Abstract
BACKGROUND:
The contaminated hands of health-care professionals (HCPs) is an implicated vector in the transmission of potentially pathogenic organisms to vulnerable patients. The aim of this study was to derive baseline data on hand hygiene (HH) practices among a cohort of students at the Lagos State School of Nursing and to determine their perception about the adequacy of instructions they receive.
MATERIALS AND METHODS:
A descriptive, cross-sectional study was conducted on a probability random sample of 69 nursing students at the Lagos State School of Nursing at the Alimosho Igando General Hospital. The knowledge, attitude, and practice as well as the perception of the respondents on the adequacy of their infection control instructions were obtained using an interviewer-administered questionnaire. Data entry and analysis were done using SPSS software version 20 (IBM Corp., Armonk, NY, USA), P < 0.05 was considered statistically significant. Multivariate linear and logistic regressions were done to assess which factors were truly significant predictors, with odds ratios (ORs) and 95% confidence intervals (CIs) specified as the measures of association between predictors and outcome variables.
RESULTS:
Majority of participants were ≤20 years old (50.7%, n = 35) and were in their second year of study (44.9%, n = 31). Participants were least knowledgeable about the importance of discarding gloves and not washing or reusing them (16 [23.1%]). The mean score on the Hand Hygiene Beliefs Scale was 86.2 ± 9.0, with scores ranging from 23 to 88 out of a possible high score of 115. The most positive health beliefs were associated with being a role model for HH (3.57 ± 0.52), while the worst was associated with imitating bad HH practices performed by senior colleagues (1.29 ± 1.20). Caring for a wound (60 [87.0%]) was most associated with the need for HH, while demonstration and clinical practice were rated as the most effective teaching methods. Results of the multivariate logistic regression analysis, with the outcome variable of good self-reported HH practices, revealed that the odds of appropriate behavior were higher if the student nurses were in their third year of study (OR = 1.59; 95% CI: 1.01–2.45). An appropriate behavior was also more likely in student nurses with a higher risk perception (OR = 1.54; 95% CI: 1.03–2.51).
CONCLUSION:
Despite the overwhelming evidence that HH is effective in the prevention of hospital-acquired infections, its performance among HCPs remains far less than optimal. Since students will someday be influencing future HH compliance behaviors of other health-care workers, the importance of HH should be adequately incorporated into their school curriculum.
Keywords: Hand hygiene, nosocomial infections, nursing students
Introduction
Healthcare-associated infections (HAIs) are those that become apparent while patients are being treated within health-care institutions, in whom the infection was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility.[1] Primarily, patients bear the burden of morbidity, mortality, and prolonged hospitalization associated with HAIs, and it is projected that there are over 1.4 million people worldwide with infections acquired in hospitals at any period of time.[2,3] The prevention of infection requires a multifaceted strategy. Infectious agents can be transmitted to a susceptible host by a host of methods such as carriage on equipment, through airflow, and direct spread on the hands of health-care workers. The contaminated hands of health-care workers is an implicated vector in the transmission of potentially pathogenic organisms to vulnerable patients;[4] hence, such transmissions are preventable. Hand hygiene (HH) is a proven method to reduce the incidence of HAIs.
