Abstract
Background
Depressive symptoms are common in children with developmental language disorder (DLD). However, risk and protective factors contributing to these problems are currently underspecified.
Aims
The current longitudinal study examined the role of emotion‐regulation (ER) strategies in the severity of depressive symptoms in children with and without DLD, taking into account the severity of communication problems of children with DLD.
Methods & Procedures
We followed clinically referred children with DLD (n = 114, 49% girls) and without DLD (n = 214, 58% girls) between the ages of 8 and 16 years across an 18‐month period. Participants completed self‐report questionnaires at three time points. Parents of children with DLD reported on their child's communication problems.
Outcomes & Results
Multilevel analyses confirmed higher levels of depressive symptoms in youngsters with DLD compared with peers without DLD, with a decrease across time in the DLD group. In both groups, higher levels of approach and increasing avoidant strategies aimed at distraction or trivializing a problem explained lower depressive symptoms, whereas more worry and externalizing strategies contributed to more depressive symptoms. Within the DLD group, semantic language problems were associated with higher depressive symptoms. However, this relation was mediated by the tendency to worry or use externalizing strategies.
Conclusions & Implications
Results suggest that interventions for children with DLD should focus on enhancing their adaptive ER strategies to help them cope with daily stressors just as in the general population.
Keywords: internalizing psychopathology, development, adolescence, specific language impairment
What this paper adds
What is already known on the subject
The high prevalence of depressive symptoms in children with DLD is not well explained by the severity of their communication problems alone. Therefore, a better understanding of the underlying mechanisms is warranted. Difficulty regulating negative emotions may put children with DLD at risk for the development of depressive symptoms.
What this paper adds to existing knowledge
The study showed that adaptive ER strategies, such as approaching a problem or distracting oneself, contributed to lower levels of depressive symptoms in children with and without DLD. Conversely, maladaptive strategies, such as worrying or externalizing, contributed to more depressive symptoms in both groups. Within the DLD group, more semantic problems related to more depressive symptoms, but this relation was mediated by the use of maladaptive ER strategies.
What are the potential or actual clinical implications of this work?
These findings suggest that children with DLD may benefit from improving their ER skills, just as children without DLD. Improving these strategies would be expected to contribute more to decreasing depressive symptoms in children with DLD than improving their communication abilities. However, the depressive symptoms of children with DLD remained elevated, even after their ER strategies were accounted for. Therefore, additional risk factors should be considered in future research.
Introduction
Seven per cent of children are reported to have a developmental language disorder (DLD) (Norbury et al. 2017, Tomblin et al. 1997), which was formerly referred to as specific language impairment (SLI) (for a discussion of DSM‐5 classification and terminology, see Bishop et al. 2017). DLD can severely impact on children's mental health, and an increased risk for depressive symptoms is consistently reported in this group. Clinical levels of depression range from 20% to 39% in children and adolescents with DLD compared with 14–18% in peers without DLD (Beitchman et al. 1996, Botting et al. 2016b, Conti‐Ramsden and Botting 2008). Yet, the level of depressive symptoms is often unrelated to or shows only small correlations with, the type and severity of communication problems in children with DLD (Beitchman et al. 1996, Botting et al. 2016b, St. Clair et al. 2011). The study examines why children with DLD are more vulnerable to developing depressive symptoms than children without DLD, given that the severity of their communication problems only makes a small contribution to explaining these symptoms.
Various studies with children from a community population have demonstrated that emotion regulation (ER) is related to fewer depressive symptoms (Joormann and Stanton 2016, Schäfer et al. 2017). ER refers to the cognitive and behavioural processes a person uses to monitor emotions, to modify the strength of the own emotional experience and the strength and timing of the expression of emotions in order to reach personal and social goals (Gross 1998). When negative emotions are overwhelming, they can impede the ability to address the emotion evoking situation adequately, resulting in greater negative affect (Fields and Prinz 1997, Joormann and Stanton 2016). Children with DLD are reported to experience difficulties regulating negative emotions (Brinton et al. 2015, Fujiki et al. 2004). However, these difficulties have not yet been shown to be associated with higher levels of depressive symptoms. Therefore, in this study we used a longitudinal design to examine the extent to which different ER strategies were risk or protective factors for the level of and changes in depressive symptoms in children with and without DLD.
Developmental language disorder and depressive symptoms
The DSM‐5 describes language disorders as significant difficulties with the acquisition and use of language (American Psychiatric Association (APA) 2013). These language problems cannot be explained by other conditions, such as hearing impairment or autism spectrum disorder, nor are the language difficulties better explained by intellectual disability or general developmental delay. Language disorders are present early in life, and continue to affect development (APA 2013). Children with DLD experience problems in the content (semantics) and/or the form of language (phonology, morphology and syntax) (APA 2013, Bishop et al. 2017). Problems can occur in both receptive (e.g., understanding of word meanings or understanding the meaning of complex phrases) or expressive language (e.g., finding the right words to express ideas or production of grammatical sentences). Additionally, children with DLD often also encounter difficulties using language in social interaction, that is pragmatics (APA 2013, Bishop et al. 2017, Norbury et al. 2004).
In addition to problems acquiring and using language, depressive symptoms are frequently noted in children with a diagnosis of DLD (Beitchman et al. 1996, Botting et al. 2016b, St. Clair et al. 2011). Children who have depressive feelings generally have low‐self‐esteem, and experience feelings of hopelessness about their lives, their future and their own ability to change their situation (Wicks‐Nelson and Israel 2015). Depressive symptoms become more prevalent during puberty, which has been related to physical and social changes in the lives of youngsters (Dahl and Gunnar 2009). However, children who experience many life stressors early are vulnerable to develop depressive symptoms (Wicks‐Nelson and Israel 2015). DLD provides children with many stressors in communication, in social interactions and in educational contexts (Andrés‐Roqueta et al. 2016, Bakopoulou and Dockrell 2016). These stressors may contribute to the higher levels of depressive symptoms, which are found in children with DLD (Beitchman et al. 1996, Conti‐Ramsden and Botting 2008, St. Clair et al. 2011). During adolescence, the levels of internalizing problems, including depressive symptoms, have been reported to show a small decrease in youngsters with DLD, although these levels still remained elevated compared with the norm of the general population (St. Clair et al. 2011). This different developmental path may indicate that children with DLD develop strategies to deal with the stressors associated with their DLD as they become older.
Depressive symptoms of children with DLD have been reported independently of the type or severity of DLD. Specifically, longitudinal studies report no associations between the severity of receptive and expressive language problems at the age of 7 years and depressive symptoms in adolescence (St. Clair et al. 2011). In addition, 5‐year‐olds with primarily expressive problems or with both receptive and expressive problems, did not differ in their level of depressive symptoms at age 12 years (Beitchman et al. 1996). Only difficulties in pragmatic language contributed to the prediction of depressive symptoms in adolescents with DLD. But again, this only accounted for a small amount of variance (St. Clair et al. 2011, Sullivan et al. 2016). The contribution of pragmatic language problems to depressive symptoms may play a more important role than structural aspects of language, because pragmatic language is an important prerequisite for social interactions, even after controlling for other language abilities (Ketelaars et al. 2010, St. Clair et al. 2011). Positive social interactions in turn are an important protective factor for depressive symptoms (Botting et al. 2016b, Van Harmelen et al. 2016).
ER in children with DLD
Learning to regulate emotions is highly dependent on social interaction with other people, in which communication plays an important role (Dunn et al. 1991, Rieffe et al. 2016). Typically, caregivers talk with their children about their feelings, why they happen, how to control themselves when emotions run high, and how children may express their emotions in ways that help achieve both personal and social goals (Denham and Auerbach 1995, Dunn et al. 1991, Rieffe et al. 2016). When children grow older, they continue to learn from their social environment, through interactions with friends and incidental exposure to others’ interactions, such as overhearing and observation (Brown and Dunn 1996). For children with DLD, communication problems limit interaction with others from an early age (Andrés‐Roqueta et al., 2016). Children with DLD miss important information, need more processing time, and often lack the vocabulary to understand fully what is going on in social interactions. Therefore, this process of emotion socialization may be hampered (Fujiki et al. 2004, Rieffe et al. 2016).
