Abstract
BACKGROUND:
Due to exhaustive working climate, health-care professionals (HCPs) are highly exposed to emotional strain and work-related stress that leads to burnout syndrome (BOS).
AIM:
We aimed to explore the prevalence of BOS among HCPs and delineate the factors that contribute to developing this emerging threat in HCPs working in Gondar University Hospital (GUH).
METHODS:
A cross-sectional study was conducted among HCPs using a self-administered validated questionnaire containing sociodemographic and job characteristics, symptoms of burnout using Astudillo and Mendinueta questionnaire, and Maslach Burnout Inventory scale. The prevalence of BOS was assessed by summation of answers to all 19 items with a range of 0–57. HCPs who scored >23 were considered as burned out. Pearson's correlation analysis and multivariate logistic regression were used to assess the relationship between BOS and job factors. Data were analyzed using descriptive and inferential statistics.
RESULTS:
A total of 250 HCPs were approached out of which 248 responded (response rate –99.2%). The overall prevalence of burnout was 13.7% and majority of the respondents experienced debility (52.8%), self-criticism (56%), and depressive symptoms (46%). BOS symptoms were significant with age (P = 0.008), number of patients treated per day (P < 0.001), and HCPs working in shifts (P < 0.001). Higher mean levels of emotional exhaustion (5.4 ± 1.2) and inefficacy (5.1 ± 1.7) were noticed than cynicism (4.8 ± 2.0). Male HCPs, being single and years of experience, were determinant factors for all the three dimensions of BOS, whereas profession was significantly determinant for emotional exhaustion (P < 0.01).
CONCLUSION:
The prevalence of BOS among HCPs working in GUH was 13.7%. Being male, unmarried, and years of experience were significant risk factors for all the three dimensions of BOS. Pragmatic measures are recommended to prevent stressful challenges for the physical and mental well-being of the HCPs in GUH.
Keywords: Burnout syndrome, emotional exhaustion, Ethiopia, health-care professionals, Maslach Burnout Inventory, stress
Introduction
The term “Burnout” was coined from the USA in 1970 as a syndrome of emotional exhaustion, cynicism, depersonalization in relationships with workers, and reduced personal accomplishment that can occur in any individuals due to excessive work in stressful conditions.[1] This overwhelming frustration due to workload may sometimes lead to depletion of individual's capacity. Health-care professionals (HCPs) often face these symptoms due to huge patient load, duty rotations, and the night shifts. Practice variability that necessitates to change for better work conditions in resource-limited settings may excavate the underlying factors associated with significant health problems.[2]
The primary responsibility of HCPs is to deliver comprehensive care to patients seeking medical care irrespective of their race, gender, and cultural classes. In addition, HCPs busy lifestyle may pose the risk of physical and emotional stress which may lead to burnout syndrome (BOS). The BOS not only affects physical and mental abilities but also affects the individual's health. Every HCPs shows a particular grade of stress due to workload linked to the job.[3,4] The BOS has been related to impaired job performance and poor health, including headaches, fatigue, sleep disturbances, irritability, marital difficulties, anxiety, depression, hypertension, myocardial infarction,[5,6] and may contribute to alcoholism and drug addiction.
These symptoms of burnout can lead to HCPs medical/medication errors, and these errors can, in turn, contribute to BOS. Dissatisfaction and distress have significant costs, not only for HCPs and their families but also for patients and health-care organizations.[3] For instance, a study conducted in palliative care nurses identified nearly half of them were stressed (48%).[7] Similarly, in Qatar study, 41.2% of the general practitioners experienced the BOS where the majority were young practitioners (<35 years of age). Of note, 50% or more of them were due to professional work stress.[4] Physical stress and emotional alterations at their professional career may impair their conducts that leads to depression and even suicide. This level of stress is much prevalent in doctors working, especially in emergency and oncology wards. A study conducted on physicians working on oncology wards highlighted majority (78%) of the oncologist feel BOS soon after a patient's death, due to failure in their self-esteem, physiological, and emotional stress.[8] Many of the young HCPs feel anxiety in their workplace due to lack of support from the senior colleagues, hostile conditions in the workplace, and lack of organization skills that fairly notable cause for BOS.[4,5] To date, no research was conducted to determine the consequence of burnout on HCPs performance in Northwest Ethiopia. This study would provide baseline information about the consequence of BOS on HCPs in Gondar University Hospital (GUH). We aimed to explore the prevalence of BOS among HCPs and delineate the factors that contribute to developing this emerging threat in Northwest Ethiopian HCPs.