HH is a comprehensive term that includes hand washing which involves removing soil and transient microorganisms from the hands using soap and water and hand antisepsis which entails the removal or elimination of microorganisms from the hands with an antiseptic agent, in the form of an alcohol-based hand rub or an antiseptic soap. HH also includes the care of the fingernails. Adherence to HH recommendations is the single most important practice for preventing the transmission of microorganisms in health care, which directly contributes to patient safety.[5] A number of studies have showed a positive effect of improved HH on nosocomial infection rates[6,7] as well as transmission risks in day-care centers, schools, and community settings.[8]
Nonetheless, in spite of CDC guidelines that recognize HH as the most significant process in the prevention of nosocomial infection,[9] an unacceptable compliance rate is still observed among health-care professionals (HCPs).[10] Nigeria is one of the countries with a high burden of HCAIs,[11,12] yet the HH campaign is not commonly promoted in many health-care facilities in the country. Some researchers have shown that adherence of HCPs to guidelines for HH is very low, generally <50%.[13,14] Many HCPs are not aware of the standard procedures involved in HH, and appropriate facilities for optimal infection control are also often lacking, including reasonably simple measures such as provision of water, soap, and clean paper towels to regularly wash hands between patient contacts.[15] Other factors perceived as contributing to poor HH compliance include unavailability of hand washing sinks, time required to perform HH, patient's condition, effect of HH products on the skin, and insufficient knowledge of the guidelines.[16,17] In addition, some authors opine that role models, group behavior, and the level of managerial support influence the reported levels of compliance.[17]
Nurses are a very strategic subset of health workers and they are more likely to have more frequent contact with patients than other HCPs. The provision of patient hygiene is one of the most regularly performed nursing care activities, making them frequently exposed to blood and other bodily fluids of the patient. The recent Ebola outbreak in Nigeria amplifies this reality as it was observed that the first Nigerian victim, who eventually died was a nurse. Health workers' education is a key strategy in the reduction of HAIs through infection prevention and control programs. Some researchers have highlighted the inadequacy of many undergraduate programs to effectively train students of various clinical disciplines,[18,19] possibly indicating a causal link between undergraduate education and the lack of compliance with infection control guidelines.
The aim of this study was thus to derive baseline data on HH practices among a cohort of students in the Lagos State School of Nursing and to determine their perception about the adequacy of instructions they receive. The information derived from this research will provide the basis for recommendations for the modification of the standard precautious component of their training with a view to significantly improve their compliance with hospital infection control guidelines.
Materials and Methods
Research design
A descriptive, cross-sectional study was conducted on a probability random sample of 69 consenting participants recruited from a pool of 120 undergraduate nursing students registered in years 1, 2, and 3 in the School of Nursing of the Alimosho Igando General Hospital of Lagos State.
Ethical considerations
The protocol for the study was submitted to the Hospital's Health Research and Ethics Committee and written approval was obtained (HREC. 10/06/277). In addition, the departmental heads of the nursing and midwifery School of Nursing were contacted, and access to their nursing students was requested. Eighty students were recruited, but only 69 agreed to participate in the anonymous survey. Participation was voluntary, and the students were assured that their responses will be kept confidential. Written informed consent was also obtained from all the participants.
Study setting
This study was conducted from August to September 2015 at the Lagos State School of Nursing located within the premises of the Alimosho Igando General Hospital, which is a multispecialty hospital serving the most populated local government area with a population of 1.28 million people. It is also a referral center for the environs and it provides services in community health; surgery; obstetrics and gynecology; pediatrics; ophthalmology; hematology; and dental and medical services. It has approximately 450 staff members inclusive of 29 administrative/clerical, 144 nurses, and 71 medical doctors. The Lagos State School of Nursing is located in the premises of the hospital. The participants in this study were years 1, 2, and 3 in the School of Nursing of the Alimosho Igando General Hospital of Lagos State. The students were surveyed at their school during their off-clinic hours.
Sample selection
From a reference study with a knowledge prevalence of 59.8%,[20] the estimated sample size of 189 was computed using an equation for descriptive studies. A total of 69 students were however enlisted for this pilot study due to the low student population in the nursing school. A multistage sampling method was utilized with stratification of the students into the three levels at the first stage and simple random sampling at the second stage using the nominal roll of students as the sampling frame.
Data collection
A self-administered questionnaire was used for data collection. The first section of the questionnaire obtained the examined sociodemographic characteristics of the study participants, while the second segment utilized the modified Hand Hygiene questionnaire which had ten multiple-choice questions that assessed basic HH knowledge; 13 Likert scale inquiries that assessed the students' opinions of the effectiveness of various teaching methods about HH; 23 Likert scale questions which assessed students' attitude and health belief about HH; and 14 Likert scale questions on the students' practices of HH. Each correct knowledge score obtained 1 mark, while each wrong response had a score of 0. Scores on individual items in the Likert scale ranged from 1 to 5.
Data collection procedure
On approval of the study by the relevant authorities, written consent was obtained from all the enlisted participants after explaining to them that their participation is voluntary and that their responses will be kept confidential. Self-administered questionnaires were then given to participants during their off-clinic hours. The questionnaires had clear instructions on how to fill the multiple response segment as well as the Likert-like questions while the students were encouraged to seek further clarification where necessary. Each filled questionnaire was checked to ensure that it was completed in its entirety, and gratitude was expressed to the participants.
