001 | 2.748 | (1.577,4.791) | <0.001 |
| Fasting plasma glucose(mg/dl) | 1.004 | (1.000,1.008) | 0.075 | 1.004 | (1.000,1.009) | 0.071 | 1.007 | (1.002,1.011) | 0.003 | 1.006 | (1.002,1.011) | 0.005 |
| LDL Cholesterol (mg/dl) | 1.007 | (1.003,1.011) | 0.002 | 1.008 | (1.003,1.012) | 0.001 | 1.001 | (0.996,1.005) | 0.817 | 1.001 | (0.997,1.005) | 0.655 |
| HDL Cholesterol (mg/dl) | 0.993 | (0.982,1.004) | 0.227 | 0.989 | (0.977,1.000) | 0.053 | 1.002 | (0.993,1.011) | 0.691 | 0.998 | (0.989,1.008) | 0.743 |
| eGFR(ml/min/1.73m2) | 0.987 | (0.976,0.999) | 0.040 | 0.988 | (0.976,1.000) | 0.048 | 0.998 | (0.988,1.008) | 0.692 | 0.998 | (0.988,1.008) | 0.682 |
| Serum uric acid(mg/dl) | 1.171 | (1.020,1.344) | 0.025 | 1.184 | (1.028,1.364) | 0.019 | 1.185 | (1.056,1.331) | 0.004 | 1.205 | (1.074,1.353) | 0.002 |
| Body mass index(kg/m2) | ||||||||||||
| BMI<24 | 1.000 | 1.000 | ||||||||||
| BMI≥24 | 1.805 | (1.249,2.610) | 0.002 | 1.796 | (1.275,2.529) | 0.001 | ||||||
| Triglycerides (mg/dl) | ||||||||||||
| <150 | 1.000 | 1.000 | ||||||||||
| ≥150 | 1.140 | (0.754,1.722) | 0.535 | 1.098 | (0.733,1.643) | 0.651 | ||||||
Table 18.
Adjusting ORs and 95%CI for BMI or TG and hypertension categorized by age in female.
| Age <68 years (n=807) | Age≥68 years (n=1003) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI and hypertension | TG and hypertension | BMI and hypertension | TG and hypertension | |||||||||
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Age(years) | 1.077 | (1.008,1.105) | 0.029 | 1.071 | (1.003,1.144) | 0.040 | 1.055 | (1.022,1.089) | 0.001 | 1.053 | (1.020,1.087) | 0.001 |
| education | ||||||||||||
| Illiterate | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than elementary school | 0.807 | (0.596,1.093) | 0.166 | 0.803 | (0.593,1.087) | 0.155 | 0.966 | (0.698,1.337) | 0.834 | 0.972 | (0.702,1.345) | 0.863 |
| High school | 0.231 | (0.027,1.980) | 0.181 | 0.277 | (0.032,2.410) | 0.245 | 0.121 | (0.014,1.046) | 0.055 | 0.116 | (0.013,1.003) | 0.050 |
| Above vocational school | 0.798 | (0.227,2.805) | 0.725 | 0.820 | (0.239,2.809) | 0.752 | 0.668 | (0.234,1.907) | 0.451 | 0.726 | (0.252,2.086) | 0.552 |
| Marital status | ||||||||||||
| Single | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Married | 0.681 | (0.457,1.017) | 0.060 | 0.717 | (0.482,1.066) | 0.100 | 0.891 | (0.663,1.196) | 0.441 | 0.904 | (0.674,1.214) | 0.502 |
| Current residence | ||||||||||||
| Urban | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Rural | 1.118 | (0.810,1.543) | 0.499 | 1.191 | (0.864,1.643) | 0.286 | 1.003 | (0.739,1.362) | 0.984 | 1.009 | (0.743,1.369) | 0.955 |
| Smoke | ||||||||||||
| NO smoke | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Former smoke | 2.322 | (0.771,6.998) | 0.134 | 2.228 | (0.743,6.681) | 0.153 | 0.715 | (0.367,1.391) | 0.323 | 0.649 | (0.333,1.267) | 0.206 |
| Current smoke | 1.502 | (0.905,2.494) | 0.116 | 1.383 | (0.840,2.277) | 0.203 | 0.888 | (0.535,1.473) | 0.644 | 0.858 | (0.517,1.424) | 0.553 |