Methods
An institutional-based cross-sectional survey was conducted among all the HCPs working in GUH, Gondar, Northwest Ethiopia were recruited from September to November 2016. GUH is the largely funded multidisciplinary specialized teaching referral hospital with a bed capacity of 550, serving >500,000 population living in and around Gondar. A total of 500 registered HCPs working in GUH were included. One out of every two HCPs working in the hospitals were randomly selected to obtain diverse opinions during their spare time and to reach our target sample size of 250 HCPs. Data was cross-checked to ensure no HCPs were selected twice.
Content of the study questionnaire
The questionnaire was divided into three parts. The first section included 17 items covered the sociodemographic details including job characteristics, gender, age, marital status, religion, ethnicity, education qualification, monthly income, years of experience, site of practice, shift working, hours of work per week, and number of patients treated per day.
Symptoms of burnout syndrome
This section contained a list of symptoms of BOS (19 items) obtained from the Astudillo and Mendinueta[9] symptoms such as irritability, self-criticism, insomnia, fatigue, spinal problem, lack of organization, depressive states, and others that affect the HCPs work and suggestions for alleviating professional stress. The 19-item self-reported symptoms of BOS are rated from 0 (never), 1 (sometimes), 2 (often), and 3 (always). The sum of the scores of the rating of the items were calculated with a total minimum score of 0 to a maximum score of 57. HCPs who scored more than 23 were considered as burned out.
Maslach Burnout Inventory
The Maslach Burnout Inventory (MBI)[10,11] was most commonly used 12-item measuring tool to self-assess the risk of burnout. MBI is a validated tool that values the three syndrome subscales of emotional exhaustion, depersonalization, and lack of personal accomplishment. The items are scored on Likert scale from 0 (never) to 7 (everyday). Relevant items were reverse-coded. The participants were not aware of the scoring system. The BOS assessment scores were calculated as a summation of answers to each item and represented with their mean and standard deviations (SDs).
The questionnaires were distributed to HCPs working in University of Gondar Hospital during their leisure time after explaining the contents, aim, and anonymity of the study. Confidentiality was maintained of their personal responses and the participants were not aware of the scoring system. The survey was conducted during regular working hours, provided with pens and asked them to sit a part, not to communicate with others during administration of questionnaire as to encourage spontaneous and honest response.
Survey questionnaire validation and reliability
All the questions were administered in English. The questionnaire was tested for reliability, psychometric, and internal validity. The internal consistency estimate of reliability of test score (Cronbach's alpha) was found to 0.87 indicating a good construct of questionnaire. Furthermore, the survey questionnaire was piloted among 15 residents, modified to meet the compatibility of local settings. The results of the piloting were not included herein. An average of 30 min time was allotted to complete the questionnaire and all the investigators equally contributed in collecting the responses from HCPs.
Ethical clearance
Ethical approval for conducting the study was obtained from Institution Review Committee of University of Gondar, School of Pharmacy. Written informed consent was obtained from each participant before the study questionnaire administration. The authors confirm that the study was conducted in accordance with the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000).
Statistical analysis
Data entry and statistical analysis were performed using SPSS (version 22; IBM, Armonk, NY, USA) for Windows. Descriptive analysis was applied to calculate the frequencies, percentages, and mean (SD) used for quantitative variables. Pearson's correlation analysis and multivariate logistic regression were assess the relationship between BOS as dependent and various personal job factors as independent factors.