Data analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 20 (IBM Corp., Armonk, NY, USA). Data were normally distributed as assessed by the Shapiro–Wilk test. Results were presented as percentages and frequencies, using charts and tables including univariate analysis. Bivariate analysis was done to measure the association between dependent and independent variables. The maximum obtainable knowledge, attitude, and practice scores were 10, 115, and 70, respectively. Knowledge scores were dichotomized as 0–3 for poor; 3.1–7 for fair; and >7 for good. Attitude and practice scores were categorized as poor or good based on scores above or below the mean scores of 86.2 ± 9.0 and 57.1 ± 6.4, respectively, while individual mean scores for each question were also obtained. The Chi-square test was used to determine the level of association between categorical variables. The Student's paired t-tests and ANOVA tests were used to compare means to determine the level of association between the variables. Multivariate linear and logistic regressions were done to assess which factors were truly significant predictors, with odds ratios (ORs) and 95% confidence intervals (CIs) specified as the measures of association between predictors and outcome variables. A 95% CI and P < 0.05 (two tailed) were considered statistically significant.
Results
Description of demographic characteristics of participants
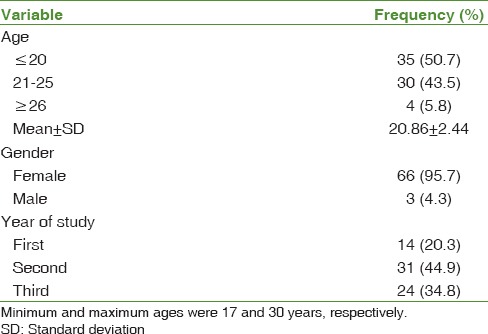
The total number of participants recruited for this study were 69, of which 95.7% (n = 66) were female and 4.3% (n = 3) were male. The majority of participants were ≤20 years old (50.7%, n = 35). Majority of the respondents (44.9%, n = 31) were in their second year of study [Table 1].
Table 1.
Demographic characteristics of the study participants
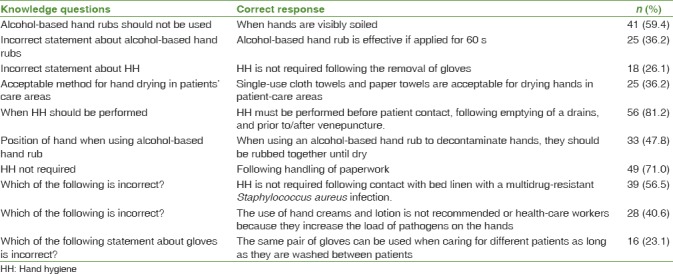
The HH knowledge was evaluated with ten multiple-choice questions. Scores on the questionnaire were presented as a percentage of correct answers. The combined scores on the ten questions ranged from 2.9% to 81.2%. Participants were most knowledgeable about the performance of HH before patient contact, following emptying of a drain, and prior to/after venepuncture. They were least knowledgeable about the importance of discarding gloves and not washing or reusing them (16 [23.1%]) [Table 2].
Table 2.
