Abstract
Background
For children with cleft lip and/or palate (CLCP), access to care is vital for optimizing speech, appearance, and psychosocial outcomes. The authors posited that that inadequate access to care negatively impacts outcomes in the CLCP population.
Methods
Sixty caregivers of children with CLCP were surveyed to assess perceived barriers using the validated Barriers to Care questionnaire (BCQ). The BCQ includes 39 items divided into five subscales, with higher scores indicating fewer barriers. Caregiver reported outcomes (CROs) were assessed using the Cleft Evaluation Profile (CEP), which captures CLCP specific appearance- and speech-related outcomes. Higher scores correspond to less satisfactory outcomes. Desire for revision surgery was assessed as a binary outcome amongst caregivers. Multivariable regression was used to evaluate the relationship between barriers to care, CROs, and desire for revision, adjusting for clinical and demographic covariates.
Results
60% of caregivers perceived barriers to care, and caregivers who reported poorer access to care described poorer cleft-related outcomes (r2=0.19, p=0.024). Caregivers with poorer Skills (r2=0.17, p=0.037), Expectations (r2=0.17, p=0.045), and Pragmatics (r2=0.18, p=0.026) subscale scores were associated with lower CEP scores. Barriers were also negatively associated with aesthetic item scores (r2=0.11, p=0.025). Finally, caregivers reporting fewer barriers were 21.2% less likely to express interest in revision surgery.
Conclusions
Barriers to care were associated with poorer appearance-related outcomes and increased interest in revision among caregivers of patients with CLCP. Enhancing access to care is critical in order to effectively meet goals of care for these families.
INTRODUCTION
Children’s access to quality medical care is influenced by family structure [1], where they live [2,3], and payer type [4]. For example, surgery is often delayed secondary to race and insurance type [5], and emergency department utilization is similarly impacted by these factors [4]. Although prior work has examined barriers and disparities in the pediatric population, little is known regarding barriers to care specific to children with cleft lip and palate (CLCP). Patients with CLCP qualify as Children with Special Healthcare Needs, defined as “those who are at increased risk for a chronic physical, development, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally” [6]. These children often have difficulty accessing the care they need, especially those living in rural or underserved communities [7]. Given the need for multiple surgeries and multidisciplinary care in patients with CLCP, ensuring long-term access is critical for optimizing both clinical and patient-reported outcomes.
Although clinical outcomes are routinely used to assess treatment effectiveness and quality [8–10], patient-reported outcomes (PROs) are increasingly emphasized [11–13]. PROs specifically demonstrate the patient’s experience and thus reflect the patient’s perception of quality of life and other relevant outcomes [14,15]. In patients with CLCP, PROs as measured by PRO measures (PROMs) may provide a clearer assessment of care, given that many clinical outcomes, such as readmission, major complications, and mortality, are infrequent. Furthermore, CLCP procedures are performed to improve orofacial function and appearance and prevent stigma and isolation [16]. Prior research has demonstrated that cleft specific outcomes, such as facial appearance and speech, are correlated with broader aspects of health-related quality of life (HRQOL) [17–19]. Interestingly, PROs were shown to be negatively impacted by barriers to care in certain populations [20,21]. Additionally, caregiver wellbeing and perceptions can significantly impact patients’ adjustment and self-perception, rendering caregiver satisfaction and perceived barriers to care important also [22]. However, the effect of access on patient and caregiver satisfaction has remained unstudied in the CLCP population.
Given the health care needs of patients with CLCP, the authors hypothesized that both caregiver-reported outcomes (CROs) and desire for revision are correlated with access, and families with improved access to care report superior CROs compared with families with poorer access to care. To evaluate these relationships, perceived barriers to care, cleft specific caregiver-reported outcomes, and desire for revision among families cared for at a multispecialty cleft and craniofacial anomalies clinic were examined. Such data could guide policy-related interventions and quality improvement efforts to improve access for cleft patients and their families.
METHODS
Caregivers of children ages 5–19 were surveyed in the University of Michigan Cleft and Craniofacial Anomalies Multidisciplinary Clinic (n=60) during routine clinic follow-up visits between January and August of 2017. Caregivers of patients with cleft lip and/or cleft palate (CLCP) able to read English were eligible for inclusion. Surveys were administered in person to caregivers by a research assistant.