Results
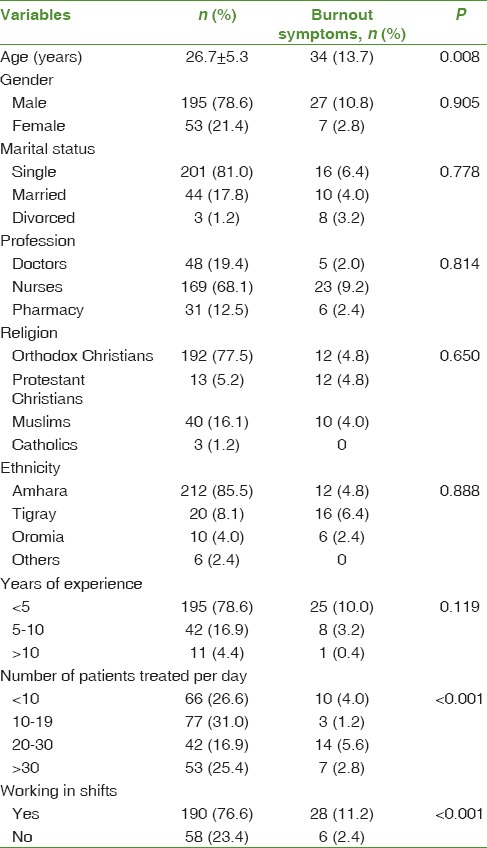
A total of 250 HCPs approached, 248 were responded (response rate – 99.2%). Majority of the participants were male (78.6%) with a mean age of 26.7 ± 5.3 (SD). Most of them were single (81%), nurses (68.1%), from Amhara state (85.5%) and were Orthodox Christians (77.5%). More than three-fourth of the HCPs (78.6%) had less than 5 years experience in clinical practice, working in shifts (76.6%) and serving 10–19 patients everyday (31%). The prevalence of BOS among HCPs working in GUH is 13.7% (scored more than 23 points). A statistical significance (P < 0.05) was noticed for variables like age, patient load, and those working in shifts. Sociodemographic details and the prevalence of BOS among the study participants are summarized in Table 1.
Table 1.
Demographic characteristics and prevalence of burnout syndrome among health-care professionals
More than 50% of the HCPs expressed that they always experience professional stress symptoms such as debility (52.8%), followed by self-criticism (56%) and irritability (52.8%) sometimes, and often experienced fatigue (30.6%), while consuming sedatives (88.7%) and analgesics (76.6%) were uncommon among the participants [Table 2]. These symptoms were higher among male (10%) and nursing professionals (9.2%), who work in shifts (11.2%), and have <5 years of experience (10%).
Table 2.
Percentage of burnout symptoms among health-care professionals in Gondar University Hospital, Ethiopia
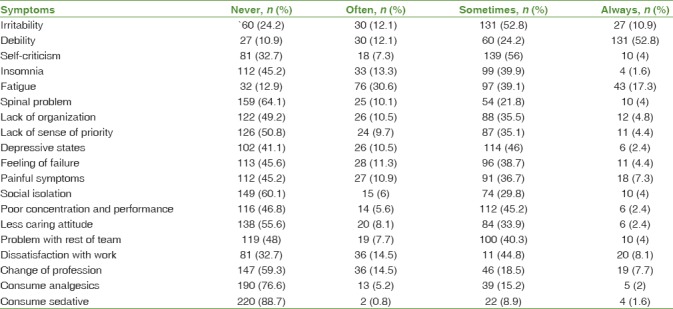
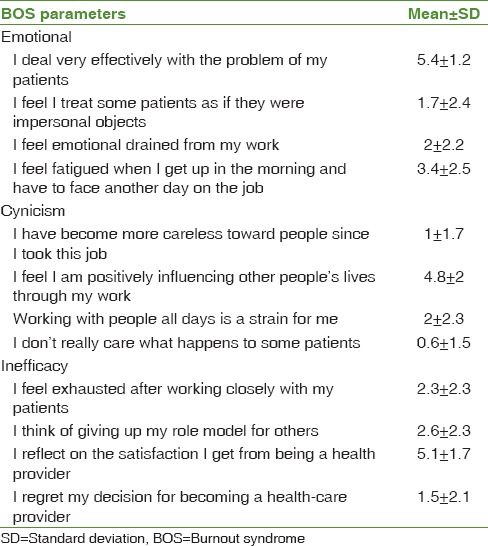
Table 3 summarizes the mean scores of MBI subscales among HCPs. The mean score of emotional exhaustion and inefficiency was higher than cynicism. In particular, the simultaneous occurrence of high level of BOS among HCPs, that is, a mean score of emotional exhaustion and inefficacy concerning HCPs felt that they were very effective to deal with patient problems (5.4 ± 1.2) and satisfied for being a health provider (5.1 ± 1.7). However, a low-level of cynicism was noticed than emotional exhaustion and inefficacy because most of the participants felt that their working life positively influenced others (4.8 ± 2.0).
Table 3.