Frequency and percentage of correct answers to knowledge questions
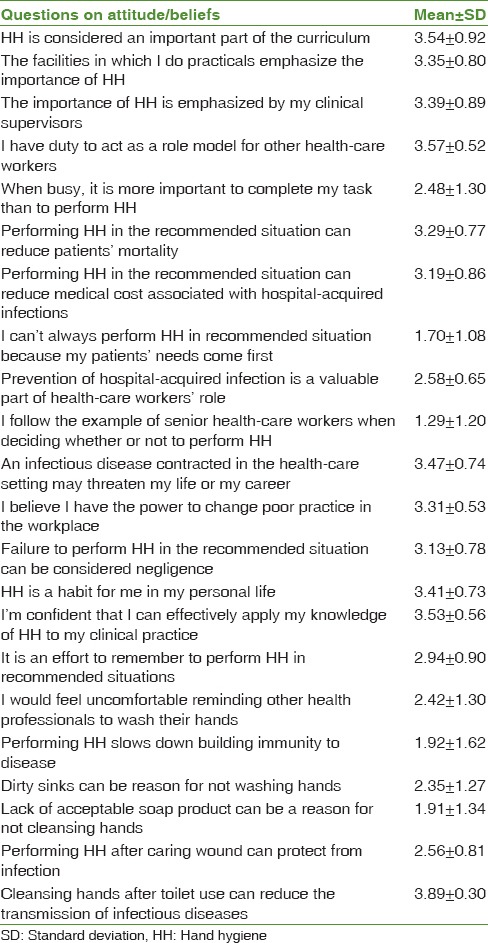
The mean score on the Hand Hygiene Beliefs Scale was 86.2 ± 9.0, with scores ranging from 23 to 88 out of a possible high score of 115; higher scores were associated with more positive health beliefs. Scores on individual items in the scale ranged from 1 to 5. The most positive health beliefs were associated with being a role model for HH (3.57 ± 0.52); having HH emphasized by supervisors (3.57 ± 0.52); and having it in the curriculum (3.54 ± 0.92), while the worst was associated with imitating bad HH practices performed by senior colleague (1.29 ± 1.20) [Table 3].
Table 3.
Attitude/positive beliefs of respondents about hand hygiene
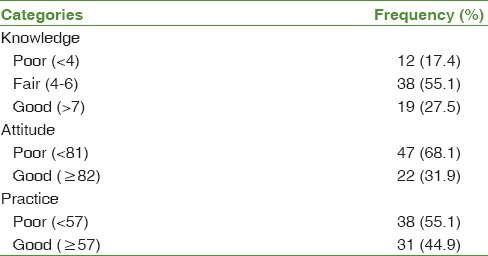
The frequency that participants reported performing HH is presented in percentages. The scores ranging from 23.2% to 81.2% and a score of 100% signify that HH is always performed on every indication. Caring for a wound (60 [87.0%] participants with mean (MN) ± standard deviation (SD) = 3.81 ± 0.58) was associated mostly with the performance of HH, while before coming in contact with a patient was least perceived to require HH (16 [23.2] participants with MN ± SD = 1.59 ± 1.06) [Table 4]. Overall, 27.5% of the respondents had good knowledge, while 31.9% and 44.9% had good practices [Table 5].
Table 4.
Self-reported hand hygiene practices of respondents
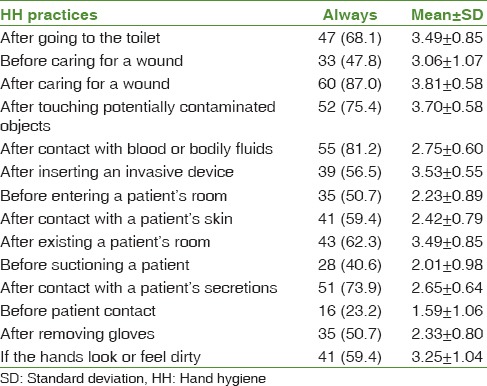
Table 5.
Knowledge, attitude, and practice of respondents about hand hygiene
The teaching methods that participants rated as the most effective were demonstration and clinical practice with mean scores of 3.47 ± 0.68 and 3.41 ± 0.63, respectively, out of a possible score of 5. The lowest rated methods included research articles, websites, computer simulations, and videos, with more than half of the participants rating each as mildly effective or not effective [Table 6].
Table 6.
Perceived effectiveness of hand hygiene teaching methods
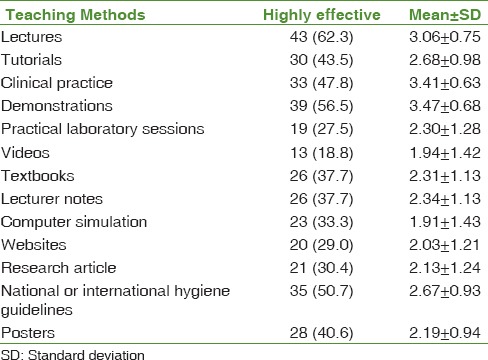
Table 7 displays the results of the multivariate logistic and linear regression models. Student nurses in their 3rd year of study (OR = 1.64; 95% CI: 1.15–3.02), those with a higher risk perception (OR = 1.35; 95% CI: 0.82–2.06), and those who perceived the HH teaching methods they received as effective (OR = 1.24; 95% CI: 0.81–2.01) had better knowledge about HH (Model 1).