A limited number of studies has examined ER in children with DLD. These studies report that children with DLD show more inappropriate expressions of emotions, with less consideration of the consequences for others or less congruent with the level of emotions expressed by other persons. This is indicative of ER problems (Brinton et al. 2015, Fujiki et al. 2002, 2004). Additionally, more negative outburst and behaviour problems have been reported, especially in younger children with DLD. However, these problems decrease during primary school (Horowitz et al. 2005, St. Clair et al. 2011). These studies suggest that children with DLD have developed less adaptive strategies to regulate their emotions. However, there has been no research examining the ER strategies of children with DLD to date.
ER strategies and depressive symptoms
ER strategies can be categorized in different ways. Here we focus on four main categories: approach and avoidant ER strategies, which are often found to be adaptive, as well as worry and externalizing strategies, which are considered maladaptive strategies (Fields and Prinz 1997, Wright et al. 2010).
Approach strategies involve strategies that try to solve a problem or diminish the negative impact of the emotion‐evoking event. This can be either behaviourally (by trying to find a solution or through seeking help from others) or cognitively (by trying to reappraise the situation). Approach strategies typically increase during late childhood and adolescence (Fields and Prinz 1997, Zimmer‐Gembeck and Skinner 2011) and are related to lower levels of depressive symptoms (Schäfer et al. 2017). Several studies have shown that children with DLD tended to seek adult support to a greater extent than children without DLD (Rice et al. 1991, Timler 2008). However, they are reported to have more difficulty negotiating with peers and navigating peer conflicts throughout the primary education years (Brinton and Fujiki 1999, Rice et al. 1991, Timler 2008). These difficulties in social skills may make it more challenging for children with DLD to use approach strategies.
In contrast, avoidant strategies involve trying to diminish the impact of a negative event by actively withdrawing from the situation, such as ignoring, distracting or distancing oneself from the situation (Fields and Prinz 1997). Avoidant strategies such as procrastination or suppression of emotions are associated with higher levels of depressive symptoms in children and adolescents (Schäfer et al. 2017). However, other avoidant strategies, aimed at distracting oneself or trivializing a situation, are associated with lower levels of depressive feelings (Joormann and Stanton 2016). The use of these adaptive cognitive avoidant strategies increases during adolescence (Zimmer‐Gembeck and Skinner 2011).
Beyond approach and avoidance strategies, a further ER strategy involves worry or rumination. By worrying, children keep reminding themselves of their problems without coming any closer to a solution, thus emotional arousal remains at a high level (Rieffe et al. 2008). This usually does not decrease, but rather increases the impact of a negative situation. In fact, worrying is a strong predictor of depressive symptoms (Schäfer et al. 2017), and is considered to be a maladaptive ER strategy (Joormann and Stanton 2016). It has been noted that school‐aged children with DLD tend to withdraw from social situations (Brinton and Fujiki 1999, Fujiki et al. 2004). While this may lead to feelings of relief at the time or help children organize their thoughts, it may also result in worrying, which presents a risk factor for depressive symptoms.
Finally, yet another maladaptive ER strategy involves venting negative emotions through externalizing behaviours, such as yelling, hitting or slamming a door. This behaviour is usually not adaptive because it provokes new negative situations, instead of diminishing the impact of the first one (Burks et al. 1999). Indeed, more externalizing strategies are associated with higher levels of depressive symptoms in children (Wright et al. 2010). Although externalizing strategies are common in toddlers, a sharp decrease in externalizing strategies is noted when children become able to communicate their emotions through language (Fields and Prinz 1997), During childhood and adolescence relatively low and stable levels of externalizing strategies are found (Fields and Prinz 1997, Zimmer‐Gembeck and Skinner 2011), although some studies found an increase during puberty (Zimmer‐Gembeck and Skinner 2011). Children with DLD in late childhood reported more externalizing strategies in response to peer conflict situations than their peers without DLD (Timler 2008). This may form another risk factor for depressive symptoms for these children.
The present study
In this longitudinal study, our first aim was to explain the differences in depressive symptoms in children with and without DLD. We examined depressive symptoms in clinically referred children between 8 and 16 years old with DLD and compared with children without DLD at three time points across 18 months. In line with previous research, we expected higher levels of depressive symptoms in children with DLD, as compared with those without DLD (Conti‐Ramsden and Botting 2008, Sullivan et al. 2016). The level of depressive symptoms may be expected to decrease in older children with DLD (St. Clair et al. 2011), while increasing levels were expected in children without DLD (Dahl and Gunnar 2009).
We expected that the tendency to use different ER strategies would explain differences in the severity of depressive symptoms both between and within children across time in both groups (Joormann and Stanton 2016, Schäfer et al. 2017). In line with earlier findings in the general population, we expected more frequent use of approach and avoidant strategies and lower levels of worry and externalizing strategies to be associated with lower levels of depressive symptoms (Joormann and Stanton 2016, Schäfer et al. 2017). Additionally, we expected that the increasing tendency to use more adaptive and less maladaptive ER strategies across time would explain decreasing depressive symptoms (Rieffe et al. 2008, Schäfer et al. 2017). In children with DLD, more difficulties in appropriate emotion expression have been reported, which may indicate ER problems (Brinton et al. 2015, Fujiki et al. 2002, 2004). This may be an important underlying factor for the elevated levels of depressive symptoms in children with DLD. Therefore, we expected stronger associations between the different ER strategies and depressive symptoms in children with DLD compared with children without DLD.
Our second aim was to explain differences in depressive symptoms within the group of children with DLD. We examined whether the type and severity of communication problems of children with DLD could explain their depressive symptoms, and we explored whether their communication problems were related to the tendency to use different ER strategies. Previous research on depressive symptoms in children with DLD found only small associations with their communication problems or associations with pragmatic problems only (St. Clair et al. 2011, Sullivan et al. 2016). Therefore, we hypothesized that the type and severity of communication problems of children with DLD would not contribute to the depressive symptoms when we accounted for their ER strategies (Conti‐Ramsden and Botting 2008, Botting et al. 2016b). Because communication problems were not expected to play a significant role in depressive symptoms of children without DLD, we only examined this in children with DLD.
Methods
Design
In this repeated measures longitudinal study, the severity of depressive symptoms was examined in children with and without DLD between the ages of 8 and 16 years across 18 months. Children completed self‐report questionnaires on three occasions with 9 months in between each measurement. Participants were recruited through primary and secondary schools in different areas of the Netherlands, including cities and more rural areas. Children with DLD were recruited through both regular and specialized schools. An active consent procedure was used.
Participants
A total of 114 children with a diagnosis of DLD and 214 without DLD participated in the study (table 1). Children with DLD were included if they had a formal diagnosis of DLD and had no identified autism spectrum disorder or hearing impairment. Information about any formal diagnoses were provided by the parents and were verified in school or medical files. In the Netherlands, children receive a diagnosis of DLD if they experience receptive and/or expressive language abilities of 1.5 SD below the mean of the population. The diagnosis is provided by a team of professionals, including a speech and language pathologist, a psychologist, and an audiological scientist in line with DSM‐4 criteria (APA 1994) and has to be renewed every 5 years to make children eligible to support from the government.
Table 1.