Primary Outcome Variables
Our primary outcomes included caregiver assessment of speech and appearance outcomes, measured using the Cleft Evaluation Profile (CEP), as well as desire for revision surgery for their child. The Cleft Evaluation Profile is a seven-item questionnaire that addresses speech, hearing, and appearance, widely used among children with CLCP (Appendix) [23]. The CEP has been shown to have satisfactory levels of internal consistency among parents [18] and has been used previously to assess caregiver satisfaction [24–27]. Caregivers rated each item on a scale of 1 to 7, with 1 being “very satisfactory” and 7 being “very unsatisfactory.” The total scores were summed across both domains, as well as separate domain scores for speech/hearing and appearance. Desire for revision was evaluated by asking caregivers, “Do you ever want to have something related to your child’s cleft improved? (example: Appearance of your child’s lip/nose/teeth/jaws or ability to talk normally)”.
Barriers to care
Perceived access to care was assessed using the Barriers to Care Questionnaire (BCQ). The BCQ is a 39-item instrument previously used in pediatric patient populations to discern the specific barriers that impact access to medical care [28]. The instrument is divided into five subscales: Skills, Marginalization, Expectations, Knowledge and Beliefs, and Pragmatics. The Skills subscale reflects abilities or acquired strategies to navigate the health care system at large, while items in Marginalization measure the degree to which negative experiences while receiving past care impact current and future care experiences. Expectation items measure the degree to which caregivers expect poor care, and the Knowledge and Beliefs subscale reflects divergence between what caregivers and doctors believe is best for the child. Pragmatic items assess barriers related to cost and/or logistical issues [28]. For each item, caregivers are asked to select “no problem” (100), “small problem” (75), “problem” (50), “big problem” (25), and “very big problem” (0), with higher scores indicating fewer barriers [Appendix]. Total scores were tabulated, as well as scores for each subscale.
Patient and caregiver characteristics
Clinical and demographic data was collected by self-report from the survey instrument. This included caregiver age, sex, employment status, education level, income, and relationship status. Specifically, cleft type, distance from the hospital, and payer were captured using the medical record. Patient data collected included patient cleft type (unilateral cleft lip, bilateral cleft lip, cleft lip and palate, and isolated cleft palate) and presence of siblings.
Statistical Analysis
To assess the relationship between barriers to care and caregiver-reported aesthetic and speech outcomes as measured by the CEP, univariate analysis was performed to provide descriptive statistics of the cohort. Since the CEP scores were normally distributed, bivariate regression was used to assess the association of each individual caregiver- and patient-variable with mean caregiver CEP scores. All variables were assessed for collinearity. A nested multivariable linear regression was then performed to determine the association of BCQ scores with caregiver CEP scores, while adjusting for known confounding and/or clinically relevant variables. The same regression model was used to determine the association of subscale scores with caregiver CEP scores.
To assess the relationship between barriers and desire for revision, logistic regression was performed, controlling for clinically significant covariates and any statistically significant covariates found on bivariate analysis. Non-parametric statistics were used for bivariate analysis to assess covariates with a non-normal distribution. Statistical significance was set at p<0.05, and all analyses were conducted using StataCorp 15.0.
Approval for this study was obtained from the University of Michigan Institutional Review Board.
RESULTS
Characteristics of the study sample
In this cohort of 60 caregivers, the mean caregiver age was 43.7 (SD 7.9), and at least one caregiver was employed in every household. Most caregivers accompanying their child in clinic were female (82%). The majority of caregivers were married and had attended college (85%), and almost half earned an income above $100,000. Based upon addresses found in the medical record, the mean distance from the hospital was a 71-minute drive (SD 63.2, range 3.2 – 341.0), and most patients had private insurance (85%). The majority (73.3%) of caregivers had children with both cleft lip and palate, and 83% had siblings at home (Table 1).
Table 1.
Characteristics of the cohort and impact of characteristics on CEP scores on bivariate regression.