| Drinking | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than once a month | 0.917 | (0.518,1.622) | 0.765 | 0.963 | (0.547,1.695) | 0.896 | 1.107 | (0.668,1.837) | 0.693 | 1.057 | (0.635,1.758) | 0.831 |
| More than once a month | 0.938 | (0.464,1.897) | 0.859 | 0.894 | (0.443,1.803) | 0.755 | 0.508 | (0.235,1.100) | 0.086 | 0.559 | (0.257,1.214) | 0.142 |
| Eating meals | ||||||||||||
| ≤2 meals per day | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| 3 meals per day | 0.843 | (0.264,2.689) | 0.773 | 0.861 | (0.269,2.754) | 0.800 | 0.637 | (0.176,2.302) | 0.492 | 0.646 | (0.179,2.332) | 0.505 |
| ≥4 meals per day | 0.744 | (0.486,1.140) | 0.174 | 0.801 | (0.524,1.225) | 0.306 | 1.213 | (0.822,1.790) | 0.330 | 1.297 | (0.879,1.914) | 0.190 |
| Taking no activities | ||||||||||||
| No | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.950 | (0.705,1.280) | 0.737 | 0.984 | (0.732,1.323) | 0.917 | 1.117 | (0.8400,1.486) | 0.446 | 1.115 | (0.838,1.482) | 0.456 |
| Ever been in major accidental injury | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 0.888 | (0.491,1.604) | 0.693 | 0.906 | (0.501,1.639) | 0.744 | 0.831 | (0.485,1.423) | 0.499 | 0.820 | (0.477,1.408) | .472 |
| Having regular physical exercises | ||||||||||||
| No physical exercise | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Less than regular physical exercises | 1.037 | (0.709,1.517) | 0.852 | 1.024 | (0.701,1.496) | 0.904 | 0.851 | (0.581,1.246) | 0.407 | 0.826 | (0.564,1.210) | .327 |
| Regular physical exercises | 0.978 | (0.669,1.432) | 0.911 | 0.953 | (0.652,1.393) | 0.804 | 0.924 | (0.627,1.361) | 0.688 | 0.944 | (0.640,1.391) | .770 |
| History of CVD | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.563 | (1.062,2.300) | 0.023 | 1.586 | (1.079,2.331) | 0.019 | 0.640 | (0.435,0.942) | 0.023 | 0.640 | (0.435,0.940) | 0.023 |
| History of liver diseases | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.100 | (0.495,2.446) | 0.815 | 1.190 | (0.533,2.654) | 0.671 | 0.645 | (0.309,1.345) | 0.242 | 0.671 | (0.322,1.398) | 0.286 |
| Antilipidemic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.487 | (0.869,2.544) | 0.148 | 1.587 | (0.930,2.708) | 0.090 | 2.127 | (1.051,4.301) | 0.036 | 2.174 | (1.082,4.368) | 0.029 |
| Anti-diabetic medication | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 1.613 | (0.806,3.229) | 0.177 | 1.728 | (0.865,3.454) | 0.122 | 1.318 | (0.594,2.925) | 0.498 | 1.429 | (0.648,3.147) | 0.376 |
| Anti-hypertensive therapy | ||||||||||||
| NO | 1.000 | 1.000 | 1.000 | 1.000 | ||||||||
| Yes | 2.039 | (1.187,3.502) | 0.010 | 2.031 | (1.185,3.479) | 0.010 | 2.260 | (1.241,4.113) | 0.008 | 2.409 | (1.321,4.396) | 0.004 |
| Fasting plasma glucose(mg/dl) | 1.003 | (1.000,1.007) | 0.077 | 1.003 | (0.999,1.007) | 0.108 | 1.005 | (1.001,1.009) | 0.027 | 1.004 | (1.000,1.008) | 0.081 |
| LDL Cholesterol (mg/dl) | 0.999 | (0.995,1.003) | 0.686 | 1.000 | (0.996,1.004) | 0.836 | 1.002 | (0.998,1.006) | 0.331 | 1.002 | (0.998,1.006) | 0.245 |