Table 7.
Multivariate logistic (1 and 3) and linear (2) regression model results
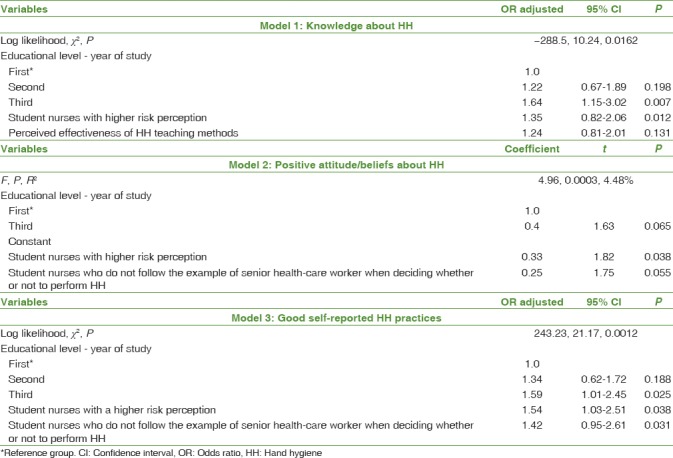
The results of the linear regression model showed that third-year student nurses, student nurses with a higher risk perception, and those who do not follow the example of senior health-care worker when deciding whether or not to perform HH had significantly more positive attitudes about HH (Model 2).
Results of the multivariate logistic regression analysis, with the outcome variable of good self-reported HH practices, also revealed that the odds of appropriate behavior were higher if the student nurses were in their third year of study (OR = 1.59; 95% CI: 1.01–2.45). An appropriate behavior was also more likely in student nurses with a higher risk perception (OR = 1.54; 95% CI: 1.03–2.51) (Model 3).
Discussion
Nurses constitute the highest percentage of HCP, and they devote more time to patient care than other HCPs, and hence their compliance with HH recommendations appears to be more critical in the prevention of disease transmission among patients. The total number of participants recruited for this study were 69 and they were mainly females since the profession is mainly populated by the female gender. Participants were most knowledgeable about the performance of HH before patient contact, following emptying of a drain, and prior to/after venepuncture. They were however least knowledgeable about the importance of discarding gloves and not washing or reusing them. Failure to replace or discard contaminated gloves, the erroneous belief that glove use negates the need for HH, and the failure of HCPs to implement HH prior to and after glove use are factors that have been previously reported as affecting HH compliance.[21] A previous descriptive study of HCPs revealed that the failure to change or remove contaminated gloves was a major factor resulting in poor HH compliance and high risk for microbial transmission.[22] The practice of using gloves, but not replacing them after contamination, increases the possibility of cross-transmission of pathogens and increased risk of HAIs.[23]
Concerning the attitude of the participants, the most positive health beliefs were associated with being a role model for HH and having HH emphasized by supervisors, while the worst was associated with imitating bad HH practices performed by senior colleague. Previous researchers have shown that the influence of poor role modeling negatively influences HH compliance among students and that intention to perform HH among health workers is often influenced by how they perceive the opinions of important role models.[24,25,26] The significance of the role model has been observed and used efficaciously as an fundamental part of campaigns promoting HH in the intensive care setting.[27,28] Seto et al.[24] confirmed that communication of information by opinion leaders was significantly more effective for implementing a new guideline on care than other strategies. Conversely, the perception of being a model to other colleagues was independently associated with better compliance with HH among physicians.[26] These studies thus imply that when opinion leaders become cognizant of their influence, they are more compliant and their commitment may have a positive impact on health-care workers' perceptions and intention to comply with HH.