Maslach Burnout Inventory
The sociodemographic and professional factors assumed to be associated with BOS among the study participants are shown in Table 4. Sex, marital status, profession, and work experience were found to be significantly associated with BOS in the multivariate analysis.
Table 4.
Bivariate and multiple logistic regression model of Maslach Burnout Inventory subscales among health-care professionals
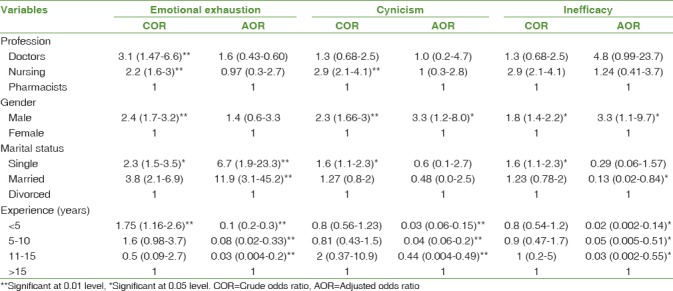
Male HCPs were more likely to experience emotional exhaustion as compared to females (adjusted odds ratio: 6.7, 95% confidence interval: [1.9–23.3]). HCPs with <15 years of work experience were strongly associated with emotional exhaustion than those with more than 15 years of experience. Being single (6.7 times) or married (11.9 times) were more likely to experience emotional exhaustion as compared to counterpart. However, professional status was not significantly associated with emotional exhaustion (P = 0.2).
Sex, marital status, and profession were strongly associated with cynicism and inefficiency in the bivariate logistic regression analysis (P < 0.01). On the other hand, multiple logistic regression showed that HCPs working experience <15 years were found to be significantly associated with cynicism (P < 0.01) and less significant with inefficiency (P < 0.05). However, sex, marital status, and profession were not significantly associated with cynicism and inefficiency in the multivariate logistic regression.
Discussion
This study investigated the prevalence and the associated factors contributing BOS among HCPs working in GUH, Northwest Ethiopia. Several studies have assessed the prevalence of this condition in different health-care fields. With the absence of information in Ethiopian HCPs, we studied to estimate the prevalence of BOS among HCPs working in our hospital. Our findings revealed that 13.7% of the HCPs have symptoms of BOS. This level is lower than other studies conducted on different group of HCPs using MBI scale and reported a prevalence ranging from 28.0% to 46.5%[12,13,14] but higher than findings from Dutch study[15] conducted among nurses with 2%–10% and a Qatari study among general practitioners (12.6%) conducted by Abdulla et al.[4] The differences may be due to focusing on specific group of HCPs and the nature of health-care system.
Previous studies have identified that demographic variables such as gender, younger age, and experience were some of the predictive factors for burnout.[16,17,18,19] In correlation with previous studies, our study showed that a higher number of males (10.8%), younger age (26.7 ± 5.3; 13.7%), and <5 years of experience (10%) experienced burnout symptoms. In contrast, some studies identified female sex,[20] high workload,[12] and conflicts in the work place[21] are some of the predictive factors for burnout. The reasons for burnout among younger HCPs may be due to excessive utilization of their potentiality while starting their carrier in order to understand the patient situations and to gain more experience. Gender and professional differences were unclear, females and nurses were overrepresented than males in previous studies.[22,23,24,25] Such differences can be explained due to cultural aspects involved in socialization process. Moreover, in this study, a significant number of HCPs with huge patient load (20–30 patients/day) and working on shifts (11.4%) also experienced BOS. Providing round-the-clock services disrupts social rhythms, leads to psychosomatic health problems and diminishes the job satisfaction. A decade ago, Demerouti et al.[26] highlighted that rotational shift working (irrespective of their profession) disrupts the social life and increases the home conflicts. Almost all studies on the effect of BOS accepted that HCPs were generally at relatively high risk of burnout. Olkinuora et al.[27] identified HCPs who are dealing with chronically ill, incurable, or dying patients can create BOS. Further, Shimizutani et al.[28] study on nurses reported that client-related burnout was closely associated with “personal relationships at the workplace” or “conflicts with patients” heightens the risk of BOS.
In correlation with previous studies,[4,29] our study found physical and psychological symptoms relating to BOS, such as debility, self-criticism, depressive states, and poor performance. It is notable that 45% of the HCPs affected dissatisfaction with work. However, majority of HCPs (>75%) working in GUH did not consider using analgesics and addictive drugs.