| HDL Cholesterol (mg/dl) | 0.997 | (0.986,1.008) | 0.629 | 0.998 | (0.986,1.010) | 0.745 | 0.995 | (0.985,1.005) | 0.344 | 0.998 | (0.987,1.008) | 0.688 |
| eGFR(ml/min/1.73m2) | 1.001 | (0.990,1.012) | 0.845 | 1.001 | (0.990,1.012) | 0.922 | 0.996 | (0.985,1.006) | 0.436 | 0.995 | (0.984,1.005) | 0.331 |
| Serum uric acid(mg/dl) | 1.132 | (0.979,1.310) | 0.095 | 1.117 | (0.965,1.294) | 0.137 | 1.103 | (0.961,1.265) | 0.163 | 1.099 | (0.958,1.262) | 0.179 |
| Body mass index(kg/m2) | ||||||||||||
| BMI<24 | 1.000 | 1.000 | ||||||||||
| BMI≥24 | 1.936 | (1.404,2.668) | <0.001 | 1.506 | (1.108,2.047) | 0.009 | ||||||
| Triglycerides (mg/dl) | ||||||||||||
| <150 | 1.000 | 1.000 | ||||||||||
| ≥150 | 1.629 | (1.149,2.309) | 0.006 | 1.596 | (1.113,2.288) | 0.011 | ||||||
4. Discussion
The effects of BMI and TG level on BP varied in elderly individuals. In the present study, we determined the prevalence of hypertension and its association with BMI and TG level. Our findings show that the prevalence of hypertension was 36.91% (668/1810) in men, 43.82% (797/1819) in women, and 40.37% (1465/3629) overall. After stratification by age, the prevalence of hypertension was 39.20% (481/1227) in men (age ≥ 65 years), 49.91% (576/1154) in women (age ≥ 65 years), and 44.39% (1057/2381) overall. In a sample collected from the Korea National Health and Nutrition Examination Survey (2007) in the elderly Korean population (age ≥ 65 years)[35], the prevalence of hypertension was 62.0%; the prevalence of hypertension in the Japan Gerontological Evaluation Survey[36], conducted in a population aged 65 or older, was 59.54%. The prevalence of hypertension in our study was lower than that observed in the Korean and Japanese studies. Moreover, men with hypertension had a higher prevalence of risk factors, such as age, marital status, eating habits, FPG, LDL-C, TG, eGFR, BMI, and SUA level, than those with normotension. Age, marital status, antilipidemic medication, FPG, TG, eGFR, and SUA level were significantly associated with BP among women. Furthermore, TG levels were positively associated with SBP and DBP in men with BMI < 24 kg/m2; however, TG levels were positively associated with both SBP and DBP in women with a BMI < 24 kg/m2 and also positively associated with DBP in women with a BMI ≥ 24 kg/m2.
Studies [37, 38] have explored the association and/or interaction analysis between BMI and SUA level and BP. Lyngdoh et al. [37] reported that adiposity substantially decreased the association between SUA level and BP in young adults, and BP was independently associated with SUA level in women. Kawamoto et al. [38] concluded that BMI changes the association between SUA level and BP status among community-dwelling men. In other studies [39, 40], the association of TG and SUA levels has been persistent after full adjustment in a multiple logistic model, suggesting that TG levels correlate independently with SUA level, with TG levels having the most influence on SUA. However, there were no previous studies on the interactive effect between BMI and TG level on BP.