Characteristics of participants at Time 1
| With DLD | Without DLD | |
|---|---|---|
| Number of children (n) | 114 | 214 |
| Age range (years) | 8.4–16.0 | 8.3–14.7 |
| Mean age (years, SD) | 11.5 (2.0) | 11.5 (1.4) |
| Male (n,%) | 58 (50.9%) | 89 (41.6%) |
| Female (n,%) | 56 (49.1%) | 125 (58.4%) |
| Regular schools (n,%) | 32 (28.1%) | 214 (100%) |
| Special education (n,%) | 82 (71.9%) | – |
| PIQ (mean, SD)*** | n = 108 | n = 184 |
| 93.41 (12.73) | 107.23 (17.22) | |
| Range PIQ | 70–140 | 78–140 |
| Neighbourhood SES (mean, SD)*** | 0.02 (1.08) | 0.55 (1.25) |
| Range neighbourhood SES | –4.19 to 2.50 | –5.24 to 2.44 |
Note: *** p < .001.
Children without DLD were included if they had no neurodevelopmental disorders, as indicated by their parents, and had language abilities in the average range, which was assessed with two subtests of the CELF (Semantic relations and Text understanding; Kort et al. 2008). The current study is part of a larger research project on the effects of communication problems on the social and emotional development of children. Earlier studies reported on deaf and hard of hearing children and children with an autism spectrum disorder in comparison with a subsample of the children without DLD of the current study (Bos et al. 2018, Rieffe et al. 2014, Theunissen et al. 2011) and on children with DLD (Van den Bedem et al. 2018).
Children with and without DLD were comparable in mean age at Time 1 (t(176.49) = .36, p = .747) and gender distribution (χ²(1) = 2.60, p = .130), with an almost equal number of boys and girls in the DLD group (table 1). Children in the DLD group had a lower Performance IQ (PIQ) than the children without DLD (t(264.65) = 7.6, p < .001). Children with DLD had a lower socioeconomic status as indicated by the neighbourhoods in which they lived. The Neighbourhood SES reflects the mean income, occupation and educational level of all adults in a neighbourhood, as compared with all other neighbourhoods in the Netherlands (with a mean of 0 and a range of –6.8 to 3.1). Children with DLD lived in lower rated neighbourhoods than children without DLD (t(326) = 3.76, p < .001), which was mostly due to above average Neighbourhood SES of children without DLD.
Materials
Depressive symptoms
Depressive symptoms were assessed with the Child Depression Inventory (CDI; Kovacs 1992), which examines behavioural, cognitive and emotional symptoms of depression in children from the age of 8 years. In the current study, the adapted version of the CDI (Theunissen et al. 2011) was used in order to reduce the amount of language for children with DLD. Children read one statement and endorsed if a statement was not (1), a bit (2) or most of the time (3) true. In order not to upset the children, the item about suicide was not included in this version leaving 26 items. The CDI shows moderate to good reliability and construct validity in different age groups (Kovacs 1992). The adapted version of the CDI has also shown to be reliable in children who have lower language abilities and showed high correlation with the original CDI (Theunissen et al. 2011). We also found acceptable Cronbach's alphas in children with (α = .75) and without DLD (α = .74). Participants completed the CDI at Times 1, 2 and 3.
ER strategies
ER strategies were measured with the self‐report Coping scale (Wright et al. 2010), which has shown to be reliable in children with lower language abilities (Theunissen et al. 2011). This questionnaire measures whether children almost never (1), sometimes (2) or often (3) use specific behaviours when they have a problem. Approach strategies were measured with 12 items (‘I try to think of different ways to solve the problem’ and ‘I ask someone in my family for advice’). Avoidant strategies (12 items) measured if children tended to trivialize problems or distract themselves from a problem (‘I tell myself it doesn't matter’ or ‘I do something else to help me forget about it’). The externalizing subscale measured the venting of emotions through verbal or physical aggressive behaviours (e.g., ‘I stamp my feet or slam or bang doors’). In addition, the Worry/Rumination Questionnaire (10 items) (Miers et al. 2007) measured how much children had the tendency to dwell on a problem without trying to change anything (e.g., ‘When I have a problem, I cannot stop thinking about it’). Mean scores were obtained for all scales. The internal consistency of the scales was good for approach, avoidant and worry in both groups (α > .80) and acceptable for externalizing strategies in children with (α = .68) and without DLD (α = .66). Children completed the ER questionnaires at Times 1, 2 and 3. However, the externalizing scale was missing for children without DLD at the third measurement. Additionally, for three participants with and one without DLD the ER strategies were not completed at one time point.
Communication problems
The level of communication problems of children with DLD was measured with the Dutch version of the Childs Communication Checklist—2 (CCC‐2; Norbury et al. 2004, Geurts et al. 2009), which was completed by the parents at Time 1. The CCC‐2 contains eight scales measuring problems with speech, syntax, semantics, coherence and pragmatic problems: initiation of conversations, non‐verbal communication, use of context and stereotypical language. Acceptable to good reliability was found for all scales (table 2). Data were missing for 17 (14.9%) children with DLD due to non‐response of parents or because of inconsistent answers in the positively stated questions. These children were excluded from the analyses with the CCC‐2.
Table 2.
Psychometric properties of the CCC‐2 for children with DLD (n = 97)
| Communication problems | Range | N items | α | Means (SD) |
|---|---|---|---|---|
| Pragmatic | 24–78 | 28 | .83 | 54.86 (7.49) |
| Speech | 8–24 | 7 | .75 | 16.08 (3.57) |
| Syntax | 7–20 | 7 | .59 | 15.31 (2.44) |
| Semantics | 5–18 | 7 | .69 | 14.22 (1.70) |
| Coherence | 6–20 | 7 | .80 | 15.02 (2.35) |
PIQ
PIQ scores of children with DLD were obtained from school or medical files. Children were tested with the Wechlers Intelligence Scale for Children (WISC; Kort et al. 2005), Snijders–Oomen Non‐Verbal Intelligence test (Tellegen and Laros 2011) or Wechlers Non‐Verbal test (Wechsler and Naglieri 2008), which all give an indication of PIQ with a mean of 100 and SD of 15. When data were unavailable, which was the case for 11 children with DLD and all children without DLD, two non‐verbal subtests of the WISC (i.e., Block Design and Picture Arrangement; Kort et al. 2005) were administered at Time 2. These two subtests are highly correlated with full intelligence tests (r = .71, p < .001; Theunissen et al. 2011). Data were missing for six (5.3%) children with DLD and 30 (14.0%) children without DLD, because they did not participate at Time 2 or because parents did not give permission to obtain information.
Procedure
Children were tested individually in a quiet room by a trained test leader. Before the test session started, it was emphasized that there were no right or wrong answers, and that all answers were anonymous. Children were able to read the questions and answer options on a laptop or tablet and privately responded by clicking on an answer. For children with DLD, all questions were read aloud. Parents and children with DLD above 12 years of age signed an informed consent form. The study was approved by the Ethical Committee of Leiden University.
Statistical analyses
In this longitudinal study, we had three measurements of the same participants across time. This means that there is dependency in the data, which violates the assumption of linear regression analyses. Therefore, we used multilevel modelling, which distinguishes between variables of an individual which stay constant across time (such as gender) and variables which change across time (such as age) and models the dependency within the data (Singer and Willett 2003, Snijders and Bosker 2012). Analyses were run using R 3.3.2 (R development Core Team 2016). Multilevel modelling is well suited to deal with longitudinal data, because it can handle missing data points of a participant. Therefore, when participants had missing data on one or two of the three measurements, they were still included in the analyses (Van Buuren 2012). We had missing data at Time 2 (8 with and 29 without DLD) and Time 3 (14 with and 56 without DLD). For 100 children with DLD (87.7%) and 158 children without DLD (73.8%), data were available at all three time points. Participants without DLD who did not participate three times lived in lower SES neighbourhoods than children without DLD who did participate every time (t(56.79) = 3.59, p = .001), and reported lower levels of externalizing strategies (t(136.61) = 2.27, p = .025). For children with DLD, no differences were found between children with and without missing data on any of the study variables. Maximum likelihood estimation was used, assuming the missing data were missing at random (Van Buuren 2012).