| Frequency (%) or Mean (SD) | Beta Coefficient | p-value | |
|---|---|---|---|
|
| |||
| Parent Gender | 0.07 | 0.83 | |
| Male | 11 (18.3%) | ||
| Female | 49 (81.7%) | ||
|
| |||
| Parent age | 43.7 (7.9) | 0.01 | 0.53 |
|
| |||
| Education | 0.14 | 0.37 | |
| Less than H.S. | 1 (1.7%) | ||
| HS diploma | 8 (13.3%) | ||
| Some college | 23 (38.3%) | ||
| College + | 28 (46.7%) | ||
|
| |||
| Income | −0.10 | 0.44 | |
| <$20K | 2 (3.4%) | ||
| $20K–$60K | 16 (27.1%) | ||
| $60K–$100K | 15 (25.4%) | ||
| >$100K | 26 (44.1%) | ||
|
| |||
| Relationship status | 0.22 | 0.25 | |
| Married | 51 (85%) | ||
| Significant other | 3 (5%) | ||
| Single | 6 (10.0%) | ||
|
| |||
| Siblings | −0.43 | 0.19 | |
| Yes | 50 (83.3%) | ||
| No | 10 (16.7%) | ||
|
| |||
| Cleft type | 0.08 | 0.68 | |
| Unilateral | 4 (6.7%) | ||
| Bilateral | 1 (1.7%) | ||
| CLCP | 44 (73.3%) | ||
| Palate only | 11 (18.3%) | ||
|
| |||
| Distance from hospital | 71.1 (63.2) | 0.001 | 0.52 |
|
| |||
| Payer | 0.15 | 0.65 | |
| Private | 51 (85.0%) | ||
| Medicaid | 9 (15.0%) | ||
|
| |||
| BCQ score | 95.2 (7.7) | −0.04 | 0.01* |
Perceived barriers to care
Sixty percent of caregivers perceived some barrier to care. Sixteen percent averaged below 90 on the BCQ, despite the average BCQ score being high (95.2 ±7.74), with higher scores indicating fewer barriers. The mean BCQ score for children with chronic conditions during validation was 78.4 [27]. Mean scores of the subscales that significantly correlated with outcomes are included in Table 2, with caregivers scoring the lowest in Skills 94.4 (SD 9.3), Expectations 96.0 (SD 10.1), and Pragmatics 91.5 (SD 12.2). The two lowest scoring questions within the Skills subscale dealt with knowing how to make the health care system work (91.1, SD 17.8) and having enough information about how the system works (91.3, SD 18.3). The lowest scoring questions within Expectations reflected poor communication between the child’s physician and others (93.3, SD 18.3) and poor communication between parts of the health care system (93.8, SD 15.0). The lowest scoring questions in the Pragmatics subscale dealt with taking time off work (86.7, SD 23.2) and cost of care (80, SD 29.8).
Table 2.
Mean scores of subscales that correlated with CEP scores, with lowest scoring questions.
| Subscale Scores | Lowest Scoring Questions | Mean Question Scores | Linear Regression R2 and p Values | |
|---|---|---|---|---|
|
| ||||
| Skills | 94.4 (9.3) | 1. Knowing how to make the health care system work for you. | 91.1 (SD 17.8) | r2=0.16 p=0.067 |
| 6. Having enough information about how the health care system works. | 91.3 (SD 18.3) | r2=0.13 p=0.188 |
||
|
| ||||
| Expectations | 96.0 (10.1) | 6. Lack of communication between my child’s doctor and others in the health care system. | 93.3 (18.3) | r2=0.15 p=0.089 |
| 7. Lack of communication between different parts of the health care system. | 93.8 (15.0) | r2=0.23 p=0.005* |
||
|
| ||||
| Pragmatics | 91.5 (12.2) | 6. Having to take time off work. | 86.7 (23.2) | r2=0.10 p=0.69 |
| 9. The cost of health care. | 80 (29.8) | r2=0.17 p=0.045* |
||
Caregiver-reported speech and appearance outcomes
The mean score on the CEP was 2.58 (SD 0.94), with lower scores indicating better caregiver-reported outcomes. The mean speech/hearing score was 2.20 (SD 1.16), and the mean aesthetic score was 2.70 (SD 1.0). Multivariable analysis was used to describe the relationship between caregiver-reported outcomes and barriers to care, adjusting for the presence of siblings, education level, income, cleft type, and payer type. After adjusting for these factors, total BCQ scores remained significantly negatively associated with CEP scores (r2=0.19, p=0.024), indicating that fewer barriers to care were associated with improved caregiver outcomes as measured by the CEP (Table 3). Skills (r2=0.17, p=0.037), Expectations (r2=0.17, p=0.045), and Pragmatics (r2=0.18, p=0.026) remained negatively associated with mean CEP scores. The two lowest scoring questions from these three subscales were then determined. Of these (Table 2), the question addressing lack of communication between parts of the healthcare system and the question addressing cost of health care were both significantly correlated with lower mean CEP scores (r2=0.23, p=0.005; r2=0.17, p=0.045, respectively). “Knowing how to make the healthcare system work for you” approached but did not reach statistical significance (r2=0.16, p=0.067)(Table 2). Collinearity was not detected between any covariates and BCQ scores.