As our general linear models adjusting for 13 related potential confounders showed, interaction between BMI and TG on BP was not observed. In our investigation of the relationships between BMI or TG and hypertension, we made several observations. First, we found that overweight and obese men and women were more likely to have hypertension. We also observed that women with high TG were more likely to experience hypertension. Thirdly, no association between TG and hypertension was found in men. Lastly, the relative results in relations between BMI or TG and hypertension categorized by age in both men and women are the same as those above. Furthermore, age differences in relations between BMI or TG and hypertension were found. Specifically, individuals with age ≥ 68 years experienced lower effects of BMI or TG level on BP. Similar evidence has been found in Brazil, in a study based on 287 men and women aged between 18 and 88 years, in which Pimenta [41] found that central obesity and TG level were independent risk factors for hypertension according to multivariate analysis. However, several studies have reported divergent findings regarding the association between obesity and hypertension. Some studies have suggested an increased risk of hypertension with higher BMI, waist circumference (WC), and waist-to-hip ratio (WHR) [42, 43], whereas other studies found that the association was not significant [44–46]. Zhou [47] conducted the first meta-analysis of cohort studies to quantify the relationship between obesity and the incidence of hypertension and found a positive association between the risk of hypertension and BMI, WC, and WHR. Arabshahi [48] conducted the first meta-analysis of cross-sectional studies to investigate the relationship between BMI or WC and hypertension, and concluded that the risk of hypertension was associated with adiposity. Jayedi [49] conducted a meta-analysis of prospective cohort studies to report the risk estimates of hypertension for abdominal adiposity (BMI, WC, and WHR) and found that the risk of hypertension increased with a somewhat steeper trend with increasing BMI, in comparison with WC and WHR. Such discrepancies between our findings and the null studies may be a result of methodological differences in design, measurement of obesity, and populations. Moreover, TG level has been associated with BP since TG level itself can cause endothelial dysfunction [24, 25], arterial stiffness [26], and the loss of vasomotor reactivity [27]. Such pathophysiology induced by increased TG and FPG levels and low HDL-C level may be greater than that of SUA. To explore the extent of the effects of TG level on blood pressure, we controlled for SUA and the related confounders, such as LDL-C and HDL-C [38]. The findings showed that TG level and hypertension were observed in women, but no independent effect was observed in men. Sanchez-Inigo [50] conducted a cohort study to identify the association of TG with the incidence of hypertension in Spain and found that the incidence of hypertension was associated with TG level in both men and women independent of adiposity. Tohidi [51] found that high TG independently predicted incidence of hypertension in Middle Eastern women.
The mechanisms that lead to hypertension in participants with high BMI or TG levels have not been completely understood. Current studies may provide insight into the pathogenic mechanisms of BMI/TG that induce hypertension. The present study suggests that TG level may play an important role in hypertension in women. We speculate that sex-specific factors may also play an important role. TG levels are higher in women than in men, which partially explains the underlying mechanism that accounts for sex difference based on hormone levels. Additionally, body fat, sex steroids, and their interaction in elderly participants may also be associated with hypertension. As an important sex hormone, estrogen may also affect BP. Elderly women have lower concentrations of estrogen, which may affect the level of TG and result in a smaller protective effect.
5. Strengths and Limitations of the Study
There are several limitations of our study. First, the association and interaction of BMI and serum TG on blood pressure become seriously more complex; we only consider the confounders as possible as we can, but there are some unknown factors. Secondly, the relationship should be studied prospectively. Our study investigated BP in the elderly participant through a cross-sectional study. Follow-up study was relatively short to comprehensively observe changes in the next step. Last, more research is needed to observe the result. Several strengths could be found in our study. Firstly, the study was based on a nationwide survey. Secondly, we conducted the analyses according to gender.
6. Conclusions
An interactive effect of BMI and TG level on BP was not observed in either men or women; however, independent effects of BMI on BP were observed in both men and women, and an association between TG level and hypertension was observed in women.
Acknowledgments
The authors are grateful to the participants and members of the CHARLS. CHARLS was supported by the NIA. Lin Zhang gives thanks to his wife (Haiyang Liu) who stands behind him for supporting him in the past year during writing the paper.