As in step‐wise linear regression analyses, in multilevel modelling increasingly more complex models are fitted to the data in order to diminish the unexplained variance in the dependent variable. Models are preferred when they explain more variance, with the lowest number of predictor variables. This is indicated by the Akaike information criterion (AIC). Lower levels of AIC indicate a better model fit (Singer and Willett 2003). Additionally, the likelihood ratio test can be used to test whether the deviance in AIC is significant. The regression weights of the predictor variables of a significant model can be interpreted with the 95% confidence intervals (CI). When the value zero is not in the 95% CI, the predictor is significantly contributing to the model (Singer and Willett 2003, Snijders and Bosker 2012).
We ran preliminary analyses examining the level of depressive symptoms and ER strategies in children with and without DLD across time. We fitted a basic means model with random intercept only (model 0) as a baseline and a model with the control variables gender, neighbourhood SES and age (centralized) as fixed effects (model 1). In the next models, diagnosis (without DLD = 0, DLD = 1) was added (model 2) and the interaction of Age × Diagnosis (model 3), in order to compare the level of depressive symptoms in both groups across time. The same steps were undertaken to compare the level of ER strategies in children with and without DLD across time. All analyses were repeated with the addition of PIQ, which did not result in a better model fit. Therefore, these results were not reported.
We also included age as a random effect in order to allow for individual differences in the rate of change of depressive symptoms during the time frame of the study (Singer and Willett 2003). However, the random slope was not found to contribute to the model. Examination of the data showed that there were many individual differences across time within participants, but that these changes were not well represented by a linear trend (figure 1). Therefore, we were unable to predict the rate of change in depressive symptoms within individuals. However, we were able to explain the individual changes in depressive symptoms across time by modelling time‐changing predictor variables (Singer and Willett 2003).
Figure 1.
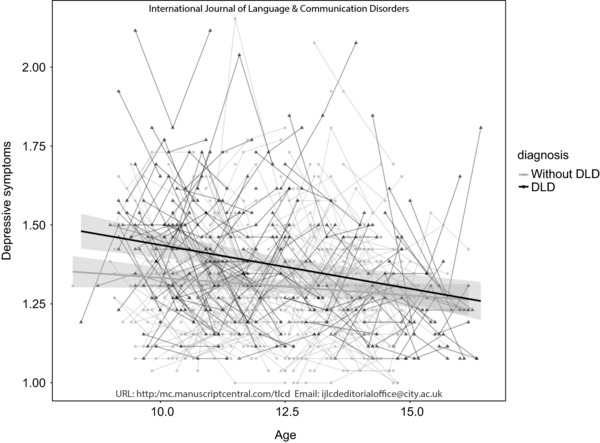
Depressive symptoms of participants with and without DLD. The measurements of one participant are connected by lines. The regression line represents the predicted value based on the age and diagnosis of the participant with 95% confidence intervals (CI).
We hypothesized that the use and the changes in the use of different ER strategies explained differences in the level of depressive symptoms. Therefore, we decomposed the different ER strategies in a person‐specific mean score and a person‐specific change score (Singer and Willett 2003). The mean score represents the mean level of an ER strategy of an individual across the three time points and was added to the model to explain differences between individuals in the level of depressive symptoms. The change scores of an individual were calculated by subtracting the mean score of a strategy from the score on every time point (Time 1 – mean, Time 2 – mean, Time 3 – mean). The combined time‐varying change score represents the changes of an individual across time in the tendency to use an ER strategy. The change scores were added to the model in order to examine whether individual changes in depressive symptoms across the three measurements, could be explained by the changes in ER strategies (Singer and Willett 2003).
First, a model was fitted with gender, neighbourhood SES, age, diagnosis, and the mean and change scores of one of the ER strategies. Second, in order to examine whether the effect of the ER strategy differed for children with and without DLD, the interaction terms of Diagnosis × ER strategy (mean and change) were added to the model. Finally, a model was fitted including all ER strategies in order to examine the unique contribution of the different ER strategies on depressive symptoms. We fitted the final model with and without non‐significant predictors and control variables in order to examine whether the number of predictors in the model obscured small effects, which was not the case.
In order to understand differences within the group of children with DLD, we examined whether the type and severity of their communication problems explained the severity of their depressive symptoms and their ER strategies. Therefore, a model with age and the control variables was compared with a model where one of the CCC‐2 scales was added. Finally, the CCC‐2 scales were added, one at the time, to the multilevel model on depressive symptoms, to examine whether the addition would generate a better model fit in addition to the ER strategies.
Results
Preliminary analyses
The mean levels of depressive symptoms and ER strategies at different ages (in years) of children with and without DLD are shown in table 3. In table 4, the models examining whether there were differences between the groups across time are described.
Table 3.
Mean (SD) levels of depressive symptoms and emotion‐regulation (ER) strategies of children with DLD and typically developing children (TD) at different ages (years)
| n | Depressive symptoms | Approach ER | Avoidant ER | Worry | Externalizing | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | DLD | TD | DLD | TD | DLD | TD | DLD | TD | DLD | TD | DLD | TD |
| <10 | 38 | 40 | 1.45 (0.21) | 1.33 (0.18) | 2.10 (0.41) | 2.13 (0.39) | 2.03 (0.43) | 1.98 (0.34) | 1.92 (0.46) | 1.81 (0.44) | 1.32 (0.34) | 1.23 (0.30) |
| 10 | 65 | 88 | 1.43 (0.17) | 1.32 (0.18) | 2.08 (0.39) | 2.14 (0.43) | 2.07 (0.40) | 1.97 (0.41) | 1.99 (0.49) | 1.9 (0.40) | 1.32 (0.41) | 1.25 (0.32) |
| 11 | 69 | 122 | 1.39 (0.20) | 1.3 (0.18) | 2.12 (0.45) | 2.16 (0.42) | 2.01 (0.42) | 1.95 (0.40) | 2.01 (0.46) | 1.86 (0.40) | 1.35 (0.44) | 1.29 (0.39) |
| 12 | 38 | 108 | 1.42 (0.20) | 1.27 (0.17) | 2.12 (0.46) | 2.20 (0.42) | 2.03 (0.39) | 1.97 (0.39) | 1.94 (0.43) | 1.91 (0.40) | 1.47 (0.47) | 1.25 (0.32) |
| 13 | 30 | 105 | 1.34 (0.21) | 1.33 (0.20) | 2.10 (0.42) | 2.25 (0.43) | 2.09 (0.40) | 1.89 (0.37) | 2.03 (0.45) | 1.90 (0.42) | 1.45 (0.53) | 1.24 (0.36) |
| 14 | 38 | 77 | 1.31 (0.18) | 1.28 (0.17) | 2.38 (0.48) | 2.38 (0.40) | 2.04 (0.45) | 1.87 (0.39) | 1.72 (0.51) | 1.86 (0.38) | 1.25 (0.38) | 1.27 (0.37) |
| ≥15 | 38 | 15 | 1.24 (0.16) | 1.34 (0.10) | 2.29 (0.39) | 2.36 (0.37) | 1.90 (0.44) | 1.76 (0.45) | 1.76 (0.45) | 1.83 (0.30) | 1.18 (0.30) | 1.27 (0.12) |
Note: Children were between 8 and 15 years old at the start of the study and were tested three times, with 9 months in between each measurement. Therefore, the mean scores per age often includes two measurement points of one participant.
Table 4.