In our study, caring for a wound and activities that were perceived to present with a higher risk of infection to the health worker were most associated with the performance of HH. Overall, compliance was greater when the perceived risk was apparently higher. In addition, the students had very high compliance for personal HH practices such as using the toilet and when the hand looks or feels dirty. Conversely, HH performance was perceived to be least important before coming in contact with a patient. These findings are in agreement with that by other studies that reveal a low rate of HH before interacting with the patients.[29,30,31] The rates of performance were higher after patient interactions, confirming the suggestions of some authors that health workers' hand washing rates increase when there is perceived risk for their own health.[29,30] This perception was demonstrated in these studies by higher percentages of HH compliance after touching patients than before touching patients and also in high-risk patient contact service centers such as the emergency room, wound dressing/treatment rooms, and labor ward than that it was in medium-risk patient contact centers such as the inpatient wards. The greatest motivating factor for hand washing among the health workers is thus the fear of contracting disease.
Age and gender were not significantly associated with the knowledge and health belief of the study participants associated with hand washing behavior. Third-year respondents were however significantly more likely to have better knowledge, attitude, and HH practices. Exposure of the senior students to more clinical practice may be responsible for this observation. Overall, 27.5% of the respondents had good knowledge, while 31.0% and 44.9% had good practices. These results reveal obvious deficits in the cognitive, affective, and behavioral domains of the respondents with regard to HH. The teaching methods that participants rated as most effective were demonstration and clinical practice, while the lowest rated methods included evidence-based sources such as research articles, websites, computer simulations, and videos, with more than half of the participants rating each as mildly effective or not effective. This result suggests that undergraduate education of the students on transmission-based precautions may be inadequate.[32] Some international studies observed that nurses prefer to approach colleagues for information rather than access evidence-based resources.[33,34] The reasons mentioned in the literature for preferring human sources to evidence-based information include convenience, an apparent lack of computer skills, and avoidance of large amounts of retrieved information which has to be read, analyzed, and evaluated.[35]
The recent outbreak of Ebola hemorrhagic fever in Nigeria due to its importation into the country by a Liberian National made these deficiencies obvious even though the public health institutions in the country eventually rose to the occasion. This was after a period of ill preparedness and glaring deficiencies in compliance to standard precaution protocols. The increasing presence of new and evolving pathogens in health-care environments and the effect of clinician education on reducing the spread of HAIs require an urgent review of the present curriculum. While it is important to educate HCPs about the theoretical and practical aspects of HH, it must however be similarly appreciated that inadequate education is not the only barrier to compliance.[36] Provision of materials and equipment for HH such as regular water supply, sinks, waste disposal facilities, alcohol-based hand rubs, and other toiletries are known to be inadequate in resource-constrained environments like Nigeria. It is imperative that these additional barriers to HH practice are eliminated if proper compliance is anticipated.
Literature shows that compliance to standard precaution measures reduces the rate of hospital-acquired infections. Hand washing with clean water and soap and/or use of alcohol-based hand rubs has been recommended by the WHO as a practical infection prevention strategy prior to and after patient contact.[37]
Conclusion