Abbreviations
- CHARLS:
China Health and Retirement Longitudinal Study
- BMI:
Body mass index
- BP:
Blood pressure
- DBP:
Diastolic blood pressure
- SBP:
Systolic blood pressure
- SUA:
Serum uric acid
- CVD:
Cardiovascular disease
- M:
Mean
- eGFR:
Estimated glomerular filtration rate
- CDC:
Centers for Disease Control and Prevention
- Scr:
Serum creatinine
- Scys:
Serum cystatin C
- SD:
Standard deviation
- LDL:
Low-density lipoprotein
- HDL:
High-density lipoprotein
- NIA:
National intelligence agency
- FPG:
Fasting plasma glucose
- TG:
Triglycerides
- WC:
Waist circumference
- WHR:
Waist to hip ratio.
Data Availability
Data sharing statement Extra data can be accessed via http://charls.pku.edu.cn/zh-CN.
Ethical Approval
The study is publicly available at http://charls.pku.edu.cn/zh-CN with no direct contact with the individual participants.
Consent
The patient's consent was obtained.
Disclosure
The funding body was not involved in the design of the study, data collection, analysis, and interpretation, or in writing the manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Lin Zhang conceived and drafted the manuscript. Jin-long Li, Li-li Zhang, Lei-lei Guo, Hong Li, and Dan Li helped revise the manuscript. All authors have read and approved the manuscript.
References
- 1.Zhao Y., Yan H., Marshall R. J., et al. Trends in population blood pressure and prevalence, awareness, treatment, and control of hypertension among middle-aged and older adults in a rural area of Northwest China from 1982 to 2010. PLoS ONE. 2013;8(4):p. e61779. doi: 10.1371/journal.pone.0061779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Y., Huxley R., Li L., et al. Prevalence, awareness, treatment, and control of hypertension in China data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118(25):2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 3.Liu X., Gu W., Li Z., Lei H., Li G., Huang W. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: An update. Journal of Hypertension. 2017;35(3):637–644. doi: 10.1097/HJH.0000000000001203. [DOI] [PubMed] [Google Scholar]
- 4.Wu L., He Y., Jiang B., et al. Trends in prevalence, awareness, treatment and control of hypertension during 2001-2010 in an urban elderly population of China. PLoS ONE. 2015;10(8):p. e0132814. doi: 10.1371/journal.pone.0132814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang S., Chen R., Liu Q., Shu Z., Zhan S., Li L. Prevalence, awareness and treatment of chronic kidney disease among middle-aged and elderly: The China Health and Retirement Longitudinal Study. Nephrology. 2015;20(7):474–484. doi: 10.1111/nep.12449. [DOI] [PubMed] [Google Scholar]
- 6.Glynn R. J., L'Italien G. J., Sesso H. D., Jackson E. A., Buring J. E. Development of predictive models for long-term cardiovascular risk associated with systolic and diastolic blood pressure. Hypertension. 2002;39(1):105–110. doi: 10.1161/hy1201.097199. [DOI] [PubMed] [Google Scholar]
- 7.Yu D., Huang J., Hu D., et al. Association between prehypertension and clustering of cardiovascular disease risk factors among chinese adults. Journal of Cardiovascular Pharmacology. 2009;53(5):388–400. doi: 10.1097/FJC.0b013e3181a02238. [DOI] [PubMed] [Google Scholar]
- 8.Gu D., Chen J., Wu X., et al. Prehypertension and risk of cardiovascular disease in Chinese adults. Journal of Hypertension. 2009;27(4):721–729. doi: 10.1097/HJH.0b013e328323ad89. [DOI] [PubMed] [Google Scholar]
- 9.Fagard R. H. Predicting risk of fatal cardiovascular disease and sudden death in hypertension. Journal of Hypertension. 2017;35(11):2165–2167. doi: 10.1097/HJH.0000000000001485. [DOI] [PubMed] [Google Scholar]
- 10.James J. E. Hypertension control and cardiovascular disease. The Lancet. 2017;389(10065):p. 154. doi: 10.1016/S0140-6736(17)30018-1. [DOI] [PubMed] [Google Scholar]