Goodness‐of‐fit (Akaike information criterion—AIC) and regression weights with 95% confidence intervals explaining depressive symptoms, and emotion‐regulation strategies (approach, avoidant, worry and externalizing), with the best fitting models and significant predictor variables shown in bold
| Model | AIC | Age | Gender | Neighbouring SES | Diagnosis | Age × Diagnosis | χ² | |
|---|---|---|---|---|---|---|---|---|
| Depressive symptoms | 0 | –647.3 | ||||||
| 1 | –663.7 | –.02 [–.03 to –.01] | –.01 [–.04 to .03] | –.02 [–.03 to –.00] | 22.41*** | |||
| 2 | –671.9 | –.02 [–.03 to –.01] | –.00 [–.04 to .03] | –.01 [–.03 to –.00] | .06 [.02 to .10] | 10.27** | ||
| 3 | –673.9 | –.01 [–.02 to .00] | –.01 [–.04 to .03] | –.01 [–.02 to .01] | .06 [.02 to .10] | –.02 [–.03 to –.00] | 3.92* | |
| Approach | 0 | 829.6 | ||||||
| 1 | 789.5 | .05 [.03 to .07] | .17 [.09 to .24] | .00 [–.03 to .03] | 46.03*** | |||
| 2 | 790.8 | .05 [.03 to .07] | .17 [.09 to .24] | –.00 [–.03 to .03] | –.03 [–.10 to .05] | 0.69 | ||
| 3 | 792.7 | .05 [.03 to .07] | .16 [.09 to .24] | –.00 [–.03 to .03] | –.03 [–.10 to .05] | –.01 [–.05 to .03] | 0.19 | |
| Avoidant | 0 | 778.7 | ||||||
| 1 | 779.8 | –.01 [–.03 to .01] | –.06 [–.13 to .01] | –.02 [–.05 to .02] | 5.02 | |||
| 2 | 776.5 | –.01 [–.03 to .01] | –.05 [–.12 to .06] | –.01 [–.02 to .02] | .09 [.01 to .16] | 5.24* | ||
| 3 | 778.3 | –.01 [–.03 to .01] | –.05 [–.12 to .06] | –.01 [–.02 to .02] | .09 [.01 to .16] | –.01 [–.05 to .03] | 0.23 | |
| Worry | 0 | 767.2 | ||||||
| 1 | 757.6 | –.02 [–.04 to –.00] | .12 [.05 to .20] | –.02 [–.06 to .02] | 15.61** | |||
| 2 | 759.0 | –.02 [–.04 to –.00] | .13 [.05 to .21] | –.01 [–.06 to .02] | .04 [–.06 to .14] | 0.67 | ||
| 3 | 761.0 | –.02 [–.04 to –.00] | .13 [.05 to .21] | –.01 [–.06 to .02] | .04 [–.06 to .14] | –.00 [–.04 to .04] | 0.01 | |
| Externalizing | 0 | 528.7 | ||||||
| 1 | 533.0 | .01 [–.01 to .02] | –.04 [–.12 to .02] | .00 [–.03 to .03] | 1.71 | |||
| 2 | 530.7 | .00 [–.02 to .02] | –.04 [–.11 to .03] | .01 [–.02 to .04] | .08 [.00 to .15] | 4.23 | ||
| 3 | 531.3 | .02 [–.02 to .02] | –.04 [–.11 to .03] | .01 [–.02 to .04] | .07 [–.00 to .15] | –.02 [–.06 to .02] | 1.48 |
Note: * p < .05, ** p < .01; *** p < .001.
Children with DLD reported higher levels of depressive symptoms than children without DLD, as shown by the significant contribution of diagnosis in model 3 (table 4). Additionally, the significant interaction between age and diagnosis showed a small decrease in depressive symptoms across time for children with DLD (–.03 per year), whereas the change in depressive symptoms of children without DLD was not significant. However as can be seen in figure 1, there was high variability within individuals in depressive symptoms across time in both groups.
No differences between children with and without DLD were found for approach strategies, worry, and externalizing strategies, but children with DLD reported higher levels of avoidant strategies than children without DLD (model 2). Children in both groups reported increasing approach strategies and decreasing worry across time (model 1).
Explaining individual differences in depressive symptoms of children with and without DLD
All ER strategies contributed to the prediction of the depressive symptoms in both groups (AIC without ER: –667.0, and with the addition of approach: –691.9***; avoidant: –683.5***; worry; –753.8***; and externalizing: –705.3***). However, the addition of the interaction effects of diagnosis with one of the ER strategies did not provide better model fits (AIC with the interaction diagnosis and approach: –688.2; avoidant: –679,8; worry; –750.1; and externalizing: –704.5). This indicates that the strengths of the effects of the ER strategies on depressive symptoms did not differ between children with and without DLD.
Table 5 shows the unique contribution of the ER strategies explaining the severity of depressive symptoms in children with and without DLD (see table A1 in appendix A for the correlations between all study variables at Time 1). Children in both groups reported less depressive symptoms when they reported higher mean levels of approach strategies, less worry, and less externalizing strategies. Higher mean levels of avoidant strategies also explained less depressive symptoms, but when the other ER strategies were included in the model, this effect did not reach significance anymore. Additionally, increasing levels of avoidant strategies and decreasing levels of worry across the 18 months, explained decreasing levels of depressive symptoms across time within individuals. The change in externalizing strategies was not included in the final analysis, because it was not administered at Time 3. However, when only Times 1 and 2 were taken into account, change in externalizing did not contribute to the model.
Table 5.
Goodness‐of‐fit (Akaike information criterion—AIC) and regression weights with 95% confidence intervals for a regression model explaining depressive symptoms with control variables, diagnosis (DLD = 1), and the mean and change scores of all predictors, with significant predictors shown in bold
| Depressive symptoms | ||
|---|---|---|
| AIC | –842.5*** | |
| Age | –.00 [–.01 to .02] | |
| Neighbourhood SES | –.01 [–.02 to .02] | |
| Gender | –.00 [–.02 to .03] | |
| Diagnosis | .05 [.02 to .07] | |
| Diagnosis × age | –.01 [–.03 to .00] | |
| Approach | Mean | –.15 [–.19 to –.11] |
| Change | –.03 [–.06 to .01] | |
| Avoidant | Mean | –.04 [–.09 to .00] |
| Change | –.06 [–.09 to –.03] | |
| Worry | Mean | .20 [.17 to .24] |
| Change | .06 [.02 to .10] | |
| Externalizing | Mean | .10 [.06 to .15] |
Explaining individual differences within the DLD group
Individual differences in the severity of pragmatic, speech, syntax or coherence problems of children with DLD did not explain the severity of their depressive symptoms. However, more semantic problems of individuals with DLD contributed to the prediction of more depressive symptoms (table 6).
Table 6.
Goodness‐of‐fit (Akaike information criterion—AIC) and regression weights with 95% confidence intervals for regression models explaining depressive symptoms of children with DLD with the control variables, with the addition of semantic problems, and with semantic problems, worry and externalizing strategies, with significant predictors shown in bold
| Depressive symptoms | ||||
|---|---|---|---|---|
| AIC | –175.9 | –178.5* | –213.4*** | |
| Age | –.03 [–.04 to –.01] | –.03 [–.04 to –.01] | –.02 [–.03 to –.01] | |
| Neighbourhood SES | –.00 [–.03 to .02] | –.00 [–.03 to .03] | –.00 [–.03 to .02] | |
| Gender | .02 [–.04 to .09] | .03 [–.04 to .09] | .02 [–.05 to .08] | |
| Semantic problems | .02 [.00 to .04] | .00 [–.01 to .02] | ||
| Worry | Mean | .16 [.09 to .23] | ||
| Change | .04 [–.02 to .10] | |||
| Externalizing | Mean | .14 [.06 to .22] | ||
Approach and avoidant strategies of children with DLD were also not related to any of the CCC‐2 scales. However, semantic problems were related to higher levels of worry (AIC without: 290.7, and with semantic problems: 285.0**; B = .07, 95% CI = [.02 to .13]) and externalizing strategies (AIC without: 205.8, and with semantic problems: 201.6**, B = .05, 95% CI = [.01 to .10]). Finally, more pragmatic problems contributed to the prediction of more externalizing strategies in children with DLD (AIC without: 205.8, and with pragmatic problems: 200.0**; B = .01 95% CI = [.00 to .02]).