Table 3.
Impact of Barriers to Care scores on outcomes as measured by the CEP, controlling for education, income, siblings, cleft type, and payer.
| R2 | Correlation coefficient | p value | |
|---|---|---|---|
| Mean BCQ score | 0.19 | −0.041 | 0.024* |
| Mean skills score | 0.17 | −0.030 | 0.037* |
| Mean marginalization score | 0.14 | −0.034 | 0.118 |
| Mean expectations score | 0.17 | −0.027 | 0.045* |
| Mean knowledge/beliefs score | 0.14 | −0.053 | 0.120 |
| Mean pragmatics score | 0.18 | −0.027 | 0.026* |
Using the same regression model, no significant relationship was found between BCQ scores and mean speech/hearing scores (Table 4). However, total BCQ scores were negatively associated with mean aesthetic scores (r2=0.19, p=0.025). Furthermore, Skills (r2=0.17, p=0.040), Expectations (r2=0.17, p=0.039), and Pragmatics (r2=0.18, p=0.034) scores were also negatively associated with aesthetic scores.
Table 4.
Impact of Barriers to Care scores on speech/hearing and aesthetic scores as measured by the CEP, controlling for education, income, siblings, cleft type, and payer.
| Speech/Hearing | Aesthetic | |||||
|---|---|---|---|---|---|---|
| R2 | Correlation Coeff | P value | R2 | Correlation Coeff | P value | |
| Mean BCQ score | 0.11 | −0.034 | 0.145 | 0.19 | −0.043 | 0.025* |
| Mean skills score | 0.11 | −0.026 | 0.156 | 0.17 | −0.032 | 0.040* |
| Mean marginalization score | 0.08 | −0.19 | 0.499 | 0.15 | −0.039 | 0.090 |
| Mean expectations score | 0.09 | −0.020 | 0.255 | 0.17 | −0.030 | 0.039* |
| Mean knowledge/beliefs score | 0.10 | −0.57 | 0.181 | 0.13 | −0.051 | 0.157 |
| Mean pragmatics score | 0.12 | −0.26 | 0.091 | 0.18 | −0.027 | 0.034* |
Desire for Revision
Of the 60 surveyed caregivers, 39 expressed an interest in revision (63.9%). These caregivers reported increased barriers to care, with corresponding lower BCQ scores (p=0.01), and higher CEP scores (p=0.047) than parents who were not interested in revision (Table 5). On logistic regression, the odds of expressing desire for revision decreased by 21.2% with each additional point on the BCQ (fewer barriers), after controlling for cleft type, presence of siblings, income, and education. Additionally, patients with higher levels of education were more likely to express interest in revision (OR 11.23, p=0.042) (Table 6).
Table 5.
BCQ and CEP scores by caregiver interest in revision surgery.
| Caregivers Not Desiring Revision | Caregivers Desiring Revision | ||
|---|---|---|---|
| Mean BCQ Score | 98.7 (3.26) | 93.5 (8.78) | 0.01* |
| Mean CEP Score | 2.25 (1.11) | 2.75 (0.80) | 0.050* |
Table 6.
Logistic regression results for caregiver interest in revision surgery.
| Odds ratio (OR) | Confidence Intervals (CI) | P value | |
|---|---|---|---|
|
| |||
| Mean BCQ score | 0.79 | 0.64–0.97 | 0.021* |
|
| |||
| Cleft Type (reference: lip only) | |||
| Lip/palate | 0.52 | 0.5–5.91 | 0.60 |
| Palate only | 0.33 | 0.02–6.24 | 0.46 |
|
| |||
| Siblings | 2.13 | 0.34–13.3 | 0.42 |
|
| |||
| Income (reference: <$60K) | |||
| $60K–$100K | 0.26 | 0.04–1.90 | 0.18 |
| >$100K | 0.48 | 0.08–2.93 | 0.42 |
|
| |||
| Education (reference: high school or less) | |||
| Some college or more | 11.23 | 1.09–116.18 | 0.042* |
DISCUSSION
In this cohort of patients with CLCP, a significant burden of care was observed for cleft patients and their families, and these barriers influenced caregiver-reported appearance outcomes. BCQ scores were higher in our CLCP sample compared with other groups of Children with Special Health Care Needs [28], likely attributable to team-based coordination of cleft care, which has become the standard of care in the United States [29]. Still, 60% of caregivers in this clinic still indicated some type of barrier to obtaining care for their child, even though a large percentage of our population of caregivers indicated high levels of education and earnings well above the median household income. Additionally, parents who perceived more barriers to care reported worse outcomes, and more specifically, poorer aesthetic outcomes. Difficulties navigating the healthcare system, poor communication, and cost of care were most closely associated with poorer scores on the CEP. Finally, caregivers with greater perceived barriers to care more frequently expressed desire for revision.