- 11.Lackland D. T., Weber M. A. Global burden of cardiovascular disease and stroke: hypertension at the core. Canadian Journal of Cardiology. 2015;31(5):569–571. doi: 10.1016/j.cjca.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Cloutier L., Morris D., Bruneau J., McLean D., Campbell N. World Health Organization celebrates World Health Day, April 7,2013--focusing on hypertension. Canadian Journal of Cardiovascular Nursing. 2013;23(2):9–11. [PubMed] [Google Scholar]
- 13.Gui Z., Zhu Y., Cai L., et al. Sugar-sweetened beverage consumption and risks of obesity and hypertension in chinese children and adolescents: a national cross-sectional analysis. Nutrients. 2017;9(12):p. 1302. doi: 10.3390/nu9121302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee M.-S., Chang C.-H., Lin R.-Y., Lai M.-S. Risks of hypertension associated with cyclosporine, nonsteroidal anti-inflammatory drugs, and systemic glucocorticoids in patients with psoriasis: A nationwide population-based nested case-control study in Taiwan. Pharmacoepidemiology and Drug Safety. 2016;25(2):133–140. doi: 10.1002/pds.3890. [DOI] [PubMed] [Google Scholar]
- 15.Kannel W. B. Hypertension: reflections on risks and prognostication. Medical Clinics of North America. 2009;93(3):541–558. doi: 10.1016/j.mcna.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beilin L. Alcohol and hypertension: Balancing the risks and benefits. Journal of Hypertension. 2005;23(11):1953–1955. doi: 10.1097/01.hjh.0000187255.19998.29. [DOI] [PubMed] [Google Scholar]
- 17.Cartier A., Malo J. L., Gautrin D., Boulet L. P., Boisjoly H. Glucocorticoid use and risks of ocular hypertension and glaucoma. Journal of the American Medical Association. 1997;277(24):1929–1930. doi: 10.1001/jama.1997.03540480029020. [DOI] [PubMed] [Google Scholar]
- 18.Isezuo S. A., Sabir A. A., Ohwovorilole A. E., Fasanmade O. A. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in Northern Nigeria. Journal of Human Hypertension. 2011;25(4):224–230. doi: 10.1038/jhh.2010.56. [DOI] [PubMed] [Google Scholar]
- 19.Kawamoto R., Kohara K., Tabara Y., Abe M., Kusunoki T., Miki T. Insulin resistance and prevalence of prehypertension and hypertension among community-dwelling persons. Journal of Atherosclerosis and Thrombosis. 2010;17(2):148–155. doi: 10.5551/jat.2584. [DOI] [PubMed] [Google Scholar]
- 20.Kawamoto R., Tabara Y., Kohara K., Miki T., Abe M., Kusunoki T. Increased high-density lipoprotein cholesterol is associated with a high prevalence of pre-hypertension and hypertension in community-dwelling persons. Endocrine Journal. 2012;42(2):321–328. doi: 10.1007/s12020-012-9625-z. [DOI] [PubMed] [Google Scholar]
- 21.Zicha J., Kuneš J., Devynck M.-A. Abnormalities of membrane function and lipid metabolism in hypertension: A review. American Journal of Hypertension. 1999;12(3):315–331. doi: 10.1016/S0895-7061(98)00178-2. [DOI] [PubMed] [Google Scholar]
- 22.Teng F., Zhu R., Zou C., et al. Interaction between serum uric acid and triglycerides in relation to blood pressure. Journal of Human Hypertension. 2011;25(11):686–691. doi: 10.1038/jhh.2010.112. [DOI] [PubMed] [Google Scholar]
- 23.Brennan P. J., Simpson J. M., Blacket R. B., McGilchrist C. A. The effects of body weight on serum cholesterol, serum triglycerides, serum urate and systolic blood pressure. Australian and New Zealand Journal of Medicine. 1980;10(1):15–20. doi: 10.1111/j.1445-5994.1980.tb03412.x. [DOI] [PubMed] [Google Scholar]
- 24.McCarty M. F. Does postprandial storage of triglycerides in endothelial cells contribute to the endothelial dysfunction associated with insulin resistance and fatty diets? Medical Hypotheses. 2003;61(2):167–172. doi: 10.1016/S0306-9877(02)00236-0. [DOI] [PubMed] [Google Scholar]