Considering MBI criterion, higher proportion of emotional exhaustion and inefficacy than cynicism was noticed in this study. Other studies, however, show a level of occurrence of similar to our findings.[30,31,32] Studies conducted on different group of HCPs showed a high level of emotional exhaustion, depolarization, and low level of inefficacy.[18,19,24] However, in our study, HCPs experienced a high level of emotional exhaustion and inefficacy, which indicates that the HCPs working in GUH are vulnerable to burnout in the workplace. The mean scores of these three dimensions in the high burnout level categories indicated that nearly 20% of the HCPs are experiencing high levels of burnout.[33,34,35] However, some other studies identified a high score of emotional exhaustion subscale with estimated prevalence ranging from 25% to 51.9%.[3,36,37] The possible explanation for this research is that HCPs found in the study area young and degree holders, which indicates the age and educational level tend to have higher expectations of their jobs.
This research showed that work experience was significantly correlated with the three dimensions of burnout. In line with what has been reported from previous studies, our findings identified a significant correlation of the three dimensions of BOS among younger employers than older employees.[33,38] This possible reasons for this may be BOS could affect mostly on less experienced HCPs as compared to more experienced HCPs. An inverse correlation between BOS and work experience was noticed, which indicates as work experience increases, BOS decreases. Further, with regard to marital status, there was a statistical significance noticed between emotional exhaustion and HCPs marital status. A study conducted by Gombor[39] on nurses found similar correlation with their marital status. These findings are different with Alkhazrajy et al. study where majority of married health-care providers had higher levels of emotional exhaustion.[40]
Some limitations of this study should be considered. First, the study was conducted on single center which cannot be generalized to other health centers in Ethiopia. Second, we used self-administered questionnaire using validated MBI scale, therefore, some of the respondents may be overestimated or underestimated due to motivations and cultural factors which might lead to recall bias.
Conclusion
The prevalence of BOS among HCPs in GUH was 13.7%. Young workers, who see a large number of patients per day and working in shifts were contributing factors for BOS symptoms. Being male, unmarried, and years of work experience were significant risk factors for all the three dimensions of BOS. Therefore, we propose the GUH to undertake pragmatic measures to prevent stressful challenges for the physical and mental well-being of the HCPs. Further in-depth qualitative studies are recommended to investigate the underlying factors related to BOS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Miss. Juliet Nkunta Mbesha from Zambia for manuscript editing.
References
- 1.Marek T, Schaufeli WB, Maslach C. Professional Burnout: Recent Developments in Theory and Research. Philadelphia, PA, US: Routledge; 2017. [Google Scholar]
- 2.Chantal UM, Jane K. Exploring the factors contributing to stress and coping strategies of nurses at university teaching hospital of Butare in Rwanda. Rwanda J. 2015;2:99. [Google Scholar]
- 3.van Mol MM, Kompanje EJ, Benoit DD, Bakker J, Nijkamp MD. The prevalence of compassion fatigue and burnout among healthcare professionals in Intensive Care Units: A Systematic review. PLoS One. 2015;10:e0136955. doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdulla L, Al-Qahtani DM, Al-Kuwari MG. Prevalence and determinants of burnout syndrome among primary healthcare professionals in Qatar. S Afr Fam Pract. 2011;53:380–3. [Google Scholar]