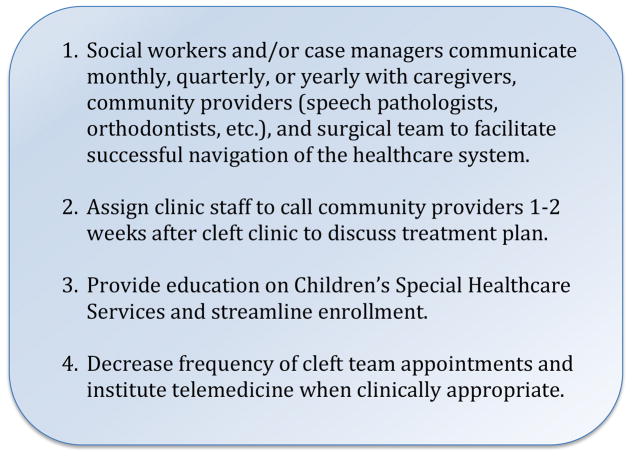
Navigating the health care system can be challenging for anyone, let alone Children with Special Healthcare Needs. Moreover, coordination of care for children with CLCP typically occurs across patients, caregivers, physicians, nurses, social workers, speech pathologists, orthodontists, school administration, and neuropsychologists. Even in a single payer system, parents of children with CLCP in the U.K. reported unmet needs with regard to care coordination and information delivery [30]. Consequences of poor coordination include wasted resources, delays in diagnosis and treatment, and reduced quality of delivered care, as well as decreased patient satisfaction [31], all of which support the results of this study. Additionally, if patients receive components of their care in different health systems, information regarding diagnoses and care received is contained within different electronic medical records, essentially placing key data in silos, rendering communication difficult for clinicians [32]. In circumstances of fragmented care, coordination of care is ultimately left to the caregiver. Despite providing a multidisciplinary team approach, many patients with CLCP receive speech therapy in their schools, undergo orthodontic and dental treatment in their communities, or have Individual Education Plans (IEPs) not routinely communicated to the neuropsychologists. In the future, utilizing social workers or care managers who communicate regularly with both caregivers and providers could help families successfully navigate the complexities of cleft care [33] (Figure 1).
Figure 1.
Recommendations for decreasing barriers to care in the CLCP population.
Communication between providers and various aspects of the health care system was also identified as a significant barrier in our cohort. In a qualitative study of inter-facility transfers, parents of Children with Special Healthcare Needs felt that communication from physicians could be significantly improved [34]. Key community stakeholders caring for Children with Special Healthcare Needs in Arizona similarly identified communication and family education as vital for improving care coordination [35]. Communication issues specific to cleft and craniofacial teams have been studied since 1957 [36], and the efforts to improve communication and decrease care fragmentation have resulted in the development of multidisciplinary teams [37]. Facilitating multispecialty care in a single day of appointments significantly reduces care burden for these families [38]. After a day of cleft clinic, all providers involved in the care of these children meet for two hours to discuss specialty-specific recommendations and finalize a plan of care. If aspects of care are conducted elsewhere, a letter summarizing recommendations is mailed to those providers. This may be the critical point at which communication breaks down, causing caregivers to perceive poor communication between providers. Instituting closed-loop communication wherein staff at our multidisciplinary clinic contact outside providers one to two weeks later to verify receipt of our recommendations may prevent communication problems where they are most likely to occur.
Finally, the cost of orofacial cleft care is substantial, with the lifetime cost approaching $700 million [39]. While most cleft-related care is “covered,” there are a significant number of patients attending cleft team who cannot purchase Children’s Special Health Care Services secondary to the cost. Fortunately, this fee is waived if the child is covered by Medicaid or lives in a foster home [40]. If caregivers cannot pay the fee, the caregivers’ private insurance will cover treatment, but some plans are characterized by high deductibles and increased cost sharing. Additionally, time off work is a major indirect cost sustained by families and society at large and is routinely considered in cost-effectiveness analyses [41]. In the future, improving access to and enrollment in Children’s Special Health Care Services could significantly decrease out-of-pocket costs for families, and instituting telemedicine appointments when clinically appropriate could diminish the loss of income and productivity caused by time taken off work. Furthermore, low-risk patients, such as those with isolated soft palate clefts, could potentially be seen every other year rather than annually, which would serve to reduce indirect costs for families.