- 25.Jagla A., Schrezenmeir J. Postprandial triglycerides and endothelial function. Experimental and Clinical Endocrinology & Diabetes. 2001;109(4):S533–S547. doi: 10.1055/s-2001-15116. [DOI] [PubMed] [Google Scholar]
- 26.Yao W.-M., Zhang H.-F., Zhu Z.-Y., et al. Genetically elevated levels of circulating triglycerides and brachial-ankle pulse wave velocity in a Chinese population. Journal of Human Hypertension. 2013;27(4):265–270. doi: 10.1038/jhh.2012.23. [DOI] [PubMed] [Google Scholar]
- 27.Lundman P., Eriksson M., Schenck-Gustafsson K., Karpe F., Tornvall P. Transient triglyceridemia decreases vascular reactivity in young, healthy men without risk factors for coronary heart disease. Circulation. 1997;96(10):3266–3268. doi: 10.1161/01.CIR.96.10.3266. [DOI] [PubMed] [Google Scholar]
- 28.Li C., Liu T., Sun W., Wu L., Zou Z.-Y. Prevalence and risk factors of arthritis in a middle-aged and older Chinese population: The China health and retirement longitudinal study. Rheumatology. 2014;54(4):697–706. doi: 10.1093/rheumatology/keu391. [DOI] [PubMed] [Google Scholar]
- 29.Ríos-González B., Ibarra-Cortés B., Ramírez-López G., Sánchez-Corona J., Magaña-Torres M. T. Association of Polymorphisms of Genes Involved in Lipid Metabolism with Blood Pressure and Lipid Values in Mexican Hypertensive Individuals. Disease Markers. 2014;2014:9. doi: 10.1155/2014/150358.150358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huo L., Ji L., Deng W., et al. Age distribution and metabolic disorders in people with Type 1 diabetes in Beijing and Shantou, China: a cross-sectional study. Diabetic Medicine. 2018;35(6):721–728. doi: 10.1111/dme.13616. [DOI] [PubMed] [Google Scholar]
- 31.Zhu Y., Ye X., Zhu B., et al. Comparisons between the 2012 new CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equations and other four approved equations. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0084688.e84688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang L., Liu K., Li H., et al. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC Public Health. 2016;16(1) doi: 10.1186/s12889-016-3864-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang H.-H., Yen S. T. Association between obesity and depression: Evidence from a longitudinal sample of the elderly in Taiwan. Aging & Mental Health. 2012;16(2):173–180. doi: 10.1080/13607863.2011.605053. [DOI] [PubMed] [Google Scholar]
- 34.Zhou B.-F. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomedical and environmental sciences : BES. 2002;15(3):245–252. [PubMed] [Google Scholar]
- 35.Kang M.-G., Kim S.-W., Yoon S.-J., Choi J.-Y., Kim K.-I., Kim C.-H. Association between frailty and hypertension prevalence, treatment, and control in the elderly Korean population. Scientific Reports. 2017;7(1) doi: 10.1038/s41598-017-07449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yazawa A., Inoue Y., Fujiwara T., et al. Association between social participation and hypertension among older people in Japan: The JAGES Study. Hypertension Research. 2016;39(11):818–824. doi: 10.1038/hr.2016.78. [DOI] [PubMed] [Google Scholar]
- 37.Lyngdoh T., Viswanathan B., Myers G. J., Bochud M., Bovet P. Impact of different adiposity measures on the relation between serum uric acid and blood pressure in young adults. Journal of Human Hypertension. 2012;26(11):677–683. doi: 10.1038/jhh.2011.85. [DOI] [PubMed] [Google Scholar]