- 5.Cañadas-De la Fuente GA, Vargas C, San Luis C, García I, Cañadas GR, De la Fuente EI, et al. Risk factors and prevalence of burnout syndrome in the nursing profession. Int J Nurs Stud. 2015;52:240–9. doi: 10.1016/j.ijnurstu.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Toker S, Melamed S, Berliner S, Zeltser D, Shapira I. Burnout and risk of coronary heart disease: A prospective study of 8838 employees. Psychosom Med. 2012;74:840–7. doi: 10.1097/PSY.0b013e31826c3174. [DOI] [PubMed] [Google Scholar]
- 7.Johns C, editor. Becoming a Reflective Practitioner. Hoboken, NJ, USA: John Wiley & Sons; 2017. [Google Scholar]
- 8.Koh MY, Chong PH, Neo PS, Ong YJ, Yong WC, Ong WY, et al. Burnout, psychological morbidity and use of coping mechanisms among palliative care practitioners: A multi-centre cross-sectional study. Palliat Med. 2015;29:633–42. doi: 10.1177/0269216315575850. [DOI] [PubMed] [Google Scholar]
- 9.Astudillo W, Mendinueta C. Exhaustion syndrome in palliative care. Support Care Cancer. 1996;4:408–15. doi: 10.1007/BF01880637. [DOI] [PubMed] [Google Scholar]
- 10.Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2:99–103. [Google Scholar]
- 11.Schaufeli WB, Leiter MP, Maslach C, Jackson SE. Maslach burnout inventory-general survey (MBI-GS) In: Maslach C, Jackson SE, Leiter MP, editors. MBI Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 12.Barbosa FT, Leão BA, Tavares GM, Santos JG. Burnout syndrome and weekly workload of on-call physicians: Cross-sectional study. Sao Paulo Med J. 2012;130:282–8. doi: 10.1590/S1516-31802012000500003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merlani P, Verdon M, Businger A, Domenighetti G, Pargger H, Ricou B, et al. Burnout in ICU caregivers: A multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184:1140–6. doi: 10.1164/rccm.201101-0068OC. [DOI] [PubMed] [Google Scholar]
- 14.Verdon M, Merlani P, Perneger T, Ricou B. Burnout in a surgical ICU team. Intensive Care Med. 2008;34:152–6. doi: 10.1007/s00134-007-0907-5. [DOI] [PubMed] [Google Scholar]
- 15.Pisanti R, van der Doef M, Maes S, Lazzari D, Bertini M. Job characteristics, organizational conditions, and distress/well-being among Italian and Dutch nurses: A cross-national comparison. Int J Nurs Stud. 2011;48:829–37. doi: 10.1016/j.ijnurstu.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Ebling M, Carlotto MS. Burnout syndrome and associated factors among health professionals of a public hospital. Trends Psychiatry Psychother. 2012;34:93–100. doi: 10.1590/s2237-60892012000200008. [DOI] [PubMed] [Google Scholar]
- 17.Zhang YY, Zhang C, Han XR, Li W, Wang YL. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: A correlative meta-analysis. Medicine (Baltimore) 2018;97:e11086. doi: 10.1097/MD.0000000000011086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang XC, Huang DS, Guan P SUBLIN Study Team. Job burnout among critical care nurses from 14 adult Intensive Care Units in Northeastern China: A cross-sectional survey. BMJ Open. 2014;4:e004813. doi: 10.1136/bmjopen-2014-004813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellieni CV, Righetti P, Ciampa R, Iacoponi F, Coviello C, Buonocore G, et al. Assessing burnout among neonatologists. J Matern Fetal Neonatal Med. 2012;25:2130–4. doi: 10.3109/14767058.2012.666590. [DOI] [PubMed] [Google Scholar]
- 20.Raftopoulos V, Charalambous A, Talias M. The factors associated with the burnout syndrome and fatigue in Cypriot nurses: A census report. BMC Public Health. 2012;12:457. doi: 10.1186/1471-2458-12-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13:482–8. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 22.Gosseries O, Demertzi A, Ledoux D, Bruno MA, Vanhaudenhuyse A, Thibaut A, et al. Burnout in healthcare workers managing chronic patients with disorders of consciousness. Brain Inj. 2012;26:1493–9. doi: 10.3109/02699052.2012.695426. [DOI] [PubMed] [Google Scholar]
- 23.Cho SH, June KJ, Kim YM, Cho YA, Yoo CS, Yun SC, et al. Nurse staffing, quality of nursing care and nurse job outcomes in Intensive Care Units. J Clin Nurs. 2009;18:1729–37. doi: 10.1111/j.1365-2702.2008.02721.x. [DOI] [PubMed] [Google Scholar]