Furthermore, barriers to care negatively impacted CROs. While barriers to implementation of PRO measures have been studied [42,43], there is surprisingly little data regarding the impact of barriers to care on PROs. For example, increased medication adherence improved health-related quality of life (HRQOL) in sickle cell patients [44], and access issues similarly correlated with HRQOL in neurology patients [20]. Improved coordination of care scores were also associated with improved PROs in a pancreatic cancer population [21].
Finally, caregivers with lower scores on the BCQ, and hence greater perceived barriers, demonstrated increasing odds of expressing interest in revision surgery for their child. It is possible that some caregivers may desire revision because specific access issues have prevented revision surgery in the past. These same caregivers had higher scores on the CEP, indicating poorer outcomes, compared with caregivers uninterested in revision. As such, their perception of outcomes may also influence their interest in additional surgery, even if they had sufficient access in the past. Surprisingly, caregivers with greater levels of education had greater odds of desiring revision, which may reflect the demographics of the community in which the authors practice. While the relationship between perceived barriers and interest in revision is likely complex, it remains critical for cleft surgeons to address these barriers, as caregivers’ opinions and preferences profoundly impact self-perception and adjustment in children [22].
Our study had several limitations. First, this study was conducted at a single academic center, and our findings may not be generalizable to patients and families in other areas. Additionally, our population was relatively advantaged with respect to sociodemographic attributes, including income and education. It is likely that perceived barriers would be increased in cleft populations with lower incomes and less education, and thus the relationship between barriers and outcomes may be more pronounced. As the primary focus was on the differences between barriers and PROs, our study may have been underpowered to detect more nuanced relationships between CEP scores and other covariates, such as income, education, and payer. Additionally, given the phrasing of the BCQ items, the extent to which barriers correspond to missed appointments or delays in diagnosis or surgery could not be captured. Adapting these questions to include concrete data points or developing a new instrument would serve to further our understanding of the relationship between perceived barriers and care utilization. Finally, while the CEP has shown internal consistency among parents [18], initial validation occurred in 1997 [27], and thus the CEP may merit repeated validation studies in both caregiver and patient populations.
CONCLUSIONS
Access to quality health care remains inequitable in the United States, and parents of our CLCP patient population perceived significant barriers related to health care system navigation, communication, and cost. These perceived barriers were correlated with poorer CROs as measured by the CEP and an increased interest in revision surgery. To reduce barriers, we recommend that cleft teams utilize care managers to enable successful navigation of the health care system, institute closed-loop communication between clinic staff and outside providers, improve enrollment in Children’s Special Health Care Services, and substitute telemedicine for clinic appointments when appropriate.
Footnotes
This paper has not been presented at any meetings.
Author contributions:
KGB conceptualized the study, implemented the instrument, performed the statistical analysis, and wrote the first draft of the manuscript. AKP and MKB assisted in implementation of the instrument and review of the manuscript. KR, CJV, SJK, and SRB assisted with review of the manuscript. JFW assisted with study design, analysis, and multiple reviews of the manuscript.
No other financial relationships to disclose.
Financial Disclosure Statement: Katelyn G. Bennett is currently supported by the National Institute of Dental and Craniofacial Research (1F32DE027604-01).