This study demonstrated inadequate HH knowledge, health beliefs, and practices among nursing students. It also showed that they were inadequately exposed to evidence-based information sources. Despite the overwhelming evidence that consistent HH practice is effective in preventing infection and reducing the spread of HAI, HH behavior among HCPs remains far less than optimal.[37] Since students will someday be influencing future HH compliance behaviors of other health-care workers, the importance of HH should be adequately incorporated into their school curriculum. Obvious limitations of the study are the sample size, the single center selected, and the fact that it would have been more effective if compliance with HH was observed rather than obtained with a questionnaire. However, the fact that some of the students were at the preclinical stage of their studies precludes direct observation. These data however provide useful baseline data for further exploratory and intervention studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ducel G, Fabry J, Nicolle L, editors. Prevention of Hospital-Acquired Infections: A Practical Guide. 2nd ed. Geneva, Switzerland: World Health Organization; 2002. [Last assessed on 2017 Mar 03]. Available from: http://www.who.int/iris/handle/10665/67350 . [Google Scholar]
- 2.Vincent JL. Nosocomial infections in adult Intensive-Care Units. Lancet. 2003;361:2068–77. doi: 10.1016/S0140-6736(03)13644-6. [DOI] [PubMed] [Google Scholar]
- 3.Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, et al. Estimating health care-associated infections and deaths in U.S. Hospitals, 2002. Public Health Rep. 2007;122:160–6. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan C. Determinants of Hand Hygiene among Registered Nurses Caring for Critically Ill Infants in the Neonatal Intensive Care Unit. [Last assessed on 2017 Jan 03];Electronic Theses and Dissertations Paper. 2012 221 Available from: http://www.scholar.uwindsor.ca/etd . [Google Scholar]
- 5.Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev. 2004;17:863–93. doi: 10.1128/CMR.17.4.863-893.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hilburn J, Hammond BS, Fendler EJ, Groziak PA. Use of alcohol hand sanitizer as an infection control strategy in an acute care facility. Am J Infect Control. 2003;31:109–16. doi: 10.1067/mic.2003.15. [DOI] [PubMed] [Google Scholar]
- 7.Munoz-Figueroa GP, Ojo O. The effectiveness of alcohol-based gel for hand sanitising in infection control. Br J Nurs. 2018;27:382–8. doi: 10.12968/bjon.2018.27.7.382. [DOI] [PubMed] [Google Scholar]
- 8.Larson E. Skin hygiene and infection prevention: More of the same or different approaches? Clin Infect Dis. 1999;29:1287–94. doi: 10.1086/313468. [DOI] [PubMed] [Google Scholar]
- 9. [Last assessed on 2017 Apr 05];Centres for Disease Control and Prevention. Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. 2002 :1–45. [Google Scholar]
- 10.Campagna M, Maria Mereu N, Mulas L, Pilia R, Francesca Piazza M, Spada L, et al. Pattern of hepatitis A virus epidemiology in nursing students and adherence to preventive measures at two training wards of a university hospital. Hepat Mon. 2016;16:e34219. doi: 10.5812/hepatmon.34219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uneke CJ, Ijeoma PA. The potential for nosocomial infection transmission by white coats used by physicians in Nigeria: Implications for improved patient-safety initiatives. World Health Popul. 2010;11:44–54. doi: 10.12927/whp.2010.21664. [DOI] [PubMed] [Google Scholar]
- 12.Uneke CJ, Ogbonna A, Oyibo PG, Ekuma U. Bacteriological assessment of stethoscopes used by medical students in Nigeria: Implications for nosocomial infection control. World Health Popul. 2008;10:53–61. [PubMed] [Google Scholar]
- 13.Salama MF, Jamal WY, Mousa HA, Al-Abdulghani KA, Rotimi VO. The effect of hand hygiene compliance on hospital-acquired infections in an ICU setting in a Kuwaiti teaching hospital. J Infect Public Health. 2013;6:27–34. doi: 10.1016/j.jiph.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 14.Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection control programme. Lancet. 2000;356:1307–12. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 15.Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients' care. Lancet. 2003;362:1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 16.Chavali S, Menon V, Shukla U. Hand hygiene compliance among healthcare workers in an accredited tertiary care hospital. Indian J Crit Care Med. 2014;18:689–93. doi: 10.4103/0972-5229.142179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teker B, Ogutlu A, Gozdas HT, Ruayercan S, Hacialioglu G, Karabay O, et al. Factors affecting hand hygiene adherence at a private hospital in Turkey. Eurasian J Med. 2015;47:208–12. doi: 10.5152/eurasianjmed.2015.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandijck DM, Labeau SO, De Somere J, Claes B, Blot SI, et al. Executive Board of the Flemish Society of Critical Care Nurses. Undergraduate nursing students' knowledge and perception of infection prevention and control. J Hosp Infect. 