Semantic problems thus seem to contribute to both depressive symptoms and maladaptive ER strategies of children with DLD. However, when both the semantic problems and maladaptive ER strategies were included, semantic problems failed to be significant, while the contribution of worry and externalizing remained (table 6). Therefore, we tested whether the relation between semantic problems and depressive symptoms was mediated by worry (mean and change) and externalizing strategies (mean). We used a direct test of mediation following Hayes (2013) with 10,000 clustered bootstraps, testing the indirect path of semantics problems, through worry and externalizing strategies to depressive symptoms. The results indicated that the relation between semantic problems and depressive symptoms was mediated by the mean level of worry and externalizing strategies (95% CI = [.004 to .157] and [.003 to .153] respectively).
Discussion
In line with previous studies (Conti‐Ramsden and Botting 2008, Sullivan et al. 2016), the outcomes of this study showed that children with DLD reported higher levels of depressive symptoms than their peers without DLD. Although the mean level of depressive symptoms decreased over time in older children with DLD, supporting the findings by St. Clair et al. (2011), we found individual differences and changes across time in the level of depressive symptoms in children with and without DLD. The current study explored whether differences in ER strategies and communication problems could elucidate the differences in depressive symptoms across time.
ER strategies explain level and changes in depressive symptoms in both groups
In a community population, worry has been shown to be an important risk factor for the emergence of depression (Muris et al. 2004), which was confirmed in this study. Worry contributed similarly in children with and without DLD to both the level of and changes in depressive symptoms. In line with earlier studies, we found relatively low levels of externalizing strategies (Fields and Prinz 1997, Zimmer‐Gembeck and Skinner 2011), which remained stable over time. We did not find an increase in externalizing strategies during puberty, possibly because a relatively small proportion of the children showed changes in their level of externalizing strategies. However, children from both groups who reported externalizing strategies also reported higher levels of depressive symptoms.
Besides risk factors, we also examined protective factors in this study: approach and avoidant ER, which both explained lower levels of depressive symptoms across time. Children with DLD reported more avoidant strategies, but did not differentially benefit from this strategy in relation to depressive symptoms compared with peers without DLD. Avoidant strategies are sometimes thought to be maladaptive, since the situation causing the negative feelings is not changed. However when a situation is considered uncontrollable, it could be more adaptive to distract oneself from a situation or try to minimize the importance of the situation. In contrast, when a situation is perceived as controllable, it could be more adaptive to act on the situation in order to diminish the chances of reoccurrence of the negative event. ER strategies are therefore especially adaptive when children are able to choose a strategy that fits the situation (Joormann and Stanton 2016). Earlier studies found more behavioural withdrawal in children with DLD (Brinton and Fujiki 1999, Fujiki et al. 2004). The current study suggests that children with DLD use more cognitive avoidant strategies, which appear to help them deal with their negative feelings.
ER strategies explain differences within the DLD group
In contrast to the ER strategies, the severity of communication problems that children with DLD experienced did not explain their depressive symptoms. Semantic problems were associated with more depressive symptoms in children with DLD, but not once ER strategies were accounted for. In fact, the relation between semantic problems and depressive symptoms was mediated by the tendency to worry and to use externalizing strategies. These findings are in line with other studies that did not find any or only weak relations with the level of depressive symptoms in children with DLD and their communication abilities (Beitchman et al. 1996, St. Clair et al. 2011, Sullivan et al. 2016).
These findings suggest that although children with DLD are at greater risk for depressive symptoms, this is not a direct effect of their communication problems in late childhood and adolescence. Beitchman et al. (1996) suggested that communication problems of children in early life may set in motion a different developmental trajectory, where the severity of communication problems has less influence in later developmental stages. Communication problems impede children with DLD in social interactions from an early age, which leads to fewer opportunities for incidental social learning (Rieffe et al. 2016). Social rules and expectations about how to regulate and express emotions are usually not made explicit, but rather ‘go without saying,’ and children typically learn a great deal through the observation of others and through overhearing others’ conversations (Brown and Dunn 1996, Denham and Auerbach 1995). However, it is much more difficult to pick up on implicit rules when children struggle to follow the conversations of others, and have less access to the social world around them. This is reflected in an impaired understanding of other people's motives, emotions, and behaviours in children with DLD (e.g., Andrés‐Roqueta et al. 2016, Bakopoulou and Dockrell 2016). This problem is also found in other groups that have less access to the social world, albeit for different reasons, such as children with a hearing loss (Rieffe et al. 2016).
When children, as a consequence of fewer social learning opportunities early in life, develop less adaptive ways of coping with their emotions, this may also affect their level of depressive symptoms later in life. Our study suggest that children with more communication problems use more maladaptive ER strategies. These maladaptive strategies in turn contributed to the prediction of higher levels of depressive symptoms. These kinds of secondary problems in ER strategies should therefore receive special attention in interventions, to support children with DLD in coping with negative life events, and in preventing negative emotionality.
Higher levels of depressive symptoms in DLD remained
Despite the reduction in the reported symptoms of depression in children with DLD over time, they continued to report more depressive symptoms than their typically developing peers did even when ER strategies were accounted for. Therefore, other explanatory factors should be considered in future research to explain these differences. First, emotion awareness or the ability to identify one's own emotions and their antecedents in the situation causing them, has a strong protective function in the development of depressive symptoms (Sendzik et al. 2017). It has been argued that one first has to understand the cause of one's emotions before one can adaptively cope with them (Gross 1998, Lambie and Marcel 2002). Children with DLD have shown impairments in the recognition of emotions, and in their understanding of emotional antecedents (e.g., Bakopoulou and Dockrell 2016, Fujiki et al. 2004). These capacities are highly dependent on emotion talk with parents in social interaction, and on social learning (Denham and Auerbach 1995, Dunn et al. 1991, Rieffe et al. 2016). It is possible that the associations we found between the semantic language problems of children with DLD and their maladaptive ER strategies are mediated by this ability to understand emotions.
Second, the frequently reported social problems of children with DLD could affect their feelings of well‐being, as a high incidence of being bullied has been shown to explain elevated levels of depressive symptoms in children with DLD (Botting et al. 2016b). Third, children with DLD might be particularly vulnerable to depressive symptoms during transitional periods when they must cope with new and demanding situations. Adolescents with DLD reported a decrease in depressive symptoms when they finished compulsory education. However when these youngsters had difficulties finding jobs as young adults, their level of depressive symptoms increased again (Botting et al. 2016a). Although we found a more gradual decline in depressive symptoms from childhood to adolescence, it is important to consider how contextual changes affect the development of depressive symptoms of children with DLD.
While this longitudinal study provides insight into the underlying mechanisms contributing to the depressive symptoms in a large group of clinically referred children with DLD, there are a few limitations to be addressed. First, this study relied on the use of self‐reports only. Although the internal consistencies of the questionnaires were sufficient, and although internal states can best be measured through self‐report (Lambie and Marcel 2002), the extent to which these symptoms of depression are also related to DLD children's social functioning could be measured through observational studies. Second, we did not include children within the clinical range for depression. Future research could examine the role of ER in depression in a group with a clinical diagnosis for depression.
Conclusions
Depression is one of the most common mental health problems in late childhood and young adolescence, and for children with DLD, the risk for early depressive symptoms is even higher than for those without DLD. It is therefore crucial to have a better understanding of factors contributing to these mental health problems. Children with DLD who had more communication problems were more inclined to use maladaptive strategies, such as worrying and externalizing strategies, which in turn are important risk factors for depressive symptoms. However, an important finding of this study was that independently of communication levels, the risk and protective factors of using different ER strategies made similar contributions to predicting depressive symptoms, in children with and without DLD. Thus it is important for professionals working with children with DLD to know that the same approach and avoidant strategies that help children without DLD seem also to be beneficial for children with DLD. It is critical that future studies further identify factors related to the development of depression for children with DLD, in order to decrease the risk for depression in this particular group.