References
- 1.Lopreiato JO, Ottolini MC. Assessment of immunization compliance among children in the Department of Defense health care system. Pediatrics. 1996;97(3):308–11. [PubMed] [Google Scholar]
- 2.Levey LM, Curry JP, Levey S. Rural-urban differences in access to Iowa child health services. J Rural Health. 1988;4(2):59–72. doi: 10.1111/j.1748-0361.1988.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 3.Dinkevich EI, Cunningham SJ, Crain EF. Parental perceptions of access to care and quality of care for inner-city children with asthma. J Asthma. 1998;35(1):63–71. doi: 10.3109/02770909809055406. [DOI] [PubMed] [Google Scholar]
- 4.Davidson AE, et al. Access to care among children visiting the emergency room with acute exacerbations of asthma. Ann Allergy. 1994;72(5):469–73. [PubMed] [Google Scholar]
- 5.Ponsky TA, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292(16):1977–82. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 6.McPherson M, et al. A new definition of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):137–40. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 7.Hooshmand M, Yao K. Challenges Facing Children with Special Healthcare Needs and Their Families: Telemedicine as a Bridge to Care. Telemed J E Health. 2017;23(1):18–24. doi: 10.1089/tmj.2016.0055. [DOI] [PubMed] [Google Scholar]
- 8.Glickman SW, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007;297(21):2373–80. doi: 10.1001/jama.297.21.2373. [DOI] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198(4):626–32. doi: 10.1016/j.jamcollsurg.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Polverini AC, et al. Time to Treatment: Measuring Quality Breast Cancer Care. Ann Surg Oncol. 2016;23(10):3392–402. doi: 10.1245/s10434-016-5486-7. [DOI] [PubMed] [Google Scholar]
- 11.Basch E. Patient-Reported Outcomes - Harnessing Patients’ Voices to Improve Clinical Care. N Engl J Med. 2017;376(2):105–108. doi: 10.1056/NEJMp1611252. [DOI] [PubMed] [Google Scholar]
- 12.Brundage M, et al. Patient-reported outcomes in randomized clinical trials: development of ISOQOL reporting standards. Qual Life Res. 2013;22(6):1161–75. doi: 10.1007/s11136-012-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Squitieri L, Bozic KJ, Pusic AL. The Role of Patient-Reported Outcome Measures in Value-Based Payment Reform. Value Health. 2017;20(6):834–836. doi: 10.1016/j.jval.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pusic AL, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345–53. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 15.Patrick DL, et al. Measuring the quality of life of youth with facial differences. Cleft Palate Craniofac J. 2007;44(5):538–47. doi: 10.1597/06-072.1. [DOI] [PubMed] [Google Scholar]
- 16.Monson LA, et al. Secondary lip and palate surgery. Clin Plast Surg. 2014;41(2):301–9. doi: 10.1016/j.cps.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Oosterkamp BC, et al. Satisfaction with treatment outcome in bilateral cleft lip and palate patients. Int J Oral Maxillofac Surg. 2007;36(10):890–5. doi: 10.1016/j.ijom.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Eckstein DA, et al. Measuring quality of life in cleft lip and palate patients: currently available patient-reported outcomes measures. Plast Reconstr Surg. 2011;128(5):518e–526e. doi: 10.1097/PRS.0b013e31822b6a67. [DOI] [PubMed] [Google Scholar]
- 19.Crerand CE, et al. Body Image and Quality of Life in Adolescents With Craniofacial Conditions. Cleft Palate Craniofac J. 2017;54(1):2–12. doi: 10.1597/15-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai JS, et al. An Item Bank to Measure Systems, Services, and Policies: Environmental Factors Affecting People With Disabilities. Arch Phys Med Rehabil. 2016;97(12):2102–2112. doi: 10.1016/j.apmr.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Beesley VL, et al. Association between pancreatic cancer patients’ perception of their care coordination and patient-reported and survival outcomes. Palliat Support Care. 2017:1–10. doi: 10.1017/S1478951517000608. [DOI] [PubMed] [Google Scholar]
- 22.Sischo L, Wilson-Genderson M, Broder HL. Quality-of-Life in Children with Orofacial Clefts and Caregiver Well-being. J Dent Res. 2017;96(13):1474–1481. doi: 10.1177/0022034517725707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noor SN, Musa S. Assessment of patients’ level of satisfaction with cleft treatment using the Cleft Evaluation Profile. Cleft Palate Craniofac J. 2007;44(3):292–303. doi: 10.1597/05-151. [DOI] [PubMed] [Google Scholar]