- 38.Kawamoto R., Ninomiya D., Senzaki K., Kumagi T. Interaction between body mass index and serum uric acid in relation to blood pressure in community-dwelling Japanese men. Clinical Hypertension. 2018;24(1) doi: 10.1186/s40885-018-0087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nejatinamini S., Ataie-Jafari A., Qorbani M., et al. Association between serum uric acid level and metabolic syndrome components. Journal of Diabetes and Metabolic Disorders. 2015;14(1):p. 70. doi: 10.1186/s40200-015-0200-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin S.-D., Tsai D.-H., Hsu S.-R. Association between serum uric acid level and components of the metabolic syndrome. Journal of the Chinese Medical Association. 2006;69(11):512–516. doi: 10.1016/S1726-4901(09)70320-X. [DOI] [PubMed] [Google Scholar]
- 41.Pimenta A. M., Kac G., Gazzinelli A., Corrêa-Oliveira R., Velásquez-Meléndez G. Associação entre obesidade central, triglicerídeos e hipertensão arterial em uma área rural do Brasil. Arquivos Brasileiros de Cardiologia. 2008;90(6):386–392. doi: 10.1590/S0066-782X2008000600006. [DOI] [PubMed] [Google Scholar]
- 42.Grootveld L. R., Van Valkengoed I. G. M., Peters R. J. G., et al. The role of body weight, fat distribution and weight change in ethnic differences in the 9-year incidence of hypertension. Journal of Hypertension. 2014;32(5):990–997. doi: 10.1097/HJH.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 43.Fuchs F. D., Gus M., Moreira L. B., et al. Anthropometrie indices and the incidence of hypertension: a comparative analysis. Obesity Research. 2005;13(9):1515–1517. doi: 10.1038/oby.2005.184. [DOI] [PubMed] [Google Scholar]
- 44.Moliner-Urdiales D., Artero E. G., Sui X., España-Romero V., Lee D. C., Blair S. N. Body adiposity index and incident hypertension: The Aerobics Center Longitudinal Study. Nutrition, Metabolism & Cardiovascular Diseases. 2013;24(9):969–975. doi: 10.1016/j.numecd.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chei C.-L., Iso H., Yamagishi K., et al. Body fat distribution and the risk of hypertension and diabetes among Japanese men and women. Hypertension Research. 2008;31(5):851–857. doi: 10.1291/hypres.31.851. [DOI] [PubMed] [Google Scholar]
- 46.Williams P. T., Hoffman K., La I. Weight-related increases in hypertension, hypercholesterolemia, and diabetes risk in normal weight male and female runners. Arteriosclerosis, Thrombosis, and Vascular Biology. 2007;27(8):1811–1819. doi: 10.1161/ATVBAHA.107.141853. [DOI] [PubMed] [Google Scholar]
- 47.Zhou W., Shi Y., Li Y., et al. Body mass index, abdominal fatness, and hypertension incidence: a dose-response meta-analysis of prospective studies. Journal of Human Hypertension. 2018;32(5):321–333. doi: 10.1038/s41371-018-0046-1. [DOI] [PubMed] [Google Scholar]
- 48.Arabshahi S., Busingye D., Subasinghe A. K., Evans R. G., Riddell M. A., Thrift A. G. Adiposity has a greater impact on hypertension in lean than not-lean populations: A systematic review and meta-analysis. European Journal of Epidemiology. 2014;29(5):311–324. doi: 10.1007/s10654-014-9911-6. [DOI] [PubMed] [Google Scholar]
- 49.Jayedi A., Rashidy-Pour A., Khorshidi M., Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2.3 million participants. Obesity Reviews. 2018;19(5):654–667. doi: 10.1111/obr.12656. [DOI] [PubMed] [Google Scholar]
- 50.Sánchez-Íñigo L., Navarro-González D., Pastrana-Delgado J., Fernández-Montero A., Martínez J. A. Association of triglycerides and new lipid markers with the incidence of hypertension in a Spanish cohort. Journal of Hypertension. 2016;34(7):1257–1265. doi: 10.1097/HJH.0000000000000941. [DOI] [PubMed] [Google Scholar]
- 51.Tohidi M., Hatami M., Hadaegh F., Azizi F. Triglycerides and triglycerides to high-density lipoprotein cholesterol ratio are strong predictors of incident hypertension in Middle Eastern women. Journal of Human Hypertension. 2012;26(9):525–532. doi: 10.1038/jhh.2011.70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing statement Extra data can be accessed via http://charls.pku.edu.cn/zh-CN.