- 24.Czaja AS, Moss M, Mealer M. Symptoms of posttraumatic stress disorder among pediatric acute care nurses. J Pediatr Nurs. 2012;27:357–65. doi: 10.1016/j.pedn.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karanikola MN, Papathanassoglou ED, Mpouzika M, Lemonidou C. Burnout syndrome indices in Greek intensive care nursing personnel. Dimens Crit Care Nurs. 2012;31:94–101. doi: 10.1097/DCC.0b013e3182445fd2. [DOI] [PubMed] [Google Scholar]
- 26.Demerouti E, Geurts SA, Bakker AB, Euwema M. The impact of shiftwork on work – Home conflict, job attitudes and health. Ergonomics. 2004;47:987–1002. doi: 10.1080/00140130410001670408. [DOI] [PubMed] [Google Scholar]
- 27.Olkinuora M, Asp S, Juntunen J, Kauttu K, Strid L, Äärimaa M. Stress symptoms, burnout and suicidal thoughts in Finnish physicians. Social Psychiatry and Psychiatric Epidemiology. 1990;25:81–6. doi: 10.1007/BF00794986. [DOI] [PubMed] [Google Scholar]
- 28.Shimizutani M, Odagiri Y, Ohya Y, Shimomitsu T, Kristensen TS, Maruta T, et al. Relationship of nurse burnout with personality characteristics and coping behaviors. Ind Health. 2008;46:326–35. doi: 10.2486/indhealth.46.326. [DOI] [PubMed] [Google Scholar]
- 29.Yousefy AR, Ghassemi GR. Job burnout in psychiatric and medical nurses in Isfahan, Islamic republic of Iran. East Mediterr Health J. 2006;12:662–9. [PubMed] [Google Scholar]
- 30.Silva SC, Nunes MA, Santana VR, Reis FP, Machado Neto J, Lima SO, et al. Burnout syndrome in professionals of the primary healthcare network in Aracaju, Brazil. Cien Saude Colet. 2015;20:3011–20. doi: 10.1590/1413-812320152010.19912014. [DOI] [PubMed] [Google Scholar]
- 31.Costa EF, Santos SA, Santos AT, Melo EV, Andrade TM. Burnout syndrome and associated factors among medical students: A cross-sectional study. Clinics (Sao Paulo) 2012;67:573–80. doi: 10.6061/clinics/2012(06)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pedersen AF, Andersen CM, Olesen F, Vedsted P. Risk of burnout in Danish GPs and exploration of factors associated with development of burnout: A Two-wave panel study. Int J Family Med 2013. 2013 doi: 10.1155/2013/603713. 603713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nataye YY. Level of Burnout among EU & ICU Nurses Addis Ababa, Ethiopia. Cross Sectional Descriptive Study. 2014. [Last accessed on 2016 Jan 24]. Available from: http://www.urn.fi/URN: NBN: fi: amk-201402102158 .
- 34.Ríos Risquez MI, Godoy Fernández C, Peñalver Hernández F, Alonso Tovar AR, López Alcaraz F, López Romera A, et al. Comparative study of burnout in intensive care and emergency care nursing staff. Enferm Intensiva. 2008;19:2–13. doi: 10.1016/s1130-2399(08)72738-x. [DOI] [PubMed] [Google Scholar]
- 35.Loiselle CG, Gélinas C, Cassoff J, Boileau J, McVey L. A pre-post evaluation of the adler/Sheiner programme (ASP): A nursing informational programme to support families and nurses in an Intensive Care Unit (ICU) Intensive Crit Care Nurs. 2012;28:32–40. doi: 10.1016/j.iccn.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Guntupalli KK, Fromm RE., Jr Burnout in the internist – Intensivist. Intensive Care Med. 1996;22:625–30. doi: 10.1007/BF01709737. [DOI] [PubMed] [Google Scholar]
- 37.Shehabi Y, Dobb G, Jenkins I, Pascoe R, Edwards N, Butt W, et al. Burnout syndrome among Australian intensivists: A survey. Crit Care Resusc. 2008;10:312–5. [PubMed] [Google Scholar]
- 38.Ayala E, Carnero AM. Determinants of burnout in acute and critical care military nursing personnel: A cross-sectional study from Peru. PLoS One. 2013;8:e54408. doi: 10.1371/journal.pone.0054408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gombor A. Budapest: University of Eotvos Lorand Hungary; 2009. Burnout in Hungarian and Swedish Emergency Nurses: Demographics Variables, Work Related Factors, Social Support, Personality, and Life Satisfaction as Determinants of Burnout. Ph. D Dissertation. [Google Scholar]
- 40.Alkhazrajy LA, Sabah S, Hassan SM. Prevalence of depressive symptoms among primary health care providers in Baghdad. Int J Health Psychol Res. 2014;2:1–20. [Google Scholar]