2008;68:92–4. doi: 10.1016/j.jhin.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 19.Jennings-Sanders A, Jury L. Assessing methicillin-resistant Staphylococcus aureus knowledge among nursing students. Nurse Educ Today. 2010;30:789–93. doi: 10.1016/j.nedt.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell BG, Say R, Wells A, Wilson F, Cloete L, Matheson L, et al. Australian graduating nurses' knowledge, intentions and beliefs on infection prevention and control: A cross-sectional study. BMC Nurs. 2014;13:43. doi: 10.1186/s12912-014-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harbarth S, Pittet D, Grady L, Goldmann DA. Compliance with hand hygiene practice in pediatric intensive care. Pediatr Crit Care Med. 2001;2:311–4. doi: 10.1097/00130478-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Girou E, Chai SH, Oppein F, Legrand P, Ducellier D, Cizeau F, et al. Misuse of gloves: The foundation for poor compliance with hand hygiene and potential for microbial transmission? J Hosp Infect. 2004;57:162–9. doi: 10.1016/j.jhin.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 23.Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6:641–52. doi: 10.1016/S1473-3099(06)70600-4. [DOI] [PubMed] [Google Scholar]
- 24.Burnett E. Perceptions, attitudes, and behavior towards patient hand hygiene. Am J Infect Control. 2009;37:638–42. doi: 10.1016/j.ajic.2009.04.281. [DOI] [PubMed] [Google Scholar]
- 25.De Wandel D, Maes L, Labeau S, Vereecken C, Blot S. Behavioral determinants of hand hygiene compliance in Intensive Care Units. Am J Crit Care. 2010;19:230–9. doi: 10.4037/ajcc2010892. [DOI] [PubMed] [Google Scholar]
- 26.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV, et al. Hand hygiene among physicians: Performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. doi: 10.7326/0003-4819-141-1-200407060-00008. [DOI] [PubMed] [Google Scholar]
- 27.Harbarth S, Pittet D, Grady L, Zawacki A, Potter-Bynoe G, Samore MH, et al. Interventional study to evaluate the impact of an alcohol-based hand gel in improving hand hygiene compliance. Pediatr Infect Dis J. 2002;21:489–95. doi: 10.1097/00006454-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Gopal Rao G, Jeanes A, Osman M, Aylott C, Green J. Marketing hand hygiene in hospitals – A case study. J Hosp Infect. 2002;50:42–7. doi: 10.1053/jhin.2001.1119. [DOI] [PubMed] [Google Scholar]
- 29.Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Handwashing compliance by health care workers: The impact of introducing an accessible, alcohol-based hand antiseptic. Arch Intern Med. 2000;160:1017–21. doi: 10.1001/archinte.160.7.1017. [DOI] [PubMed] [Google Scholar]
- 30.Lankford MG, Zembower TR, Trick WE, Hacek DM, Noskin GA, Peterson LR, et al. Influence of role models and hospital design on hand hygiene of healthcare workers. Emerg Infect Dis. 2003;9:217–23. doi: 10.3201/eid0902.020249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fadeyi A, Bolaji BO, Oyedepo OO, Adesiyun OO, Adeboye MA, Olanrewaju T, et al. Methicillin resistant Staphylococcus aureus carriage amongst healthcare workers of the critical care units in a Nigerian hospital. Am J Infect Dis. 2010;6:18–23. [Google Scholar]
- 32.Tropea J, Brand C, Roberts C. A National Stakeholder Review of Australian Infection Control Programs: The Scope of Practice of the Infection Control Professional. Sydney: Australian Commission on Safety and Quality in Healthcare; 2008. [Google Scholar]
- 33.Pravikoff DS, Tanner AB, Pierce ST. Readiness of U.S. Nurses for evidence-based practice. Readiness of US Nurses for evidence-based practice. Am J Nurs. 2005;105:40–51. doi: 10.1097/00000446-200509000-00025. [DOI] [PubMed] [Google Scholar]
- 34.O'leary DF, Mhaolrúnaigh SN. Information-seeking behaviour of nurses: Where is information sought and what processes are followed? J Adv Nurs. 2012;68:379–90. doi: 10.1111/j.1365-2648.2011.05750.x. [DOI] [PubMed] [Google Scholar]
- 35.Thompson C, Cullum N, McCaughan D, Sheldon T, Raynor P. Nurses, information use, and clinical decision making – The real world potential for evidence-based decisions in nursing. Evid Based Nurs. 2004;7:68–72. doi: 10.1136/ebn.7.3.68. [DOI] [PubMed] [Google Scholar]
- 36.Ward DJ. The role of education in the prevention and control of infection: A review of the literature. Nurse Educ Today. 2011;31:9–17. doi: 10.1016/j.nedt.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 37.A Guide to the Implementation of the WHO Multimodal Hand Hygiene Improvement Strategy. Geneva: World Health Organization; 2009. World Health Organization. World Health Organization Save lives clean your hands-Guide to Implementation. [Google Scholar]