Acknowledgements
The authors thank all the children who participated in this study, their parents and the schools. The authors also thank Jennifer Schoerke for correcting the English in this paper. This research was supported by the Nuts Ohra Fund (grant number 1303‐049), the Dutch organization for scientific research (NOW; grant number 452‐07‐004) and Royal Dutch Kentalis. Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Appendix A.
Table A1.
Pearson's correlations between Time 1 variables (without DLD/DLD)
| Approach | Avoidant | Worry | Externalizing | Age | PIQ | Education parents | Neighbouring SES | |
|---|---|---|---|---|---|---|---|---|
| Depressive symptoms | –.21** | –.06 | .39*** | .28*** | –.19** | –.07 | –.02 | –.13* |
| Approach | –.01/.46*** | .07 | –.23**/.04 | .13* | .08 | .03 | –.02 | |
| Avoidant | –.10 | .07 | –.05 | –.12* | –.13* | –.08 | ||
| Worry | .13* | –.04 | –.04 | .10 | –.05 | |||
| Externalizing | –.06 | –.07 | –.05 | .01 | ||||
| Age | –.12 | –.04 | –.02 | |||||
| PIQ | .35*** | .14* | ||||||
| Education parents | .24*** |
Notes: Differences in relations in children with and without DLD were tested with Fisher's r to Z transformations: Avoidant and Approach Coping: Z = –4.31, p < .001; and Approach and Externalizing: Z = –.2.31, p = .021.
* p < .05, ** p < .01; *** p < .001.
References
- American Psychiatric Association (APA) , 1994, Diagnostic and statistical manual of mental disorders, 4th Ed. (Washington, DC: APA; ). [Google Scholar]
- American Psychiatric Association (APA) , 2013, Diagnostic and Statistical Manual of Mental Disorders, 5th Ed. (Arlington, VA: APA; ). [Google Scholar]
- Andrés‐Roqueta, C. , Adrian, J. E. , Clemente, R. A. and Villanueva, L. , 2016, Social cognition makes an independent contribution to peer relations in children with specific language impairment. Research in Developmental Disabilities, 49, 277–290. [DOI] [PubMed] [Google Scholar]
- Bakopoulou, I. and Dockrell, J. E. , 2016, The role of social cognition and prosocial behavior in relation to the socio‐emotional competence of primary aged children with specific language impairment. Research in Developmental Disabilities, 49–50, 354–370. [DOI] [PubMed] [Google Scholar]
- Beitchman, J. H. , Brownlie, E. B. , Inglis, A. , Wild, J. , Ferguson, B. , Schachter, D. , Lancee, W. , Wilson, B. and Mathews, R. , 1996, Seven‐year follow‐up of speech/language impaired and control children: psychiatric outcome. Journal of Child Psychology and Psychiatry, 37, 961–997. [DOI] [PubMed] [Google Scholar]
- Bishop, D. V. M. , Snowling, M. J. , Thompson, P. A. , Greenhalgh, T. and The Catalise‐2 Consortium , 2017, Phase 2 of CATALISE: a multinational and multidisciplinary Delphi consensus study of problems with language development: terminology. Journal of Child Psychology and Psychiatry, 58, 1068–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos, M. G. N. , Diamantopoulou, S. , Stockmann, L. , Begeer, S. and Rieffe, C. , 2018, Emotion control predicts internalizing and externalizing behavior problems in boys with and without an autism spectrum disorder. Journal of Autism and Developmental Disorders, 48, 2727–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botting, N. , Durkin, K. , Toseeb, U. , Pickles, A. and Conti‐Ramsden, G. , 2016a, Emotional health, support, and self‐efficacy in young adults with a history of language impairment. British Journal of Developmental Psychology, 34, 538–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botting, N. , Toseeb, U. , Pickles, A. , Durkin, K. and Conti‐Ramsden, G. , 2016b, Depression and anxiety change from adolescence to adulthood in individuals with and without language impairment. PLoS ONE, 11, e0156678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinton, B. and Fujiki, M. , 1999, Social interactional behaviors of children with specific language impairment. Topics in Language Disorder, 19, 49–69. [Google Scholar]
- Brinton, B. , Fujiki, M. , Hurst, N. Q. , Jones, E. R. and Spackman, M. P. , 2015, The ability of children with language impairment to dissemble emotions in hypothetical scenarios and natural situations. Language, Speech, and Hearing Services in Schools, 46, 325–336. [DOI] [PubMed] [Google Scholar]
- Brown, J. R. and Dunn, J. , 1996, Continuities in emotion understanding from three to six years. Child Development, 67, 789–802. [PubMed] [Google Scholar]
- Burks, V. S. , Laird, R. D. and Dodge, K. A. , 1999, Knowledge structures, social information processing, and children's aggressive behavior. Social Development, 8, 220–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti‐Ramsden, G. and Botting, G. , 2008, Emotional health in adolescents with and without a history of specific language impairment (SLI). Journal of Child Psychology and Psychiatry, 49, 516–525. [DOI] [PubMed] [Google Scholar]
- Dahl, R. and Gunnar, M. , 2009, Heightened stress responsiveness and emotional reactivity during pubertal maturation: Implications for psychopathology. Development and Psychopathology, 21, 1–6. [DOI] [PubMed] [Google Scholar]
- Fujiki, M. , Brinton, B. and Clarke, D. , 2002, Emotion regulation in children with specific language impairment. Language, Speech, and Hearing Services in Schools, 33, 102–111. [DOI] [PubMed] [Google Scholar]
- Fujiki, M. , Spackman, M. P. , Brinton, B. and Hall, A. , 2004, The relationship of language and emotion regulation skills to reticence in children with specific language impairment. Journal of Speech, Language, and Hearing Research, 47, 637–646. [DOI] [PubMed] [Google Scholar]
- Denham, S. A. and Auerbach, S. , 1995, Mother–child dialogue about emotions and preschoolers’ emotional competence. Genetic Social General Psychology Monographs, 121, 313–337. [PubMed] [Google Scholar]
- Dunn, J. , Brown, J. and Beardsall, L. , 1991, Family talk about feeling states and children's later understanding of others’ emotions. Developmental Psychology, 27, 448–455. [Google Scholar]
- Fields, L. and Prinz, R. J. , 1997, Coping and adjustment during childhood and adolescence. Clinical Psychology Review, 17, 937–976. [DOI] [PubMed] [Google Scholar]
- Geurts, H. , Hartman, H. , Verté, C. , Oosterlaan, S. , Roeyers, J. and Sergeant, H. , 2009, Pragmatics fragmented: the factor structure of the Dutch children's communication checklist, CCC. International Journal of Language and Communication, 44, 549–574. [DOI] [PubMed] [Google Scholar]
- Gross, J. J. , 1998, The emerging field of emotion regulation: an integrative review. Review of General Psychology, 2, 271–299. [Google Scholar]
- Hayes, A. F. , 2013, Introduction to Mediation, Moderation, and Conditional Process Analysis (New York: Guilford; ). [Google Scholar]
- Horowitz, L. , Jansson, L. , Ljungberg, T. and Hedenbro, M. , 2005, Behavioural patterns of conflict resolution strategies in preschool boys with language impairment in comparison with boys with typical language development. International Journal of Language and Communication Disorders, 40, 431–454. [DOI] [PubMed] [Google Scholar]
- Joorman, J. and Stanton, C. H. , 2016, Examining emotion regulation in depression: a review and future directions. Behaviour Research and Therapy, 86, 35–49. [DOI] [PubMed] [Google Scholar]
- Kort, W. , Schittekatte, M. and Compaan, E. L. 2008, CELF‐4‐NL: Clinical Evaluation of Language Fundatmentals‐vierde‐editie (Amsterdam: Person Assessment and Information; ). [Google Scholar]