- 24.Gatti GL, et al. Cleft Lip and Palate Repair. J Craniofac Surg. 2017;28(8):1918–1924. doi: 10.1097/SCS.0000000000003820. [DOI] [PubMed] [Google Scholar]
- 25.Ha P, Li C, Shi B. Parent satisfaction with primary repair of paediatric cleft lip in Southwest China. Int J Oral Maxillofac Surg. 2017;46(3):281–285. doi: 10.1016/j.ijom.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 26.Feragen KB, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 10. Parental perceptions of appearance and treatment outcomes in their 5-year-old child. J Plast Surg Hand Surg. 2017;51(1):81–87. doi: 10.1080/2000656X.2016.1254642. [DOI] [PubMed] [Google Scholar]
- 27.Turner SR, Thomas PW, Dowell T, Rumsey N, Sandy JR. Psychological outcomes amongst cleft patients and their families. Br J Plast Surg. 1997 Jan;50(1):1–9. doi: 10.1016/s0007-1226(97)91275-3. [DOI] [PubMed] [Google Scholar]
- 28.Seid M, et al. Parents’ reports of barriers to care for children with special health care needs: development and validation of the barriers to care questionnaire. Ambul Pediatr. 2004;4(4):323–31. doi: 10.1367/A03-198R.1. [DOI] [PubMed] [Google Scholar]
- 29.Thomas PC. Multidisciplinary care of the child born with cleft lip and palate. ORL Head Neck Nurs. 2000;18(4):6–16. [PubMed] [Google Scholar]
- 30.Nelson PA, Kirk SA. Parents’ Perspectives of Cleft Lip and/or Palate Services: A Qualitative Interview. Cleft Palate Craniofac J. 2013;50(3):275–85. doi: 10.1597/11-293. [DOI] [PubMed] [Google Scholar]
- 31.Bodenheimer T. Coordinating care--a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064–71. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 32.Ranade-Kharkar P, et al. Information needs of physicians, care coordinators, and families to support care coordination of children and youth with special health care needs (CYSHCN) J Am Med Inform Assoc. 2017;24(5):933–941. doi: 10.1093/jamia/ocx023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller K. Care coordination impacts on access to care for children with special health care needs enrolled in Medicaid and CHIP. Matern Child Health J. 2014;18(4):864–72. doi: 10.1007/s10995-013-1312-z. [DOI] [PubMed] [Google Scholar]
- 34.Rosenthal JL, et al. Familial Caregiver and Physician Perceptions of the Family-Physician Interactions During Interfacility Transfers. Hosp Pediatr. 2017;7(6):344–351. doi: 10.1542/hpeds.2017-0017. [DOI] [PubMed] [Google Scholar]
- 35.Lyles AA, et al. Stakeholders’ Perceptions of Care Coordination: A Participatory Process. J Pediatr Health Care. 2017;31(5):555–559. doi: 10.1016/j.pedhc.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 36.Lillywhite H. Communication problems in the cleft palate rehabilitation team. Cleft Palate Bull. 1957;7:8–10. [Google Scholar]
- 37.Strauss RP. The organization and delivery of craniofacial health services: the state of the art. Cleft Palate Craniofac J. 1999;36(3):189–95. doi: 10.1597/1545-1569_1999_036_0189_toadoc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 38.Robin NH, et al. The multidisciplinary evaluation and management of cleft lip and palate. South Med J. 2006;99(10):1111–20. doi: 10.1097/01.smj.0000209093.78617.3a. [DOI] [PubMed] [Google Scholar]
- 39.Albert MG, et al. Inpatient versus outpatient cleft lip repair and alveolar bone grafting: a cost analysis. Ann Plast Surg. 2014;73(Suppl 2):S126–9. doi: 10.1097/SAP.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 40. [Accessed November 21, 2017];General Information for Families About “Children’s Special Health care Services”. Available at: (CSHCS). http://www.michigan.gov/mdhhs/0,5885,7-339-71547_35698-15087--,00.html.
- 41.Black WC, et al. Cost-effectiveness of CT screening in the National Lung Screening Trial. N Engl J Med. 2014;371(19):1793–802. doi: 10.1056/NEJMoa1312547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Basch E, Snyder C. Overcoming barriers to integrating patient-reported outcomes in clinical practice and electronic health records. Ann Oncol. 2017;28(10):2332–2333. doi: 10.1093/annonc/mdx506. [DOI] [PubMed] [Google Scholar]
- 43.Hartkopf AD, et al. Electronic-Based Patient-Reported Outcomes: Willingness, Needs, and Barriers in Adjuvant and Metastatic Breast Cancer Patients. JMIR Cancer. 2017;3(2):e11. doi: 10.2196/cancer.6996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Badawy SM, et al. Adherence to hydroxyurea, health-related quality of life domains, and patients’ perceptions of sickle cell disease and hydroxyurea: a cross-sectional study in adolescents and young adults. Health Qual Life Outcomes. 2017;15(1):136. doi: 10.1186/s12955-017-0713-x. [DOI] [PMC free article] [PubMed] [Google Scholar]