- Kort, W. , Schittekatte, M. , Dekker, P. H. , Verhaeghe, P. , Compaan, E. L. , Bosmans, M. and Vermeir, G. , 2005, WISC‐III NL Wechsler Intelligence Scale for Children. Derde Editie NL (Amsterdam: Harcourt Test/Nederlands Instituut voor Psychologen; ). [Google Scholar]
- Ketelaars, M. P. , Cuperus, J. , Jansonius, K. and Verhoeven, L. , 2010, Pragmatic language impairment and associated behavioural problems. International Journal of Language and Communication Disorders, 45, 204–214. [DOI] [PubMed] [Google Scholar]
- Kovacs, M. , 1992, Children's Depression Inventory (North Tonawanda, NY: Multi‐Health Systems; ). [Google Scholar]
- Lambie, J. A. and Marcel, A. J. , 2002, Consciousness and the varieties of emotional experience: a theoretical framework. Psychological Review, 109, 219–259. [DOI] [PubMed] [Google Scholar]
- Miers, A. C. , Rieffe, C. , Meerum Terwogt, M. , Cowan, R. and Linden, W. , 2007, The relation between anger coping strategies, anger mood and somatic complaints in children and adolescents. Journal of Abnormal Child Psychology, 35, 653–664. [DOI] [PubMed] [Google Scholar]
- Muris, P. , Roelofs, J. , Meesters, C. and Boomsma, P. , 2004, Rumination and worry in nonclinical adolescents. Cognitive Therapy and Research, 28, 539–554. [Google Scholar]
- Norbury, C. , Nash, C. , Baird, M. and Bishop, G. , 2004, Using a parental checklist to identify diagnostic groups in children with communication impairment: a validation of the Children's Communication Checklist‐2. International Journal of Language and Communication Disorders, 39, 345–364. [DOI] [PubMed] [Google Scholar]
- Norbury, C. F. , Vamvakas, G. , Gooch, D. , Baird, G. , Charman, T. , Simonoff, E. and Pickles, A. , 2017, Language growth in children with heterogeneous language disorders: a population study. Journal of Child Psychology and Psychiatry, 58, 1092–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team , 2016, R: A language and environment for statistical computing. R Foundation for Statistical Computing. (Vienna, Austria). Retrieved from https://www.r-project.org/ [Google Scholar]
- Rice, M. L. , Sell, M. A. and Hadley, P. A. , 1991, Social interactions of speech, and language impaired children. Journal of Speech and Hearing Research, 34, 1299–1307. [DOI] [PubMed] [Google Scholar]
- Rieffe, C. , De Bruine, M. , De Rooij, M. and Stockmann, L. , 2014, Approach and avoidant emotion regulation prevent depressive symptoms in children with an autism spectrum disorder. International Journal for Developmental Neuroscience, 39, 37–43. [DOI] [PubMed] [Google Scholar]
- Rieffe, C. , Dirks, E. , Van Vlerken, W. and Veiga, G. , 2016, The empathic mind in children with communication impairments: the case of children who are deaf or hard of hearing (DHH); children with an autism spectrum disorder (ASD); and children with specific language impairments (SLI), In Slaughter V. and Rosnay M. De. (eds), Theory of Mind Development in Context (Hove: Psychology Press; ), pp. 106–120. [Google Scholar]
- Rieffe, C , Oosterveld, P. , Miers, A. C. , Meerum Terwogt, M. and Ly, V. , 2008, Emotion awareness and internalising symptoms in children and adolescents: The Emotion Awareness Questionnaire revised. Personality and Individual Differences, 45, 756–761. [Google Scholar]
- Schäfer, J. Ö. , Naumann, E. , Holmes, E. A. , Tuschen‐Caffier, B. and Samson, A. C. , 2017, Emotion regulation strategies in depressive and anxiety symptoms in youth: a meta‐analytic review. Journal of Youth and Adolescence, 46, 261–276. [DOI] [PubMed] [Google Scholar]
- Sendzik, L. , Schäfer, J. , Samson, A. C. , Naumann, E. and Tuschen‐Caffier, B. , 2017, Emotional awareness in depressive and anxiety symptoms in youth: a meta‐analytic review. Journal of Youth and Adolescence, 46, 687–700. [DOI] [PubMed] [Google Scholar]
- Singer, J. D. and Willett, J. B. , 2003, Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence (New York: Oxford University Press; ). [Google Scholar]
- Snijders, T. A. B. and Bosker, R. J. , 2012, Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling, 2nd edn (London: Sage; ). [Google Scholar]
- St. Clair, M. C. , Pickles, A. , Durkin, K. and Conti‐Ramsden, G. , 2011, A longitudinal study of behavioral, emotional and social difficulties in individuals with a history of specific language impairment, Journal of Communication Disorders, 44, 186–199. [DOI] [PubMed] [Google Scholar]
- Sullivan, S. A. , Hollen, L. , Wren, Y. , Thompson, A. D. , Lewis, G. and Zammit, S. , 2016, A longitudinal investigation of childhood communication ability and adolescent psychotic experiences in a community sample. Schizophrenia Research, 173, 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellegen, P. J. and Laros, J. A. , 2011, SON‐R 6‐40. Snijders‐Oomen niet‐verbale intelligentietest. (Amsterdam: Hogrefe uitgevers; ). [Google Scholar]
- Theunissen, S. C. P. M. , Rieffe, C. , Kouwenberg, M , Soede, W. , Briaire, J. J. and Frijns, J. H. M. , 2011, Depression in hearing‐impaired children. International Journal of Pediatric Otorhinolaryngology, 75, 1313–1317. [DOI] [PubMed] [Google Scholar]
- Timler, G. R. , 2008, Social knowledge in children with language impairments: examination of strategies, predicted consequences, and goals in peer conflict situations. Clinical Linguistics and Phonetics, 22, 741–763. [DOI] [PubMed] [Google Scholar]
- Tomblin, J. B. , Records, N. L. , Buckwalter, P. , Zhang, X. , Smith, E. and O'Brien, M. , 1997, Prevalence of specific language impairment in kindergarten children. Journal of Speech Language and Hearing Research, 40, 1245–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Buuren, S. , 2012, Flexible Imputation of Missing Data (Boca Raton, FL: Chapman & Hall/CRC Press; ). [Google Scholar]
- Van Den Bedem, N. P. , Dockrell, J. E. , Van Alphen, P. M. , Kalicharan, S. V. and Rieffe, C. , 2018, Victimization, bullying, and emotional competence: longitudinal associations in (pre)adolescents with and without developmental language disorder. Journal of Speech, Language, and Hearing Research. Jul 9, 1–17. 10.1044/2018_JSLHR-L-17-0429 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Van Harmelen, A. , Gibson, J. L. , St Clair, M. C. , Owens, M. , Brodbeck, J. , Dunn, V. , … Goodyer, I. M. , 2016, Friendships and family support reduce subsequent depressive symptoms in at‐risk adolescents. PLoS One, 11, E0153715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler, D. and Naglieri, J. A. , 2008, Wechsler Nonverbal Scale of Ability Nederlandstalige bewerking. (Amsterdam: Pearson Assessment and Information B.V; ). [Google Scholar]
- Wicks‐Nelson, R. and Israel, A. C. , 2015, Abnormal Child and Adolescent Psychology. DSM‐V Update, 8th edn (Amsterdam: Pearson; ). [Google Scholar]
- Wright, M. , Banerjee, R. , Hoek, W. , Rieffe, C. and Novin, S. , 2010, Depression and social anxiety in children: differential links with coping strategies. Journal of Abnormal Child Psychology, 38, 405–419. [DOI] [PubMed] [Google Scholar]
- Zimmer‐Gembeck, M. J. and Skinner, E. A. , 2011, The development of coping across childhood and adolescence: an integrative review and critique of research. International Journal of Behavioral Development, 35, 1–17. [Google Scholar]


